Developing a Risk Model for Assessment and Control of the Spread of COVID-19
Abstract
:1. Introduction
2. Study Objectives
- Understanding the existing literature on critical risk factors and identifying the most recent studies regarding COVID-19’s spread based on risk analysis.
- Identifying the risk factors and the main risk groups that affect COVID-19’s spread. It is essential to produce awareness of these risk factors as well as their probabilities of occurrence, and declare the degree to which of them has high impacts on COVID-19’s spread.
- Developing and designing a new risk analysis model that can be used for risk factors weighting and prioritizing based on the available data such as probabilities of occurrences and impacts of risk factors on COVID-19’s spread with further application among variable community sectors accordingly. The proposed model can support decision makers who deal with COVID-19’s spread effects in all country sectors to analyze their problems and make sound decisions concerning such spread.
- Collecting data from real case studies to apply the new model in medical sector and other related sectors in Saudi Arabia. The data will include critical risk factors, probabilities of occurrences of risk sources, and their impacts on COVID-19’s spread.
- Applying and verifying the new model using the collected data on case studies in Saudi Arabia as well as discussing in detail the model results and critical risk factors. The model can be adopted to satisfy other similar situations in Saudi Arabia.
3. Research Plan
- Conducting a comprehensive literature reviewing risk sources of COVID-19’s spread in many countries all over the world. The literature includes a deep review for the risk analysis models used in assessment similar viruses spread. The literature concentrates on identifying risks associated to COVID-19’s spread in developing countries, especially in Saudi Arabia.
