Oral Capsaicinoid Administration Alters the Plasma Endocannabinoidome and Fecal Microbiota of Reproductive-Aged Women Living with Overweight and Obesity
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethical Approval
2.2. Subjects and Treatment Protocol
2.3. Assessment of Anthropometric Parameters
2.4. Measurement of Appetite Sensations and Eating Behaviors
2.5. Measurement of Eating Behavior
2.6. Lipid Extraction and HPLC–MS/MS for the Analysis of eCBome Mediators
2.7. DNA Extraction and 16S rRNA Gene Sequencing
2.8. Statistical Analyses
3. Results
3.1. Trial Completion and Side Effects
3.2. Effect of CAE and Caloric Restriction on Body Weight, BMI, Waist Circumference and Fat Mass
3.3. Effect of CAE and Caloric Restriction on Measures of Appetite Sensation and Eating Behavior
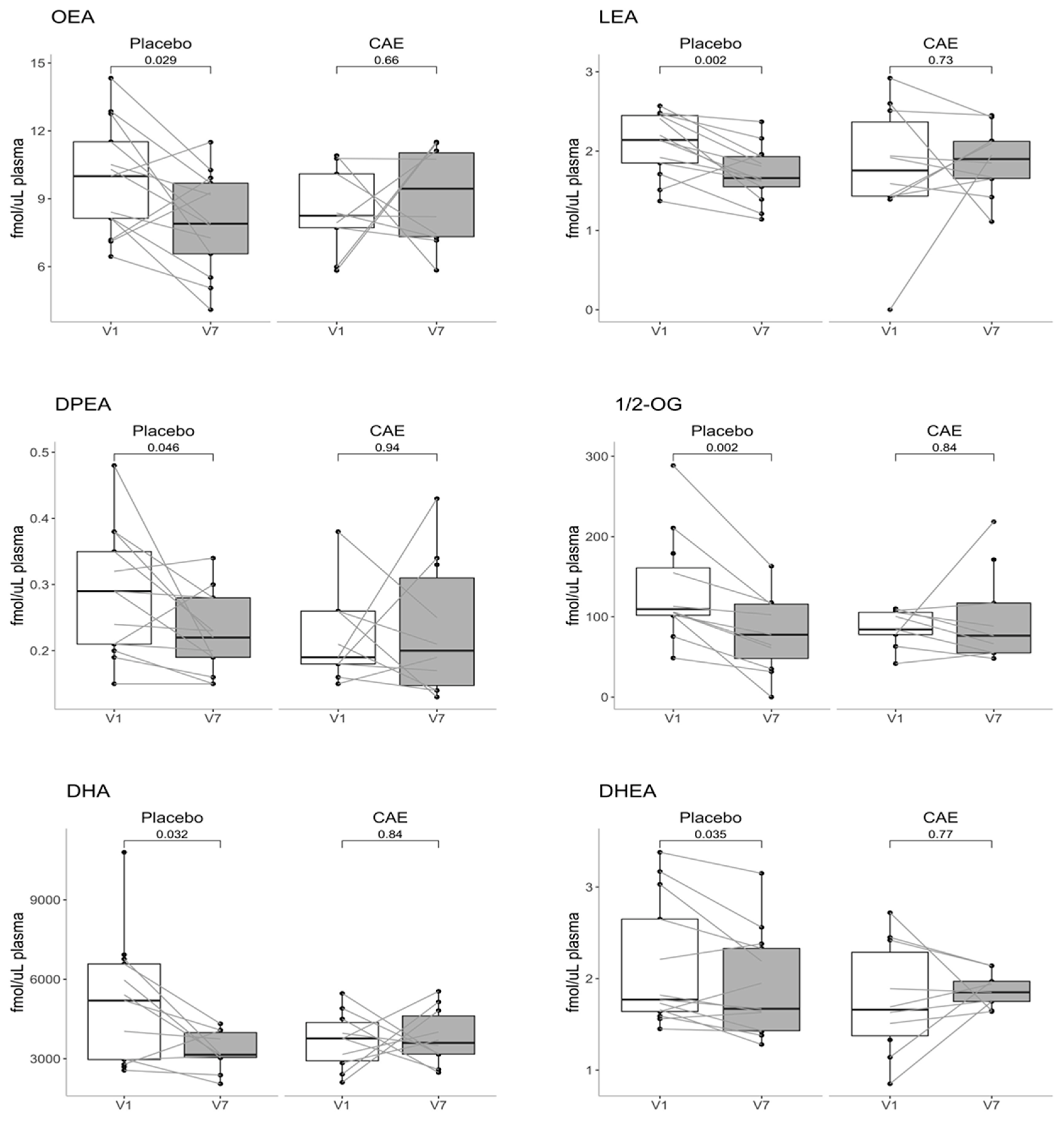
3.4. Effect of CAE and Caloric Restriction on Plasma ECBome Mediator Levels
3.5. Effect of CAE and Caloric Restriction on Fecal Microbiota Composition
3.6. Correlations between Plasma ECBome Mediator Levels, Anthropometric Measures and Fecal Microbiota Composition
3.7. Correlations between Plasma ECBome Mediator Levels and Appetite Sensations and Eating Behaviors
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Non Communicable Diseases. Available online: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed on 26 January 2021).
- Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 26 January 2021).
