Abstract
This study aimed to report the surgical outcomes of laparoscopic glue hernioplasty (LGH) compared with conventional laparoscopic suture hernioplasty (LSH) in pediatric female inguinal hernia repair. We retrospectively analyzed 465 female pediatric patients who underwent laparoscopic inguinal hernia repair between January 2013 and December 2020. LGH and LSH were performed in 95 and 370 cases, respectively. Surgical outcomes (length of hospital stay, operative time, complications, and recurrences) were compared between the LGH and LSH groups. We found that the operation times for bilateral hernia repair were shorter in the LGH group (LGH: 35.5 ± 8.2 min, LSH: 45.2 ± 11.6 min; p < 0.001). No significant differences in complications or recurrences were observed between the two groups during the follow-up period. Our findings suggest that LGH is a feasible and easily applied surgical technique for the treatment of pediatric female inguinal hernia.
1. Introduction
Inguinal hernia is one of the most common pediatric surgical diseases [1]. With modern advancements in anesthesia and surgical instrument refinements, laparoscopic hernioplasty has become a popular choice for pediatric surgeries [2,3]. According to a recent meta-analysis of evidence from the last 10 years, the recurrence rates for laparoscopic and open inguinal hernia repair are similar (odds ratio [OR] 1.05, p = 0.66) [4]. The recurrence rates for inguinal hernia repair are lower in children than in adults, ranging from 0.5 to 4% [5], while those following laparoscopic repair range from 0.7 to 4.5% [6].
However, there is still an ongoing debate about the best approach and the advantages and disadvantages of intracorporeal [7,8] and extracorporeal methods [9,10]. Both surgical methods involve suturing for the closure of the internal inguinal ring. Unfortunately, the correct placing of the internal inguinal suturing is difficult and requires laparoscopic surgical skills. The intracorporeal method typically requires a surgeon who is highly skilled in laparoscopy to suture the inguinal ring and tie the knots. Recently, percutaneous internal ring suturing (PIRS), which represents a kind of extracorporeal method, has been developed [11,12,13]. As conversion rates have been reported to reach a plateau after surgeons have performed at least 30 procedures [14,15], PIRS has been spotlighted by some pediatric surgeons as a technically easier, safe, and effective approach for pediatric hernia repair. However, extracorporeal methods require an extra incision, and some procedures can only be performed with specially designed instruments [10]. In addition, adverse events associated with extraperitoneal knotting, such as infection, pain, blood vessel injury, and a palpable thread knot around the inguinal area of the abdominal wall, might occur with extracorporeal methods [16,17].
To overcome these limitations, using glue as a tissue adhesive has been proposed as an alternative to conventional laparoscopic inguinal hernioplasty [18]. In 1835, Velpeau observed an inguinal hernia that was cured by the accidental introduction of iodine into the inguinal canal during the injection of a hydrocele [19]. Since then, glue has been used internally and externally on the human body [20,21,22]. Previously, the effectiveness and safety of laparoscopic glue hernioplasty (LGH) were evaluated in a series of animal studies [18,23,24]. Here, we report our single-institution experience, which provides evidence that the LGH technique is effective in treating inguinal hernia in pediatric female patients [25]. However, so far, there are no reports on how LGH results compare to conventional laparoscopic suture hernioplasty (LSH). Thus, this study aimed to compare the surgical outcomes of LGH with those of conventional LSH in the treatment of pediatric female inguinal hernias.
2. Materials and Methods
2.1. Patients
We retrospectively analyzed the medical records of patients with inguinal hernias who were treated at Severance Children’s Hospital between January 2013 and December 2020. Inclusion criteria were (i) aged 0 to 18 years and (ii) female sex. Exclusion criteria were (i) older than 18 years of age and (ii) a combination surgery including another procedure. The choice of surgical method was surgeon-dependent, and determined by the surgeon’s experience, beliefs, and confidence in their skills to perform a certain technique. Ultimately, 465 patients were included in the study. LGH was performed in 95 cases and LSH in 370; accordingly, the patients were divided into an LGH and an LSH groups. This study was reviewed and approved by the Institutional Review Board of Yonsei University Health System, Severance Hospital (approval date: 27 January 2021; approval No. 4-2020-1368). The requirement for informed consent was waived because of the retrospective design of the study.
2.2. Outcome Measurements
The primary outcome of the study was to evaluate surgical outcomes regarding operation time, complication, and recurrence. The secondary outcome was to compare the surgical outcomes of the two groups and confirm the novel surgical method–(LGH)’s safety and efficiency. A further follow-up evaluation was performed through a telephonic survey.
2.3. Statistical Analysis
All data were analyzed using IBM® SPSS® Statistics version 25 (IBM, Armonk, NY, USA). Two-sample t-tests, chi-squared tests, and the Mann–Whitney U test were used to analyze the data; p-values < 0.05 were considered statistically significant.