- Conducting field surveys to identify risk factors at health care facilities in Saudi Arabia. These surveys will cover some medical organizations and medical staff involved in the problem of COVID-19’s spread.
- A full statistical analysis of the survey data is also introduced to assess risk factors based on their probabilities of occurrence as well as their impacts on COVID-19’s spread.
- Developing and proving the proposed risk analysis model to satisfy the research objectives.
- Applying and verifying the new model on the selected case study data and receiving outputs. A comparative analysis for the results from the model outputs with the real results from the case study is executed.
4. Evaluation of Risks Affecting Diseases
5. Using Fuzzy Techniques in Disease Assessment
6. Field Survey and Data Collection
7. Risks Affecting the Spread of Coronavirus Disease 2019 (COVID-19)
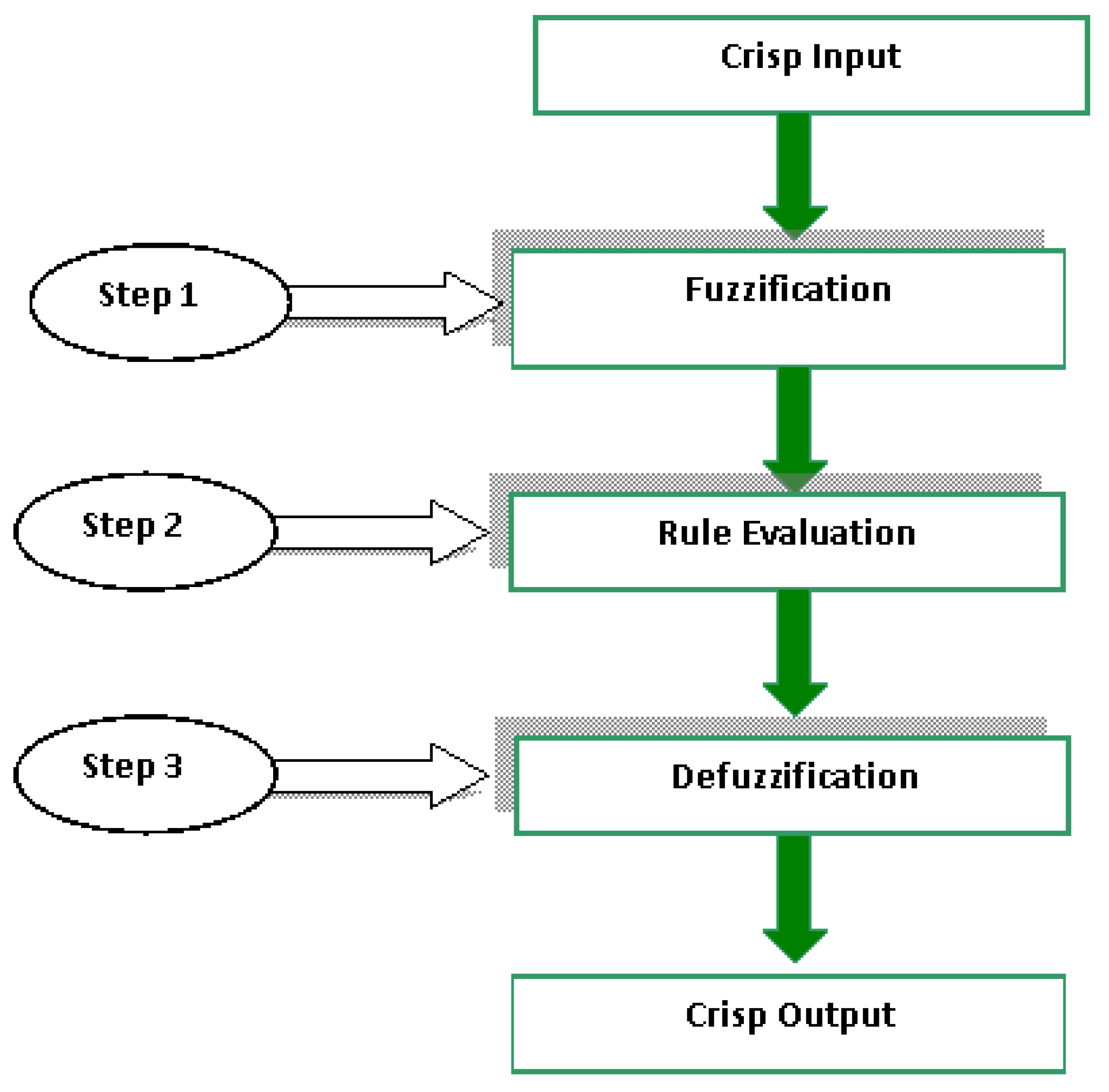
8. Risk Analysis Model for COVID-19 Spread (RAMCS)
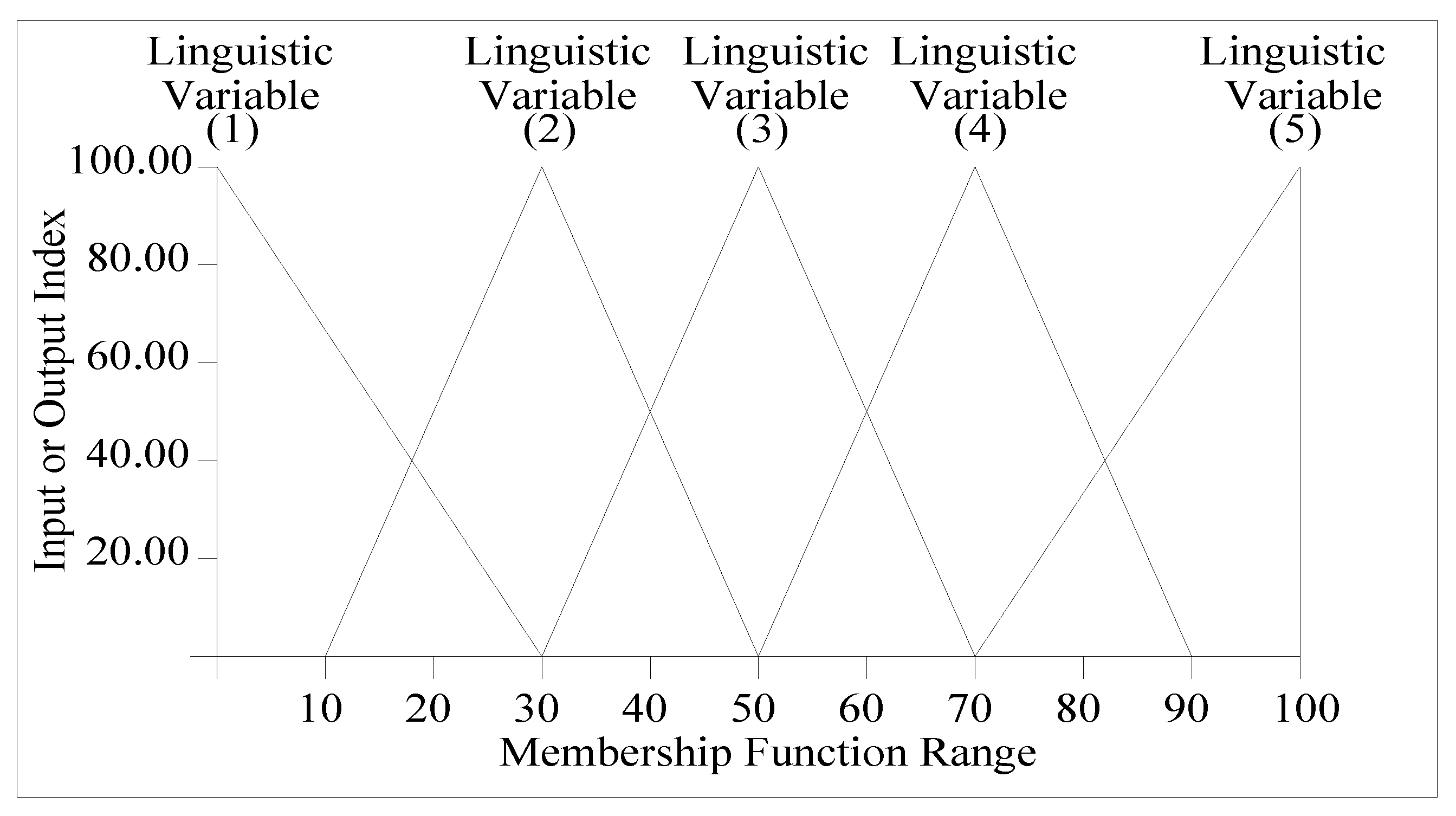
8.1. Membership Functions
8.2. Fuzzy Logical Rules
- If PI is Minor and IIVS is Likely then FIVS is Medium.
- If PI is Major and IIVS is Moderate then FIVS is Medium.
- If PI is Trivial and IIVS is Likely the FIVS is Low.
8.3. Model Verification
8.4. Model Limitations
- The number of linguistic terms applied in the model inputs or output are restricted to five only. Using more than five linguistics, particularly in model inputs, may give more accurate results because it allows the user or respondents to select a linguistic variable among a number greater than five.
- There is no chance for a case of zero risk probability of occurrence, or impact on COVID-19’s spread choice. For example, minimum value for inputs is 0.1, not zero.
- The model is limited to qualitatively analyzing risks and it cannot determine the quantitative effects of such risks on COVID-19’s spread.
