Enhanced Milieu Teaching with Phonological Emphasis: A Pilot Telepractice Parent Training Study for Toddlers with Clefts
Abstract
:1. Introduction
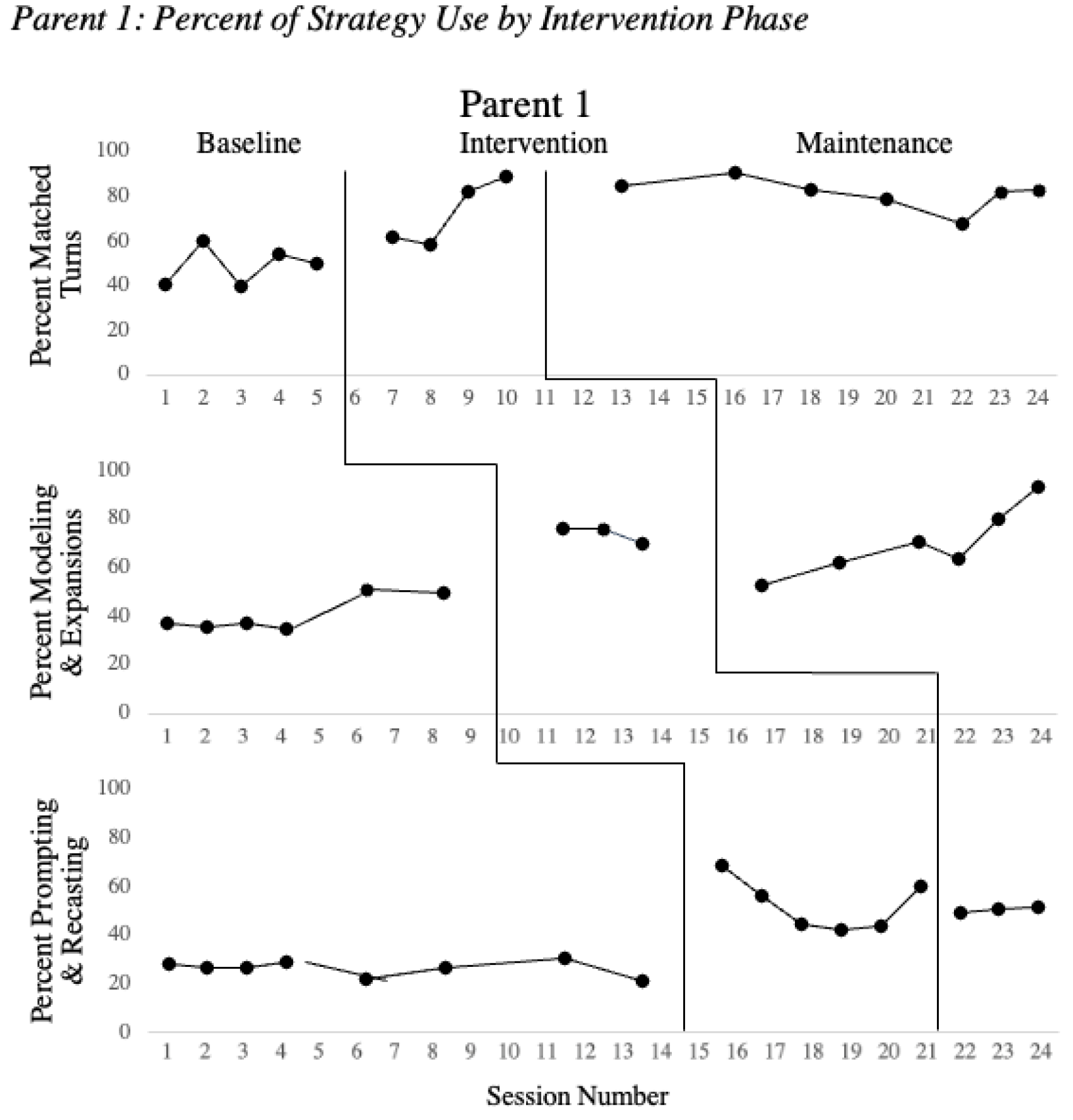
- Does parent use of EMT + PE strategies, including (a) matched turns and environmental arrangement, (b) modeling and expansions, and (c) prompting and speech recasting increase with parent-training on these specific strategies during intervention and maintain following the intervention?