2.4. Surgical Techniques
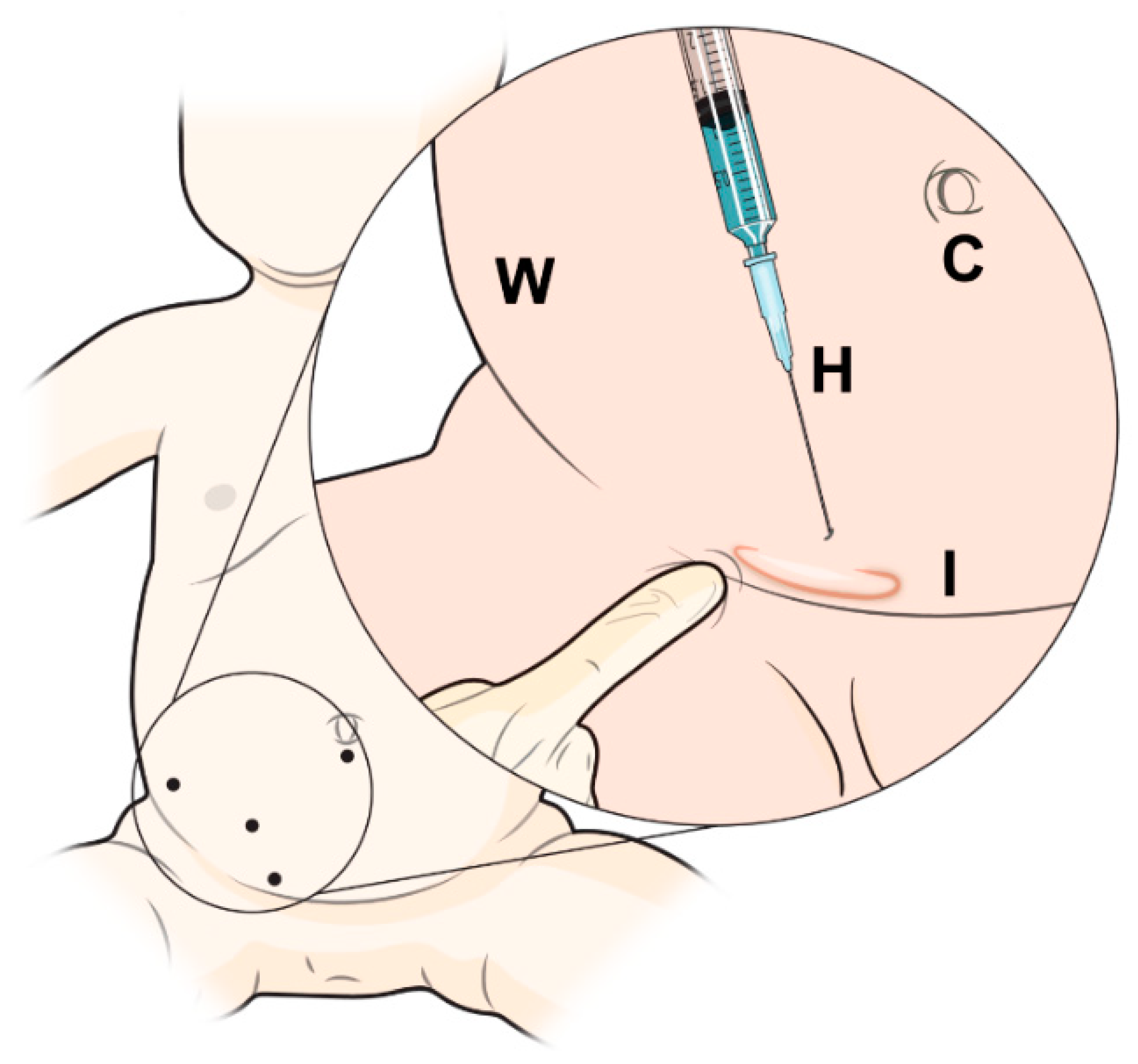
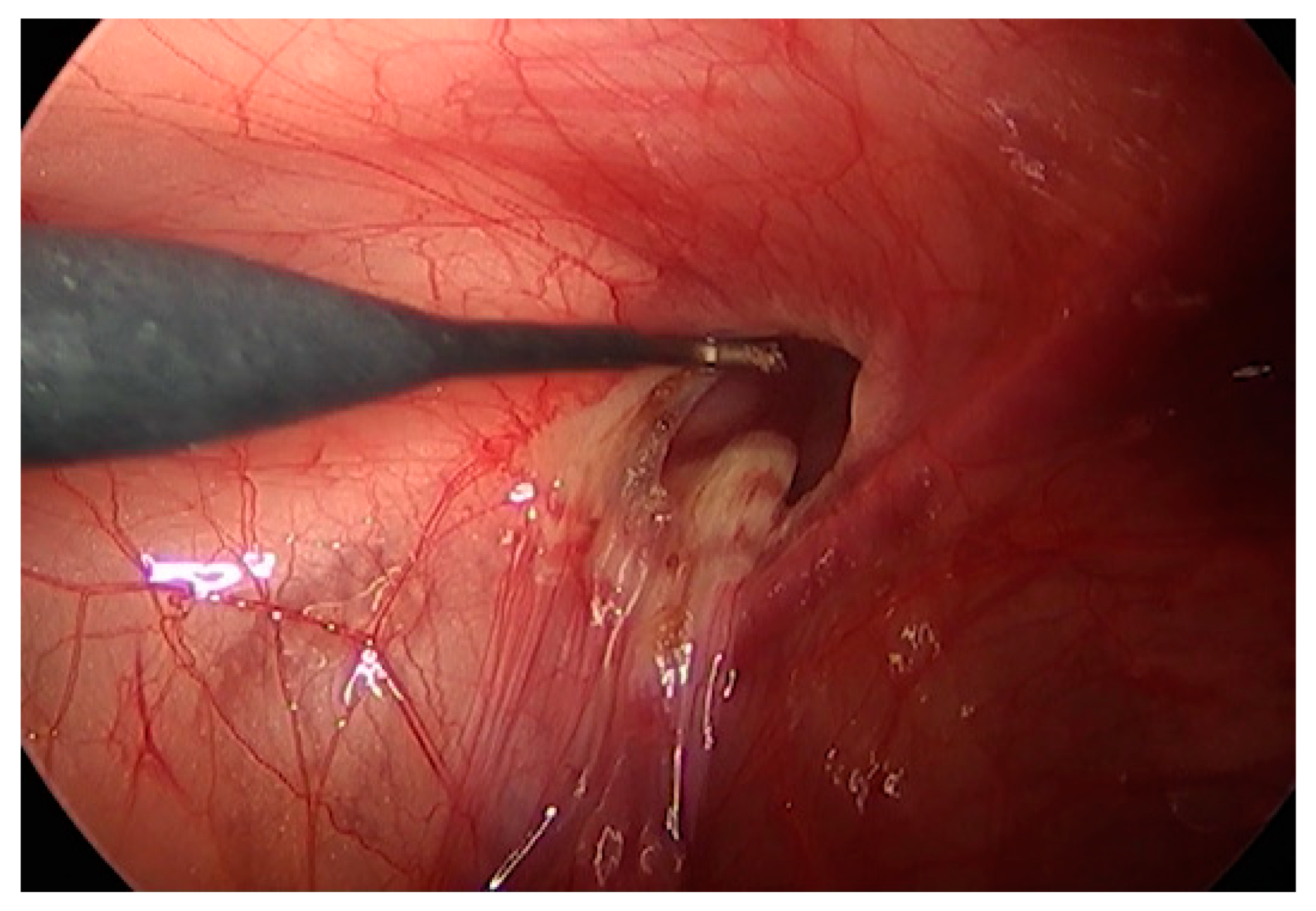
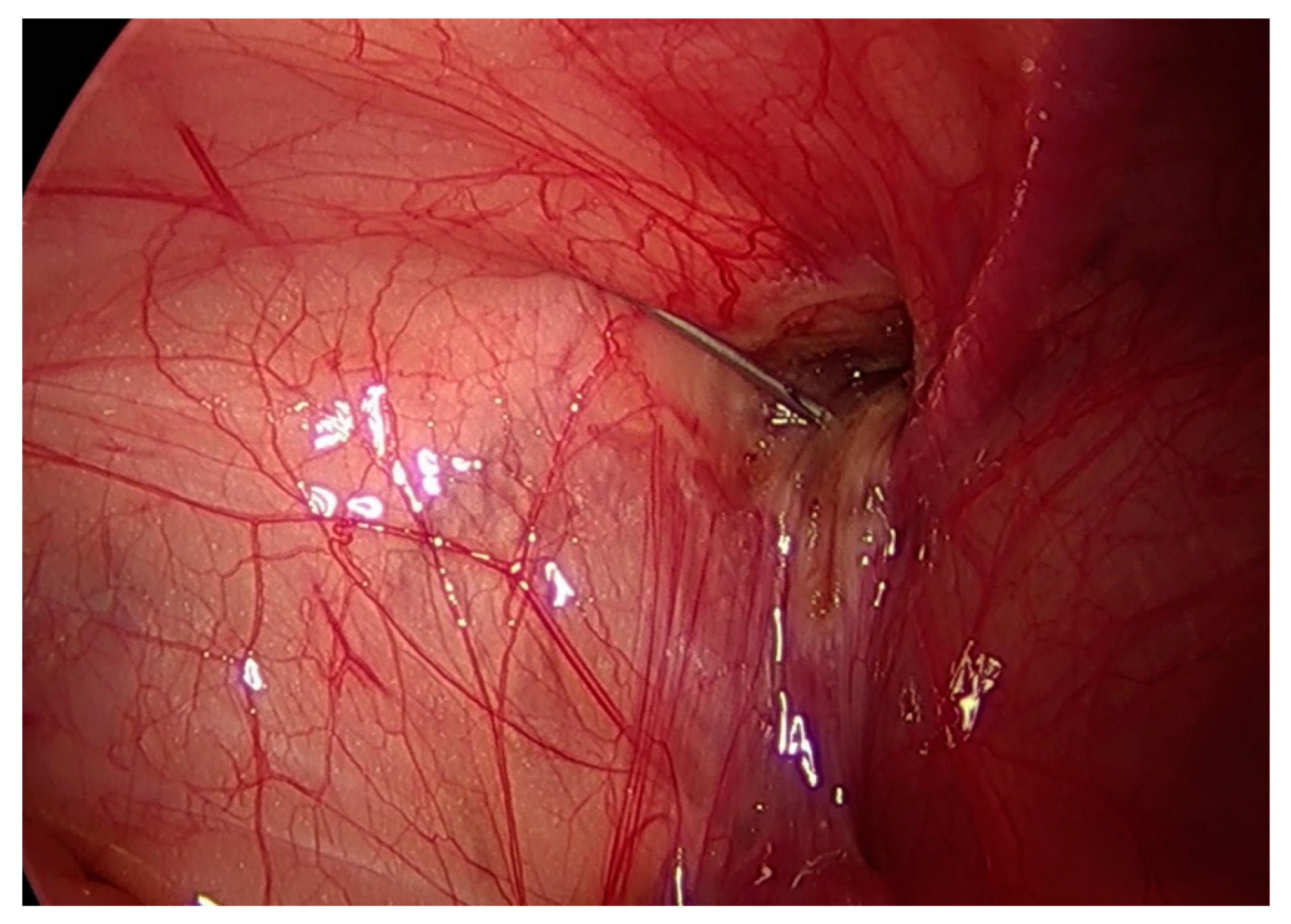
We adopted the previously published techniques of LGH [25] and LSH [8]. All procedures were performed while the patients were under general anesthesia. After the trocars were introduced, a pneumoperitoneum was created with a resulting intraabdominal pressure of 5–12 mmHg. For the LSH procedure, three trocars were used: a 5 mm optical trocar was inserted through the umbilicus, and two 3 mm trocars were inserted lateral to the rectus abdominis muscle, slightly below the level of the umbilicus. The mesothelial layer surrounding the internal inguinal ring was electrically cauterized, the peritoneum was circumferentially divided at the level of the internal inguinal ring, and the hernia ring was ligated using purse-string sutures with a 3-0 non-absorbable suture (3-0 Ethibond Excel, Ethicon, Somerville, NJ, USA) (Online Resource S1: laparoscopic suture hernioplasty). For LGH, two trocars were used: a 5 mm camera port was inserted through the umbilicus and a 3 mm instrument working port was inserted lateral to the rectus abdominis muscle. The internal inguinal ring was divided in the same way as during LSH; following electrical cauterization, the internal inguinal ring was narrowed by applying external pressure through finger pushing (Figure 1 and Figure 2). A long, 25-gauge needle attached to a 1 mL syringe filled with N-butyl-2-cyanoacrylate (b-can; Histoacryl®; B. Braun, Melungeon, Germany) was then inserted into the peritoneal cavity, 2–3 cm above the targeted internal inguinal ring. The injection of 0.5–1 mL of Histoacryl® was generally sufficient to close the internal inguinal ring (Figure 3). The peritoneum was held in place until the Histoacryl® hardened, after approximately 4–5 s. The closure of the internal ring was then confirmed by probing with the laparoscopic instrument (Online Resource S2: laparoscopic glue hernioplasty).