9. Model Application and Results
9.1. Inputs and Output Variables Correlations
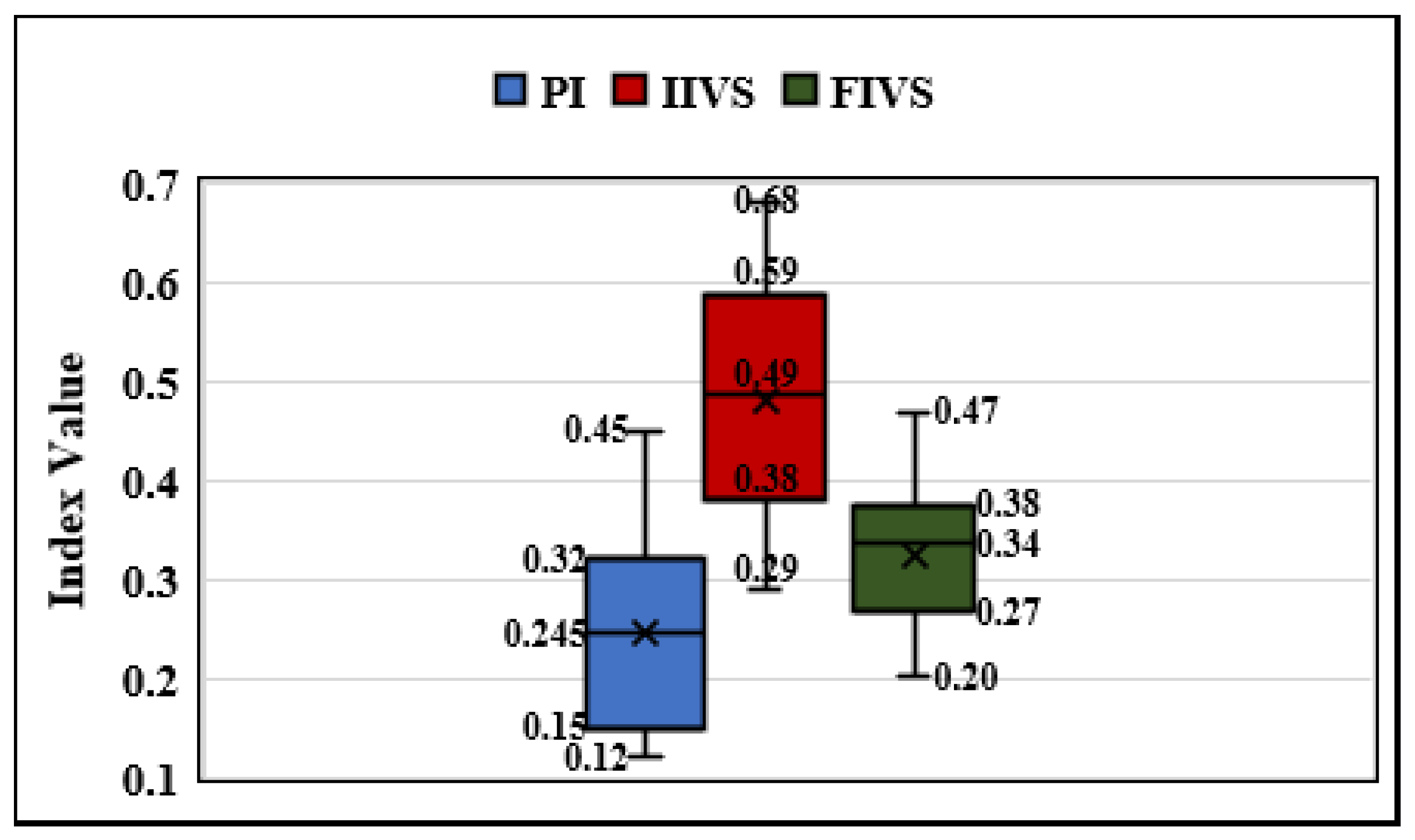
9.2. Box Plot Analysis
9.3. Risk Groups Analysis
10. Applying the Model to Other Case Studies
- Identifying all risk factors affecting the epidemic. The risk factors and risk groups defined in this study may be suitable and can be utilized and modified.
- Defining the objectives which will be affected by the epidemic such as virus spread.
- Collecting data concern the risk factors characteristics such as probability of occurrence and the impact on the identified objectives.
- Defining the logical rules and the relation among inputs and the output as introduced in the proposed model.
- Applying the model on all risk factors and studying the results to support any required decisions.
11. Conclusions
- Poor social distance and overcrowding are the most important risk factors. On the level of risk groups, (daily activities) is the most important risk group followed by (Home isolation) risk group.
- Although risk group (Early preventive actions) was affected by 12 risk factors which give it great importance, the impact of such group is insignificant. This result is achieved due to the application of preventive measures by the Saudi government.