- Do the children’s consonant inventory, percent of consonants correct (PCC), word structure match (WSM), whole word accuracy (ACM) and expressive language use result in significant effect size differences between pre-intervention to post-intervention? And how do these changes compare with the performance of a noncleft twin who did not participate in the intervention?
2. Materials and Methods
2.1. Study Design
2.1.1. Pre–Post Intervention Assessment
2.1.2. Baseline Phase
2.1.3. Intervention Phase
2.1.4. Maintenance Phase
2.1.5. Reliability and Procedural Fidelity
2.2. Analysis
3. Results
3.1. Parent Strategy Use over the Course of Intervention
3.2. Procedural Fidelity
3.3. Parent Strategy Effect Sizes
3.4. Parent Feedback
3.5. Child Speech and Language Characteristics
4. Discussion
4.1. Parent Use of EMT + PE Strategies
4.2. Maintenance of Strategy Use
4.3. Child Language and Speech Outcomes
4.4. Speech Outcomes
4.5. Structural Considerations
5. Clinical Implications
6. Limitations
7. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Cleft Palate Association. Parameters for Evaluation and Treatment of Patients with Cleft Lip/Palate or Other Craniofacial Differences; American Cleft Palate Association: Chapel Hill, NC, USA, 2018; Available online: https://journals.sagepub.com/doi/pdf/10.1177/1055665617739564 (accessed on 11 February 2020).
- Peterson-Falzone, S.J.; Trost-Cardamone, J.E.; Karnell, M.P.; Hardin-Jones, M.A. The Clinician’s Guide to Treating Cleft Palate Speech, 2nd ed.; Elsevier: Amsterdam, The Netherlands, 2017. [Google Scholar]
- Hardin-Jones, M.; Chapman, K.L. Early Lexical Characteristics of Toddlers with Cleft Lip and Palate. Cleft-Palate Craniofacial J. 2014, 51, 622–631. [Google Scholar] [CrossRef] [PubMed]
- Lancaster, H.S.; Lien, K.M.; Chow, J.C.; Frey, J.R.; Scherer, N.J.; Kaiser, A.P. Early Speech and Language Development in Children with Nonsyndromic Cleft Lip and/or Palate: A Meta-Analysis. J. Speech Lang. Hear. Res. 2020, 63, 14–31. [Google Scholar] [CrossRef]
- Bessell, A.; Sell, D.; Whiting, P.; Roulstone, S.; Albery, L.; Persson, M.; Verhoeven, A.; Burke, M.; Ness, A.R. Speech and language therapy interventions for children with cleft palate: A systematic review. Cleft-Palate Craniofacial J. 2013, 50, e1–e17. [Google Scholar] [CrossRef] [PubMed]
- Alighieri, C.; Bettens, K.; Bruneel, L.; Sseremba, D.; Musasiki, D.; Ojok, I.; Van Lierde, K. Comparison of motor-phonetic versus phonetic-phonological speech therapy approaches in a patient with cleft (lip and) palate: A study in Uganda. Int. J. Pediatric Otorhinolaryngol. 2020, 131, 109849. [Google Scholar] [CrossRef] [PubMed]
- Scherer, N.J.; Kaiser, A.P.; Frey, J.R.; Lancaster, H.P.; Lien, K.; Roberts, M.Y. Effects of a naturalistic early intervention on the speech outcomes of young children with cleft palate. Int. J. Speech-Lang. Pathol. 2020, 22, 549–558. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, A.P.; Scherer, N.J.; Frey, J.R.; Roberts, M.Y. The Effects of Enhanced Milieu Teaching with Phonological Emphasis on the Speech and Language of Young Children with Cleft Palate: A Pilot Study. Am. J. Speech-Lang. Pathol. 2017, 26, 806–818. [Google Scholar] [CrossRef]
