A Novel Model of Venovenous Extracorporeal Membrane Oxygenation in Rats with Femoral Cannulation and Insights into Hemodynamic Changes
Abstract
:1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Induction and Maintenance of Anesthesia
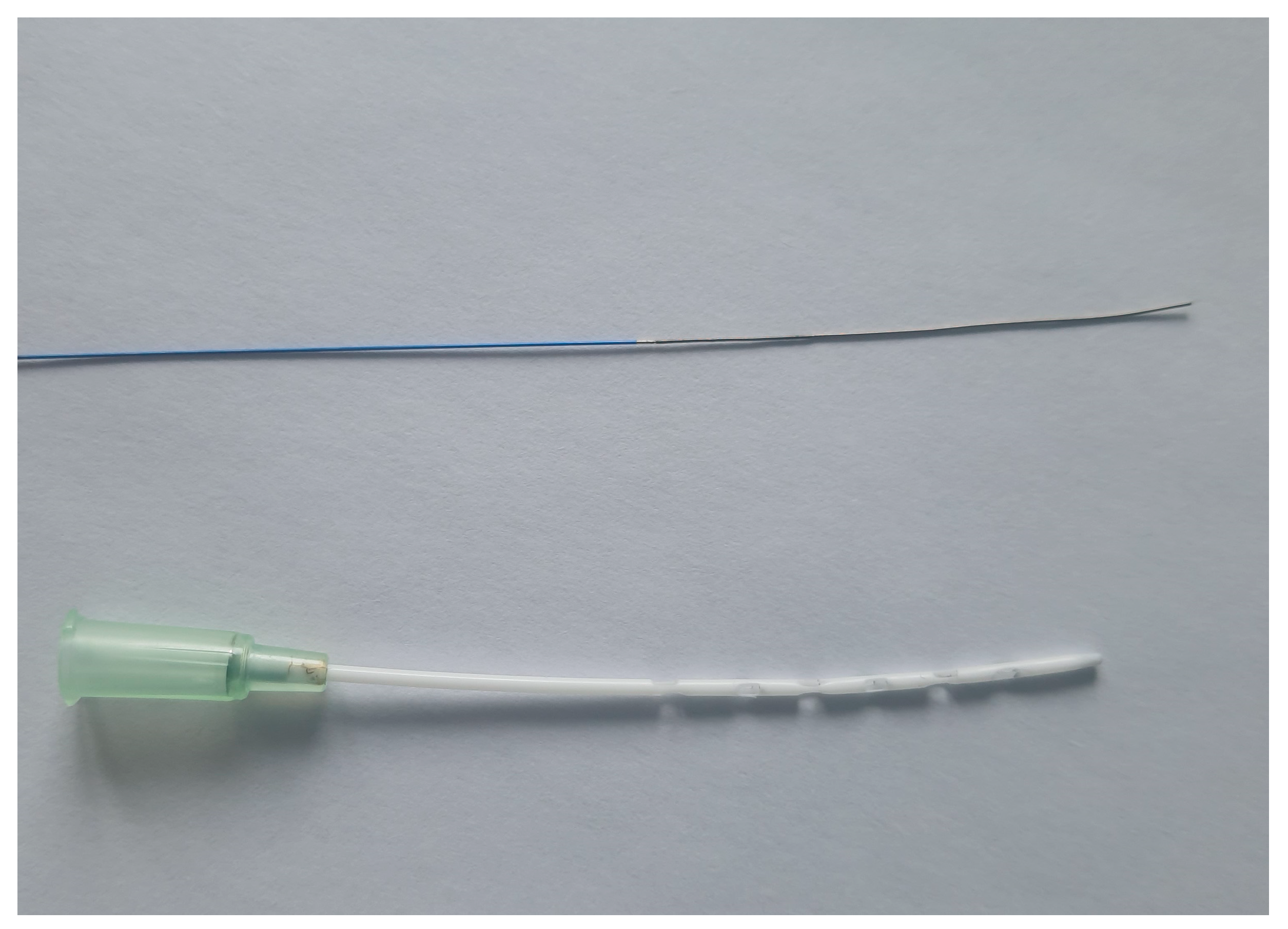
2.3. Cannulation
2.4. Extracorporeal Membrane Oxygenation
2.5. Timepoints of Hemodynamic Measurements
2.6. Blood Analyses
2.7. End of Experiments
2.8. Enzyme-Linked Immunosorbent Assays
2.9. Statistics
3. Results
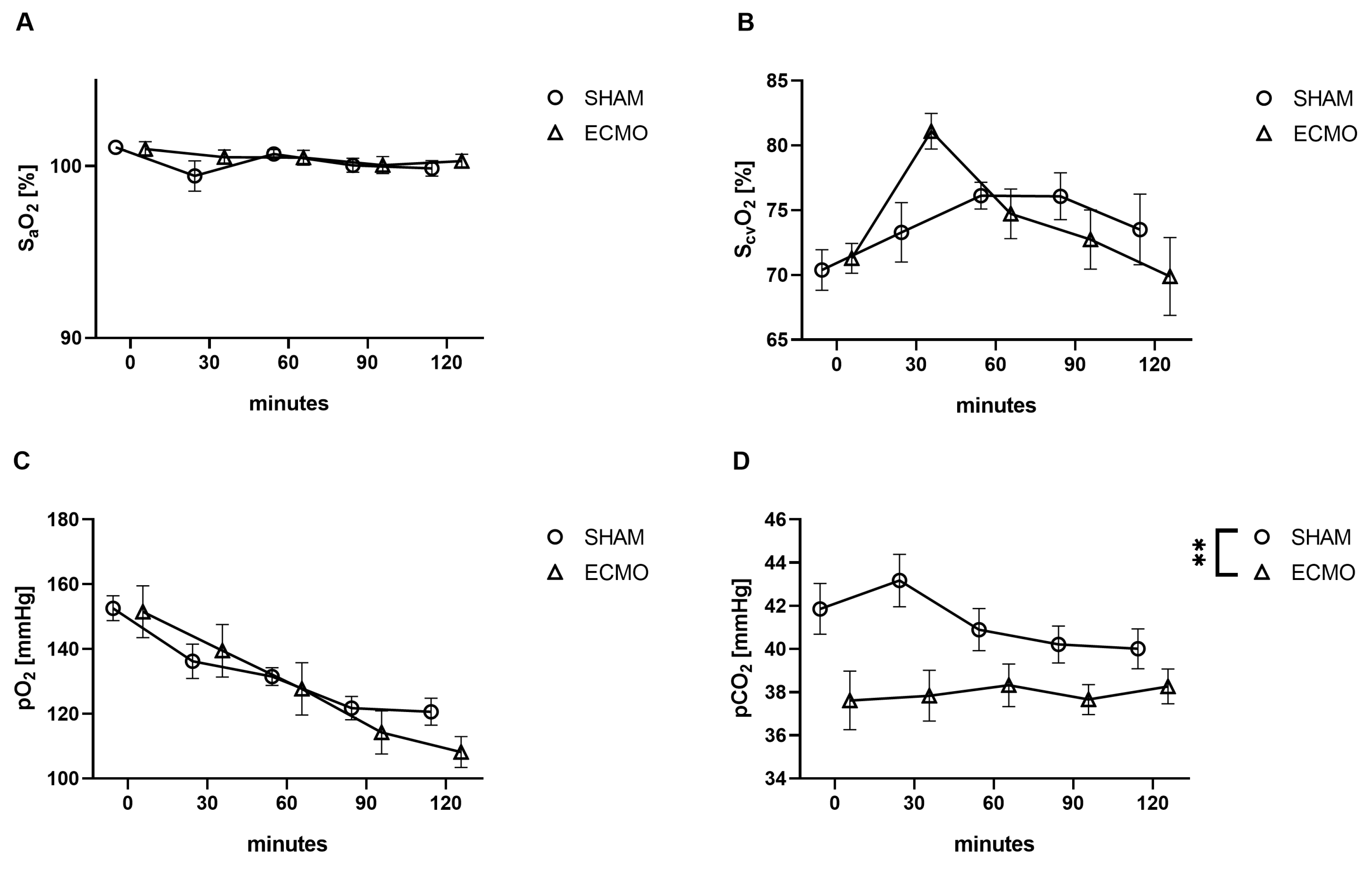
3.1. Blood Gas Analysis
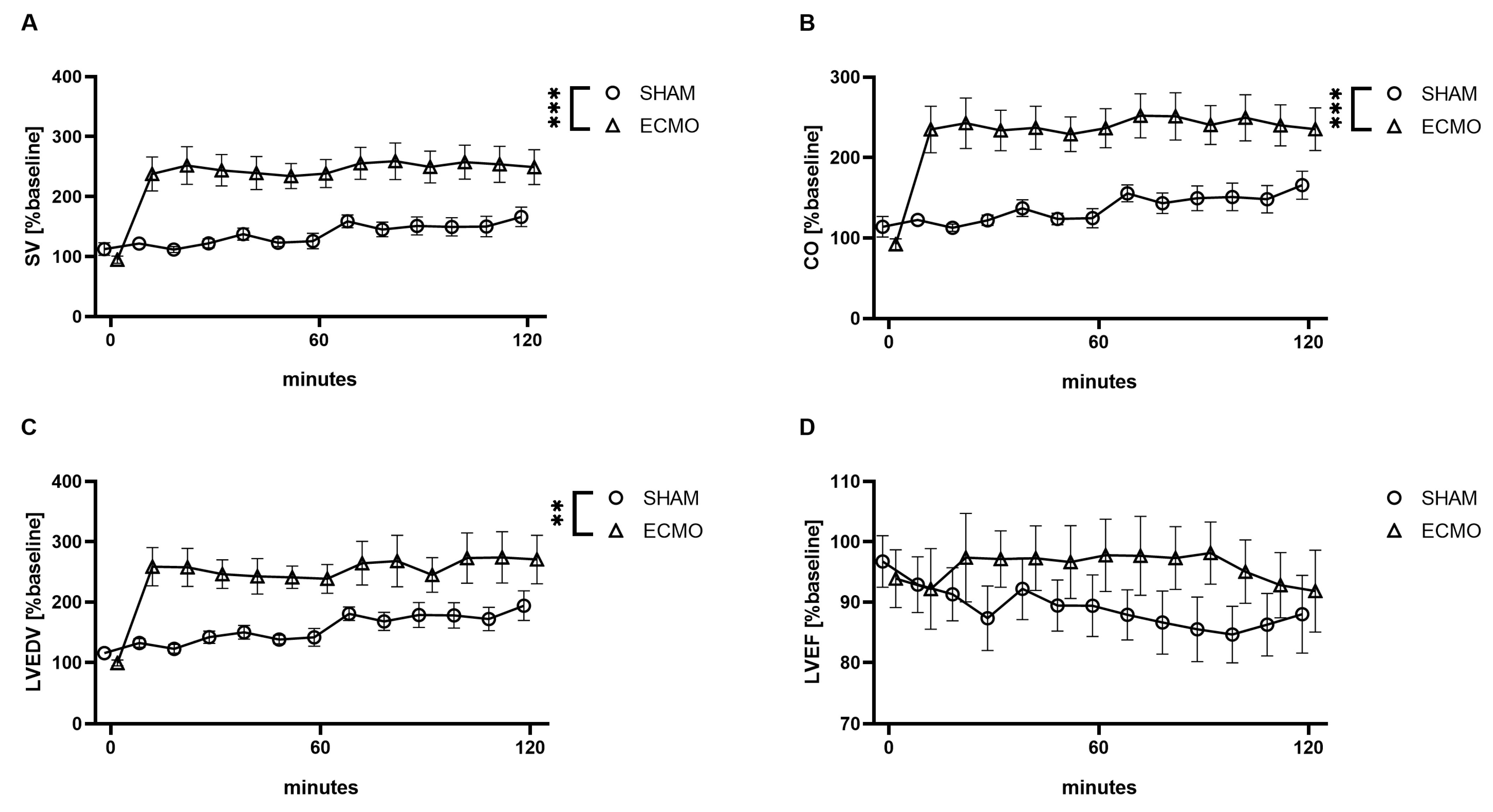
3.2. Hemodynamic Parameters
3.3. Inflammatory Parameters
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gibbon, J.H. Application of a mechanical heart and lung apparatus to cardiac surgery. Minn. Med. 1954, 37, 171–185. [Google Scholar] [PubMed]
- Hill, J.D.; Le O’Brien, T.G.; Murray, J.J.; Dontigny, L.; Bramson, M.L.; Osborn, J.J.; Gerbode, F. Prolonged Extracorporeal Oxygenation for Acute Post-Traumatic Respiratory Failure (Shock-Lung Syndrome). N. Engl. J. Med. 1972, 286, 629–634. [Google Scholar] [CrossRef] [PubMed]
- Peek, G.J.; Elbourne, D.; Mugford, M.; Tiruvoipati, R.; Wilson, A.; Allen, E.; Clemens, F.; Firmin, R.; Hardy, P.; Hibbert, C.; et al. Randomised controlled trial and parallel economic evaluation of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR). Health Technol. Assess. 2010, 14, 1–46. [Google Scholar] [CrossRef] [PubMed]
- Noah, M.A.; Peek, G.J.; Finney, S.J.; Griffiths, M.J.; Harrison, D.A.; Grieve, R.; Sadique, M.Z.; Sekhon, J.S.; McAuley, D.F.; Firmin, R.K.; et al. Referral to an extracorporeal membrane oxygenation center and mortality among patients with severe 2009 influenza A(H1N1). JAMA 2011, 306, 1659–1668. [Google Scholar] [CrossRef] [PubMed]