- Zheng, J.; Zheng, S.; Feng, Q.; Zhang, Q.; Xiao, X. Dietary Capsaicin and Its Anti-Obesity Potency: From Mechanism to Clinical Implications. Biosci. Rep. 2017, 37. [Google Scholar] [CrossRef]
- Hill, J.O.; Wyatt, H.R.; Peters, J.C. Energy Balance and Obesity. Circulation 2012, 126, 126–132. [Google Scholar] [CrossRef]
- Hruby, A.; Hu, F.B. The Epidemiology of Obesity: A Big Picture. Pharmacoeconomics 2015, 33, 673–689. [Google Scholar] [CrossRef]
- Yanovski, S.Z.; Yanovski, J.A. Long-Term Drug Treatment for Obesity: A Systematic and Clinical Review. JAMA 2014, 311, 74. [Google Scholar] [CrossRef]
- Filippatos, T.D.; Derdemezis, C.S.; Gazi, I.F.; Nakou, E.S.; Mikhailidis, D.P.; Elisaf, M.S. Orlistat-Associated Adverse Effects and Drug Interactions: A Critical Review. Drug Saf. 2008, 31, 53–65. [Google Scholar] [CrossRef] [PubMed]
- Wilding, J.P.H.; Batterham, R.L.; Calanna, S.; Davies, M.; van Gaal, L.F.; Lingvay, I.; McGowan, B.M.; Rosenstock, J.; Tran, M.T.D.; Wadden, T.A.; et al. Once-Weekly Semaglutide in Adults with Overweight or Obesity. N. Engl. J. Med. 2021. [Google Scholar] [CrossRef] [PubMed]
- Dietrich, M.O.; Horvath, T.L. Limitations in Anti-Obesity Drug Development: The Critical Role of Hunger-Promoting Neurons. Nat. Rev. Drug Discov. 2012, 11, 675–691. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Lee, J.; Salazar Hernandez, M.A.; Mazitschek, R.; Ozcan, U. Treatment of Obesity with Celastrol. Cell 2015, 161, 999–1011. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martel, J.; Ojcius, D.M.; Chang, C.-J.; Lin, C.-S.; Lu, C.-C.; Ko, Y.-F.; Tseng, S.-F.; Lai, H.-C.; Young, J.D. Anti-Obesogenic and Antidiabetic Effects of Plants and Mushrooms. Nat. Rev. Endocrinol. 2017, 13, 149–160. [Google Scholar] [CrossRef]
- Varghese, S.; Kubatka, P.; Rodrigo, L.; Gazdikova, K.; Caprnda, M.; Fedotova, J.; Zulli, A.; Kruzliak, P.; Büsselberg, D. Chili Pepper as a Body Weight-Loss Food. Int. J. Food Sci. Nutr. 2017, 68, 392–401. [Google Scholar] [CrossRef]
- Richards, B.L.; Whittle, S.L.; Buchbinder, R. Neuromodulators for Pain Management in Rheumatoid Arthritis. Cochrane Database Syst. Rev. 2012, 1. [Google Scholar] [CrossRef]
- Zheng, L.; Chen, J.; Ma, Z.; Liu, W.; Yang, F.; Yang, Z.; Wang, K.; Wang, X.; He, D.; Li, L.; et al. Capsaicin Enhances Anti-Proliferation Efficacy of Pirarubicin via Activating TRPV1 and Inhibiting PCNA Nuclear Translocation in 5637 Cells. Mol. Med. Rep. 2016, 13, 881–887. [Google Scholar] [CrossRef] [Green Version]
- Liu, Y.-P.; Dong, F.-X.; Chai, X.; Zhu, S.; Zhang, B.-L.; Gao, D.-S. Role of Autophagy in Capsaicin-Induced Apoptosis in U251 Glioma Cells. Cell. Mol. Neurobiol. 2016, 36, 737–743. [Google Scholar] [CrossRef]
- Dairam, A.; Fogel, R.; Daya, S.; Limson, J.L. Antioxidant and Iron-Binding Properties of Curcumin, Capsaicin, and S -Allylcysteine Reduce Oxidative Stress in Rat Brain Homogenate. J. Agric. Food Chem. 2008, 56, 3350–3356. [Google Scholar] [CrossRef]
- Singh, U.; Bernstein, J.A. Intranasal Capsaicin in Management of Nonallergic (Vasomotor) Rhinitis. Prog Drug Res. 2014, 68, 147–170. [Google Scholar] [CrossRef] [PubMed]
- Tremblay, A.; Arguin, H.; Panahi, S. Capsaicinoids: A Spicy Solution to the Management of Obesity? Int J. Obes 2016, 40, 1198–1204. [Google Scholar] [CrossRef] [PubMed]
- Yoshioka, M.; St-Pierre, S.; Drapeau, V.; Dionne, I.; Doucet, E.; Suzuki, M.; Tremblay, A. Effects of Red Pepper on Appetite and Energy Intake. Br. J. Nutr. 1999, 82, 115–123. [Google Scholar] [CrossRef] [PubMed]
- Westerterp-Plantenga, M.S.; Smeets, A.; Lejeune, M.P.G. Sensory and Gastrointestinal Satiety Effects of Capsaicin on Food Intake. Int. J. Obes. 2005, 29, 682–688. [Google Scholar] [CrossRef] [Green Version]
- Yoshioka, M.; Doucet, E.; Drapeau, V.; Dionne, I.; Tremblay, A. Combined Effects of Red Pepper and Caffeine Consumption on 24 h Energy Balance in Subjects given Free Access to Foods. Br. J. Nutr. 2001, 85, 203–211. [Google Scholar] [CrossRef] [Green Version]
- Wahlqvist, M.L.; Wattanapenpaiboon, N. Hot Foods—Unexpected Help with Energy Balance? Lancet 2001, 358, 348–349. [Google Scholar] [CrossRef]