- Ha, S. Effectiveness of a parent-implemented intervention program for young children with cleft palate. Int. J. Pediatric Otorhinolaryngol. 2015, 79, 707–715. [Google Scholar] [CrossRef]
- Scherer, N.J.; Williams, A.L.; Proctor-Williams, K. Early and Later Vocalization Skills in Children With and without Cleft Palate. Int. J. Pediatric Otorhinolaryngol. 2008, 72, 827–840. [Google Scholar] [CrossRef]
- Scherer, N.J. The Speech and Language Status of Toddlers with Cleft Lip and/or Palate Following Early Vocabulary Intervention. Am. J. Speech Lang. Pathol. 1999, 8, 81–93. [Google Scholar] [CrossRef]
- Scherer, N.J.; Yamashita, R.; de Oliveira, D.N.; DiLallo, J.; Trindade, I.; Fukushiro, A.P.; Richards, K. Early speech and language intervention in Brazilian-Portuguese toddlers with cleft lip and/or palate. Clin. Linguist. Phon. 2021. [Google Scholar] [CrossRef]
- Kaiser, A.P.; Roberts, M.Y. Parents as communication partners: An evidence-based strategy for improving parent support for language and communication in everyday settigngs. SIG 1 Perspect. Lang. Learn. Educ. 2013, 20, 96–111. [Google Scholar] [CrossRef]
- Roberts, M.Y.; Kaiser, A.P. Early intervention for toddlers with language delays: A randomized control trial. Pediatrics 2015, 135, 686–693. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roberts, M.Y.; Kaiser, A.P.; Wolfe, C.E.; Bryant, J.D.; Spidalieri, A.M. Effects of the Teach-Model-Coach-Review Instructional Approach on Caregiver Use of Language Support Strategies and Children’s Expressive Language Skills. J. Speech Lang. Hear. Res. 2014, 57, 1851–1869. [Google Scholar] [CrossRef] [PubMed]
- Roberts, M.Y.; Kaiser, A.P. The Effectiveness of Parent-Implemented Language Interventions: A Meta-Analysis. Am. J. Speech-Lang. Pathol. 2011, 20, 180–199. [Google Scholar] [CrossRef]
- McDuffie, A.; Oakes, A.; Machalicek, W.; Ma, M.; Bullard, L.; Nelson, S.; Abbeuto, L. Early Language Intervention Using Distance Video-Teleconfrencing: A Pilot Study of Young Boys with Fragile X Syndrome and Their Mothers. Am. J. Speech-Lang. Pathol. 2016, 24, 45–66. [Google Scholar]
- Akemoglu, Y.; Muharib, R.; Meadan, H. A Systematic and Quality Review of Parent-Implemented Language and Communication Interventions Conducted via Telepractice. J. Behav. Educ. 2020, 29, 282–316. [Google Scholar] [CrossRef]
- Wainer, A.; Ingersoll, B. Intervention fidelity: An essential component for understanding ASD parent training research and practice. Clin. Psychol. Sci. Pract. 2013, 20, 335–357. [Google Scholar] [CrossRef]
- Snodgrass, M.R.; Chung, M.Y.; Biller, M.F.; Appel, K.E.; Meadan, H.; Halle, J.W. Telepractice in Speech-Language Therapy: The Use of Online Technologies for Parent Training and Coaching. Commun. Disord. Q. 2017, 38, 242–254. [Google Scholar] [CrossRef]
- Scherer, N.J.; D’Antonio, L.L.; Kalbfleisch, J.H. Early speech and language development in children with velocardiofacial syndrome. Am. J. Med. Genet. 1999, 88, 714–723. [Google Scholar] [CrossRef]
- Chapman, K.L.; Hardin-Jones, M.; Halter, K.A. The Relationship Between Early Speech and Later Language Performance for Children with Cleft Lip and Palate. Clin. Linguist. Phon. 2003, 17, 173–197. [Google Scholar] [CrossRef]
