Combined Effects of NMES and Mendelsohn Maneuver on the Swallowing Function and Swallowing–Quality of Life of Patients with Stroke-Induced Sub-Acute Swallowing Disorders
Abstract
:1. Introduction
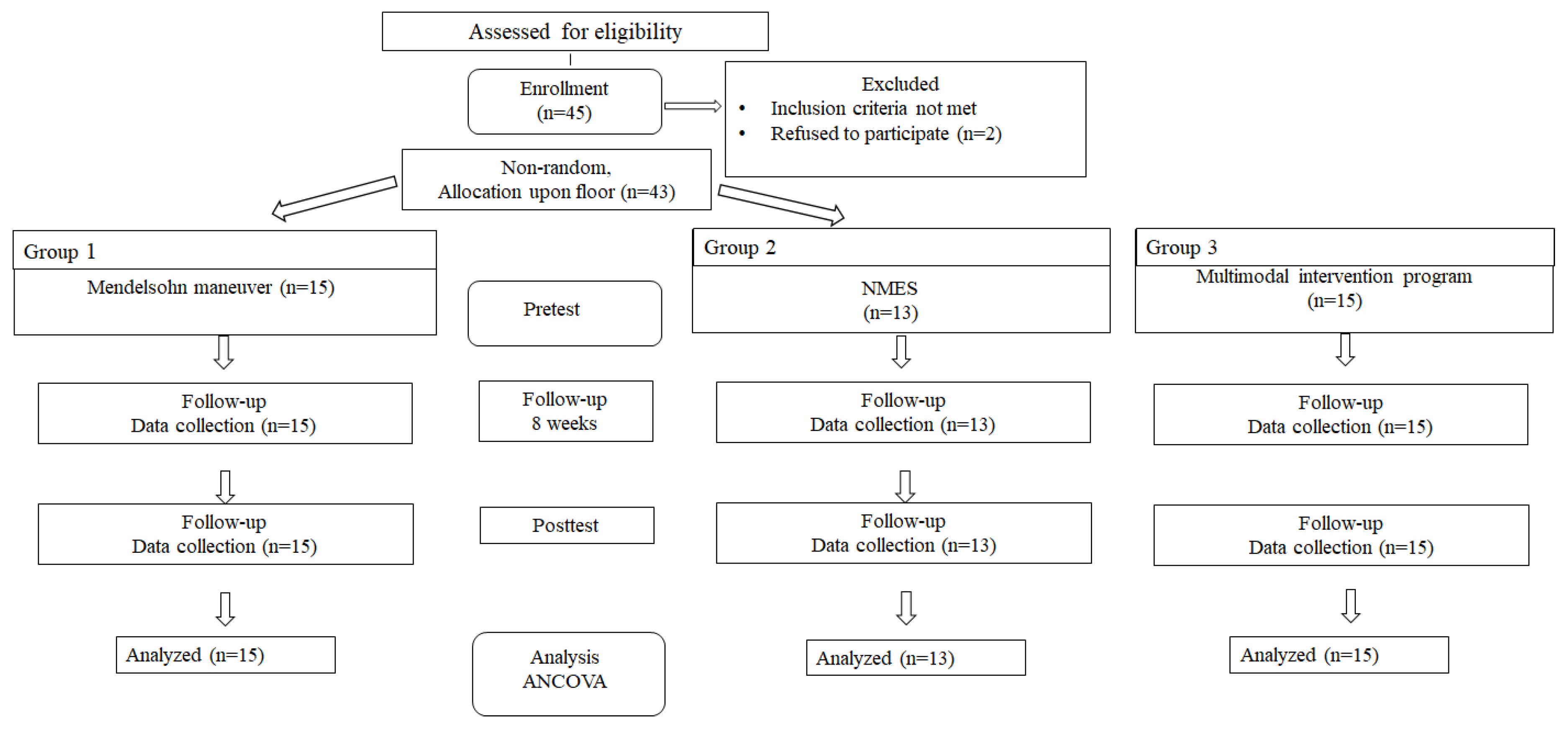
2. Methods and Materials
2.1. Study Subjects
2.2. Measurements
2.3. Measurement
2.3.1. Mendelsohn Maneuver
2.3.2. NMES
2.3.3. Compound Intervention Program
2.3.4. Swallowing Function
2.3.5. Swallowing-Related Quality of Life
2.3.6. Longest Occupation
2.4. Statistical Analyses
3. Results
3.1. Pre-Homogeneity Test for FDS and SWAL–QOL
3.2. Changes in the Swallowing Function, According to Intervention Methods
3.3. Changes in Swallowing–Quality of Life According to Intervention Methods
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Daniels, S.K.; Brailey, K.; Priestly, D.H.; Herrington, L.R.; Weisberg, L.A.; Foundas, A.L. Aspiration in patients with acute stroke. Arch. Phys. Med. Rehabil. 1998, 79, 14–19. [Google Scholar] [CrossRef]
- Kidd, D.; Lawson, J.; Nesbitt, R.; MacMahon, J. Aspiration in acute stroke: A clinical study with videofluoroscopy. QJM Int. J. Med. 1993, 86, 825–829. [Google Scholar]
- Perry, L.; Love, C.P. Screening for dysphagia and aspiration in acute stroke: A systematic review. Dysphagia 2001, 16, 7–18. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.Y.; Lee, Y.W.; Cho, E.Y.; Kang, H.W. The phenomenological study on the experience of nasogastric tube feeding among cerebral stroke patients with dysphagia. Korean J. Adult Nurs. 2014, 26, 592–602. [Google Scholar] [CrossRef]
- Ekberg, O.; Hmady, S.; Wuttge-Hanning, A.; Ortege, P. Social and psychological burden of dysphagia: Its impact on diagnosis and treatment. Dysphagia 2002, 17, 139–146. [Google Scholar] [CrossRef] [PubMed]
- Critchlow, J.; Bauer-Wu, S.M. Dehydration in terminally ill patients: Perceptions of longterm care nurse. J. Gerontol. Nurs. 2002, 28, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Logemann, J.A. The evaluation and treatment of swallowing disorders. Curr. Opin. Otolaryngol. Head Neck Surg. 1998, 6, 395–400. [Google Scholar] [CrossRef]
- Sura, L.; Madhavan, A.; Carnaby, G.; Crary, M.A. Dysphagia in the elderly: Management and nutritional considerations. Clin. Interv. Aging 2012, 7, 287–298. [Google Scholar]
- McCullough, G.H.; Kim, Y. Effects of the Mendelsohn maneuver on extent of hyoid movement and UES opening post-stroke. Dysphagia 2013, 28, 511–519. [Google Scholar] [CrossRef]