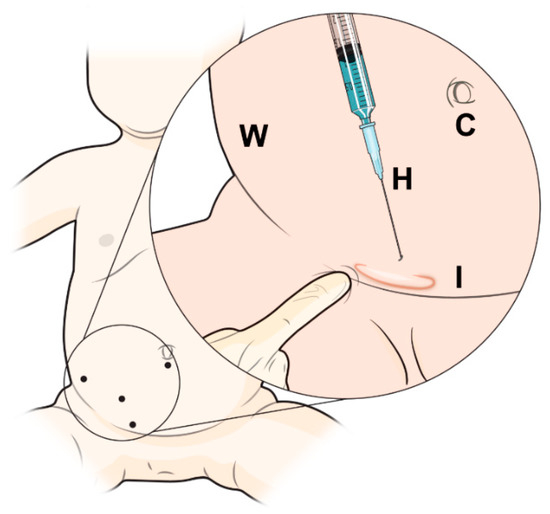
Figure 1.
Schematic image of laparoscopic glue hernioplasty. C: Camera, W: Abdomen wall, H: Histoacryl®, I: Inguinal ring.
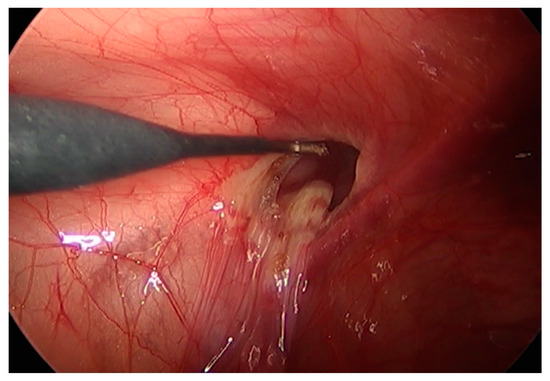
Figure 2.
The mesothelial layer surrounding the internal ring was electrically cauterized.
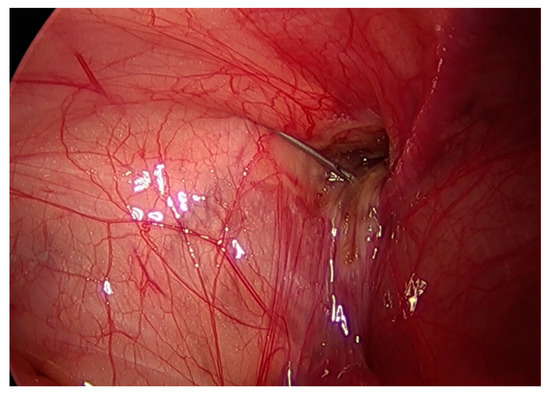
Figure 3.
Histoacryl® was injected and a long 25-gauge needle was used to close the internal inguinal ring.
3. Results
3.1. Demographics
The clinical characteristics of the patients are shown in Table 1.

Table 1.
Characteristics of patients.
The median age at the time of surgery was 45 months (range: 1–138 months) in the LGH group and 48 months (range: 0–188 months) in the LSH group (p = 0.063). The mean body weight at the time of surgery was 15.6 ± 7.19 kg in the LGH group and 15.5 ± 8.9 kg in the LSH group (p = 0.065). There were no statistically significant differences in age or weight at the time of surgery between the two groups. Lateralization in the LGH group was 25 (right) and 33 (left), compared to 110 (right) and 82 (left) in the LSH group. There were 37 LGH and 178 LSH bilateral hernia repairs. There were no significant differences in the type of surgery performed between the two groups (p = 0.058 and p = 0.11).
3.2. Operative Time
The summarized surgical outcomes are shown in Table 2.

Table 2.
Surgical outcomes.
With respect to the mean operative time for the repair of unilateral inguinal hernias, there was no significant difference between the LGH and LSH groups (LGH: 32.2 ± 15.4 min, LSH: 37.5 ± 12.4 min; p = 0.26). However, the mean operative time for the repair of bilateral inguinal hernias was shorter for the LGH than for the LSH group (LGH: 35.5 ± 8.2 min, LSH: 45.2 ± 11.6 min; p < 0.001).
3.3. Length of Hospital Stay
Most patients were discharged on the day of their surgery or 1 day after the surgery. There was no significant difference between the two groups in this regard (LGH: 1.06 ± 1.05 days, LSH: 0.93 ± 0.99 days; p = 0.412).
3.4. Follow-Up and Recurrence
There were two recurrence cases in the LGH group and none in the LSH group during the follow-up (LGH: 124.7 ± 61.2 months, LSH: 102.8 ± 61.1 months; p = 0.433). However, there was no significant difference between the two groups (p = 0.062).
3.5. Postoperative Complications
In the LGH group, postoperative wound infection in the umbilical trocar insertion site occurred in three patients. In the LSH group, postoperative wound infection occurred in four patients and postoperative ileus occurred in two patients. The cause of the ileus was paralytic ileus after surgery, and the patients recovered after conservative treatment. There was no significant difference between the two groups (p = 0.332).
4. Discussion
In this study, we assessed the outcomes of a novel surgical technique (LGH) and compared them to those of the conventional surgical method (LSH) for pediatric inguinal hernia repair in female patients. We found shorter operation times for LGH bilateral hernioplasty and good cosmetic effects compared to conventional LSH.
Minimally invasive surgery has been the major revolutionary change in many conventional surgical procedures, and has resulted in a remarkable reduction in morbidity [26,27,28]. After the introduction of laparoscopic hernia repair, the paradigm of pediatric inguinal hernia treatment has changed to laparoscopic surgery as an alternative to the existing open inguinal hernia repair approach [2,3,29]. Various laparoscopic surgical methods have been developed that can be classified into two major approaches: intracorporeal [7,8] and extracorporeal [15,30] methods.