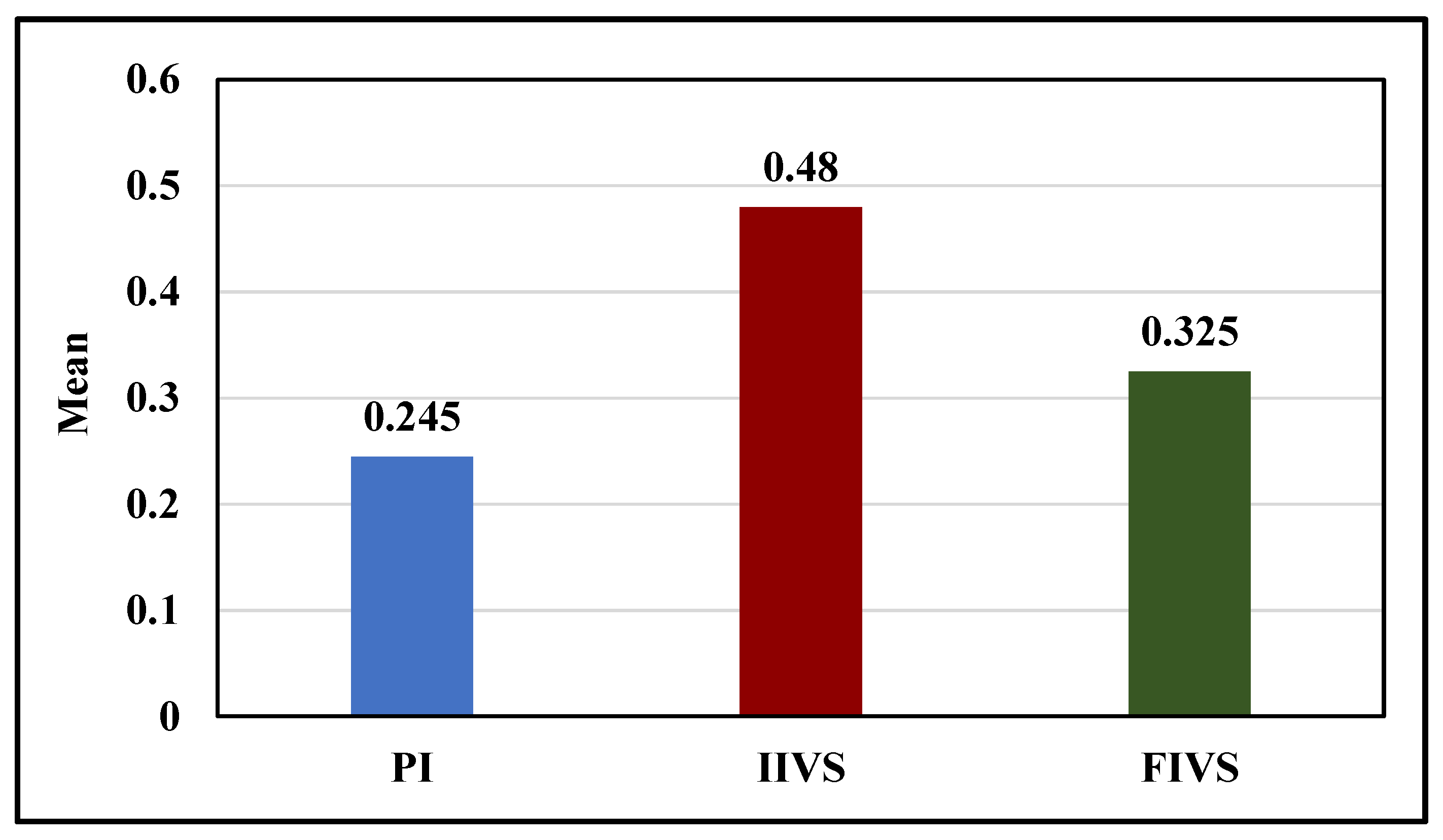
- By studying the statistical results due to relation among the three developed indices, it was concluded that average mean for IIVS represents the maximum value among the three indices followed by FIVS, then PI. On the other hand, the maximum range value is for IIVS followed by PI, while the lowest value is for FIVS. The maximum values for risk factors appear in the IIVS and minimum values appear in PI. There is significant correlation between IIVS and FIVS while the correlation between PI and FIVS is positive with no significance. In contrast, it can be noted that there is no association between PI and IIVS.
- The existing model can be applied in all countries using slight modifications and it is not restricted to Saudi Arabia. Applying the fuzzy logic technique appended flexibility and ease of usage in addressing the problem.
- It is recommended that in medical health facilities key risk factors obtainable in this study to be considered as well as the proposed model for the assessment of risk factors affecting any virus’s spread.
- As the proposed model represents a new technique in epidemics science, it is recommended for extending this work to cover risk management processes. The proposed model determines the qualitative effect only for the risk factors for COVID-19’s spread, so the model should be extended to cover quantitative risk analysis. Furthermore, the model should be studied to support decisions based on quantitative risk analysis to solve many epidemic problems.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Aldila, Dipo, Sarbaz H. A. Khoshnaw, Egi Safitri, Yusril Rais Anwar, Aanisah R. Q. Bakry, Brenda M. Samiadji, Demas A. Anugerah, M. Farhan Alfarizi Gh, Indri D. Ayulani, and Sheryl N. Salim. 2020. A Mathematical Study on the Spread of COVID-19 Considering Social Distancing and Rapid Assessment: The Case of Jakarta, Indonesia. Chaos, Solitons & Fractals 139: 110042. [Google Scholar] [CrossRef]
- Alshammari, Thamir M., Ali F. Altebainawi, and Khalidah A. Alenzi. 2020. Importance of Early Precautionary Actions in Avoiding the Spread of COVID-19: Saudi Arabia as an Example. Saudi Pharmaceutical Journal 28: 898–902. [Google Scholar] [CrossRef] [PubMed]
- Alzahrani, Saleh I., Ibrahim A. Aljamaan, and Ebrahim A. Al-Fakih. 2020. Forecasting the Spread of the COVID-19 Pandemic in Saudi Arabia Using ARIMA Prediction Model under Current Public Health Interventions. Journal of Infection and Public Health 13: 914–19. [Google Scholar] [CrossRef]
- Arji, Goli, Hossein Ahmadi, Mehrbakhsh Nilashi, Tarik A. Rashid, Omed Hassan Ahmed, Nahla Aljojo, and Azida Zainol. 2019. Fuzzy Logic Approach for Infectious Disease Diagnosis: A Methodical Evaluation, Literature and Classification. Biocybernetics and Biomedical Engineering 39: 937–55. [Google Scholar] [CrossRef]
- Ceylan, Zeynep. 2020. Estimation of COVID-19 Prevalence in Italy, Spain, and France. Science of The Total Environment 729: 138817. [Google Scholar] [CrossRef]
- Coşkun, Hamit, Nazmiye Yıldırım, and Samettin Gündüz. 2021. The Spread of COVID-19 Virus through Population Density and Wind in Turkey Cities. Science of The Total Environment 751: 141663. [Google Scholar] [CrossRef]
- Crotta, Matteo, Antonio Lavazza, Ana Mateus, and Javier Guitian. 2018. Quantitative Risk Assessment of Hepatitis E Virus: Modelling the Occurrence of Viraemic Pigs and the Presence of the Virus in Organs of Food Safety Interest. Microbial Risk Analysis 9: 64–71. [Google Scholar] [CrossRef] [Green Version]
- Dai, Zhichu, Kitling Fan, Li Zhang, Meixiang Yang, Qingqin Yu, Lichang Liu, and Lingpong Leung. 2020. Risk Factors for Influenza B Virus–Associated Pneumonia in Adults. American Journal of Infection Control 48: 194–98. [Google Scholar] [CrossRef] [PubMed]
- Hossain, M. Pear, Alvin Junus, Xiaolin Zhu, Pengfei Jia, Tzai-Hung Wen, Dirk Pfeiffer, and Hsiang-Yu Yuan. 2020. The Effects of Border Control and Quarantine Measures on the Spread of COVID-19. Epidemics 32: 100397. [Google Scholar] [CrossRef] [PubMed]