- Barbaro, R.P.; MacLaren, G.; Boonstra, P.S.; Combes, A.; Agerstrand, C.; Annich, G.; Diaz, R.; Fan, E.; Hryniewicz, K.; Lorusso, R.; et al. Extracorporeal membrane oxygenation for COVID-19: Evolving outcomes from the international Extracorporeal Life Support Organization Registry. Lancet 2021, 398, 1230–1238. [Google Scholar] [CrossRef] [PubMed]
- Millar, J.E.; Fanning, J.P.; McDonald, C.I.; McAuley, D.F.; Fraser, J.F. The inflammatory response to extracorporeal membrane oxygenation (ECMO): A review of the pathophysiology. Crit. Care 2016, 20, 387. [Google Scholar] [CrossRef] [PubMed]
- Gattinoni, L.; Vasques, F.; Quintel, M. Use of ECMO in ARDS: Does the EOLIA trial really help? Crit. Care 2018, 22, 171. [Google Scholar] [CrossRef] [PubMed]
- Edinger, F.; Schneck, E.; Schulte, C.; Gehron, J.; Mueller, S.; Sander, M.; Koch, C. Comparison of the effect of membrane sizes and fibre arrangements of two membrane oxygenators on the inflammatory response, oxygenation and decarboxylation in a rat model of extracorporeal membrane oxygenation. BMC Cardiovasc. Disord. 2020, 20, 294. [Google Scholar] [CrossRef]
- Edinger, F.; Schneck, E.; Schulte, C.; Schmidt, G.; Gehron, J.; Sander, M.; Koch, C. Impact of the inspiratory oxygen fraction on the cardiac output during jugulo-femoral venoarterial extracorporeal membrane oxygenation in the rat. BMC Cardiovasc. Disord. 2022, 22, 174. [Google Scholar] [CrossRef] [PubMed]
- Fujii, Y.; Shirai, M.; Inamori, S.; Takewa, Y.; Tatsumi, E. A novel small animal extracorporeal circulation model for studying pathophysiology of cardiopulmonary bypass. J. Artif. Organs 2015, 18, 35–39. [Google Scholar] [CrossRef] [PubMed]