Advantages of laparoscopic inguinal hernia repair have been reported, such as the ability to evaluate the contralateral side, avoid excess trauma to the spermatic cord structures, iatrogenic cryptorchidism, testicular atrophy, as well as less postoperative pain [31]. However, over the last decade, the laparoscopic technique for inguinal hernia repair in children has not undergone major technical advances [3,13,32]. The existing laparoscopic surgical technique has some disadvantages regarding the closing of the internal inguinal ring. Intracorporeal methods require advanced laparoscopic skills, and are technically challenging and time consuming [3]. Recently, percutaneous internal ring suturing (PIRS) procedures, which represent a kind of extracorporeal method, have been developed; these techniques are technically easier to implement than intracorporeal methods, and lead to lower recurrence rates and shorter operation times [11]. In addition, they have been reported as safe and effective not only for young children, but also for young adolescent patients [33], and have, thus, been spotlighted by some pediatric surgeons. However, extracorporeal methods require an extra incision, and some can only be conducted with specially designed instruments. In addition, adverse events associated with extra peritoneal knotting, such as infection, pain, and a palpable thread knot around the inguinal area of the abdominal wall, have been reported for extracorporeal methods [16,17]. These issues have limited the widespread use of such methods in pediatric surgical practice. Ideally, an advanced technique of laparoscopic inguinal hernia repair should be simple and easy to adopt, and not come with the above limitations.
To overcome these challenges, the use of glue in combination with a laparoscopic surgical technique has been developed and published as an attractive, easy, and reproducible technique [18,19,24,25]. Various studies have reported on surgical glue injection into the human body, and there has been much discussion about the safety and efficacy of this approach [21,22,34].
Cyanoacrylates (CNAs) were developed in the 1960s and 1970s. Short-chain CNAs were found to be toxic to human tissue and to cause tissue necrosis. Conversely, long-chain CNAs, such as b-CNA and 0-CNA, are degradable and can be used in humans, without adverse effects [35]. In the pediatric surgery field, glue has been used to reduce the risk of postoperative complications, especially in cases of parenchymal resection or vascular anastomosis [36,37]. Glue has also been applied in pediatric laparoscopic surgery as a good means of controlling bleeding, particularly in cases of spleen or liver bleeding, and is a valid method for completing and securing sutures in cases of organ perforation [34].
One important characteristic of b-CNA (Histoacryl®) is that when it comes into contact with a liquid, it is polymerized through an exothermic reaction to form a strong bond. However, it produces heat during the polymerization process, releases toxic products that inhibit cell growth, and is not completely biodegradable. Therefore, potential concerns related to Histoacryl® use include the possibility of a foreign body response and tissue damage from the exothermic reaction during polymerization [38]. Adverse effects related to these characteristics of b-CNA, such as mild chronic inflammation and obstruction due to tissue adhesion and tissue toxicity, have been reported during long-term follow-ups after intraperitoneal interventions [39,40].
For this reason, and considering that not much has been reported on the stability of glue, our study only included female patients to avoid potential damage to the vas deferens. In previous studies, Kato and Ayman reported that the use of glue was effective in the repair of inguinal hernia, with no recurrence on long-term follow-up, no damage to spermatic cord structures, and no clear impact on fertility [18,41]. Similarly, in our study, the glue was partially absorbed after LGH, which was confirmed by a second surgery due to ovarian torsion, where the glue injection site remained completely closed, without any intraperitoneal organ adhesion [42]. In contrast, Miyano et al. reported concerns on the increased risk of intestinal obstruction by adhesive syndrome, hernia recurrence, postoperative hydrocele, and long-term carcinogenesis [24]. Recently, Maria et al. published a comparative study on the laparoscopic injection of tissue adhesives and standard laparoscopic suture inguinal hernia repair in a male rabbit model. The authors describe several critical issues that are associated with a higher incidence of postoperative complications and a significant decrease in testicular maturity in tissue adhesive models [43].
As an alternative, we are focusing on bioinspired tissue adhesives going forward. These adhesives were developed recently [44] and are receiving attention as potential biomedical materials in various clinical fields [45,46]. Mussel adhesive proteins (MAPs) have been considered as a potential bio-adhesive, due to their unique features [47,48]. MAPs are able to maintain their adhesion in a wet environment, and such water-immiscible mussel adhesives have potential diverse biotechnological applications, such as cell and tissue adhesives. They also have the advantage of being biodegradable, with less toxicity [49,50]. More advanced MAPs are currently being developed, based on recombinant DNA and bioengineering technology. According to recent research based on animal experiments, regenerative bio-glue leads to better results and reduces foreign body reactions in the treatment of vesico-vaginal fistula, compared with existing glue and surgical suture repair [51]. Therefore, MAPs can be used as medical adhesives as they are harmless to the human body. In the future, through animal experiments, we will further research the safety and efficacy of bioinspired adhesives, specifically MAPs, in the treatment of pediatric inguinal hernias.
Our study provides important findings regarding the use of LGH. We found significantly shorter operative times for LGH than for LSH in bilateral hernia repair, and no significant difference in surgical complications or recurrence rates. Additionally, LGH requires only two laparoscopic ports, which makes it superior to conventional LSH, not only in terms of its easy adoption, but also its better cosmetic outcomes. Similar to our findings, a previous study reported that patients who underwent laparoscopic inguinal hernia repair exhibited lower levels of pain and inflammatory stress responses than those treated with an open approach [52]. Therefore, in our study, we assume that LGH is the less invasive and easier operation, and it reduces surgery-related stress for the patient.
These advantages are considered to provide a significant benefit to surgeons who are not experts in laparoscopic surgery. In low- and middle-income countries, pediatric inguinal hernia is still a major cause of morbidity and mortality, yet elective surgical treatment remains largely unavailable [53,54]. The development of such an easy surgical method is, thus, regarded to be a great help in the treatment of pediatric inguinal hernia in developing countries.