- Huang, Lei, Xiuwen Zhang, Xinyue Zhang, Zhijian Wei, Lingli Zhang, Jingjing Xu, Peipei Liang, Yuanhong Xu, Chengyuan Zhang, and Aman Xu. 2020. Rapid Asymptomatic Transmission of COVID-19 during the Incubation Period Demonstrating Strong Infectivity in a Cluster of Youngsters Aged 16-23 Years Outside Wuhan and Characteristics of Young Patients with COVID-19: A Prospective Contact-Tracing Study. Journal of Infection 80: e1–e13. [Google Scholar] [CrossRef]
- Iqbal, Muhammad Mazhar, Irfan Abid, Saddam Hussain, Naeem Shahzad, Muhammad Sohail Waqas, and Muhammad Jawed Iqbal. 2020. The Effects of Regional Climatic Condition on the Spread of COVID-19 at Global Scale. Science of The Total Environment 739: 140101. [Google Scholar] [CrossRef]
- Issa, Usama Hamed. 2012a. Developing an Assessment Model for Factors Affecting the Quality in the Construction Industry. Journal of Civil Engineering and Architecture 6: 364–71. [Google Scholar] [CrossRef] [Green Version]
- Issa, Usama Hamed. 2012b. A Model for Time Overrun Quantification in Construction of Industrial Projects Based on Risk Evaluation. Journal of American Science 8: 523–29. [Google Scholar]
- Issa, Usama H., and Aly Ahmed. 2014. On the Quality of Driven Piles Construction Based on Risk Analysis. International Journal of Civil Engineering 12: 121–29. [Google Scholar]
- Issa, Usama Hamed, Aly Ahmed, and Keizo Ugai. 2013. A Decision Support System for Ground Improvement Projects Using Gypsum Waste Case Study: Embankments Construction in Japan. Civil and Environmental Research 3: 74–84. [Google Scholar]
- Issa, Usama Hamed, Salah Attia Mosaad, and Mohamed Salah Hassan. 2019. A Model for Evaluating the Risk Effects on Construction Project Activities. Journal of Civil Engineering and Management 25: 687–99. [Google Scholar] [CrossRef]
- Kindhi, Berlian Al, Tri Arief Sardjono, Mauridhi Hery Purnomo, and Gijbertus Jacob Verkerke. 2019. Hybrid K-Means, Fuzzy C-Means, and Hierarchical Clustering for DNA Hepatitis C Virus Trend Mutation Analysis. Expert Systems with Applications 121: 373–81. [Google Scholar] [CrossRef]
- Liebetrau, Albert M. 1983. Measures of Association. Newcastle upon Tyne: SAGE. [Google Scholar]
- Lin, Jun, Weihao Huang, Muchen Wen, Dehong Li, Shuyi Ma, Jiawen Hua, Hang Hu, Shan Yin, Yanjun Qian, Peiling Chen, and et al. 2020. Containing the Spread of Coronavirus Disease 2019 (COVID-19): Meteorological Factors and Control Strategies. Science of The Total Environment 744: 140935. [Google Scholar] [CrossRef]
- Ma, Yueling, Yadong Zhao, Jiangtao Liu, Xiaotao He, Bo Wang, Shihua Fu, Jun Yan, Jingping Niu, Ji Zhou, and Bin Luo. 2020. Effects of Temperature Variation and Humidity on the Death of COVID-19 in Wuhan, China. Science of The Total Environment 724: 138226. [Google Scholar] [CrossRef]
- Massad, Eduardo, Marcelo Nascimento Burattini, and Neli Regina Ortega. 1999. Fuzzy Logic and Measles Vaccination: Designing a Control Strategy. International Journal of Epidemiology 28: 550–57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ndaïrou, Faïçal, Iván Area, Juan J. Nieto, and Delfim F. M. Torres. 2020. Mathematical Modeling of COVID-19 Transmission Dynamics with a Case Study of Wuhan. Chaos, Solitons & Fractals 135: 109846. [Google Scholar] [CrossRef]
- Novák, Vilém, and Stephan Lehmke. 2006. Logical Structure of Fuzzy IF-THEN Rules. Fuzzy Sets and Systems 157: 2003–29. [Google Scholar] [CrossRef]
- Oliveira, Ana R. S., José Piaggio, Lee W. Cohnstaedt, D. Scott McVey, and Natalia Cernicchiaro. 2018. A Quantitative Risk Assessment (QRA) of the Risk of Introduction of the Japanese Encephalitis Virus (JEV) in the United States via Infected Mosquitoes Transported in Aircraft and Cargo Ships. Preventive Veterinary Medicine 160: 1–9. [Google Scholar] [CrossRef]