- McCullough, G.H.; Kamarunas, E.; Mann, G.C.; Schmidley, J.W.; Robbins, J.A.; Crary, M.A. Effects of Mendelsohn maneuver on measures of swallowing duration post stroke. Top. Stroke Rehabil. 2012, 19, 234–243. [Google Scholar] [CrossRef] [Green Version]
- Logemann, J.A.; Rademaker, A.; Pauloski, B.R.; Kelly, A.; Stangl-McBreen, C.; Antinoja, J.; Grande, B.; Farquharson, J.; Kern, M.; Easterling, C.; et al. A randomized study comparing the Shaker exercise with traditional therapy: A preliminary study. Dysphagia 2009, 24, 403–411. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Permsirivanich, W.; Tipchatyotin, S.; Wongchai, M.; Leelamanit, V.; Setthawatcharawanich, S.; Sathirapanya, P.; Phabphal, K.; Juntawises, U.; Boonmeeprakob, A. Comparing the effects of rehabilitation swallowing therapy vs. neuromuscular electrical stimulation therapy among stroke patients with persistent pharyngeal dysphagia: A randomized controlled study. J. Med. Assoc. Thail. 2009, 92, 259–265. [Google Scholar]
- Carnaby-Mann, G.D.; Crary, M.A. Examining the evidence on neuromuscular electrical stimulation for swallowing: A meta-analysis. Arch. Otolaryngol. Head Neck Surg. 2007, 133, 564–571. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, L.; Li, Y.; Huang, R.; Yin, J.; Shen, Y.; Shi, J. The value of adding transcutaneous neuromuscular electrical stimulation (VitalStim) to traditional therapy for post-stroke dysphagia: A randomized controlled trial. Eur. J. Phys. Rehabil. Med. 2015, 51, 71–78. [Google Scholar]
- Humbert, I.A.; Poletto, C.J.; Saxon, K.G.; Kearney, P.R.; Ludlow, C.L. The effect of surface electrical stimulation on vocal fold position. Laryngoscope 2008, 118, 14–19. [Google Scholar] [CrossRef] [Green Version]
- Ludlow, C.L.; Humbert, I.; Saxon, K.; Poletto, C.; Sonies, B.; Crujido, L. Effects of surface electrical stimulation both at rest and during swallowing in chronic pharyngeal Dysphagia. Dysphagia 2007, 22, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Steele, C.M.; Thrasher, A.T.; Popovic, M.R. Electric stimulation approaches to the restoration and rehabilitation of swallowing: A review. Neurol. Res. 2007, 29, 9–15. [Google Scholar] [CrossRef]
- Shaw, G.Y.; Sechtem, P.R.; Searl, J.; Keller, K.; Rawi, T.A.; Dowdy, E. Transcutaneous neuromuscular electrical stimulation (VitalStim) curative therapy for severe dysphagia: myth or reality? Ann. Otol. Rhinol. 2007, 116, 36–44. [Google Scholar] [CrossRef]