- Fujii, Y.; Shirai, M.; Tsuchimochi, H.; Pearson, J.T.; Takewa, Y.; Tatsumi, E.; Taenaka, Y. Hyperoxic Condition Promotes an Inflammatory Response During Cardiopulmonary Bypass in a Rat Model. Artif. Organs 2013, 37, 1034–1040. [Google Scholar] [CrossRef] [PubMed]
- Fujii, Y.; Tatsumi, E.; Nakamura, F.; Oite, T. PaO2 greater than 300 mmHg promotes an inflammatory response during extracorporeal circulation in a rat extracorporeal membrane oxygenation model. J. Thorac. Dis. 2020, 12, 749–757. [Google Scholar] [CrossRef] [PubMed]
- Edinger, F.; Schmitt, C.; Koch, C.; McIntosh, J.M.; Janciauskiene, S.; Markmann, M.; Sander, M.; Padberg, W.; Grau, V. Application of alpha1-antitrypsin in a rat model of veno-arterial extracorporeal membrane oxygenation. Sci. Rep. 2021, 11, 15849. [Google Scholar] [CrossRef] [PubMed]
- Koning, N.J.; de Lange, F.; Vonk, A.B.A.; Ahmed, Y.; van den Brom, C.E.; Bogaards, S.; van Meurs, M.; Jongman, R.M.; Schalkwijk, C.G.; Begieneman, M.P.V.; et al. Impaired microcirculatory perfusion in a rat model of cardiopulmonary bypass: The role of hemodilution. Am. J. Physiol.-Heart Circ. Physiol. 2016, 310, H550–H558. [Google Scholar] [CrossRef] [PubMed]
- Samarska, I.V.; Henning, R.H.; Buikema, H.; Bouma, H.R.; Houwertjes, M.C.; Mungroop, H.; Struys, M.M.; Absalom, A.R.; Epema, A.H. Troubleshooting the rat model of cardiopulmonary bypass: Effects of avoiding blood transfusion on long-term survival, inflammation and organ damage. J. Pharmacol. Toxicol. Methods 2013, 67, 82–90. [Google Scholar] [CrossRef] [PubMed]
- Magnet, I.A.M.; Ettl, F.; Schober, A.; Warenits, A.-M.; Grassmann, D.; Wagner, M.; Schriefl, C.; Clodi, C.; Teubenbacher, U.; Högler, S.; et al. Extracorporeal Life Support Increases Survival After Prolonged Ventricular Fibrillation Cardiac Arrest in the Rat. SHOCK 2017, 48, 674–680. [Google Scholar] [CrossRef] [PubMed]