- Pasalari, Hasan, Angila Ataei-Pirkooh, Mahdi Aminikhah, Ahmad Jonidi Jafari, and Mahdi Farzadkia. 2019. Assessment of Airborne Enteric Viruses Emitted from Wastewater Treatment Plant: Atmospheric Dispersion Model, Quantitative Microbial Risk Assessment, Disease Burden. Environmental Pollution 253: 464–73. [Google Scholar] [CrossRef] [PubMed]
- Pereira, Claudia Cristina de Aguiar, Carla Jorge Machado, and Roberto do Nascimento Rodrigues. 2007. Profiles of multiple causes of death related to HIV/AIDS in the cities of São Paulo and Santos, Brazil, 2001. Cadernos de Saude Publica 23: 645–55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reyna, Valerie F., and Mary B. Adam. 2003. Fuzzy-Trace Theory, Risk Communication, and Product Labeling in Sexually Transmitted Diseases. Risk Analysis: An Official Publication of the Society for Risk Analysis 23: 325–42. [Google Scholar] [CrossRef]
- Robson, Barry. 2020. COVID-19 Coronavirus Spike Protein Analysis for Synthetic Vaccines, a Peptidomimetic Antagonist, and Therapeutic Drugs, and Analysis of a Proposed Achilles’ Heel Conserved Region to Minimize Probability of Escape Mutations and Drug Resistance. Computers in Biology and Medicine 121: 103749. [Google Scholar] [CrossRef]
- Saadat, Saeida, Deepak Rawtani, and Chaudhery Mustansar Hussain. 2020. Environmental Perspective of COVID-19. Science of The Total Environment 728: 138870. [Google Scholar] [CrossRef]
- Shiina, Akihiro, Tomihisa Niitsu, Osamu Kobori, Keita Idemoto, Tasuku Hashimoto, Tsuyoshi Sasaki, Yoshito Igarashi, Eiji Shimizu, Michiko Nakazato, Kenji Hashimoto, and et al. 2020. Relationship between Perception and Anxiety about COVID-19 Infection and Risk Behaviors for Spreading Infection: A National Survey in Japan. Brain, Behavior, & Immunity-Health 6: 100101. [Google Scholar] [CrossRef]
- Tah, Joseph H. M., and V. Carr. 2000. A Proposal for Construction Project Risk Assessment Using Fuzzy Logic. Construction Management and Economics 18: 491–500. [Google Scholar] [CrossRef]
- Tah, Joseph H. M., and V. Carr. 2001. Knowledge-Based Approach to Construction Project Risk Management. Journal of Computing in Civil Engineering 15: 170–77. [Google Scholar] [CrossRef]
- Teng, Yue, Dehua Bi, Guigang Xie, Yuan Jin, Yong Huang, Baihan Lin, Xiaoping An, Yigang Tong, and Dan Feng. 2017. Model-Informed Risk Assessment for Zika Virus Outbreaks in the Asia-Pacific Regions. Journal of Infection 74: 484–91. [Google Scholar] [CrossRef] [Green Version]
- Thukral, Sunny, and Vijay Rana. 2019. Versatility of Fuzzy Logic in Chronic Diseases: A Review. Medical Hypotheses 122: 150–56. [Google Scholar] [CrossRef]
- Tukey, John W. 1977. Exploratory Data Analysis. London: Pearson. [Google Scholar]
- Varotsos, Costas A., and Vladimir F. Krapivin. 2020. A New Model for the Spread of COVID-19 and the Improvement of Safety. Safety Science 132: 104962. [Google Scholar] [CrossRef] [PubMed]
- Vieira, Luciana Cristina Pompeo Ferreira da Silva, Paloma Maria da Silva Rocha Rizol, and Luiz Fernando Costa Nascimento. 2019. Fuzzy Logic and Hospital Admission Due to Respiratory Diseases Using Estimated Values by Mathematical Model. Ciencia & Saude Coletiva 24: 1083–90. [Google Scholar]
- Xia, Xiao-ying, Jing Wu, He-lei Liu, Hong Xia, Bei Jia, and Wen-xiang Huang. 2020. Epidemiological and Initial Clinical Characteristics of Patients with Family Aggregation of COVID-19. Journal of Clinical Virology 127: 104360. [Google Scholar] [CrossRef]
- Yan, Qinling, Yingling Tang, Dingding Yan, Jiaying Wang, Linqian Yang, Xinpei Yang, and Sanyi Tang. 2020. Impact of Media Reports on the Early Spread of COVID-19 Epidemic. Journal of Theoretical Biology 502: 110385. [Google Scholar] [CrossRef] [PubMed]
- Zadeh, Lotfi A. 2008. Is There a Need for Fuzzy Logic? Information Sciences 178: 2751–79. [Google Scholar] [CrossRef]
| Factor No. | Risk Factor |
|---|---|
| Risk Group 01: Travel Abroad | |
| 1 | Destination: To far places or to area with high epidemics |
| 2 | Transit |
| 3 | Long duration and Prolonged stay |
| 4 | High contact rate between passengers and crews |
| 5 | Poor compliance to personal protective measures |