- Tan, C.; Liu, Y.; Li, W.; Liu, J.; Chen, L. Transcutaneous neuromuscular electrical stimulation can improve swallowing function in patients with dysphagia caused by non-stroke diseases: A meta-analysis. J. Oral Rehabil. 2013, 40, 472–480. [Google Scholar] [CrossRef]
- Cohen, J. A power primer. In Methodological Issues & Strategies in Clinical Research; Kazdin, A.E., Ed.; American Psychological Association: Washington, DC, USA, 2003. [Google Scholar]
- Kang, Y.; Na, D.L.; Hahn, S.A. validity study on the Korean Mini-Mental State Examination (K-MMSE) in dementia patients. J. Korean Neurol. Assoc. 1997, 15, 300–308. [Google Scholar]
- Han, T.R.; Paik, N.J.; Park, J.W. Quantifying swallowing function after stroke: A functional dysphagia scale based on videofluoroscopic studies. Arch. Phys. Med. Rehabil. 2001, 82, 677–682. [Google Scholar] [CrossRef] [PubMed]
- McHorney, C.A.; Robbins, J.; Lomax, K.; Rosenbek, J.C.; Chignell, K.; Kramer, A.E.; Bricker, D.E. The SWAL–QOL and SWAL–CARE outcomes tool for oropharyngeal dysphagia in adults: III. Documentation of reliability and validity. Dysphagia 2002, 17, 97–114. [Google Scholar] [CrossRef] [PubMed]
- Korea National Statistical Office. Korean Standard Classification of Occupations; Korea National Statistical Office: Daejeon, Korea, 2007. [Google Scholar]
- Ashford, J.; McCabe, D.; Wheeler-Hegland, K.; Frymark, T.; Mullen, R.; Musson, N.; Schooling, T.; Hammond, C.S. Evidence-based systematic review: Oropharyngeal dysphagia behavioral treatments. Part III—Impact of dysphagia treatments on populations with neurological disorders. J. Rehabil. Res. Dev. 2009, 46, 195–204. [Google Scholar] [CrossRef] [PubMed]
- Speyer, R.; Baijens, L.; Heijnen, M.; Zwijnenberg, I. Effects of therapy in oropharyngeal dysphagia by speech and language therapists: A systematic review. Dysphagia 2010, 25, 40–65. [Google Scholar] [CrossRef] [Green Version]
- Lake, D.A. Neuromuscular electrical stimulation. Sports Med. 1992, 13, 320–336. [Google Scholar] [CrossRef]
- Bulow, M.; Speyer, R.; Baijens, L.; Woisard, V.; Ekberg, O. Neuromuscular electrical stimulation in stroke patients with oral and pharyngeal dysfunction. Dysphagia 2008, 23, 302–309. [Google Scholar] [CrossRef]
- Chen, Y.W.; Chang, K.H.; Chen, H.C.; Liang, W.M.; Wang, Y.H.; Lin, Y.N. The effects of surface neuromuscular electrical stimulation on post-stroke dysphagia: A systemic review and meta-analysis. Clin. Rehabil. 2016, 30, 24–35. [Google Scholar] [CrossRef]