- Fujii, Y.; Sumikura, H.; Nagahama, D. Establishment of a novel miniature veno-venous extracorporeal membrane oxygenation model in the rat. Artif. Organs 2021, 45, 63–67. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Zhang, R.; Zhai, K.; Li, J.; Yao, M.; Wei, S.; Cheng, X.; Yang, J.; Gao, B.; Wu, X.; et al. Venovenous extracorporeal membrane oxygenation promotes alveolar epithelial recovery by activating Hippo/YAP signaling after lung injury. J. Heart Lung Transplant. Off. Publ. Int. Soc. Heart Transplant. 2022, 41, 1391–1400. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Huang, J.; Zhang, R.; Wang, S.; Cheng, X.; Zhang, P.; Zhai, K.; Wang, W.; Liu, D.; Gao, B. Establishment of a venovenous extracorporeal membrane oxygenation in a rat model of acute respiratory distress syndrome. Perfusion 2023, 38, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Cho, H.-J.; Kayumov, M.; Kim, D.; Lee, K.; Onyekachi, F.O.; Jeung, K.-W.; Kim, Y.; Suen, J.Y.; Fraser, J.F.; Jeong, I.-S. Acute Immune Response in Venoarterial and Venovenous Extracorporeal Membrane Oxygenation Models of Rats. ASAIO J. 2021, 67, 546–553. [Google Scholar] [CrossRef] [PubMed]
- Zhang, R.; Zhai, K.; Huang, J.; Wei, S.; Yang, J.; Zhang, Y.; Wu, X.; Li, Y.; Gao, B. Sevoflurane alleviates lung injury and inflammatory response compared with propofol in a rat model of VV ECMO. Perfusion 2022, 39, 142–150. [Google Scholar] [CrossRef] [PubMed]
- Kilkenny, C.; Browne, W.J.; Cuthill, I.C.; Emerson, M.; Altman, D.G. Improving bioscience research reporting: The ARRIVE guidelines for reporting animal research. PLoS Biol. 2010, 8, e1000412. [Google Scholar] [CrossRef] [PubMed]
