Abstract
Childhood obesity is associated with low socioeconomic status in developed countries, and community programs can deliver cost-effective obesity interventions to vulnerable children and adolescents at scale. Evaluating these programs in a low-cost, time-efficient, and culturally appropriate way with valid and reliable measures is essential to determining their effectiveness. We aimed to identify existing valid and reliable short-form instruments (≤50 items for diet, ≤15 items for physical activity) suitable for the assessment of change in diet, physical activity, and sedentary behaviour in an Australian obesity intervention program for children and adolescents aged 7–13 years from low socioeconomic groups, with a focus on Aboriginal and Torres Strait Islander children. Relevant electronic databases were searched, with a focus on Australian literature. Validity and/or reliability studies using diet instruments (5), physical activity/sedentary behaviour instruments (12), and diet and physical activity/sedentary behaviour instruments used with Aboriginal and Torres Strait Islander (3) children were identified. Seven questions on diet, one question on physical activity, and no questions on sedentary behaviour were recommended. These questions can be used for evaluation in community-based obesity programs among Australian children and adolescents, including those from low socioeconomic groups and Aboriginal and Torres Strait Islander children.
1. Introduction
Obesity in childhood and adolescence is associated with low socioeconomic status in developed countries [1,2,3]. Children who are overweight or obese are more likely to experience health problems, including higher metabolic and cardiometabolic risk factors, asthma, negative psychological outcomes, poorer dental health, and sleep issues [4,5]. They also have a greater likelihood of being overweight or obese as adults [6,7]. Consequently, the lifetime societal and individual burden of childhood obesity may be substantial for those least able to bear the financial cost. Effective, cost-efficient obesity treatment and prevention programs that are accessible to vulnerable groups are critically needed.
Although economic evaluations of childhood obesity interventions have some limitations [8,9,10], there is evidence that childhood obesity interventions of even modest effectiveness are also economically viable from a broader policy perspective [8,11,12]. However, different types of interventions may vary in effectiveness depending on context. In their systematic review and meta-analysis of interventions to treat childhood obesity, Oude Luttikhuis et al. [13] found that specialised obesity clinics run within hospital settings were common among trials included in the review. Obesity clinics may be less available or accessible outside a research setting [13], and barriers such as transport may interfere with participation [14], particularly for non-metropolitan and socioeconomically disadvantaged children. In Australia, 27.4% of children and adolescents aged 5–17 were overweight or obese in 2014–2015 [15], with higher prevalence reported in Aboriginal and Torres Strait Islander children aged 2–14 years [16] and in children aged 2–17 from socioeconomically disadvantaged backgrounds [17]. It is therefore critical that programs that are more relevant for these groups be available. Community programs aiming to improve weight-related behaviours including diet, physical activity, and sedentary behaviours may be more accessible and have the potential for greater reach [13,18]. In a recent survey of obesity prevention practice in Australia, around two-thirds of community interventions targeted vulnerable groups such as low socioeconomic status, Aboriginal or Torres Strait Islander people, or culturally and linguistically diverse groups [19]. However, evaluation using instruments which demonstrate validity and reliability (while also being of low-cost and culturally appropriate) is needed to determine efficacy and support subsequent funding efforts. Moores et al. additionally report that collection of evaluation data may impact program engagement and attendance, and suggest that participant burden may be reduced and evaluation participation enhanced by implementing short instruments [20].
In Australia, Go4Fun® is a government funded community-based healthy lifestyle program intended to improve the health, diet, fitness and self-esteem of children above a healthy weight aged 7–13 years and their families [21,22]. It is based on the UK MEND program (Mind, Exercise, Nutrition… Do it!) [23,24], and has been translated to a community-based program for the Australian context. In 2015–2016, the New South Wales Office of Preventive Health (OPH), which manages Go4Fun®, was undertaking quality improvement of the evaluation measures in the program and requested a rapid review of existing validated short-form survey instruments that assess diet, physical activity, and sedentary behaviour among children. The aim of this review was to inform the OPH of the best available evidence on, and recommend suitable evaluation questions in, the pre/post monitoring of programs that promote healthy eating and physical activity among children over the healthy weight range, such as Go4Fun®. Importantly, the review also considered suitability for Australian Aboriginal and Torres Strait Islander children and families.
2. Results
There were 18 unique validity and/or reliability studies meeting the inclusion criteria identified through two searches of the literature (see Section 3) and from experts in the fields: 5 short diet questions, 12 physical activity and/or sedentary behaviour measures, and 1 additional study identified from the search specific to Aboriginal and Torres Strait Islander children. Two of the papers identified in the search for non-indigenous specific studies were also identified in the search specific to Aboriginal and Torres Strait Islander children. A detailed narrative of each study included in the current review and the project-specific report is provided in Flood et al. [25]. A final list of the short-form questions recommended from the review can be found in the Supplementary Materials.
2.1. Diet Questionnaires
Five studies [26,27,28,29,30] were identified. Of these, one conducted reliability testing only [26], and the remaining studies conducted both validity and reliability testing [27,28,29,30]. Most of the studies did not indicate ethnicity and only half indicated weight status of the participants. Socioeconomic status was generally not indicated. The details of these studies are included in Table 1.

Table 1.
Diet questionnaires included in the review from peer-reviewed journal articles *.
The review identified questions on fruit and vegetable intake, water and sugary drink consumption, discretionary food intake, breakfast consumption, and eating in front of the television as common. The questions we recommended for use in evaluation included frequency of consumption of fruit, vegetables, sugar sweetened beverages, water, and discretionary foods [29]. These have been tested in Aboriginal and Torres Strait Island groups (see Section 2.3). An additional question on eating the dinner meal in front of the television [26] was also recommended.
2.2. Physical Activity and Sedentary Behaviour Questionnaires
Twelve validity and/or reliability studies on physical activity and/or sedentary behaviour measures were identified. Four studies were on physical activity only [31,32,33,34], four were on sedentary behaviour only [35,36,37,38], and four combined physical activity and sedentary behaviour measures [26,39,40,41]. There was a wide age range across the studies, and most of the studies did include details on ethnicity but not on the weight status of the participants. Only three studies involved parents answering the questionnaire [37,38,41]. Inclusion of children with low literacy was indicated in the pilot phase of one of the studies only [26], one included rural Aboriginal and Torres Strait Islander and non-Indigenous children [32], and three studies indicated mixed socioeconomic status (two used maternal education as an indicator) [33,37,41]. The details of these studies are included in Table 2.