The results of this study show that, compared with conventional LSH, LGH is technically easy, reproducible, has a shorter operating time, and does not require advanced laparoscopic skills; therefore, it can be easily applied in the treatment of pediatric female inguinal hernia. The limitations of our study include the absence of male patients, the fact that it was a single-center study, and the retrospective study design, which makes it difficult to extrapolate our findings to the entire pediatric population. Moreover, the safety of the glue is still controversial. Further research regarding the stability and safety of bioinspired adhesives in the treatment of pediatric inguinal hernia is warranted.
Supplementary Materials
The following are available online at https://doi.org/10.5281/zenodo.6475697: Online Resource S1: laparoscopic suture hernioplasty; Online Resource S2: laparoscopic glue hernioplasty.
Author Contributions
S.J.H. contributed to the study conception and design. Material preparation, data collection and analysis were performed by K.I., H.J.J., D.L. and Y.N. The first draft of the manuscript was written by I.G.H., and all authors commented on previous versions of the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and the study protocol was approved by the Institutional Review Board of Severance Hospital (IRB approval No. 4-2020-1368).
Informed Consent Statement
Patient consent was waived because of the retrospective nature of the study and the use of anonymous clinical data.
Data Availability Statement
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
The authors thank Medical Illustration & Design, part of the Medical Research Support Services of Yonsei University College of Medicine, for all artistic support related to this work.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study, in the collection, analyses, or interpretation of data, in the writing of the manuscript, or in the decision to publish the results.
References
- Esposito, C.; Escolino, M.; Turrà, F.; Roberti, A.; Cerulo, M.; Farina, A.; Caiazzo, S.; Cortese, G.; Servillo, G.; Settimi, A. Current concepts in the management of inguinal hernia and hydrocele in pediatric patients in laparoscopic era. Semin. Pediatr. Surg. 2016, 25, 232–240. [Google Scholar] [CrossRef] [PubMed]
- Parelkar, S.V.; Oak, S.; Gupta, R.; Sanghvi, B.; Shimoga, P.H.; Kaltari, D.; Prakash, A.; Shekhar, R.; Gupta, A.; Bachani, M. Laparoscopic inguinal hernia repair in the pediatric age group--experience with 437 children. J. Pediatric Surg. 2010, 45, 789–792. [Google Scholar] [CrossRef] [PubMed]
- Esposito, C.; Escolino, M.; Cortese, G.; Aprea, G.; Turrà, F.; Farina, A.; Roberti, A.; Cerulo, M.; Settimi, A. Twenty-year experience with laparoscopic inguinal hernia repair in infants and children: Considerations and results on 1833 hernia repairs. Surg. Endosc. 2017, 31, 1461–1468. [Google Scholar] [CrossRef] [PubMed]
- Bada-Bosch, I.; Escolino, M.; De Agustín, J.C.; Esposito, C. Pediatric inguinal hernia repair, laparoscopic versus open approach: A systematic review and meta-analysis of the last 10-year evidence. J. Laparoendosc. Adv. Surg. Tech. Part A 2022. [Google Scholar] [CrossRef] [PubMed]
- Pogorelić, Z.; Rikalo, M.; Jukić, M.; Katić, J.; Jurić, I.; Furlan, D.; Budimir, D.; Biočić, M. Modified marcy repair for indirect inguinal hernia in children: A 24-year single-center experience of 6826 pediatric patients. Surg. Today 2017, 47, 108–113. [Google Scholar] [CrossRef] [PubMed]
- Okunobo, T.; Nakamura, H.; Yoshimoto, S.; Satake, R.; Shigeta, Y.; Doi, T. The detail profile of cause of recurrences after laparoscopic percutaneous extraperitoneal closure (lpec) in children: A systematic review. Pediatr. Surg. Int. 2022, 38, 359–363. [Google Scholar] [CrossRef]
- Yip, K.F.; Tam, P.K.; Li, M.K. Laparoscopic flip-flap hernioplasty: An innovative technique for pediatric hernia surgery. Surg. Endosc. 2004, 18, 1126–1129. [Google Scholar] [CrossRef]
- Wheeler, A.A.; Matz, S.T.; Schmidt, S.; Pimpalwar, A. Laparoscopic inguinal hernia repair in children with transperitoneal division of the hernia sac and proximal purse string closure of peritoneum: Our modified new approach. Eur. J. Pediatr. Surg. 2011, 21, 381–385. [Google Scholar] [CrossRef]
- Harrison, M.R.; Lee, H.; Albanese, C.T.; Farmer, D.L. Subcutaneous endoscopically assisted ligation (seal) of the internal ring for repair of inguinal hernias in children: A novel technique. J. Pediatric Surg. 2005, 40, 1177–1180. [Google Scholar] [CrossRef]
- Laparoscopic closure of patent processus vaginalis in girls with inguinal hernia using a specially devised suture needle. Pediatric Endosurgery Innov. Tech. 2001, 5, 187–191. [CrossRef]
- Pogorelić, Z.; Čohadžić, T.; Jukić, M.; Nevešćanin Biliškov, A. Percutaneous internal ring suturing for the minimal invasive treatment of pediatric inguinal hernia: A 5-year single surgeon experience. Surg. Laparosc. Endosc. Percutan. Tech. 2021, 31, 150–154. [Google Scholar] [CrossRef] [PubMed]