- Dong, G.-H.; Xu, B.; Wang, C.-T.; Qian, J.-J.; Liu, H.; Huang, G.; Jing, H. A rat model of cardiopulmonary bypass with excellent survival. J. Surg. Res. 2005, 123, 171–175. [Google Scholar] [CrossRef] [PubMed]
- Engels, M.; Bilgic, E.; Pinto, A.; Vasquez, E.; Wollschläger, L.; Steinbrenner, H.; Kellermann, K.; Akhyari, P.; Lichtenberg, A.; Boeken, U. A cardiopulmonary bypass with deep hypothermic circulatory arrest rat model for the investigation of the systemic inflammation response and induced organ damage. J. Inflamm. 2014, 11, 26. [Google Scholar] [CrossRef] [PubMed]
- Abrams, D.; Bacchetta, M.; Brodie, D. Recirculation in venovenous extracorporeal membrane oxygenation. ASAIO J. 2015, 61, 115–121. [Google Scholar] [CrossRef]
- Zeng, C.; Lagier, D.; Lee, J.-W.; Melo, M.F.V. Perioperative Pulmonary Atelectasis—Part I: Biology and Mechanisms. Anesthesiology 2022, 136, 181–205. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, M.; Tachon, G.; Devilliers, C.; Muller, G.; Hekimian, G.; Bréchot, N.; Merceron, S.; Luyt, C.E.; Trouillet, J.-L.; Chastre, J.; et al. Blood oxygenation and decarboxylation determinants during venovenous ECMO for respiratory failure in adults. Intensive Care Med. 2013, 39, 838–846. [Google Scholar] [CrossRef] [PubMed]
- Rose-John, S.; Winthrop, K.; Calabrese, L. The role of IL-6 in host defence against infections: Immunobiology and clinical implications. Nat. Rev. Rheumatol. 2017, 13, 399–409. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Xiao, C.; Zheng, H. Prognostic value of inflammatory cytokine detection for sepsis patients in ICU: A meta-analysis. Am. J. Transl. Res. 2024, 16, 2612–2621. [Google Scholar] [CrossRef] [PubMed]
- Agoston, D.V. How to Translate Time? The Temporal Aspect of Human and Rodent Biology. Front. Neurol. 2017, 8, 92. [Google Scholar] [CrossRef] [PubMed]