- Lejeune, M.P.G.M.; Kovacs, E.M.R.; Westerterp-Plantenga, M.S. Effect of Capsaicin on Substrate Oxidation and Weight Maintenance after Modest Body-Weight Loss in Human Subjects. Br. J. Nutr. 2003, 90, 651–659. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kelava, L.; Nemeth, D.; Hegyi, P.; Keringer, P.; Kovacs, D.K.; Balasko, M.; Solymar, M.; Pakai, E.; Rumbus, Z.; Garami, A. Dietary Supplementation of Transient Receptor Potential Vanilloid-1 Channel Agonists Reduces Serum Total Cholesterol Level: A Meta-Analysis of Controlled Human Trials. Crit. Rev. Food Sci. Nutr. 2021, 1–11. [Google Scholar] [CrossRef]
- Chen, J.; Li, L.; Li, Y.; Liang, X.; Sun, Q.; Yu, H.; Zhong, J.; Ni, Y.; Chen, J.; Zhao, Z.; et al. Activation of TRPV1 Channel by Dietary Capsaicin Improves Visceral Fat Remodeling through Connexin43-Mediated Ca2+ Influx. Cardiovasc. Diabetol. 2015, 14, 22. [Google Scholar] [CrossRef] [Green Version]
- Sun, F.; Xiong, S.; Zhu, Z. Dietary Capsaicin Protects Cardiometabolic Organs from Dysfunction. Nutrients 2016, 8, 174. [Google Scholar] [CrossRef]
- Gram, D.X.; Ahrén, B.; Nagy, I.; Olsen, U.B.; Brand, C.L.; Sundler, F.; Tabanera, R.; Svendsen, O.; Carr, R.D.; Santha, P.; et al. Capsaicin-Sensitive Sensory Fibers in the Islets of Langerhans Contribute to Defective Insulin Secretion in Zucker Diabetic Rat, an Animal Model for Some Aspects of Human Type 2 Diabetes: Systemic Capsaicin in ZDF Rats. Eur. J. Neurosci. 2007, 25, 213–223. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Yan, Z.; Zhong, J.; Chen, J.; Ni, Y.; Li, L.; Ma, L.; Zhao, Z.; Liu, D.; Zhu, Z. Transient Receptor Potential Vanilloid 1 Activation Enhances Gut Glucagon-Like Peptide-1 Secretion and Improves Glucose Homeostasis. Diabetes 2012, 61, 2155–2165. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kang, J.-H.; Kim, C.-S.; Han, I.-S.; Kawada, T.; Yu, R. Capsaicin, a Spicy Component of Hot Peppers, Modulates Adipokine Gene Expression and Protein Release from Obese-Mouse Adipose Tissues and Isolated Adipocytes, and Suppresses the Inflammatory Responses of Adipose Tissue Macrophages. FEBS Lett. 2007, 581, 4389–4396. [Google Scholar] [CrossRef] [Green Version]
- Di Marzo, V.; Lastres-Becker, I.; Bisogno, T.; De Petrocellis, L.; Milone, A.; Davis, J.B.; Fernandez-Ruiz, J.J. Hypolocomotor Effects in Rats of Capsaicin and Two Long Chain Capsaicin Homologues. Eur. J. Pharmacol. 2001, 420, 123–131. [Google Scholar] [CrossRef]
- Acharya, N.; Penukonda, S.; Shcheglova, T.; Hagymasi, A.T.; Basu, S.; Srivastava, P.K. Endocannabinoid System Acts as a Regulator of Immune Homeostasis in the Gut. Proc. Natl. Acad. Sci. USA 2017, 114, 5005–5010. [Google Scholar] [CrossRef] [Green Version]
- Silvestri, C.; di Marzo, V. The Endocannabinoid System in Energy Homeostasis and the Etiopathology of Metabolic Disorders. Cell Metab. 2013, 17, 475–490. [Google Scholar] [CrossRef] [Green Version]
- Di Marzo, V.; Wang, J. (Eds.) The Endocannabinoidome the World of Endocannabinoids and Related Mediators; Academic Press: London, UK, 2014. [Google Scholar]
- Zygmunt, P.M.; Ermund, A.; Movahed, P.; Andersson, D.A.; Simonsen, C.; Jönsson, B.A.G.; Blomgren, A.; Birnir, B.; Bevan, S.; Eschalier, A.; et al. Monoacylglycerols Activate TRPV1—A Link between Phospholipase C and TRPV. PLoS ONE 2013, 8, e81618. [Google Scholar] [CrossRef] [Green Version]
- Movahed, P.; Jönsson, B.A.G.; Birnir, B.; Wingstrand, J.A.; Jørgensen, T.D.; Ermund, A.; Sterner, O.; Zygmunt, P.M.; Högestätt, E.D. Endogenous Unsaturated C18 N-Acylethanolamines Are Vanilloid Receptor (TRPV1) Agonists. J. Biol. Chem. 2005, 280, 38496–38504. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cani, P.D.; Plovier, H.; Van Hul, M.; Geurts, L.; Delzenne, N.M.; Druart, C.; Everard, A. Endocannabinoids—At the Crossroads between the Gut Microbiota and Host Metabolism. Nat. Rev. Endocrinol. 2016, 12, 133–143. [Google Scholar] [CrossRef] [PubMed]
- Di Marzo, V.; Silvestri, C. Lifestyle and Metabolic Syndrome: Contribution of the Endocannabinoidome. Nutrients 2019, 11, 1956. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dione, N.; Lacroix, S.; Taschler, U.; Deschênes, T.; Abolghasemi, A.; Leblanc, N.; Di Marzo, V.; Silvestri, C. Mgll Knockout Mouse Resistance to Diet-Induced Dysmetabolism Is Associated with Altered Gut Microbiota. Cells 2020, 9, 2705. [Google Scholar] [CrossRef] [PubMed]