- Scherer, N.J.; Boyce, S.; Martin, G. Pre-linguistic children with cleft palate: Growth of gesture, vocalization, and word use. Int. J. Speech Lang. Pathol. 2013, 15, 586–592. [Google Scholar] [CrossRef]
- Coufal, K.; Parham, D.; Jakubowitz, M.; Howell, C.; Reyes, J. Comparing Traditional Service Delivery and Telepractice for Speech Sound Production Using a Functional Outcome Measure. Am. J. Speech Lang. Pathol. 2018, 27, 82–90. [Google Scholar] [CrossRef] [PubMed]
- Sweeney, T.; Hegarty, F.; Powell, K.; Deasy, L.; O’ Regan, M.; Sell, D. Randomized control trial comparing Parent Led Therapist Supervised Articulation Therapy (PLAT) with routine intervention for children with speech sound disorders associated with cleft palate. Int. J. Lang. Commun. Disord. 2020, 55, 639–660. [Google Scholar] [CrossRef] [PubMed]
- Kratochwill, T.R.; Hitchcock, J.; Horner, R.H.; Levin, J.R.; Odom, S.L.; Rindskopf, D.M.; Shadish, W.R. Single-Case Designs Techincal Documentation; What Works Clearinghouse: Washington, DC, USA, 2010. Available online: http://ies.ed.gov/ncee/wwc/pdf/wwc_scd.pdf (accessed on 23 September 2019).
- Kratochwill, T.R.; Levin, J.R.; Horner, R.H.; Swoboda, C.M. Visual analysis of single-case intervention research: Conceptual and methodological issues. In Single-Case Intervention Research: Methodological and Statistical Advamces; Kratochwill, T.R., Levin, J.R., Eds.; American Psychological Association: Washington, DC, USA, 2014; pp. 91–125. [Google Scholar]
- Byiers, B.J.; Reichle, J.; Symons, F.J. Single-Subject Experimental Design for Evidence-Based Practice. Am. J. Speech Lang. Pathol. 2012, 21, 397–414. [Google Scholar] [CrossRef] [Green Version]
- Byun, T.M.; Hitchcock, E.R.; Ferron, J. Masked Visual Analysis: Minimizing Type I Error in Visually Guided Single-Case Design for Communication Disorders. J. Speech-Lang. Hear. Res. 2017, 60, 1455–1466. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zoom Video Communications, Inc. ZOOM Cloud Meetings. 2020. Available online: https://apps.apple.com/us/app/zoom-cloud-meetings/id546505307 (accessed on 1 October 2019).
- LENATM Recorder. Understanding LENA Technology. 2021. Available online: https://www.lena.org/technology/ (accessed on 21 August 2021).
- Bayley, N. Bayley Scales of Infant and Toddler Development, 3rd ed.; Pearson: San Antonino, TX, USA, 2006. [Google Scholar]
- Fenson, L.; Marchman, V.A.; Thal, D.J.; Dale, P.S.; Reznick, J.S.; Bates, E. MacArthur-Bates Communicative Development Inventories, 2nd ed.; Brookes: Baltimore, MD, USA, 2007. [Google Scholar]
- Zimmerman, I.L.; Steiner, V.G.; Pond, R.A. The Preschool Language Scale-5; Pearson: San Antonio, TX, USA, 2011. [Google Scholar]
- Stoel-Gammon, C.; Williams, A. Early phonological development: Creating an assessment test. Clin. Linguist. Phon. 2013, 7, 278–286. [Google Scholar] [CrossRef]
- McLeod, S.; Harrison, L.J.; McCormack, J. Intelligibility in Context Scale; Charles Sturt University: Bathurst, Australia, 2012; Available online: http://www.csu.edu.au/research/multilingual-speech/ics (accessed on 1 October 2019).