- Seok, J.; Warren, H.S.; Cuenca, A.G.; Mindrinos, M.N.; Baker, H.V.; Xu, W.; Richards, D.R.; McDonald-Smith, G.P.; Gao, H.; Hennessy, L.; et al. Genomic responses in mouse models poorly mimic human inflammatory diseases. Proc. Natl. Acad. Sci. USA 2013, 110, 3507–3512. [Google Scholar] [CrossRef] [PubMed]


| 0 Min | 30 Min | 60 Min | 90 Min | 120 Min | ||
|---|---|---|---|---|---|---|
| pH | ECMO | 7.38 [7.37–7.43] | 7.39 [7.35–7.43] | 7.40 [7.39–7.41] | 7.39 [7.37–7.42] | 7.40 [7.37–7.42] |
| SHAM | 7.38 [7.35–7.39] | 7.36 [7.35–7.40] | 7.40 [7.39–7.41] | 7.37 [7.34–7.42] | 7.36 [7.35–7.41] | |
| Bic | ECMO | 23.4 [22.7–24.1] | 23.0 [22.0–23.1] | 24.0 [23.3–24.9] | 22.9 [22.0–24.2] | 23.7 [23.1–24.0] |
| [mmol/L] | SHAM | 22.9 [21.8–24.7] | 23.2 [22.5–26.1] | 23.8 [22.4–26.6] | 23.4 [21.7–25.9] | 23.2 [22.1–24.6] |
| BE | ECMO | −1.6 [−2.6–−0.9] | −1.7 [−3.0–−1.1] | −1.0 [−1.6–0.2] | −1.8 [−2.7–−0.3] | −1.1 [−1.6–−0.6] |
| SHAM | −1.4 [−3.2–0.2] | −1.4 [−2.2–1.4] | −0.8 [−2.4–2.3] | −1.7 [−3–1.2] | −2.0 [−3.4–−0.2] | |
| Lac ** | ECMO | 1.5 [1.0–1.6] | 1.2 [1.1–1.4] | 1.0 [0.9–1.2] | 1.3 [1.1–1.5] | 1.2 [1.0–1.3] |
| [mmol/L] | SHAM | 1.5 [1.2–1.7] | 1.0 [0.9–1.0] | 0.9 [0.8–1.1] | 0.9 [0.9–1.1] | 0.9 [0.8–1.1] |
| Hb *** | ECMO | 14.4 [14.1–14.8] | 7.6 [7.4–7.8] | 7.5 [7.3–8.0] | 7.4 [6.8–7.6] | 7.1 [6.8–7.5] |
| [g/dL] | SHAM | 14.2 [13.8–15.0] | 12.7 [12.0–14.5] | 12.2 [11.5–13.2] | 11.0 [9.9–11.7] | 10.1 [9.6–11.0] |
| Glu * | ECMO | 161 [140–172] | 126 [121–131] | 117 [112–122] | 114 [111–117] | 118 [111–124] |
| [mg/dL] | SHAM | 166 [160–186] | 139 [129–149] | 129 [119–136] | 121 [113–125] | 115 [110–121] |
| Na | ECMO | 144 [142–144] | 144 [143–145] | 145 [144–146] | 146 [144–146] | 145 [144–146] |