- Kang, C.; Wang, B.; Kaliannan, K.; Wang, X.; Lang, H.; Hui, S.; Huang, L.; Zhang, Y.; Zhou, M.; Chen, M.; et al. Gut Microbiota Mediates the Protective Effects of Dietary Capsaicin against Chronic Low-Grade Inflammation and Associated Obesity Induced by High-Fat Diet. mBio 2017, 8, e00470-17. [Google Scholar] [CrossRef] [Green Version]
- Song, J.-X.; Ren, H.; Gao, Y.-F.; Lee, C.-Y.; Li, S.-F.; Zhang, F.; Li, L.; Chen, H. Dietary Capsaicin Improves Glucose Homeostasis and Alters the Gut Microbiota in Obese Diabetic Ob/Ob Mice. Front. Physiol. 2017, 8, 602. [Google Scholar] [CrossRef] [Green Version]
- Kumar, V.; Mahajan, N.; Khare, P.; Kondepudi, K.K.; Bishnoi, M. Role of TRPV1 in Colonic Mucin Production and Gut Microbiota Profile. Eur. J. Pharmacol. 2020, 888, 173567. [Google Scholar] [CrossRef]
- Drapeau, V.; King, N.; Hetherington, M.; Doucet, E.; Blundell, J.; Tremblay, A. Appetite Sensations and Satiety Quotient: Predictors of Energy Intake and Weight Loss. Appetite 2007, 48, 159–166. [Google Scholar] [CrossRef] [Green Version]
- Arvaniti, K.; Richard, D.; Tremblay, A. Reproducibility of Energy and Macronutrient Intake and Related Substrate Oxidation Rates in a Buffet-Type Meal. Br. J. Nutr 2000, 83, 489–495. [Google Scholar] [CrossRef] [Green Version]
- Green, S.M.; Delargy, H.J.; Joanes, D.; Blundell, J.E. A Satiety Quotient: A Formulation to Assess the Satiating Effect of Food. Appetite 1997, 29, 291–304. [Google Scholar] [CrossRef]
- Stunkard, A.J.; Messick, S. The Three-Factor Eating Questionnaire to Measure Dietary Restraint, Disinhibition and Hunger. J. Psychosom. Res. 1985, 29, 71–83. [Google Scholar] [CrossRef]
- Cepeda-Benito, A.; Gleaves, D.H.; Fernández, M.C.; Vila, J.; Williams, T.L.; Reynoso, J. The Development and Validation of Spanish Versions of the State and Trait Food Cravings Questionnaires. Behav. Res. Ther. 2000, 38, 1125–1138. [Google Scholar] [CrossRef]
- Turcotte, C.; Archambault, A.; Dumais, É.; Martin, C.; Blanchet, M.; Bissonnette, E.; Ohashi, N.; Yamamoto, K.; Itoh, T.; Laviolette, M.; et al. Endocannabinoid Hydrolysis Inhibition Unmasks That Unsaturated Fatty Acids Induce a Robust Biosynthesis of 2-arachidonoyl-glycerol and Its Congeners in Human Myeloid Leukocytes. FASEB J. 2020, 34, 4253–4265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Callahan, B.J.; McMurdie, P.J.; Rosen, M.J.; Han, A.W.; Johnson, A.J.A.; Holmes, S.P. DADA2: High-Resolution Sample Inference from Illumina Amplicon Data. Nat. Methods 2016, 13, 581–583. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paulson, J.N.; Stine, O.C.; Bravo, H.C.; Pop, M. Differential Abundance Analysis for Microbial Marker-Gene Surveys. Nat. Methods 2013, 10, 1200–1202. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bakdash, J.Z.; Marusich, L.R. Repeated Measures Correlation. Front. Psychol. 2017, 8, 456. [Google Scholar] [CrossRef] [Green Version]
- Rochefort, G.; Provencher, V.; Castonguay-Paradis, S.; Perron, J.; Lacroix, S.; Martin, C.; Flamand, N.; Di Marzo, V.; Veilleux, A. Intuitive Eating Is Associated with Elevated Levels of Circulating Omega-3-Polyunsaturated Fatty Acid-Derived Endocannabinoidome Mediators. Appetite 2021, 156, 104973. [Google Scholar] [CrossRef] [PubMed]
- Urbina, S.L.; Roberts, M.D.; Kephart, W.C.; Villa, K.B.; Santos, E.N.; Olivencia, A.M.; Bennett, H.M.; Lara, M.D.; Foster, C.A.; Purpura, M.; et al. Effects of Twelve Weeks of Capsaicinoid Supplementation on Body Composition, Appetite and Self-Reported Caloric Intake in Overweight Individuals. Appetite 2017, 113, 264–273. [Google Scholar] [CrossRef] [PubMed]
- Rogers, J.; Urbina, S.L.; Taylor, L.W.; Wilborn, C.D.; Purpura, M.; Jäger, R.; Juturu, V. Capsaicinoids Supplementation Decreases Percent Body Fat and Fat Mass: Adjustment Using Covariates in a Post Hoc Analysis. BMC Obes. 2018, 5, 22. [Google Scholar] [CrossRef]
- McCarty, M.F.; DiNicolantonio, J.J.; O’Keefe, J.H. Capsaicin May Have Important Potential for Promoting Vascular and Metabolic Health. Open Heart 2015, 2, e000262. [Google Scholar] [CrossRef] [Green Version]