Table 2.
Physical activity and sedentary behaviour questionnaires included in the review from peer-reviewed journal articles *.
Frequency and duration of different physical activity and sedentary behaviour domains were commonly reported. One question that had been tested for validity and reliability in a range of child/adolescent profiles [34] and used in the Australian setting [42] was recommended to evaluate physical activity. A suitable short-form question was not found for the evaluation of sedentary behaviour for the Go4Fun® program, however a single question assessing children’s television screen time could be considered [26].
2.3. Diet and Physical Activity/Sedentary Behaviour Questionnaires in Aboriginal and Torres Strait Islander Groups
Only one dietary intake questionnaire [29] and two physical activity questionnaires [32,43] were identified that had been validated with Aboriginal and Torres Strait Islander children. There were no sedentary behaviour questionnaires identified. There was a narrow age range across the studies—none of the studies involved parental response, and only one study included the weight status of the participants [32]. Socioeconomic status and literacy levels were not indicated in these studies. The details of these studies are included in Table 3.

Table 3.
Diet, physical activity and sedentary behaviour questionnaires used in Aboriginal and Torres Strait Islander children included in the review from peer-reviewed journal articles *.
2.4. Quality Ratings
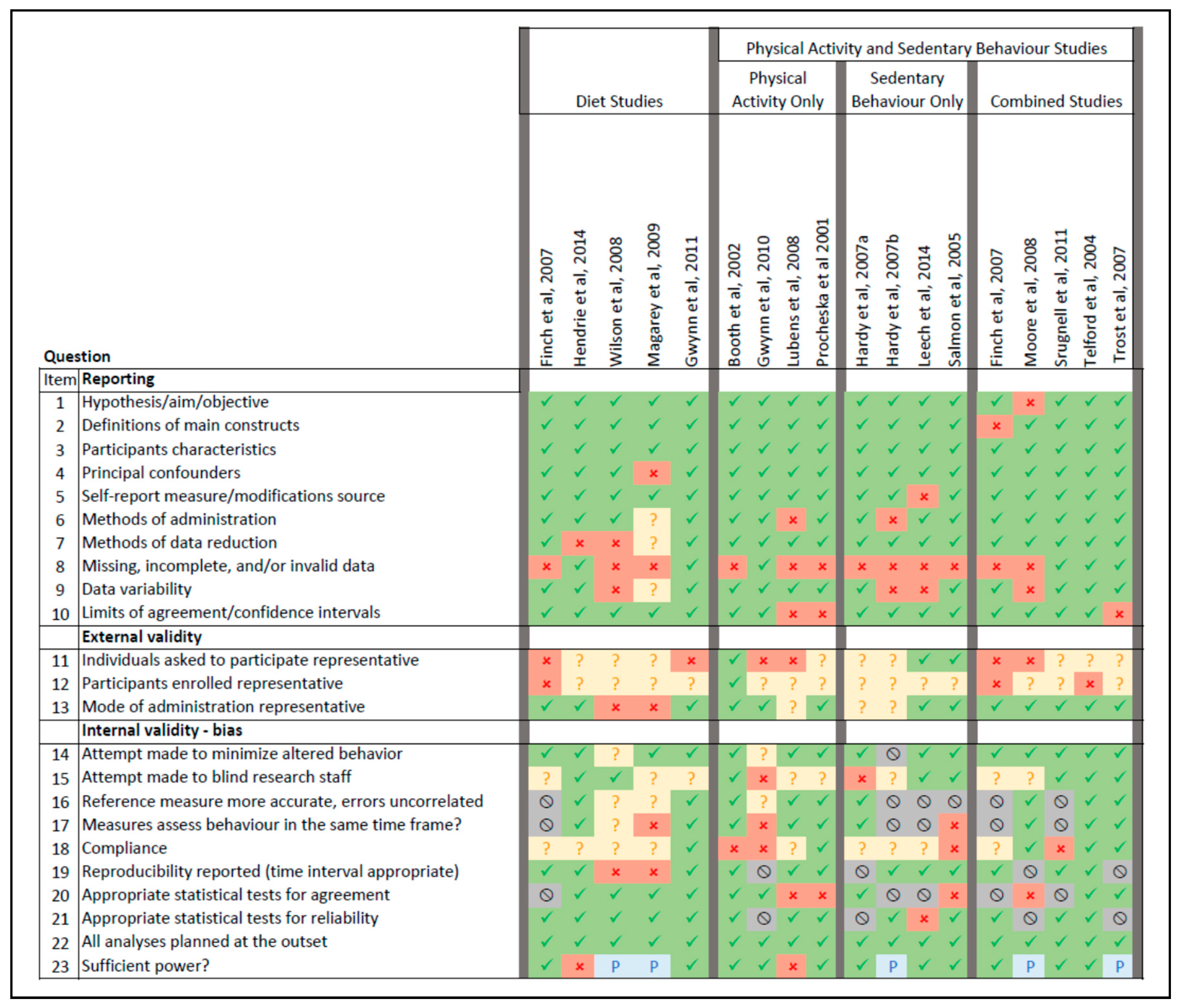
Figure 1 summarises the quality rating for studies.
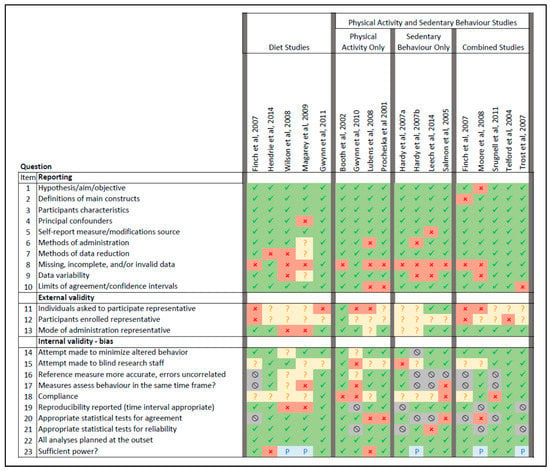
Figure 1.
Visual summary of quality ratings for included individual studies. Green = yes, red = No, amber = unsure/unable to determine, grey = not applicable, blue = partially. The description of each question has been abbreviated.