- Blumenfeld, L.; Hahn, Y.; Lepage, A.; Leonard, R.; Belafsky, P.C. Transcutaneous electrical stimulation versus traditional dysphagia therapy: A nonconcurrent cohort study. Otolaryngol. Head Neck Surg. 2006, 135, 754–757. [Google Scholar] [CrossRef]
- Santos, G.D.; Nunes, P.A.; Stella, F.; Brum, P.S.; Yassuda, M.S.; Ueno, L.M.; Gattaz, W.F.; Forlenza, O.V. Multidisciplinary rehabilitation program; effects of a multimodal intervention for patients with Alzheimer’s disease and cognitive impairment without dementia. Arch. Clin. Psychiatry 2015, 42, 153–156. [Google Scholar]
| Variables | Mendelsohn Maneuver (n = 15) | NMES (n = 13) | Compound Intervention Program (n = 15) | p |
|---|---|---|---|---|
| Gender, n (%) | 0.31 | |||
| Male | 8 (53.3) | 7 (53.8) | 9 (60.0) | |
| Female | 7 (46.7) | 6 (46.2) | 6 (40.0) | |
| Age (years), m ± sd | 63.5 ± 5.7 | 65.1 ± 9.3 | 65.0 ± 7.3 | 0.75 |
| Mean monthly household income, n (%) | <0.001 | |||
| >2,000,000 KRW | 5 (33.3) | 7 (53.8) | 7 (46.7) | |
| 2,000,000–3,000,000 KRW | 6 (40.0) | 6 (46.2) | 5 (33.3) | |
| <3,000,000 KRW | 4 (26.7) | 0 | 3 (20.0) | |
| Longest occupation | <0.001 | |||
| Manual workers | 6 (40.0) | 4 (30.8) | 7 (46.7) | |
| Non-manual workers | 1 (6.7) | 3 (23.1) | 2 (13.3) | |
| Economically inactive population | 8 (53.3) | 6 (46.1) | 6 (40.0) | |
| Highest level of education | 0.56 | |||
| Graduation below junior high school | 12 (80.0) | 11 (84.6) | 12 (80.0) | |
| High school graduation or above | 3 (20.0) | 2 (15.4) | 3 (20.0) | |
| Time since dysphagia (month) | 5.1 ± 1.8 | 5.5 ± 1.5 | 4.9 ± 1.5 | 0.81 |
| FDS * | 34.1 ± 21.5 | 36.7 ± 17.9 | 31.9 ± 19.8 | 0.75 |
| FDS | Mendelsohn Maneuver (n = 15) | NMES (n = 13) | Compound Intervention Program (n = 15) | p |
|---|---|---|---|---|
| Total Score | 34.1 ± 21.5 | 37.8 ± 17.9 | 51.9 ± 19.8 | <0.001 |
| LC | 1.3 ± 2.3 | 0.6 ± 1.2 | 1.3 ± 2.0 | <0.001 |
| BF | 1.7 ± 2.5 | 1.0 ± 1.5 | 1.3 ± 2.1 | 0.532 |
| ROC | 1.3 ± 1.7 | 1.5 ± 1.5 | 1.7 ± 1.6 | 0.085 |
| OTT | 1.7 ± 2.2 | 1.4 ± 2.3 | 2.1 ± 2.5 | 0.323 |
| TPS | 5.1 ± 5.0 | 6.5 ± 4.7 | 7.7 ± 4.3 | 0.256 |
| LEEC | 6.0 ± 6.1 | 6.2 ± 6.0 | 7.6 ± 4.6 | 0.018 |
| NP | 1.2 ± 3.4 | 0.8 ± 2.7 | 0.9 ± 3.0 | 0.563 |
| RV | 5.8 ± 4.6 | 5.8 ± 3.1 | 8.2 ± 3.2 | 0.001 |
| RPS | 4.6 ± 4.2 | 4.7 ± 3.5 | 7.6 ± 3.5 | 0.017 |
| CPWSF | 4.5 ± 4.7 | 6.7 ± 4.5 | 8.3 ± 3.6 | 0.001 |
| PTT | 1.1 ± 1.7 | 1.5 ± 1.9 | 1.4 ± 1.7 | 0.256 |