- Miller, J.; Chapman, R. SALT: Systematic Analysis of Language Transcripts; University Park Press: Baltimore, MD, USA, 2008. [Google Scholar]
- Parker, R.I.; Vannest, K.J.; Davis, J.L.; Sauber, S.B. Combining Nonoverlap and Trend for Single-Case Research: Tau-U. Behav. Ther. 2011, 42, 284–299. [Google Scholar] [CrossRef]
- Law, J.; Kot, A.; Barnett, G. A comparison of Two Methods for Providing Intervention to Three Year Old Children with Expressive/Receptive Language Impairment; City University of London: London, UK, 1999; Unpublished Report to NHS; Available online: http://eresearch.qmu.ac.uk/422/ (accessed on 3 June 2021).
- Frey, J.R.; Kaiser, A.P.; Scherer, N.J. The Influences of Child Intelligibility and Rate on Caregiver Responses to Toddlers with and without Cleft Palate. Cleft-Palate Craniofacial J. 2018, 55, 276–286. [Google Scholar] [CrossRef]




| Measure | Child 1 | Child 2 | Child 3 | Non-Cleft Comparison |
|---|---|---|---|---|
| Gender | F | M | M | F |
| Age at Pre-Intervention Assessment | 2;03 | 1;9 | 1;10 | 2;03 |
| Cleft Type | Unilateral cleft lip and palate | Bilateral cleft lip and palate | Unilateral cleft lip and alveolar notch | - |
| Age at Lip Repair | 5 months | 6 months | 7 months | - |
| Age at Palate Repair | 11 months | 10 months | - | - |
| Additional Conditions | Hemifacial microsomia | Glanzmann Thrombasthenia, palatal fistula | - | - |
| Hearing Status | WNL | WNL | WNL | WNL |
| Mother Demographics | ||||
| Age | 35 | 33 | 39 | 35 |
| Education Level | Some college | Bachelor’s Degree | Master’s Degree | Some college |
| Occupation | Retail manager | Stay at home mom | Stay at home mom | Retail manager |
| Name: | Reviewer: | |||||
|---|---|---|---|---|---|---|
| Video Session: | ||||||
| Item | 0 | 1 | 2 | 3 | ||
| Pull it all together | ||||||
| The environment provides physical boundaries and contains age-appropriate toys. Environmental Arrangement | ||||||
| Materials can be used to elicit multiple types of conversation and play (e.g., books, block with trucks, routines for snacks or group times). Environmental Arrangement | ||||||
| The parent is responsive to the child’s interests (i.e., joins in activities, is positive and energetic, is physically accessible, is at child’s level). Matched Turns | ||||||
| Time delays are used when the child requests nonverbally or with minimal verbalizations. Prompting | ||||||
| Models include the child’s targets. Models, Speech Recasting | ||||||
| Provide a question or a model with “say X,” if the child does not respond to the initial time delay. Models, Prompting | ||||||
| Praise all correct requests, responses, and behaviors. Matched Turns | ||||||
| Uses choice questions during session to elicit child targets. Prompting | ||||||
| Adult language, including expansions, do not exceed 2–3 words longer than child’s MLU). Expansions | ||||||