The reporting of studies was generally adequate, however many studies did not describe the characteristics of participants with missing, incomplete, and/or invalid data. The external validity of both diet and physical activity studies in terms of the representativeness of those invited to participate and those participating was often not able to be determined or was not adequate. However, the mode of administration of instruments was usually representative of similar study designs. Some aspects of internal validity such as attempts to minimise altered behaviour, appropriate statistics to test reliability (where applicable), planning of analyses, and having sufficient power were adequate across the studies.
For validity studies, the reference measure was generally deemed to be more accurate than the test method and assessed behaviour in the same timeframe, however while studies on dietary measurement used appropriate statistics to assess agreement, this was not always the case for studies measuring physical activity/sedentary behaviour. For those studies that assessed reliability, statistics were mostly assessed to be appropriate. Clear exposition of compliance was frequently not provided, and blinding of research staff was either not able to be determined or not done.
3. Discussion
Valid and reliable short-form questions to measure dietary intake, physical activity, and sedentary behaviours are ideal for routine monitoring and evaluation of community programs to treat child and adolescent obesity. Despite the general availability of questionnaires, many of the articles reviewed in the current study did not have information on ethnicity, weight status, socioeconomic status, and literacy levels to determine their suitability for Go4Fun® and similar programs, and many were not tested with a parent proxy. There were few studies specifically conducted with Australian Aboriginal and Torres Strait Island children. Although the general representativeness of the samples recruited across reviewed studies was not optimal, some recommendations were still able to be made based on question validity and reliability, suitability to address the targeted outcomes of Go4Fun® and similar programs, and potential to be administered in different ways and among different population groups. Additionally, the quality of the studies from which questions were recommended [29,34] were satisfactorily rated by reviewers.
The dietary factors evaluated by the recommended short-form dietary questions from the current review align with public health concerns and are similar to those identified by Golley et al. in their recent systematic literature review [44]. These questions demonstrated good reliability, however, satisfactory validity was not consistently demonstrated. Golley et al. similarly found that short-form food questions were more likely to be reliable than valid, and seldom both [44]. Responsiveness (ability to detect change) to an intervention compared with an alternative diet assessment at both time points was not identified in studies included in the current review. The recommended dietary intake questions may therefore be useful to indicate pre–post change in program interventions that target these behaviours, but not the magnitude of change. We found that frequency versus quantity of intake was generally found to be a superior measure. Children under 12 years old may be poor at conceptualising portion size even when prompts are provided [45]. Additionally, questionnaires with prespecified portion sizes may rely on serving sizes that more closely represent population food selection guides, however both adults and children may typically consume portion sizes that vary from guidelines [46,47].
The physical activity questions identified in the current review tended to perform poorly for validation of activity. Accurate assessment of activity in children is known to be difficult and may reflect the cognitive ability of this group in recalling different aspects of physical activity (e.g., intensity, frequency and duration) [48,49,50], as well as the sporadic nature of some activities, particularly of younger children [50,51,52]. In fact, in their systematic review and appraisal of studies of self-administered and proxy-reported physical activity questionnaires in youth, Chinapaw et al. determined that there were no questionnaires available with acceptable validity and reliability [53]. In any case, where program evaluation includes elements across the whole program, the inclusion of longer, more complex physical activity questionnaires [31,41] would impose an unacceptable burden, particularly for low literacy groups. Short-form questions which have demonstrated adequate reliability and validity in the USA as well as having been evaluated across different ethnicities [34] have been recommended for national monitoring in Australia [42], and one of these questions was recommended from our current review for evaluation of physical activity in community programs for children and adolescents. The value of using objective measures of physical activity (e.g., activity trackers such as pedometers and accelerometers) for children and adolescents is often discussed in the physical activity literature, however these may not be suitable. Gwynn et al. found that around 20% of children may remove these devices for various reasons [32]. If they are used in programs where assessment of change is important, it is recommended that a standardised protocol be used across timepoints [54].
Sedentary behaviour occurs across a range of activities in children and adolescents, for example inactive transport, desk-based schoolwork, and various forms of screen time. Australian national guidelines for children and adolescents aged 5–17 years recommend minimising the time spent on sedentary behaviour, and specifically limiting the use of electronic media (including television watching and computer use) to less than two hours a day [55]. The Adolescent Sedentary Activities Questionnaire (ASAQ) [36] was identified in the current review as having reliability and face validity, and does include questions on screen time; however, it is likely to be too lengthy for community program settings. We could not recommend any short-form questions to assess sedentary behaviour more broadly, however a single question assessing children’s television screen time [26] was considered to be potentially suitable for use in community programs if validated in the target population. Although a number of sedentary behaviours are associated with reduced energy expenditure and passive consumption of food [56], the most common measure of sedentary behaviour in this children and adolescents is television watching [57]. In their systematic review of over 200 studies, Tremblay et al. found that watching television for more than 2 h per day was associated with a range of adverse health outcomes, including unfavourable body composition, decreased physical fitness, and poorer scores on psychosocial and academic measures [57]. However, in community programs that target multiple forms of sedentary behaviour, a more global measure would be required. An additional consideration is that screen devices are constantly evolving [58,59], which may require modification of questions that address screen time behaviour.
Few studies were available that were specifically tested in Australian Aboriginal and Torres Strait Islander groups, representing a gap in the literature. In addition to the three studies identified by our review [29,32,43], Thurber et al. recently evaluated the relationship of screen time and dietary factors such as sugar-sweetened beverage and discretionary food intake reported by carers to body mass index trajectories in Aboriginal and Torres Strait Islander children [60]. However, the instrument used was not validated. Healthy physical activity and eating may be experienced differently among Australian indigenous children, as explained by Crowe et al. in their qualitative study of 40 Australian Aboriginal and Torres Strait Islander children aged 5–12 years recruited from the southeastern coast of Australia [61]. They found that healthy lifestyle behaviours were connected and influenced by cultural connections and activities [61], which may need further consideration in future questionnaires that measure diet, physical activity, and sedentary behaviours in this group.
A strength of this study is the consideration of short-form questions suitable for vulnerable child and adolescent populations, including Australian Aboriginal and Torres Strait Island groups. Children from Aboriginal, Torres Strait Islander, and low socioeconomic groups have higher rates of obesity than in the general population [16,17] and there is a need for measures to evaluate suitable programs for these children. A further strength of this study is the inclusion of only short-form questions since many available questionnaires for use in research are lengthy, burdensome, and not suited to a community intervention setting. A limitation of the review is that psychometric assessment of some of the included questionnaires may have favoured recruitment of children from less disadvantaged backgrounds, and as such it may be less applicable for very disadvantaged children, however most of the dietary questions identified were tested for validity and reliability in “priority funded” (disadvantaged) schools. A further weakness of the current work is the timeframe of the review. The searches were completed in mid-2016 due to the requirements of the commissioning body.