| 6 | Cheap flights or using economic class |
| Risk Group 02: Travel Within the Country | |
| 7 | Far destination |
| 8 | Crowded public transport |
| 9 | Poor compliance to personal protective measures |
| Risk Group 03: Daily activities | |
| 10 | Poor social distance |
| 11 | Poor compliance to personal protective measures |
| 12 | Crowdedness |
| 13 | Reusable items |
| Risk Group 04: Home Isolation | |
| 14 | Lack of consciousness |
| 15 | Poor Personal hygiene practices |
| 16 | Lack of separate healthy isolation room |
| 17 | Lack of single use items |
| 18 | Lack of awareness and compliance of contacts at home |
| Risk Group 05: Early Preventive Actions | |
| 19 | Late border control and quarantine measures |
| 20 | Incomplete restriction of international and domestic flights |
| 21 | Poor screening programme |
| 22 | Shortage of surveillance data |
| 23 | Shortage of protective supplies at health care centers |
| 24 | Lack of remote health education programme |
| 25 | Lack of appropriate treatment protocol |
| 26 | Delayed curfew when needed |
| 27 | Poor ability for remote/online working |
| 28 | Lack of areas for isolation and quarantine |
| 29 | Inappropriate disposal of garbage and sewage |
| 30 | Lack of financial support |
| Risk Group 06: Health Conditions | |
| 31 | Underlying health conditions |
| 32 | Age extremities |
| 33 | Pregnancy |
| Risk Group 07: Hospitals and Healthcare Buildings | |
| 34 | Shortage of isolation hospitals |
| 35 | Lack of PPE supplies |
| 36 | Shortage of medications and inappropriate treatment protocols |
| 37 | Lack of infection control programme |
| Risk Group 08: Meteorological Factors or Microclimatic Conditions | |
| 38 | Poor airflow and ventilation |
| 39 | High humidity |
| 40 | inappropriate air temperature |
| 41 | Lack of exposure to sunlight |
| Risk Group 09: Socioeconomic Status | |
| 42 | Lack of financial support |
| 43 | Inappropriate sick leave system |
| 44 | Lack of remote health education |
| 45 | Low Per capita income level |
| 46 | Low level of culture and education |
| Scale | Impact on COVID-19 Spread | |||||
|---|---|---|---|---|---|---|
| Rare | Unlikely | Moderate | Likely | Very Likely | ||
| Probability | Trivial | Very Low | Very Low | Low | Low | Medium |
| Minor | Very Low | Low | Low | Medium | Medium | |
| Moderate | Low | Low | Medium | Medium | High | |
| Major | Low | Medium | Medium | High | Very High | |
| Extreme | Medium | Medium | High | Very High | Very High | |
| Factor No. | Group No. | Risk Factor | PI | IIVS | SIVS | FIVS | Rank Due to FIVS |
|---|---|---|---|---|---|---|---|
| 10 | G03 | Poor social distance | 0.38 | 0.68 | 0.26 | 0.469 | 1 |
| 12 | G03 | Crowdedness | 0.39 | 0.68 | 0.27 | 0.468 | 2 |
| 15 | G04 | Poor Personal hygiene practices | 0.29 | 0.66 | 0.19 | 0.452 | 3 |
| 14 | G04 | Lack of consciousness | 0.32 | 0.63 | 0.20 | 0.424 | 4 |
| 37 | G07 | Lack of infection control programme | 0.31 | 0.62 | 0.19 | 0.416 | 5 |
| 11 | G03 | Poor compliance to personal protective measures | 0.39 | 0.62 | 0.24 | 0.413 | 6 |
| 8 | G02 | Crowded public transport | 0.28 | 0.61 | 0.17 | 0.408 | 7 |
| 31 | G06 | Underlying health conditions | 0.41 | 0.38 | 0.16 | 0.387 | 8 |
| 9 | G02 | Poor compliance to personal protective measures | 0.31 | 0.58 | 0.18 | 0.384 | 9 |
| 18 | G04 | Lack of awareness and compliance of contacts at home | 0.38 | 0.53 | 0.20 | 0.384 | 10 |
| 5 | G01 | Poor compliance to personal protective measures | 0.24 | 0.57 | 0.14 | 0.376 | 11 |
| 13 | G03 | Reusable items | 0.32 | 0.57 | 0.18 | 0.376 | 12 |
| 27 | G05 | Poor ability for remote/online working | 0.19 | 0.55 | 0.10 | 0.373 | 13 |
| 19 | G05 | Late border control and quarantine measures | 0.15 | 0.62 | 0.09 | 0.369 | 14 |
| 16 | G04 | Lack of separate healthy isolation room | 0.34 | 0.56 | 0.19 | 0.367 | 15 |
| 25 | G05 | Lack of appropriate treatment protocol | 0.14 | 0.58 | 0.08 | 0.357 | 16 |