| Uses open-ended questions (i.e., “Tell me what you want?”, “What do you want to do?”). Prompting | ||||||
| Expansions preserve as much of the child utterance as possible. Expansions | ||||||
| The adult emphasizes the target sound in the word the child produced incorrectly when recasting. Speech Recasting | ||||||
| Overall rating of EMT + PE strategies throughout video | ||||||
| Parent | Measure | PND (%) | PND | Tau | Tau | CI 90% | Tau Qualitative Interpretation |
|---|---|---|---|---|---|---|---|
| p-Value | p-Value | ||||||
| 1 | Phase 1 | 75 | 0.0319 | 0.9 | 0.0275 | 0.228<>1 | Effective |
| Phase 2 | 100 | 0.0111 | 1.1333 | 0.0113 | 0.398<>1 | Very effective | |
| Phase 3 | 100 | 0.0014 | 1.1 | 0.0026 | 0.499<>1 | Very Effective | |
| 2 | Phase 1 | 100 | 0.0025 | 0.84 | 0.0283 | 0.210<>1 | Effective |
| Phase 2 | 100 | 0.0025 | 0.75 | 0.0372 | 0.398<>1 | Effective | |
| Phase 3 | 100 | 0.0111 | 1 | 0.0253 | 0.264<>1 | Very Effective | |
| 3 | Phase 1 | 40 | 0.0902 | 0.675 | 0.0283 | 0.113<>1 | Effective |
| Phase 2 | 100 | 0.0003 | 0.9111 | 0.0372 | 0.398<>1 | Effective | |
| Weighted Average | Phase 1 | - | - | 0.7979 | 0.0003 | 0.4384<>1 | Effective |
| Phase 2 | - | - | 0.9173 | 0 | 0.5532<>1 | Effective | |
| Phase 3 | - | - | 1.0551 | 0.0003 | 0.5802<>1 | Very effective |
| Measure | Assessment | Child 001 | Child 002 | Child 003 | |||
|---|---|---|---|---|---|---|---|
| Pre-Intervention | Post-Intervention | Pre-Intervention | Post-Intervention | Pre-Intervention | Post-Intervention | ||
| PCC Total | Profiles of Early Expressive Phonological Skills (PEEPS) [35] | 30.6% | 66.2% | 9% | 37.8% | 7.7% | 14.3% |
| PCC Stops | 44% | 74.4% | 9.3% | 31.4% | 20% | 40% | |
| Consonant inventory in the initial position of words | p, b, t, d, k, g, f, m, n, l, w, h, j, ʔ, ʕ | p, b, t, d, k, g, f, ∫, t∫, dʒ, m, n l, w, h, ʔ | b, k, m, n, ʔ | p, b, m, n, w, ʔ, , j | 0 | b, d, h | |
| Consonant inventory in the final position of words WSM ACM | p, t, s, n, ŋ, ʔ 18.6% 3.4% | p, t, d, k, g, θ, f, s, z, ∫, n, ŋ, l, r 71.7% 38.3% | k, l, ʔ, 9.3% 0% | p, t, k, f, n, l, r, ʔ, 37.8% 6.7% | t, h 0% 0% | p, t, h 0% 0% | |
| Expressive Communication Standard Score | Preschool Language Scales (PLS-5) [34] | 88 | 103 | 94 | - | 88 | - |
| Auditory Comprehension Standard Score | 106 | 104 | 117 | - | 88 | - | |
| ICS Average Score | Intelligibility in Context Scale (ICS) [36] | 2.67 Rarely-to-sometimes | 3.57 Sometimes-to-usually | 2.71 Rarely-to-sometimes | 3.71 Sometimes-to-usually | 2 Rarely | 2.29 Rarely |
| MCDI Words Produced | McArthur Bates Communicative Development Inventory (CDI) [33] | 233 | 532 | 70 | 161 | 2 | 22 |
| Percentile | 15 | 40 | 35 | 30–35 | <5 | <5 | |
| MCDI Word Forms | 1/25 | 11/25 | 0/25 | 1/25 | 0/25 | 0/25 | |
| Percentile | 5–10 | 15–20 | 55 | 30 | 35 | 10 | |
| MCDI Complexity | 2/37 | 22/37 | 0/37 | 0/37 | 0/37 | 0/37 | |