4. Materials and Methods
This review was conducted by a research team with expertise in: diet and physical activity interventions with Australian Aboriginal and Torres Strait Islander children as well as non-Indigenous children, the development and interpretation of relevant measurement instruments, and in associated validity/reliability studies.
4.1. Search Criteria
Searches were devised to locate: (1) validity/reliability studies on diet, physical activity, and sedentary behaviour measurement instruments suitable for Australian children and adolescents aged 7–13 years; and (2) studies with a focus on Australian Aboriginal and Torres Strait Islander children; hence, Australian papers were the focus of the search. The search strategy was developed by the review team, and one researcher (J.A.G.) conducted a systematic literature search to identify studies addressing the review questions. English language studies published between 1 January 2005 and 18 April 2016 were identified from the following electronic databases: Medline, CINAHL, EMBASE, and ATSIhealth. Search terms are shown in Table 4.

Table 4.
Search terms *.
4.2. Selection and Inclusion Criteria
The literature search predominately comprised Australian studies in peer-reviewed journal articles, however selected publications from the international literature were also included if they met the inclusion criteria. Diet, physical activity, and sedentary behaviour questions were also sourced from the Parenting, Eating and Activity for Child Health [62] and GRx Active Families [63] as these were known childhood obesity programs in Australia and New Zealand respectively.
Studies were included where the following items were described:
- components of diet, physical activity or sedentary behaviour questions relevant to current Australian nutrition and physical activity/sedentary behaviour policies for those aged 5–12 and 13–17 years, or that make a significant contribution to components of concern identified in policy documents; and
- short questionnaires with ≤50 items for diet [44] and ≤15 items for physical activity (expert opinion); and
- validity or reliability information in the population of interest (7–13 year old Australians); and
- questionnaire administration details indicating completion by children/adolescents or parent proxy.
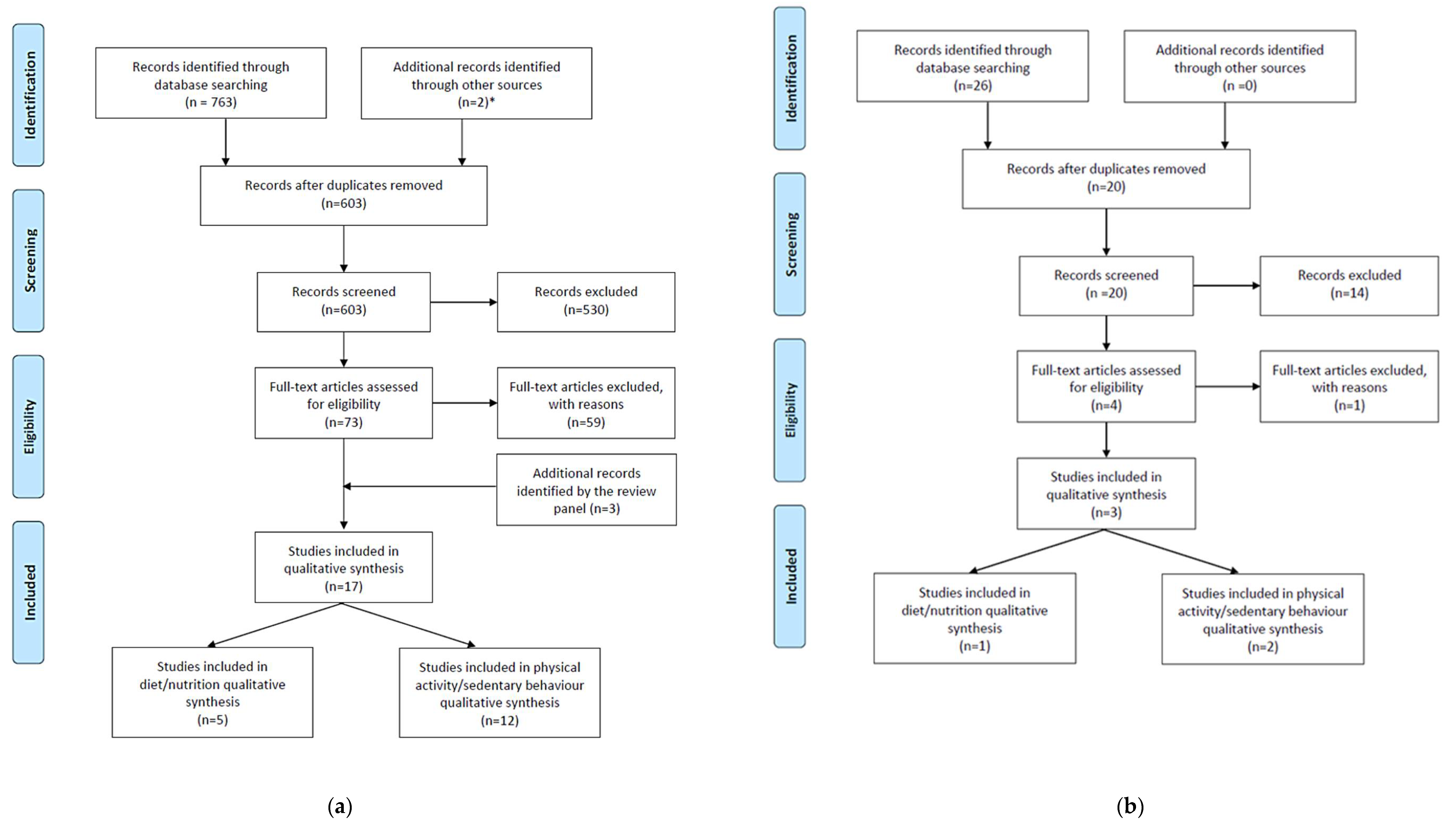
One reviewer (J.A.G.) screened the titles and abstracts of studies identified from the searches following removal of duplicates. Studies not meeting inclusion criteria were removed by the same reviewer. The same inclusion/exclusion criteria were applied to the full text of the remaining studies. Validity/reliability studies from the reference lists of relevant intervention studies and systematic reviews which met the inclusion criteria were included (if publication date was prior to 2005, inclusion was based on expert opinion). Additional references were included as advised by the review team. Figure 2 illustrates the flow of information through the different phases of the review according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) process [64].