| SWAL–QOL | Mendelsohn Maneuver (n = 15) | NMES (n = 13) | Compound Intervention Program (n = 15) | p |
|---|---|---|---|---|
| Total score | 120.8 ± 20.5 | 111.2 ± 22.1 | 133.8 ± 18.7 | <0.001 |
| Burden | 5.3 ± 1.3 | 6.5 ± 1.5 | 8.8 ± 1.2 | <0.001 |
| Fear | 10.9 ± 2.2 | 8.0 ± 2.0 | 9.5 ± 2.2 | 0.085 |
| Eating duration | 6.3 ± 1.5 | 7.0 ± 2.1 | 9.1 ± 1.3 | 0.015 |
| Eating desire | 10.7 ± 2.2 | 9.3 ± 2.1 | 11.2 ± 2.0 | 0.530 |
| Symptoms and frequency | 30.1 ± 7.7 | 25.1 ± 8.3 | 33.5 ± 7.2 | <0.001 |
| Food selection | 7.8 ± 1.4 | 7.3 ± 1.7 | 8.3 ± 1.5 | 0.751 |
| Communication | 7.7 ± 1.5 | 8.1 ± 1.8 | 7.0 ± 1.8 | 0.275 |
| Social | 11.9 ± 4.1 | 12.1 ± 4.5 | 12.3 ± 4.1 | 0.380 |
| Fatigue | 9.2 ± 2.6 | 8.7 ± 2.1 | 9.7 ± 2.0 | 0.581 |
| Sleep | 6.0 ± 1.8 | 6.5 ± 1.7 | 6.8 ± 2.0 | 0.070 |
| Mental health | 15.5 ± 2.3 | 11.9 ± 3.3 | 18.5 ± 2.3 | <0.001 |
| FDS | Mendelsohn Maneuver (n = 15) | NMES (n = 13) | Compound Intervention Program (n = 15) | p | Scheffe Test | |||
|---|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | Pre | Post | |||
| Total Score | 34.1 ± 21.5 | 24.7 ± 20.2 | 37.8 ± 17.9 | 32.6 ± 16.2 | 51.9 ± 19.8 | 37.5 ± 17.7 | 0.001 | b < a < c |
| LC | 1.3 ± 2.3 | 0.9 ± 1.8 | 0.6 ± 1.2 | 0.4 ± 1.1 | 1.3 ± 2.0 | 0.8 ± 1.8 | 0.371 | |
| BF | 1.7 ± 2.5 | 0.9 ± 1.8 | 1.0 ± 1.5 | 0.7 ± 1.3 | 1.3 ± 2.1 | 0.8 ± 2.0 | 0.570 | |
| ROC | 1.3 ± 1.7 | 1.2 ± 1.6 | 1.5 ± 1.5 | 1.2 ± 1.6 | 1.7 ± 1.6 | 1.3 ± 1.5 | 0.551 | |
| OTT | 1.7 ± 2.2 | 0.8 ± 2.0 | 1.4 ± 2.3 | 1.0 ± 2.1 | 2.1 ± 2.5 | 1.6 ± 2.3 | 0.487 | |
| TPS | 5.1 ± 5.0 | 4.5 ± 4.3 | 6.5 ± 4.7 | 6.0 ± 3.8 | 7.7 ± 4.3 | 7.0 ± 4.1 | 0.153 | |
| LEEC | 6.0 ± 6.1 | 3.5 ± 5.5 | 6.2 ± 6.0 | 5.1 ± 5.6 | 7.6 ± 4.6 | 3.3 ± 4.4 | <0.001 | b < a < c |
| NP | 1.2 ± 3.4 | 0.4 ± 1.3 | 0.8 ± 2.7 | 0.6 ± 2.0 | 0.9 ± 3.0 | 0.6 ± 2.9 | 0.315 | |
| RV | 5.8 ± 4.6 | 5.2 ± 4.1 | 5.8 ± 3.1 | 5.0 ± 3.3 | 8.2 ± 3.2 | 7.7 ± 3.1 | 0.870 | |
| RPS | 4.6 ± 4.2 | 4.3 ± 3.5 | 4.7 ± 3.5 | 3.7 ± 3.7 | 7.6 ± 3.5 | 7.0 ± 3.3 | 0.461 | |
| CPWSF | 4.5 ± 4.7 | 2.8 ± 4.3 | 6.7 ± 4.5 | 4.3 ± 4.2 | 8.3 ± 3.6 | 4.1 ± 3.3 | <0.001 | a = b < c |
| PTT | 1.1 ± 1.7 | 0.7 ± 1.6 | 1.5 ± 1.9 | 0.8 ± 1.8 | 1.4 ± 1.7 | 0.5 ± 1.7 | 0.385 | |
| SWAL–QOL | Test | Mendelsohn Maneuver (n = 15) | NMES (n = 13) | Compound Intervention Program (n = 15) | p | Scheffe Test |
|---|---|---|---|---|---|---|
| Total score | Pre | 120.8 ± 20.5 | 111.2 ± 22.1 | 133.8 ± 18.7 | 0.001 | b < a < c |
| Post | 134.8 ± 21.7 | 120.5 ± 23.0 | 152.3 ± 20.1 | |||