| [mmol/L] | SHAM | 141 [141–145] | 143 [141–144] | 143 [142–144] | 143 [142–145] | 143 [142–145] |
| K ** | ECMO | 4.1 [3.9–4.3] | 4.0 [3.8–4.1] | 4.1 [3.9–4.1] | 4.1 [ 3.9–4.3] | 4.1 [4.0–4.3] |
| [mmol/L] | SHAM | 4.2 [3.9–4.5] | 4.5 [4.4–4.5] | 4.4 [4.3–4.5] | 4.3 [4.2–4.4] | 4.3 [4.1–4.4] |
| Cl ** | ECMO | 109 [108–110] | 112 [110–113] | 112 [111–113] | 113 [112–114] | 113 [112–114] |
| [mmol/L] | SHAM | 107 [106–109] | 109 [107–111] | 109 [107–111] | 111 [109–112] | 112 [110–113] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Edinger, F.; Zajonz, T.; Mayer, N.; Schmidt, G.; Schneck, E.; Sander, M.; Koch, C. A Novel Model of Venovenous Extracorporeal Membrane Oxygenation in Rats with Femoral Cannulation and Insights into Hemodynamic Changes. Biomedicines 2024, 12, 1819. https://doi.org/10.3390/biomedicines12081819
Edinger F, Zajonz T, Mayer N, Schmidt G, Schneck E, Sander M, Koch C. A Novel Model of Venovenous Extracorporeal Membrane Oxygenation in Rats with Femoral Cannulation and Insights into Hemodynamic Changes. Biomedicines. 2024; 12(8):1819. https://doi.org/10.3390/biomedicines12081819
Chicago/Turabian StyleEdinger, Fabian, Thomas Zajonz, Nico Mayer, Götz Schmidt, Emmanuel Schneck, Michael Sander, and Christian Koch. 2024. "A Novel Model of Venovenous Extracorporeal Membrane Oxygenation in Rats with Femoral Cannulation and Insights into Hemodynamic Changes" Biomedicines 12, no. 8: 1819. https://doi.org/10.3390/biomedicines12081819
APA StyleEdinger, F., Zajonz, T., Mayer, N., Schmidt, G., Schneck, E., Sander, M., & Koch, C. (2024). A Novel Model of Venovenous Extracorporeal Membrane Oxygenation in Rats with Femoral Cannulation and Insights into Hemodynamic Changes. Biomedicines, 12(8), 1819. https://doi.org/10.3390/biomedicines12081819