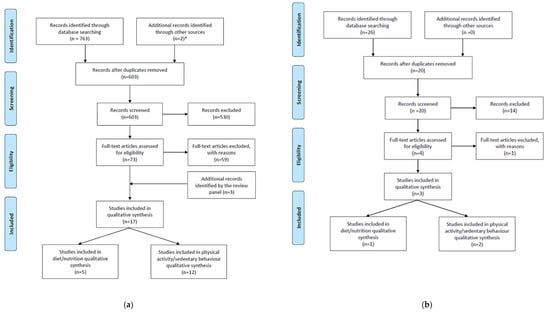
Figure 2.
Flow of information through the different phases of the rapid review for identification of (a) studies on diet and physical activity/sedentary behaviour, and (b) studies on diet and physical activity/sedentary behaviour that specifically relate to Aboriginal and Torres Strait Islander children. The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) diagrams are modified from Moher et al. [64]. * [62,63].
4.3. Data Extraction
Data were extracted by two researchers (J.A.G., J.D.G.) in standardised tables that included: author, year and country of study, program setting and name (if applicable), design, characteristics of the participants (sample size, ethnicity, age, sex, weight status, literacy details, comparison group), tool type and number of items, response variables, recall period, administration method, respondent (child or parent), respondent burden, duration of the study, period between administration (for reliability), reliability statistics, reference method (for validity), and validity statistics.
4.4. Assessment of Quality
The methodological quality of each paper that met inclusion criteria was independently assessed by two of four members of the review team (J.A.G., J.D.G., L.L.H., V.M.F.) using a modified version of the Hagströmer–Bowles Physical Activity/Sedentary Behaviour Questionnaire Checklist (HBQC) [65], which is based on the scale devised by Downs and Black [66]. Members of the review team did not rate studies for which they were also an author.
The HBQC was modified to assess dietary validation/reliability papers simply by inserting relevant terminology in place of the physical activity/sedentary behaviour terminology. Additionally, in order to assess reliability in the studies, one question was added as follows:
“Were the statistical tests used appropriate to assess reliability for the main physical activity constructs between tests for the self-report measure?”(The statistical techniques used must be appropriate to the data e.g., intra-class correlation co-efficient, weighted kappa).
While the HBQC scores items numerically, questions were simply assigned a value of yes, no, or unable to be determined/unsure for the current review. A “partially” option was available for the final question on statistical power, as per the HBQC. To accommodate studies that reported either validity or reliability but not both, a not applicable (N/A) option was included for relevant questions. A decision was made not to score the papers numerically because some individual questions may have more or less perceived importance qualitatively, and some methodological areas may have more or less questions; these two factors may bias the impression of the overall quality of the paper for low or high numerical scores.
All four raters met to discuss the ratings and settle differences in ratings at an interim stage to assist with consistency by checking interpretation on quality items. When all papers had been rated individually, pairs met by phone or in person to discuss any differences. Differences that were not resolved by discussion were shared with the full team for adjudication. A record of decisions on interpretations was kept and shared with the team for review of past decisions to ensure all quality items were rated consistently within and across pairs of raters.
4.5. Recommendations on Questions
Four members of the review team (J.A.G., J.D.G., L.L.H., V.M.F.) were involved in the final recommendations on the questions. Deliberations were made by group discussion following (and based on) data extraction of included studies. Factors considered by reviewers included the questions’ validity and reliability, suitability to address the objectives (targeted outcomes) of the Go4Fun® program, and potential to be administered in different ways and among different population groups, in particular, Aboriginal and Torres Strait Islander children. Acceptable (statistically significant) validity and reliability were required. Specific outcomes measured in the Go4Fun® program included daily servings of fruit, dairy foods, vegetables, sugar-sweetened beverages, and discretionary foods, as well as hours in physical activity and sedentary behaviour (screen time and non-active transport).
5. Conclusions
In conclusion, there were some valid and reliable questionnaires that were considered useful for evaluation of our community-based obesity intervention targeting healthier diet, physical activity, and sedentary behaviour in Australian children and adolescents. Questionnaires selected for evaluation of programs need to capture the objectives of the intervention. The questions identified in this rapid review can provide information on the primary factors involved in child obesity prevention, that is, consumption of fruit and vegetables, sugar-sweetened beverages, and energy-dense nutrients, poor eating habits, time spent in physical activity, and screen time. Culturally appropriate support must be provided for Aboriginal and Torres Strait Islander children completing the survey questions. Central to this is ensuring a key role for their community members in survey administration and in interpretation of results.
Supplementary Materials
The following are available online at http://www.mdpi.com/2227-9067/5/7/95/s1.
Author Contributions
Conceptualization, L.C.H. and C.I.-H.; Data curation, J.A.G.; Formal analysis, J.A.G., J.D.G., L.L.H., and V.M.F.; Funding acquisition, L.C.H., C.I.-H., and V.M.F.; Investigation, J.A.G., J.D.G., L.L.H., and V.M.F.; Methodology, J.A.G., J.D.G., L.L.H., N.T., and V.M.F.; Project administration, L.C.H., C.I.-H., and V.M.F.; Resources, V.M.F.; Writing—original draft, J.A.G., J.D.G., L.L.H., and V.M.F.; Writing—review and editing, J.A.G., J.D.G., L.L.H., N.T., V.M.F., L.C.H., and C.I.-H.
Funding
NSW Ministry of Health.
Acknowledgments
This review was brokered by the Sax Institute for the NSW Ministry of Health. The authors would like to acknowledge funding received from the NSW Ministry of Health to conduct and publish this study. We would like to thank Gai Moore and Jillian Hutchinson from the Sax Institute for their administrative skills on the project. The authors would like to acknowledge the contribution of the Better Health Company, which contributes to quality improvement initiatives for the Go4Fun® program, in particular the review of participants’ surveys.
Conflicts of Interest
The funding sponsors advised on the study question and supplied reports for consideration on the literature. The funders did not participate in the collection, analyses or interpretation of data, the writing of the manuscript, or in the decision to publish the results.