- Sanati, S.; Razavi, B.M.; Hosseinzadeh, H. A Review of the Effects of Capsicum Annuum L. and Its Constituent, Capsaicin, in Metabolic Syndrome. Iran. J. Basic Med. Sci. 2018, 21, 439. [Google Scholar] [CrossRef]
- Shi, Z.; Riley, M.; Brown, A.; Page, A. Chilli Intake Is Inversely Associated with Hypertension among Adults. Clin. Nutr. ESPEN 2018, 23, 67–72. [Google Scholar] [CrossRef] [PubMed]
- Ludy, M.-J.; Moore, G.E.; Mattes, R.D. The Effects of Capsaicin and Capsiate on Energy Balance: Critical Review and Meta-Analyses of Studies in Humans. Chem. Senses 2012, 37, 103–121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kang, J.-H.; Tsuyoshi, G.; Han, I.-S.; Kawada, T.; Kim, Y.M.; Yu, R. Dietary Capsaicin Reduces Obesity-Induced Insulin Resistance and Hepatic Steatosis in Obese Mice Fed a High-Fat Diet. Obesity 2010, 18, 780–787. [Google Scholar] [CrossRef] [PubMed]
- Kwon, D.Y.; Kim, Y.S.; Ryu, S.Y.; Cha, M.-R.; Yon, G.H.; Yang, H.J.; Kim, M.J.; Kang, S.; Park, S. Capsiate Improves Glucose Metabolism by Improving Insulin Sensitivity Better than Capsaicin in Diabetic Rats. J. Nutr. Biochem. 2013, 24, 1078–1085. [Google Scholar] [CrossRef]
- Shen, W.; Shen, M.; Zhao, X.; Zhu, H.; Yang, Y.; Lu, S.; Tan, Y.; Li, G.; Li, M.; Wang, J.; et al. Anti-Obesity Effect of Capsaicin in Mice Fed with High-Fat Diet Is Associated with an Increase in Population of the Gut Bacterium Akkermansia Muciniphila. Front. Microbiol. 2017, 8, 272. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.; Jung, D.Y.; Kim, J.H.; Patel, P.R.; Hu, X.; Lee, Y.; Azuma, Y.; Wang, H.-F.; Tsitsilianos, N.; Shafiq, U.; et al. Transient Receptor Potential Vanilloid Type-1 Channel Regulates Diet-Induced Obesity, Insulin Resistance, and Leptin Resistance. FASEB J. 2015, 29, 3182–3192. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, L.L.; Yan Liu, D.; Ma, L.Q.; Luo, Z.D.; Cao, T.B.; Zhong, J.; Yan, Z.C.; Wang, L.J.; Zhao, Z.G.; Zhu, S.J.; et al. Activation of Transient Receptor Potential Vanilloid Type-1 Channel Prevents Adipogenesis and Obesity. Circ. Res. 2007, 100, 1063–1070. [Google Scholar] [CrossRef] [Green Version]
- Baboota, R.K.; Singh, D.P.; Sarma, S.M.; Kaur, J.; Sandhir, R.; Boparai, R.K.; Kondepudi, K.K.; Bishnoi, M. Capsaicin Induces “Brite” Phenotype in Differentiating 3T3-L1 Preadipocytes. PLoS ONE 2014, 9, e103093. [Google Scholar] [CrossRef] [Green Version]
- Baskaran, P.; Krishnan, V.; Ren, J.; Thyagarajan, B. Capsaicin Induces Browning of White Adipose Tissue and Counters Obesity by Activating TRPV1 Channel-Dependent Mechanisms: TRPV1 Activates Browning of WAT to Counter Obesity. Br. J. Pharmacol. 2016, 173, 2369–2389. [Google Scholar] [CrossRef]
- Montecucco, F.; Lenglet, S.; Quercioli, A.; Burger, F.; Thomas, A.; Lauer, E.; Silva, D.A.R.; Mach, F.; Vuilleumier, N.; Bobbioni-Harsch, E.; et al. Gastric Bypass in Morbid Obese Patients Is Associated with Reduction in Adipose Tissue Inflammation via N-Oleoylethanolamide (OEA)-Mediated Pathways. Thromb. Haemost. 2015, 113, 838–850. [Google Scholar] [CrossRef] [Green Version]
- Fanelli, F.; Mezzullo, M.; Repaci, A.; Belluomo, I.; Ibarra Gasparini, D.; Di Dalmazi, G.; Mastroroberto, M.; Vicennati, V.; Gambineri, A.; Morselli-Labate, A.M.; et al. Profiling Plasma N-Acylethanolamine Levels and Their Ratios as a Biomarker of Obesity and Dysmetabolism. Mol. Metab. 2018, 14, 82–94. [Google Scholar] [CrossRef]
- Azar, S.; Sherf-Dagan, S.; Nemirovski, A.; Webb, M.; Raziel, A.; Keidar, A.; Goitein, D.; Sakran, N.; Shibolet, O.; Tam, J.; et al. Circulating Endocannabinoids Are Reduced Following Bariatric Surgery and Associated with Improved Metabolic Homeostasis in Humans. Obes. Surg. 2019, 29, 268–276. [Google Scholar] [CrossRef] [PubMed]
- Castonguay-Paradis, S.; Lacroix, S.; Rochefort, G.; Parent, L.; Perron, J.; Martin, C.; Lamarche, B.; Raymond, F.; Flamand, N.; di Marzo, V.; et al. Dietary Fatty Acid Intake and Gut Microbiota Determine Circulating Endocannabinoidome Signaling beyond the Effect of Body Fat. Sci. Rep. 2020, 10, 15975. [Google Scholar] [CrossRef] [PubMed]