- Patkowski, D.; Czernik, J.; Chrzan, R.; Jaworski, W.; Apoznański, W. Percutaneous internal ring suturing: A simple minimally invasive technique for inguinal hernia repair in children. J. Laparoendosc. Adv. Surg. Tech. Part A 2006, 16, 513–517. [Google Scholar] [CrossRef] [PubMed]
- Prasad, R.; Lovvorn, H.N., 3rd; Wadie, G.M.; Lobe, T.E. Early experience with needleoscopic inguinal herniorrhaphy in children. J. Pediatric Surg. 2003, 38, 1055–1058. [Google Scholar] [CrossRef]
- Barroso, C.; Etlinger, P.; Alves, A.L.; Osório, A.; Carvalho, J.L.; Lamas-Pinheiro, R.; Correia-Pinto, J. Learning curves for laparoscopic repair of inguinal hernia and communicating hydrocele in children. Front. Pediatr. 2017, 5, 207. [Google Scholar] [CrossRef]
- Pogorelić, Z.; Huskić, D.; Čohadžić, T.; Jukić, M.; Šušnjar, T. Learning curve for laparoscopic repair of pediatric inguinal hernia using percutaneous internal ring suturing. Children 2021, 8, 294. [Google Scholar] [CrossRef]
- Li, S.; Tang, S.T.; Aubdoollah, T.H.; Li, S.; Li, K.; Tong, Q.S.; Wang, Y.; Mao, Y.Z.; Cao, G.; Yang, L.; et al. A modified approach for inguinal hernias in children: Hybrid single-incision laparoscopic intraperitoneal ligation. J. Laparoendosc. Adv. Surg. Tech. Part A 2015, 25, 689–693. [Google Scholar] [CrossRef]
- Wang, Y.J.; Zhang, Q.L.; Chen, L.; Lin, Y.; Zhang, J.Q.; Wu, D.M.; Huang, W.H.; Zhou, C.M. Laparoscopic percutaneous extraperitoneal internal ring closure for pediatric inguinal hernia: 1,142 cases. J. Laparoendosc. Adv. Surg. Tech. Part A 2019, 29, 845–851. [Google Scholar] [CrossRef]
- Kato, Y.; Yamataka, A.; Miyano, G.; Tei, E.; Koga, H.; Lane, G.J.; Miyano, T. Tissue adhesives for repairing inguinal hernia: A preliminary study. J. Laparoendosc. Adv. Surg. Tech. Part A 2005, 15, 424–428. [Google Scholar] [CrossRef]
- Patterson, D.C. The injection treatment of hernia. Yale J. Biol. Med. 1936, 9, 159–166. [Google Scholar]
- Amiel, G.E.; Sukhotnik, I.; Kawar, B.; Siplovich, L. Use of n-butyl-2-cyanoacrylate in elective surgical incisions--longterm outcomes. J. Am. Coll. Surg. 1999, 189, 21–25. [Google Scholar] [CrossRef]
- Osman, M.A. Histoacryl injection in the management of fourth branchial fistula. Ann. Pediatric Surg. 2012, 8, 74–76. [Google Scholar] [CrossRef]
- Yoon, J.H.; Lee, H.L.; Lee, O.Y.; Yoon, B.C.; Choi, H.S.; Hahm, J.S.; Rhim, S.Y.; Jung, P.M. Endoscopic treatment of recurrent congenital tracheoesophageal fistula with histoacryl glue via the esophagus. Gastrointest. Endosc. 2009, 69, 1394–1396. [Google Scholar] [CrossRef] [PubMed]
- Kozlov, Y.; Novogilov, V.; Rasputin, A.; Podkamenev, A.; Krasnov, P.; Weber, I.; Solovjev, A. Laparoscopic inguinal preperitoneal injection--novel technique for inguinal hernia repair: Preliminary results of experimental study. J. Laparoendosc. Adv. Surg. Tech. Part A 2012, 22, 276–279. [Google Scholar] [CrossRef] [PubMed]
- Miyano, G.; Yamataka, A.; Kato, Y.; Tei, E.; Lane, G.J.; Kobayashi, H.; Sueyoshi, N.; Miyano, T. Laparoscopic injection of dermabond tissue adhesive for the repair of inguinal hernia: Short- and long-term follow-up. J. Pediatric Surg. 2004, 39, 1867–1870. [Google Scholar] [CrossRef]
- Park, S.M.; Shukri, N.; Chang, E.Y.; Ho, I.G.; Han, S.J. Laparoscopic surgical glue injection hernioplasty: A single-institution experience. J. Laparoendosc. Adv. Surg. Tech. Part A 2016, 26, 488–492. [Google Scholar] [CrossRef]
- Ghanbari, H.; Kidane, A.G.; Burriesci, G.; Bonhoeffer, P.; Seifalian, A.M. Percutaneous heart valve replacement: An update. Trends Cardiovasc. Med. 2008, 18, 117–125. [Google Scholar] [CrossRef]
- Calero, A.; Illig, K.A. Overview of aortic aneurysm management in the endovascular era. Semin Vasc Surg 2016, 29, 3–17. [Google Scholar] [CrossRef]
- Carnero-Alcázar, M.; Maroto, L.C.; Cobiella-Carnicer, J.; Vilacosta, I.; Nombela-Franco, L.; Alswies, A.; Villagrán-Medinilla, E.; Macaya, C. Transcatheter versus surgical aortic valve replacement in moderate and high-risk patients: A meta-analysis. Eur. J. Cardiothorac. Surg. 2017, 51, 644–652. [Google Scholar] [CrossRef]
- Brandt, M.L. Pediatric hernias. Surg. Clin. N. Am. 2008, 88, 27–43. [Google Scholar] [CrossRef]
- Shalaby, R.Y.; Fawy, M.; Soliman, S.M.; Dorgham, A. A new simplified technique for needlescopic inguinal herniorrhaphy in children. J. Pediatric Surg. 2006, 41, 863–867. [Google Scholar] [CrossRef]
- Schier, F.; Montupet, P.; Esposito, C. Laparoscopic inguinal herniorrhaphy in children: A three-center experience with 933 repairs. J. Pediatric Surg. 2002, 37, 395–397. [Google Scholar] [CrossRef] [PubMed]
- Montupet, P.; Esposito, C. Laparoscopic treatment of congenital inguinal hernia in children. J. Pediatric Surg. 1999, 34, 420–423. [Google Scholar] [CrossRef]