References
- Broyles, S.T.; Denstel, K.D.; Church, T.S.; Chaput, J.P.; Fogelholm, M.; Hu, G.; Kuriyan, R.; Kurpad, A.; Lambert, E.V.; Maher, C.; et al. The epidemiological transition and the global childhood obesity epidemic. Int. J. Obes. Suppl. 2015, 5, S3–S8. [Google Scholar] [CrossRef] [PubMed]
- Hardy, L.L.; Mihrshahi, S.; Gale, J.; Drayton, B.A.; Bauman, A.; Mitchell, J. 30-year trends in overweight, obesity and waist-to-height ratio by socioeconomic status in australian children, 1985 to 2015. Int. J. Obes. 2017, 41, 76–82. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Report of the Commission on Ending Childhood Obesity; World Health Organisation: Geneva, Switzerland, 2016. [Google Scholar]
- Sanders, R.H.; Han, A.; Baker, J.S.; Cobley, S. Childhood obesity and its physical and psychological co-morbidities: A systematic review of Australian children and adolescents. Eur. J. Pediatr. 2015, 174, 715–746. [Google Scholar] [CrossRef] [PubMed]
- Pulgaron, E.R. Childhood obesity: A review of increased risk for physical and psychological comorbidities. Clin. Ther. 2013, 35, A18–A32. [Google Scholar] [CrossRef] [PubMed]
- Laitinen, J.; Power, C.; Jarvelin, M.R. Family social class, maternal body mass index, childhood body mass index, and age at menarche as predictors of adult obesity. Am. J. Clin. Nutr. 2001, 74, 287–294. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.S.; Mulder, C.; Twisk, J.W.; van Mechelen, W.; Chinapaw, M.J. Tracking of childhood overweight into adulthood: A systematic review of the literature. Obes. Rev. 2008, 9, 474–488. [Google Scholar] [CrossRef] [PubMed]
- Ma, S.; Frick, K.D. A simulation of affordability and effectiveness of childhood obesity interventions. Acad. Pediatr. 2011, 11, 342–350. [Google Scholar] [CrossRef] [PubMed]
- Doring, N.; Mayer, S.; Rasmussen, F.; Sonntag, D. Economic evaluation of obesity prevention in early childhood: Methods, limitations and recommendations. Int. J. Environ. Res. Public Health 2016, 13, 911. [Google Scholar] [CrossRef] [PubMed]
- John, J.; Wolfenstetter, S.B.; Wenig, C.M. An economic perspective on childhood obesity: Recent findings on cost of illness and cost effectiveness of interventions. Nutrition 2012, 28, 829–839. [Google Scholar] [CrossRef] [PubMed]
- Wen, L.M.; Baur, L.A.; Simpson, J.M.; Rissel, C.; Wardle, K.; Flood, V.M. Effectiveness of home based early intervention on children’s BMI at age 2: Randomised controlled trial. Br. Med. J. 2012, 344. [Google Scholar] [CrossRef] [PubMed]
- Wen, L.M.; Baur, L.A.; Rissel, C.; Flood, V.; Simpson, J.M.; Hayes, A.; Hardy, L.L.; Wardle, K. Healthy beginnings trial phase 2 study: Follow-up and cost-effectiveness analysis. Contemp. Clin. Trials 2012, 33, 396–401. [Google Scholar] [CrossRef] [PubMed]
- Oude Luttikhuis, H.; Baur, L.; Jansen, H.; Shrewsbury, V.A.; O’Malley, C.; Stolk, R.P.; Summerbell, C.D. Interventions for treating obesity in children. Cochrane Database Syst. Rev. 2009. [Google Scholar] [CrossRef] [PubMed]
- Berry, D.; Melkus, G.; Savoye, M.; Grey, M. An intervention for multiethnic obese parents and overweight children. Appl. Nurs. Res. 2007, 20, 63–71. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. 4364.0.55.001—National Health Survey: First Results, 2014–2015. Available online: http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/4364.0.55.001~2014-15~Main%20Features~Children’s%20risk%20factors~31 (accessed on 14 July 2017).
- Australian Bureau of Statistics. 4727.0.55.001—Australian Aboriginal and Torres Strait Islander Health Survey: First Results, Australia, 2012–2013. Available online: http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/A07BD8674C37D838CA257C2F001459FA?opendocument (accessed on 14 July 2017).
- Australian Bureau of Statistics. 4364.0.55.003—Australian Health Survey: Updated Results, 2011–2012. Available online: http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/33C64022ABB5ECD5CA257B8200179437?opendocument (accessed on 14 July 2017).
- Nichols, M.S.; Reynolds, R.C.; Waters, E.; Gill, T.; King, L.; Swinburn, B.A.; Allender, S. Community-based efforts to prevent obesity: Australia-wide survey of projects. Health Promot. J. Aust. 2013, 24, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Pettman, T.; Bolton, K.; Love, P.; Waters, E.; Gill, T.; Whelan, J.; Boylan, S.; Armstrong, R.; Coveney, J.; Booth, S.; et al. A snapshot of the scope of obesity prevention practice in Australia. Health Promot. Int. 2016, 31, 582–594. [Google Scholar] [CrossRef] [PubMed]
- Moores, C.J.; Miller, J.; Perry, R.A.; Chan, L.L.H.; Daniels, L.A.; Vidgen, H.A.; Magarey, A.M. Consort to community: Translation of an RCT to a large-scale community intervention and learnings from evaluation of the upscaled program. BMC Public Health 2017, 17, 918. [Google Scholar] [CrossRef] [PubMed]
- Welsby, D.; Nguyen, B.; O’Hara, B.J.; Innes-Hughes, C.; Bauman, A.; Hardy, L.L. Process evaluation of an up-scaled community based child obesity treatment program: NSW Go4Fun®. BMC Public Health 2014, 14, 140. [Google Scholar] [CrossRef] [PubMed]
- Henderson, L.; Lukeis, S.; O’Hara, B.; McGill, B.; Innes-Hughes, C.; Rissel, C. Go4Fun®: Evidence and Evaluation Summary (2011–2015); NSW Ministry of Health: North Sydney, Australia, 2016.