| Percentile | 20 | 69 | 70 | 30 | 55 | 30 | |
| NDW | Language Sample | 37 | 63 | 14 | 34 | 2 | 9 |
| MLUm | 1.26 | 2.07 | 1.38 | 1.10 | 1.19 | 1.15 | |
| TNW | 86 | 208 | 36 | 88 | 19 | 23 | |
| WPM | 8.67 | 21.82 | 4.43 | 7.37 | 5.3 | 7.36 | |
| Cognitive Scaled Score (Pre-test only) | Bayley Scales of Infant Development—III [32] | 10 | - | 10 | - | 7 | - |
| Cognitive Percentile Score | 50% | - | 50% | - | 16% | - | |
| Measure | Assessment | Non-Cleft Comparison | |
|---|---|---|---|
| Pre-Intervention | Post-Intervention | ||
| PCC Total | Profiles of Early Expressive Phonological Skills (PEEPS, Stoel-Gammon, 2013) [35] | 83.6% | 81.2% |
| PCC Stops | 95.8% | 84.5% | |
| Consonant Inventory in the Initial Position of Words | p, b, m, w, f, t, d, s, n, k, g, h, ∫ | p, b, m, w, f, t, d, s, z, n, l, k, g, h, θ | |
| Consonant Inventory in the Final Position of Words WSM ACM | p, m, f, θ, t, d, s, z, n, l, t∫, k, g 83.6% 67.3% | p, b, m, f, t, d, s, n, l, k, g, t∫, ŋ 79.7% 59.3% | |
| Expressive Communication Standard Score | Preschool Language Scales (PLS-5, Zimmerman et al., 2011) [34] | 110 | - |
| Auditory Comprehension Standard Score | 124 | - | |
| ICS Average Score | Intelligibility in Context Scale (ICS, McLeod, Harrison, and McCormack, 2012a) [36] | 4.17 Usually | - - |
| MCDI Words Produced | McArthur Bates Communicative Development Inventory (CDI, Fenson et al., 2007) [33] | 413 | - |
| Percentile | 35–40 | - | |
| MCDI Word Forms | 14/25 | - | |
| Percentile | 70 | - | |
| MCDI Complexity | 22/37 | - | |
| Percentile | 55–60 | - | |
| NDW | Language Sample | 76.5 | 68 |
| MLUm | 1.71 | 2.01 | |
| TNW | 234 | 160 | |
| WPM | 15.50 | 10.68 | |
| Cognitive Scaled Score (Pre-Test Only) | Bayley Scales of Infant Development—III (Bayley, 2006) [32] | 9 | |
| Cognitive Percentile Score | 37 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Philp, J.; Ellis, P.K.; Scherer, N.J.; Lien, K.M. Enhanced Milieu Teaching with Phonological Emphasis: A Pilot Telepractice Parent Training Study for Toddlers with Clefts. Children 2021, 8, 736. https://doi.org/10.3390/children8090736
Philp J, Ellis PK, Scherer NJ, Lien KM. Enhanced Milieu Teaching with Phonological Emphasis: A Pilot Telepractice Parent Training Study for Toddlers with Clefts. Children. 2021; 8(9):736. https://doi.org/10.3390/children8090736
Chicago/Turabian StylePhilp, Jennifer, Paige K. Ellis, Nancy J. Scherer, and Kari M. Lien. 2021. "Enhanced Milieu Teaching with Phonological Emphasis: A Pilot Telepractice Parent Training Study for Toddlers with Clefts" Children 8, no. 9: 736. https://doi.org/10.3390/children8090736
APA StylePhilp, J., Ellis, P. K., Scherer, N. J., & Lien, K. M. (2021). Enhanced Milieu Teaching with Phonological Emphasis: A Pilot Telepractice Parent Training Study for Toddlers with Clefts. Children, 8(9), 736. https://doi.org/10.3390/children8090736