- Pogorelić, Z.; Batinović, T.; Jukić, M.; Šušnjar, T. Percutaneous internal ring suturing is a safe and effective method for inguinal hernia repair in young adolescents. J. Laparoendosc. Adv. Surg. Tech. Part A 2022, 32, 452–457. [Google Scholar] [CrossRef] [PubMed]
- Esposito, C.; Damiano, R.; Settimi, A.; De Marco, M.; Maglio, P.; Centonze, A. Experience with the use of tissue adhesives in pediatric endoscopic surgery. Surg. Endosc. 2004, 18, 290–292. [Google Scholar] [CrossRef] [PubMed]
- Vinters, H.V.; Galil, K.A.; Lundie, M.J.; Kaufmann, J.C. The histotoxicity of cyanoacrylates. A selective review. Neuroradiology 1985, 27, 279–291. [Google Scholar] [CrossRef]
- Watson, D.P. Use of cyanoacrylate tissue adhesive for closing facial lacerations in children. BMJ 1989, 299, 1014. [Google Scholar] [CrossRef][Green Version]
- Loh, D.C.; Wilson, R.B. Endoscopic management of refractory gastrointestinal non-variceal bleeding using histoacryl (n-butyl-2-cyanoacrylate) glue. Gastroenterol. Rep. 2016, 4, 232–236. [Google Scholar] [CrossRef][Green Version]
- Schneider, G.; Otto, K. In vitro and in vivo studies on the use of histoacryl(®) as a soft tissue glue. Eur. Arch. Otorhinolaryngol. 2012, 269, 1783–1789. [Google Scholar] [CrossRef]
- Fotiadis, C.; Leventis, I.; Adamis, S.; Gorgoulis, V.; Domeyer, P.; Zografos, G.; Sechas, M.; Skalkeas, G. The use of isobutylcyanoacrylate as a tissue adhesive in abdominal surgery. Acta Chir. Belg. 2005, 105, 392–396. [Google Scholar] [CrossRef]
- Ensari, C.O.; Genc, V.; Cakmak, A.; Erkek, B.; Karayalcin, K. Effects of n-butyl-2-cyanoacrylate on high-level jejunojejunostomy. Eur. Surg. Res. 2010, 44, 13–16. [Google Scholar] [CrossRef]
- Al-Jazaeri, A.; Asiri, Y.; Alkahtani, S.; Al-Rikabi, A.; Alzahem, A. Percutaneous obliteration of patent processus vaginalis: A rat model for future inguinal hernia repair in children. J. Pediatric Surg. 2013, 48, 203–208. [Google Scholar] [CrossRef] [PubMed]
- Park, S.M.; Hong, Y.J.; Chang, E.Y.; Han, S.J. A human case study demonstrating the safety and effectiveness of laparoscopic surgical glue injection hernioplasty for pediatric indirect inguinal hernia. J. Pediatric Surg. Case Rep. 2014, 2, 432–435. [Google Scholar] [CrossRef][Green Version]
- Escolino, M.; Esposito, C.; Eaton, S.; Di Maro, E.; Cozzolino, S.; Vitagliano, G.; D’Armiento, M.; Esposito, G.; De Coppi, P. Laparoscopic injection of tissue adhesives for inguinal hernia repair in a rabbit model: Results of an experimental comparative study with the standard laparoscopic inguinal hernia repair. J. Laparoendosc. Adv. Surg. Tech. Part A 2020, 30, 847–853. [Google Scholar] [CrossRef] [PubMed]
- Waite, J.H. Nature’s underwater adhesive specialist. Int. J. Adhes. Adhes. 1987, 7, 9–14. [Google Scholar] [CrossRef]
- Jeon, E.Y.; Choi, B.H.; Jung, D.; Hwang, B.H.; Cha, H.J. Natural healing-inspired collagen-targeting surgical protein glue for accelerated scarless skin regeneration. Biomaterials 2017, 134, 154–165. [Google Scholar] [CrossRef]
- Jeon, E.Y.; Lee, J.; Kim, B.J.; Joo, K.I.; Kim, K.H.; Lim, G.; Cha, H.J. Bio-inspired swellable hydrogel-forming double-layered adhesive microneedle protein patch for regenerative internal/external surgical closure. Biomaterials 2019, 222, 119439. [Google Scholar] [CrossRef]
- Dove, J.; Sheridan, P. Adhesive protein from mussels: Possibilities for dentistry, medicine, and industry. J. Am. Dent. Assoc. 1986, 112, 879. [Google Scholar]
- Grande, D.A.; Pitman, M.I. The use of adhesives in chondrocyte transplantation surgery. Preliminary studies. Bull. Hosp. Jt. Dis. Orthop. Inst. 1988, 48, 140–148. [Google Scholar]
- Sáez, C.; Pardo, J.; Gutierrez, E.; Brito, M.; Burzio, L.O. Immunological studies of the polyphenolic proteins of mussels. Comp. Biochem. Physiol. Part B: Comp. Biochem. 1991, 98, 569–572. [Google Scholar] [CrossRef]
- Waite, J.H. Adhesion a la moule. Integr. Comp. Biol. 2002, 42, 1172–1180. [Google Scholar] [CrossRef]
- Kim, H.J.; Pyun, J.H.; Park, T.Y.; Yoon, S.G.; Maeng, S.W.; Choi, H.S.; Joo, K.I.; Kang, S.H.; Cha, H.J. Preclinical evaluation of a regenerative immiscible bioglue for vesico-vaginal fistula. Acta Biomater 2021, 125, 183–196. [Google Scholar] [CrossRef] [PubMed]
- Jukić, M.; Pogorelić, Z.; Šupe-Domić, D.; Jerončić, A. Comparison of inflammatory stress response between laparoscopic and open approach for pediatric inguinal hernia repair in children. Surg. Endosc. 2019, 33, 3243–3250. [Google Scholar] [CrossRef] [PubMed]
- Bickler, S.W.; Rode, H. Surgical services for children in developing countries. Bull. World Health Organ. 2002, 80, 829–835. [Google Scholar] [PubMed]
- Eeson, G.; Birabwa-Male, D.; Pennington, M.; Blair, G.K. Costs and cost-effectiveness of pediatric inguinal hernia repair in uganda. World J. Surg. 2015, 39, 343–349. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).