- Manchanda, M.; Leishman, E.; Sangani, K.; Alamri, A.; Bradshaw, H.B. Activation of TRPV1 by Capsaicin or Heat Drives Changes in 2-Acyl Glycerols and N-Acyl Ethanolamines in a Time, Dose, and Temperature Dependent Manner. Front. Cell Dev. Biol. 2021, 9, 611952. [Google Scholar] [CrossRef] [PubMed]
- Ahern, G.P. Activation of TRPV1 by the Satiety Factor Oleoylethanolamide. J. Biol. Chem. 2003, 278, 30429–30434. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lauffer, L.M.; Iakoubov, R.; Brubaker, P.L. GPR119 Is Essential for Oleoylethanolamide-Induced Glucagon-like Peptide-1 Secretion from the Intestinal Enteroendocrine L-Cell. Diabetes 2009, 58, 1058–1066. [Google Scholar] [CrossRef] [Green Version]
- Im, D.-S. GPR119 and GPR55 as Receptors for Fatty Acid Ethanolamides, Oleoylethanolamide and Palmitoylethanolamide. Int. J. Mol. Sci. 2021, 22, 1034. [Google Scholar] [CrossRef] [PubMed]
- Syed, S.K.; Bui, H.H.; Beavers, L.S.; Farb, T.B.; Ficorilli, J.; Chesterfield, A.K.; Kuo, M.-S.; Bokvist, K.; Barrett, D.G.; Efanov, A.M. Regulation of GPR119 Receptor Activity with Endocannabinoid-like Lipids. Am. J. Physiol. Endocrinol. Metab. 2012, 303, E1469–E1478. [Google Scholar] [CrossRef]
- Di Marzo, V. New Approaches and Challenges to Targeting the Endocannabinoid System. Nat. Rev. Drug Discov 2018, 17, 623–639. [Google Scholar] [CrossRef] [PubMed]
- Figueroa, J.D.; Cordero, K.; Serrano-Illan, M.; Almeyda, A.; Baldeosingh, K.; Almaguel, F.G.; De Leon, M. Metabolomics Uncovers Dietary Omega-3 Fatty Acid-Derived Metabolites Implicated in Anti-Nociceptive Responses after Experimental Spinal Cord Injury. Neuroscience 2013, 255, 1–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wojdasiewicz, P.; Poniatowski, Ł.A.; Turczyn, P.; Frasuńska, J.; Paradowska-Gorycka, A.; Tarnacka, B. Significance of Omega-3 Fatty Acids in the Prophylaxis and Treatment after Spinal Cord Injury in Rodent Models. Mediat. Inflamm. 2020, 2020, 3164260. [Google Scholar] [CrossRef] [PubMed]
- Izzo, A.A.; Piscitelli, F.; Capasso, R.; Marini, P.; Cristino, L.; Petrosino, S.; di Marzo, V. Basal and Fasting/Refeeding-Regulated Tissue Levels of Endogenous PPAR-α Ligands in Zucker Rats. Obesity 2010, 18, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Baboota, R.K.; Murtaza, N.; Jagtap, S.; Singh, D.P.; Karmase, A.; Kaur, J.; Bhutani, K.K.; Boparai, R.K.; Premkumar, L.S.; Kondepudi, K.K.; et al. Capsaicin-Induced Transcriptional Changes in Hypothalamus and Alterations in Gut Microbial Count in High Fat Diet Fed Mice. J. Nutr. Biochem. 2014, 25, 893–902. [Google Scholar] [CrossRef] [PubMed]
- Peterson, C.T.; Rodionov, D.A.; Iablokov, S.N.; Pung, M.A.; Chopra, D.; Mills, P.J.; Peterson, S.N. Prebiotic Potential of Culinary Spices Used to Support Digestion and Bioabsorption. Evid. Based Complement. Altern. Med. 2019, 2019, 8973704. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leyva-Diaz, A.A.; Hernandez-Patlan, D.; Solis-Cruz, B.; Adhikari, B.; Kwon, Y.M.; Latorre, J.D.; Hernandez-Velasco, X.; Fuente-Martinez, B.; Hargis, B.M.; Lopez-Arellano, R.; et al. Evaluation of Curcumin and Copper Acetate against Salmonella Typhimurium Infection, Intestinal Permeability, and Cecal Microbiota Composition in Broiler Chickens. J. Anim. Sci. Biotechnol. 2021, 12, 1–12. [Google Scholar] [CrossRef]
- Kasai, C.; Sugimoto, K.; Moritani, I.; Tanaka, J.; Oya, Y.; Inoue, H.; Tameda, M.; Shiraki, K.; Ito, M.; Takei, Y.; et al. Comparison of the Gut Microbiota Composition between Obese and Non-Obese Individuals in a Japanese Population, as Analyzed by Terminal Restriction Fragment Length Polymorphism and next-Generation Sequencing. BMC Gastroenterol. 2015, 15, 100. [Google Scholar] [CrossRef] [Green Version]
- Mikami, A.; Ogita, T.; Namai, F.; Shigemori, S.; Sato, T.; Shimosato, T. Oral Administration of Flavonifractor Plautii Attenuates Inflammatory Responses in Obese Adipose Tissue. Mol. Biol. Rep. 2020, 47, 6717–6725. [Google Scholar] [CrossRef]
- Kang, C.; Zhang, Y.; Zhu, X.; Liu, K.; Wang, X.; Chen, M.; Wang, J.; Chen, H.; Hui, S.; Huang, L.; et al. Healthy Subjects Differentially Respond to Dietary Capsaicin Correlating with Specific Gut Enterotypes. J. Clin. Endocrinol. Metab. 2016, 101, 4681–4689. [Google Scholar] [CrossRef] [Green Version]