- Kolotourou, M.; Radley, D.; Gammon, C.; Smith, L.; Chadwick, P.; Sacher, P.M. Long-term outcomes following the MEND 7–13 child weight management program. Child. Obes. 2015, 11, 325–330. [Google Scholar] [CrossRef] [PubMed]
- Sacher, P.M.; Kolotourou, M.; Chadwick, P.M.; Cole, T.J.; Lawson, M.S.; Lucas, A.; Singhal, A. Randomized controlled trial of the MEND program: A family-based community intervention for childhood obesity. Obesity 2010, 18 (Suppl. 1), S62–S68. [Google Scholar] [CrossRef] [PubMed]
- Flood, V.; Gwynn, J.; Gifford, J.; Tuner, N.; Hardy, L. Evidence on Existing, Validated Short-Form Survey Instruments for Children’s Diet, Physical Activity, and Sedentary Behaviour: An Evidence Check Review Brokered by the Sax Institute (www.Saxinstitute.Org.Au) for the NSW Ministry of Health, 2016; Sax Institute: Ultimo, Australia, 2016; Available online: https://www.saxinstitute.org.au/category/publications/ (accessed on 29 March 2018).
- Finch, M.; Begley, A.; Sutherland, R.; Harrison, M.; Collins, C. Development and reproducibility of a tool to assess school food-purchasing practices and lifestyle habits of Australian primary school-aged children. Nutr. Diet. 2007, 64, 86–92. [Google Scholar] [CrossRef]
- Hendrie, G.A.; Viner Smith, E.; Golley, R.K. The reliability and relative validity of a diet index score for 4-11-year-old children derived from a parent-reported short food survey. Public Health Nutr. 2014, 17, 1486–1497. [Google Scholar] [CrossRef] [PubMed]
- Magarey, A.; Golley, R.; Spurrier, N.; Goodwin, E.; Ong, F. Reliability and validity of the Children’s Dietary Questionnaire; a new tool to measure children’s dietary patterns. Int. J. Pediatr. Obes. 2009, 4, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Gwynn, J.D.; Flood, V.M.; D’Este, C.A.; Attia, J.R.; Turner, N.; Cochrane, J.; Wiggers, J.H. On Behalf of the Many Rivers Diabetes Prevention Project Study Team. The reliability and validity of a short FFQ among Australian Aboriginal and Torres Strait Islander and non-Indigenous rural children. Public Health Nutr. 2011, 14, 388–401. [Google Scholar] [CrossRef] [PubMed]
- Wilson, A.M.; Magarey, A.M.; Mastersson, N. Reliability and relative validity of a child nutrition questionnaire to simultaneously assess dietary patterns associated with positive energy balance and food behaviours, attitudes, knowledge and environments associated with healthy eating. Int. J. Behav. Nutr. Phys. Act. 2008, 5, 5. [Google Scholar] [CrossRef] [PubMed]
- Booth, M.L.; Okely, A.D.; Chey, T.N.; Bauman, A. The reliability and validity of the Adolescent Physical Activity Recall Questionnaire. Med. Sci. Sports Exerc. 2002, 34, 1986–1995. [Google Scholar] [CrossRef] [PubMed]
- Gwynn, J.D.; Hardy, L.L.; Wiggers, J.H.; Smith, W.T.; D’Este, C.A.; Turner, N.; Cochrane, J.; Barker, D.J.; Attia, J.R. The validation of a self-report measure and physical activity of Australian Aboriginal and Torres Strait Islander and non-Indigenous rural children. Aust. N. Z. J. Public Health 2010, 34 (Suppl. 1), S57–S65. [Google Scholar] [CrossRef] [PubMed]
- Lubans, D.; Morgan, P. Impact of an extra-curricular school sport programme on determinants of objectively measured physical activity among adolescents. Health Educ. J. 2008, 67, 305–320. [Google Scholar] [CrossRef]
- Prochaska, J.J.; Sallis, J.F.; Long, B. A physical activity screening measure for use with adolescents in primary care. Arch. Pediatr. Adolesc. Med. 2001, 155, 554–559. [Google Scholar] [CrossRef] [PubMed]
- Hardy, L.L.; Bass, S.L.; Booth, M.L. Changes in sedentary behavior among adolescent girls: A 2.5-year prospective cohort study. J. Adolesc. Health 2007, 40, 158–165. [Google Scholar] [CrossRef] [PubMed]
- Hardy, L.L.; Booth, M.L.; Okely, A.D. The reliability of the Adolescent Sedentary Activity Questionnaire (ASAQ). Prev. Med. 2007, 45, 71–74. [Google Scholar] [CrossRef] [PubMed]
- Leech, R.M.; McNaughton, S.A.; Timperio, A. Clustering of children’s obesity-related behaviours: Associations with sociodemographic indicators. Eur. J. Clin. Nutr. 2014, 68, 623–628. [Google Scholar] [CrossRef] [PubMed]
- Salmon, J.; Timperio, A.; Telford, A.; Carver, A.; Crawford, D. Association of family environment with children’s television viewing and with low level of physical activity. Obes. Res. 2005, 13, 1939–1951. [Google Scholar] [CrossRef] [PubMed]
- Moore, H.J.; Ells, L.J.; McLure, S.A.; Crooks, S.; Cumbor, D.; Summerbell, C.D.; Batterham, A.M. The development and evaluation of a novel computer program to assess previous-day dietary and physical activity behaviours in school children: The Synchronised Nutrition and Activity Program (SNAP). Br. J. Nutr. 2008, 99, 1266–1274. [Google Scholar] [CrossRef] [PubMed]
- Strugnell, C.; Renzaho, A.; Ridley, K.; Burns, C. Reliability of the modified Child and Adolescent Physical Activity and Nutrition Survey, Physical Activity (CAPANS-PA) Questionnaire among Chinese-Australian youth. BMC Med. Res. Methodol. 2011, 11, 122. [Google Scholar] [CrossRef] [PubMed]
- Telford, A.; Salmon, J.; Jolley, D.; Crawford, D. Reliability and validity of physical activity questionnaires for children: The Children’s Leisure Activities Study Survey (CLASS). Pediatr. Exerc. Sci. 2004, 16, 64–78. [Google Scholar] [CrossRef]
- Active Healthy Kids Australia. Is Sport Enough? The 2014 Active Healthy Kids Australia Report Card on Physical Activity for Children and Young People; Active Healthy Kids Australia: Adelaide, Australia, 2014. [Google Scholar]
- Trost, S.G.; Marshall, A.L.; Miller, R.; Hurley, J.T.; Hunt, J.A. Validation of a 24-h physical activity recall in Indigenous and non-Indigenous Australian adolescents. J. Sci. Med. Sport 2007, 10, 428–435. [Google Scholar] [CrossRef] [PubMed]