| 26 | G05 | Delayed curfew when needed | 0.14 | 0.56 | 0.08 | 0.357 | 17 |
| 7 | G02 | Far destination | 0.39 | 0.33 | 0.13 | 0.345 | 18 |
| 23 | G05 | Shortage of protective supplies at health care centers | 0.13 | 0.61 | 0.08 | 0.345 | 19 |
| 35 | G07 | Lack of PPE supplies | 0.13 | 0.62 | 0.08 | 0.344 | 20 |
| 41 | G08 | Lack of exposure to sunlight | 0.36 | 0.33 | 0.12 | 0.34 | 21 |
| 38 | G08 | Poor airflow and ventilation | 0.25 | 0.53 | 0.13 | 0.339 | 22 |
| 17 | G04 | Lack of single use items | 0.33 | 0.49 | 0.16 | 0.338 | 23 |
| 30 | G05 | Lack of financial support | 0.12 | 0.61 | 0.07 | 0.332 | 24 |
| 46 | G09 | Low level of culture and education | 0.32 | 0.39 | 0.12 | 0.332 | 25 |
| 4 | G01 | High contact rate between passengers and crews | 0.24 | 0.52 | 0.12 | 0.329 | 26 |
| 32 | G06 | Age extremities | 0.45 | 0.32 | 0.14 | 0.328 | 27 |
| 33 | G06 | Pregnancy | 0.32 | 0.33 | 0.11 | 0.327 | 28 |
| 1 | G01 | Destination:To far places or to area with high epidemics | 0.21 | 0.51 | 0.11 | 0.317 | 29 |
| 40 | G08 | inappropriate air temperature | 0.29 | 0.32 | 0.09 | 0.295 | 30 |
| 45 | G09 | Low Per capita income level | 0.29 | 0.35 | 0.10 | 0.295 | 31 |
| 36 | G07 | Shortage of medications and inappropriate treatment protocols | 0.14 | 0.48 | 0.07 | 0.283 | 32 |
| 42 | G09 | Lack of financial support | 0.25 | 0.29 | 0.07 | 0.276 | 33 |
| 39 | G08 | High humidity | 0.25 | 0.39 | 0.10 | 0.272 | 34 |
| 20 | G05 | Incomplete restriction of international and domestic flights | 0.14 | 0.46 | 0.06 | 0.267 | 35 |
| 6 | G01 | Cheap flights or using economic class | 0.21 | 0.38 | 0.08 | 0.252 | 36 |
| 34 | G07 | Shortage of isolation hospitals | 0.14 | 0.42 | 0.06 | 0.238 | 37 |
| 24 | G05 | Lack of remote health education programme | 0.15 | 0.42 | 0.06 | 0.236 | 38 |
| 28 | G05 | Lack of areas for isolation and quarantine | 0.15 | 0.42 | 0.06 | 0.236 | 39 |
| 44 | G09 | Lack of remote health education | 0.12 | 0.41 | 0.05 | 0.232 | 40 |
| 29 | G05 | Inappropriate disposal of garbage and sewage | 0.18 | 0.41 | 0.07 | 0.228 | 41 |
| 43 | G09 | Inappropriate sick leave system | 0.15 | 0.39 | 0.06 | 0.22 | 42 |
| 2 | G01 | Transit | 0.16 | 0.32 | 0.05 | 0.207 | 43 |
| 3 | G01 | Long duration and Prolonged stay | 0.16 | 0.31 | 0.05 | 0.207 | 44 |
| 22 | G05 | Shortage of surveillance data | 0.12 | 0.38 | 0.05 | 0.206 | 45 |
| 21 | G05 | Poor screening programme | 0.15 | 0.36 | 0.054 | 0.203 | 46 |
| Input/Output | PI and IIVS | PI and FIVS | IIVS and FIVS |
|---|---|---|---|
| Spearmann | −0.001 | 0.558 | 0.739 |
| Kendall | −0.004 | 0.413 | 0.582 |
| Group No. | Group Name | Factors Numbers in Group | Mean | Range |
|---|---|---|---|---|
| 1 | Travel Abroad | 6 | 0.28 | 0.17 |
| 2 | Travel Within the Country | 3 | 0.38 | 0.06 |
| 3 | Daily activities | 4 | 0.43 | 0.09 |
| 4 | Home Isolation | 5 | 0.39 | 0.11 |
| 5 | Early Preventive Actions | 12 | 0.29 | 0.17 |
| 6 | Health Conditions | 3 | 0.35 | 0.06 |
| 7 | Hospitals and Healthcare Buildings | 4 | 0.32 | 0.18 |
| 8 | Meteorological Factors or Microclimatic Conditions | 4 | 0.31 | 0.07 |
| 9 | Socioeconomic Status | 5 | 0.27 | 0.11 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Issa, U.H.; Balabel, A.; Abdelhakeem, M.; Osman, M.M.A. Developing a Risk Model for Assessment and Control of the Spread of COVID-19. Risks 2021, 9, 38. https://doi.org/10.3390/risks9020038
Issa UH, Balabel A, Abdelhakeem M, Osman MMA. Developing a Risk Model for Assessment and Control of the Spread of COVID-19. Risks. 2021; 9(2):38. https://doi.org/10.3390/risks9020038
Chicago/Turabian StyleIssa, Usama H., Ashraf Balabel, Mohammed Abdelhakeem, and Medhat M. A. Osman. 2021. "Developing a Risk Model for Assessment and Control of the Spread of COVID-19" Risks 9, no. 2: 38. https://doi.org/10.3390/risks9020038
APA StyleIssa, U. H., Balabel, A., Abdelhakeem, M., & Osman, M. M. A. (2021). Developing a Risk Model for Assessment and Control of the Spread of COVID-19. Risks, 9(2), 38. https://doi.org/10.3390/risks9020038