- Perez-Burgos, A.; Wang, L.; McVey Neufeld, K.-A.; Mao, Y.-K.; Ahmadzai, M.; Janssen, L.J.; Stanisz, A.M.; Bienenstock, J.; Kunze, W.A. The TRPV1 Channel in Rodents Is a Major Target for Antinociceptive Effect of the Probiotic Lactobacillus Reuteri DSM 17938: Visceral Analgesic Effect of a Lactobacillus Depends on TRPV. J. Physiol. 2015, 593, 3943–3957. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Iannotti, F.A.; Di Marzo, V. The Gut Microbiome, Endocannabinoids and Metabolic Disorders. J. Endocrinol. 2021, 248, R83–R97. [Google Scholar] [CrossRef]
- Depommier, C.; Everard, A.; Druart, C.; Plovier, H.; Van Hul, M.; Vieira-Silva, S.; Falony, G.; Raes, J.; Maiter, D.; Delzenne, N.M.; et al. Supplementation with Akkermansia Muciniphila in Overweight and Obese Human Volunteers: A Proof-of-Concept Exploratory Study. Nat. Med. 2019, 25, 1096–1103. [Google Scholar] [CrossRef]
- Hoareau, L.; Buyse, M.; Festy, F.; Ravanan, P.; Gonthier, M.-P.; Matias, I.; Petrosino, S.; Tallet, F.; D’Hellencourt, C.L.; Cesari, M.; et al. Anti-Inflammatory Effect of Palmitoylethanolamide on Human Adipocytes. Obesity 2009, 17, 431–438. [Google Scholar] [CrossRef]
- Annunziata, C.; Lama, A.; Pirozzi, C.; Cavaliere, G.; Trinchese, G.; Di Guida, F.; Nitrato Izzo, A.; Cimmino, F.; Paciello, O.; De Biase, D.; et al. Palmitoylethanolamide Counteracts Hepatic Metabolic Inflexibility Modulating Mitochondrial Function and Efficiency in Diet-induced Obese Mice. FASEB J. 2020, 34, 350–364. [Google Scholar] [CrossRef] [Green Version]
- Peters, B.A.; Shapiro, J.A.; Church, T.R.; Miller, G.; Trinh-Shevrin, C.; Yuen, E.; Friedlander, C.; Hayes, R.B.; Ahn, J. A Taxonomic Signature of Obesity in a Large Study of American Adults. Sci. Rep. 2018, 8, 9749. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, T.-R.; Lin, C.-S.; Chang, C.-J.; Lin, T.-L.; Martel, J.; Ko, Y.-F.; Ojcius, D.M.; Lu, C.-C.; Young, J.D.; Lai, H.-C. Gut Commensal Parabacteroides Goldsteinii Plays a Predominant Role in the Anti-Obesity Effects of Polysaccharides Isolated from Hirsutella Sinensis. Gut 2019, 68, 248–262. [Google Scholar] [CrossRef]
- Wang, K.; Liao, M.; Zhou, N.; Bao, L.; Ma, K.; Zheng, Z.; Wang, Y.; Liu, C.; Wang, W.; Wang, J.; et al. Parabacteroides Distasonis Alleviates Obesity and Metabolic Dysfunctions via Production of Succinate and Secondary Bile Acids. Cell Rep. 2019, 26, 222–235.e5. [Google Scholar] [CrossRef] [Green Version]
- Naderpoor, N.; Mousa, A.; Gomez-Arango, L.; Barrett, H.; Dekker Nitert, M.; de Courten, B. Faecal Microbiota Are Related to Insulin Sensitivity and Secretion in Overweight or Obese Adults. JCM 2019, 8, 452. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Muñiz Pedrogo, D.A.; Jensen, M.D.; Van Dyke, C.T.; Murray, J.A.; Woods, J.A.; Chen, J.; Kashyap, P.C.; Nehra, V. Gut Microbial Carbohydrate Metabolism Hinders Weight Loss in Overweight Adults Undergoing Lifestyle Intervention With a Volumetric Diet. Mayo Clin. Proc. 2018, 93, 1104–1110. [Google Scholar] [CrossRef]



| OmniActive Health Technologies CAE Capsules | Placebo Capsules | |
|---|---|---|
| Medicinal ingredient | Capsicum annuum extract (100 mg) | Corn starch (230 mg) |
| Extract (per capsule) | 15:1 DHE 1.5 mg (dry herb) | |
| Potency (per capsule) | 0.7% Dihydrocapsaicin, 0.1% nordihydrocapsaicin and 1.2% capsaicin (2% capsaicinoids) | |
| Non-medicinal ingredients | Cellulose gum, hypromellose | Cellulose gum, hypromellose |
| Pharmaceutical glaze | Sucrose | Sucrose |
| Variable | Treatment | V1 | V7 | p-Value | p-Value | p-Value | ||
|---|---|---|---|---|---|---|---|---|
| Mean | SE | Mean | SE | Treatment | Time | Interaction | ||
| BMI | Placebo | 29.47 | 0.7 | 28.78 | 0.7 | ns | 0.0001 | ns |
| CAE | 28.99 | 0.7 | 27.84 | 0.8 | ||||
| Body weight (kg) | Placebo | 81.2 | 2.1 | 78.7 | 2.1 | 0.1 | <0.0001 | 0.1 |
| CAE | 76.1 | 2.4 | 73.2 | 2.4 | ||||
| Waist Circumference (cm) | Placebo | 91.8 | 1.8 | 89.8 | 1.8 | ns | <0.0001 | ns |
| CAE | 88.4 | 2.1 | 85.9 | 2.1 | ||||
| Fat mass (%) | Placebo | 40.6 | 0.9 | 39.3 | 0.9 | ns | <0.0001 | ns |
| CAE | 39.7 | 1.1 | 38.1 | 1.1 | ||||