| Burden | Pre | 5.3 ± 1.3 | 6.5 ± 1.5 | 8.8 ± 1.2 | 0.795 | |
| Post | 5.9 ± 1.4 | 6.7 ± 1.5 | 9.3 ± 1.2 | |||
| Fear | Pre | 10.9 ± 2.2 | 8.0 ± 2.0 | 9.5 ± 2.2 | 0.271 | |
| Post | 11.6 ± 2.1 | 8.5 ± 2.0 | 10.4 ± 2.1 | |||
| Eating duration | Pre | 6.3 ± 1.5 | 7.0 ± 2.1 | 9.1 ± 1.3 | 0.381 | |
| Post | 7.7 ± 1.6 | 8.3 ± 2.0 | 10.0 ± 1.4 | |||
| Eating desire | Pre | 10.7 ± 2.2 | 9.3 ± 2.1 | 11.2 ± 2.0 | 0.450 | |
| Post | 11.3 ± 2.3 | 10.2 ± 2.0 | 11.8 ± 2.0 | |||
| Symptoms and frequency | Pre | 30.1 ± 7.7 | 25.1 ± 8.3 | 33.5 ± 7.2 | <0.001 | b = a < c |
| Post | 34.3 ± 7.4 | 27.5 ± 8.1 | 41.8 ± 6.9 | |||
| Food selection | Pre | 7.8 ± 1.4 | 7.3 ± 1.7 | 8.3 ± 1.5 | 0.275 | |
| Post | 8.5 ± 1.5 | 8.0 ± 1.8 | 8.9 ± 1.5 | |||
| Communication | Pre | 7.7 ± 1.5 | 8.1 ± 1.8 | 7.0 ± 1.8 | 0.015 | b < a < c |
| Post | 8.9 ± 1.3 | 8.8 ± 1.8 | 9.1 ± 1.6 | |||
| Social | Pre | 11.9 ± 4.1 | 12.1 ± 4.5 | 12.3 ± 4.1 | 0.883 | |
| Post | 12.5 ± 4.0 | 12.8 ± 4.5 | 12.9 ± 4.0 | |||
| Fatigue | Pre | 9.2 ± 2.6 | 8.7 ± 2.1 | 9.7 ± 2.0 | 0.570 | |
| Post | 10.5 ± 2.3 | 9.9 ± 1.9 | 10.8 ± 1.9 | |||
| Sleep | Pre | 6.0 ± 1.8 | 6.5 ± 1.7 | 6.8 ± 2.0 | 0.001 | b < a < c |
| Post | 6.7 ± 1.8 | 7.5 ± 1.8 | 8.5 ± 1.8 | |||
| Mental health | Pre | 15.5 ± 2.3 | 11.9 ± 3.3 | 18.5 ± 2.3 | 0.550 | |
| Post | 16.3 ± 2.2 | 12.8 ± 3.1 | 19.5 ± 2.2 |
© 2020 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Byeon, H. Combined Effects of NMES and Mendelsohn Maneuver on the Swallowing Function and Swallowing–Quality of Life of Patients with Stroke-Induced Sub-Acute Swallowing Disorders. Biomedicines 2020, 8, 12. https://doi.org/10.3390/biomedicines8010012
Byeon H. Combined Effects of NMES and Mendelsohn Maneuver on the Swallowing Function and Swallowing–Quality of Life of Patients with Stroke-Induced Sub-Acute Swallowing Disorders. Biomedicines. 2020; 8(1):12. https://doi.org/10.3390/biomedicines8010012
Chicago/Turabian StyleByeon, Haewon. 2020. "Combined Effects of NMES and Mendelsohn Maneuver on the Swallowing Function and Swallowing–Quality of Life of Patients with Stroke-Induced Sub-Acute Swallowing Disorders" Biomedicines 8, no. 1: 12. https://doi.org/10.3390/biomedicines8010012
APA StyleByeon, H. (2020). Combined Effects of NMES and Mendelsohn Maneuver on the Swallowing Function and Swallowing–Quality of Life of Patients with Stroke-Induced Sub-Acute Swallowing Disorders. Biomedicines, 8(1), 12. https://doi.org/10.3390/biomedicines8010012