- Golley, R.K.; Bell, L.K.; Hendrie, G.A.; Rangan, A.M.; Spence, A.; McNaughton, S.A.; Carpenter, L.; Allman-Farinelli, M.; de Silva, A.; Gill, T.; et al. Validity of short food questionnaire items to measure intake in children and adolescents: A systematic review. J. Hum. Nutr. Diet. 2016. [Google Scholar] [CrossRef] [PubMed]
- Nelson, M.; Bingham, S. Assessment of food consumption and nutrient intake. In Design Concepts in Nutritional Epidemiology, 2nd ed.; Margetts, B., Nelson, M., Eds.; Oxford University Press: Oxford, UK, 1997; pp. 123–169. [Google Scholar]
- Collins, C.E.; Bucher, T.; Taylor, A.; Pezdirc, K.; Lucas, H.; Watson, J.; Rollo, M.; Duncanson, K.; Hutchesson, M.J.; Burrows, T. How big is a food portion? A pilot study in Australian families. Health Promot. J. Aust. 2015, 26, 83–88. [Google Scholar] [CrossRef] [PubMed]
- Zheng, M.; Wu, J.H.; Louie, J.C.; Flood, V.M.; Gill, T.; Thomas, B.; Cleanthous, X.; Neal, B.; Rangan, A. Typical food portion sizes consumed by Australian adults: Results from the 2011–12 Australian National Nutrition and Physical Activity Survey. Sci. Rep. 2016, 6, 19596. [Google Scholar] [CrossRef] [PubMed]
- Baranowski, T. Validity and reliability of self report measures of physical activity: An information-processing perspective. Res. Q. Exerc. Sport 1988, 59, 314–327. [Google Scholar] [CrossRef]
- Sallis, J.F. Self-report measures of children’s physical activity. J. Sch. Health 1991, 61, 215–219. [Google Scholar] [CrossRef] [PubMed]
- Sirard, J.R.; Pate, R.R. Physical activity assessment in children and adolescents. Sports Med. 2001, 31, 439–454. [Google Scholar] [CrossRef] [PubMed]
- Willis, E.A.; Ptomey, L.T.; Szabo-Reed, A.N.; Honas, J.J.; Lee, J.; Washburn, R.A.; Donnelly, J.E. Length of moderate-to-vigorous physical activity bouts and cardio-metabolic risk factors in elementary school children. Prev. Med. 2015, 73, 76–80. [Google Scholar] [CrossRef] [PubMed]
- Poitras, V.J.; Gray, C.E.; Borghese, M.M.; Carson, V.; Chaput, J.P.; Janssen, I.; Katzmarzyk, P.T.; Pate, R.R.; Gorber, S.C.; Kho, M.E.; et al. Systematic review of the relationships between objectively measured physical activity and health indicators in school-aged children and youth. Appl. Physiol. Nutr. Metab. 2016, 41, S197–S239. [Google Scholar] [CrossRef] [PubMed]
- Chinapaw, M.J.; Mokkink, L.B.; van Poppel, M.N.; van Mechelen, W.; Terwee, C.B. Physical activity questionnaires for youth: A systematic review of measurement properties. Sports Med. 2010, 40, 539–563. [Google Scholar] [CrossRef] [PubMed]
- Pedisic, Z.; Zhong, A.; Hardy, L.L.; Salmon, J.; Okely, A.D.; Chau, J.; van der Ploeg, H.P.; Bauman, A. Physical activity prevalence in Australian children and adolescents: Why do different surveys provide so different estimates, and what can we do about it? Kinesiology 2017, 49, 135–145. [Google Scholar] [CrossRef]
- Australian Government Department of Health. Australia’s Physical Activity and Sedentary Behaviour Guidelines. Available online: http://www.health.gov.au/internet/main/publishing.nsf/Content/health-pubhlth-strateg-phys-act-guidelines (accessed on 31 January 2018).
- Chaput, J.P.; Klingenberg, L.; Astrup, A.; Sjodin, A.M. Modern sedentary activities promote overconsumption of food in our current obesogenic environment. Obes. Rev. 2011, 12, e12–e20. [Google Scholar] [CrossRef] [PubMed]
- Tremblay, M.S.; LeBlanc, A.G.; Kho, M.E.; Saunders, T.J.; Larouche, R.; Colley, R.C.; Goldfield, G.; Connor Gorber, S. Systematic review of sedentary behaviour and health indicators in school-aged children and youth. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 98. [Google Scholar] [CrossRef] [PubMed]
- Lenhart, A. Teens, Smartphones & Texting; Pew Research Center’s Internet and American Life Project: Washington, DC, USA, 2012. [Google Scholar]
- Weerakkody, N. Mobile phones and children: An Australian perspective. In Proceedings of the 2008 Informing Science + Information Technology Education Conference, Varna, Bulgaria, 22–25 June 2008; Informing Science Institute: Varna, Bulgaria, 2008. [Google Scholar]
- Thurber, K.A.; Dobbins, T.; Neeman, T.; Banwell, C.; Banks, E. Body mass index trajectories of Indigenous Australian children and relation to screen time, diet, and demographic factors. Obesity 2017, 25, 747–764. [Google Scholar] [CrossRef] [PubMed]
- Crowe, R.; Stanley, R.; Probst, Y.; McMahon, A. Culture and healthy lifestyles: A qualitative exploration of the role of food and physical activity in three urban Australian indigenous communities. Aust. N. Z. J. Public Health 2017, 41, 411–416. [Google Scholar] [CrossRef] [PubMed]
- Croyden, D. PEACHTM QLD Final Report; Queensland Government Department of Health: Brisbane, Australia, 2016.
- Wood, A.; Johnson, M. Green Prescriptions (GRX) Active Families Survey Report; Ministry of Health: Wellington, DC, USA, 2015.
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The prisma statement. J. Clin. Epidemiol. 2009, 62, 1006–1012. [Google Scholar] [CrossRef] [PubMed]
- Hagstromer, M.; Ainsworth, B.E.; Kwak, L.; Bowles, H.R. A checklist for evaluating the methodological quality of validation studies on self-report instruments for physical activity and sedentary behavior. J. Phys. Act. Health 2012, 9 (Suppl. 1), S29–S36. [Google Scholar] [CrossRef] [PubMed]
- Downs, S.H.; Black, N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J. Epidemiol. Community Health 1998, 52, 377–384. [Google Scholar] [CrossRef] [PubMed]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).