| Fat-free mass (kg) | Placebo | 45.5 | 1.0 | 45.2 | 1.0 | 0.08 | 0.02 | ns (0.08) |
| CAE | 43.1 | 1.1 | 42.5 | 1.1 | ||||
| Variable | Treatment | V1 | V7 | p-Value | p-Value | p-Value | ||
|---|---|---|---|---|---|---|---|---|
| Mean | SE | Mean | SE | Treatment | Time | Interaction | ||
| DE_60 (mm) | Placebo | 1576 | 277 | 1792 | 281 | ns | 0.1 | ns |
| CAE | 1265 | 311 | 1678 | 311 | ||||
| DE_180 (mm) | Placebo | 5308 | 551 | 6253 | 560 | 0.07 | 0.02 | ns |
| CAE | 3842 | 619 | 5017 | 619 | ||||
| Hun_AUC_60 | Placebo | 1246 | 262 | 1775 | 267 | ns | 0.08 | ns |
| CAE | 1122 | 294 | 1401 | 294 | ||||
| Hun_AUC60_180 | Placebo | 4800 | 573 | 5832 | 583 | ns | 0.04 | ns |
| CAE | 4225 | 644 | 5023 | 644 | ||||
| Sat_AUC_60 | Placebo | 6536 | 299 | 6353 | 304 | ns | ns | ns |
| CAE | 6596 | 336 | 6762 | 336 | ||||
| Sat_AUC60_180 | Placebo | 10,698 | 651 | 10,028 | 659 | ns | ns | ns |
| CAE | 10,846 | 732 | 11,116 | 732 | ||||
| PFC_AUC_60 | Placebo | 2032 | 293 | 2190 | 297 | ns | ns | ns |
| CAE | 1786 | 329 | 1941 | 329 | ||||
| PFC_AUC60_180 | Placebo | 6049 | 539 | 6818 | 548 | ns | 0.04 | ns |
| CAE | 5102 | 606 | 6026 | 606 | ||||
| Variable | Treatment | V1 | V7 | p-Value | p-Value | p-Value | ||
|---|---|---|---|---|---|---|---|---|
| Mean | SE | Mean | SE | Treatment | Time | Interaction | ||
| TFEQ_hunger | Placebo | 5.96 | 0.64 | 4.17 | 0.64 | ns | ns | 0.09 |
| CAE | 5.27 | 0.72 | 5.75 | 0.73 | ||||
| Variable | Treatment | V1 | V7 | p-Value | p-Value | p-Value | ||
|---|---|---|---|---|---|---|---|---|
| Mean | SE | Mean | SE | Treatment | Time | Interaction | ||
| DQuaN0 | Placebo | 28.1 | 5.0 | 104.6 | 4.9 | ns | <0.001 | ns |
| CAE | 26.6 | 5.9 | 99.8 | 4.7 | ns | <0.001 | ns | |
| DQuaN180 | Placebo | 78.3 | 6.8 | 80.5 | 4.8 | ns | ns | ns |
| CAE | 70.6 | 6.8 | 76.7 | 5.2 | ns | ns | ns | |
| BEnvM_30 | Placebo | 85.9 | 6.9 | 99.9 | 3.6 | ns | ns | ns |
| CAE | 82.6 | 7.2 | 84.5 | 6.7 | ns | ns | ns | |
| BEnvM180 | Placebo | 39.2 | 5.9 | 40.5 | 4.7 | ns | ns | ns |
| CAE | 43.5 | 6.5 | 42.2 | 6.8 | ns | ns | ns | |
| BSenF_30 | Placebo | 81.3 | 7.1 | 94.4 | 5.6 | ns | ns | ns |
| CAE | 86.7 | 6.9 | 80.8 | 6.0 | ns | ns | ns | |
| BSenF180 | Placebo | 34.2 | 5.1 | 42.7 | 4.5 | ns | ns | ns |
| CAE | 47.2 | 6.6 | 39.7 | 5.4 | ns | ns | ns | |
| TFEQ-HUN | Placebo | 5.5 | 0.7 | 4.2 | 0.5 | ns | 0.04 | ns |
| CAE | 5.7 | 0.7 | 5.9 | 0.9 | ns | ns | ns | |
| TFEQ-HIL | Placebo | 1.8 | 0.4 | 1.3 | 0.3 | ns | 0.05 | ns |
| CAE | 1.8 | 0.4 | 1.9 | 0.5 | ns | ns | ns | |
| TFEQ-HEL | Placebo | 2.4 | 0.3 | 1.8 | 0.3 | ns | ns | ns |
| CAE | 2.7 | 0.3 | 2.7 | 0.4 | ns | ns | ns | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Manca, C.; Lacroix, S.; Pérusse, F.; Flamand, N.; Chagnon, Y.; Drapeau, V.; Tremblay, A.; Di Marzo, V.; Silvestri, C. Oral Capsaicinoid Administration Alters the Plasma Endocannabinoidome and Fecal Microbiota of Reproductive-Aged Women Living with Overweight and Obesity. Biomedicines 2021, 9, 1246. https://doi.org/10.3390/biomedicines9091246
Manca C, Lacroix S, Pérusse F, Flamand N, Chagnon Y, Drapeau V, Tremblay A, Di Marzo V, Silvestri C. Oral Capsaicinoid Administration Alters the Plasma Endocannabinoidome and Fecal Microbiota of Reproductive-Aged Women Living with Overweight and Obesity. Biomedicines. 2021; 9(9):1246. https://doi.org/10.3390/biomedicines9091246
Chicago/Turabian StyleManca, Claudia, Sébastien Lacroix, Francine Pérusse, Nicolas Flamand, Yvon Chagnon, Vicky Drapeau, Angelo Tremblay, Vincenzo Di Marzo, and Cristoforo Silvestri. 2021. "Oral Capsaicinoid Administration Alters the Plasma Endocannabinoidome and Fecal Microbiota of Reproductive-Aged Women Living with Overweight and Obesity" Biomedicines 9, no. 9: 1246. https://doi.org/10.3390/biomedicines9091246
APA StyleManca, C., Lacroix, S., Pérusse, F., Flamand, N., Chagnon, Y., Drapeau, V., Tremblay, A., Di Marzo, V., & Silvestri, C. (2021). Oral Capsaicinoid Administration Alters the Plasma Endocannabinoidome and Fecal Microbiota of Reproductive-Aged Women Living with Overweight and Obesity. Biomedicines, 9(9), 1246. https://doi.org/10.3390/biomedicines9091246






