1. Introduction
Proteinuric kidney disease is accompanied by a progressive increase in the amount of protein spilling into the urine which can reach nephrotic range proportions i.e., loss of ≥3 gm protein/day [
1,
2]. Left untreated proteinuric kidney disease can progress to end-stage renal disease (ESRD). The majority of proteinuric kidney diseases is thought to be glomerular in nature and is characterized by glomerular hypertrophy and deposition of matrix therein [
3]. The matrix is composed of one more types of collagen depending on the disease and the heterogeneity of the patient population. Glomerular accumulation of collagen types I, IV, and VI have been reported in diabetic nephropathy which affects a relatively large population across the globe [
4,
5]. In focal segmental glomerulosclerosis, collagen type IV, and to a lesser degree collagen type VI, accumulates in the enlarged glomerular mesangial matrix and in the glomerular basement membrane [
6]. Glomerular accumulation of collagen type III is the predominant finding in, and almost exclusively characterizes, collagenofibrotic glomerulopathy, also known as collagen type III glomerulopathy, and nail-patella syndrome [
7,
8]. Both these rare diseases are characterized by overt proteinuria and need for renal replacement, typically within 10 years of diagnosis [
7].
Curiously, proteinuric kidney disease glomerulosclerosis are eventually accompanied by tubulointerstitial matrix deposition. The presence of scar in the tubulointerstitium accelerates the progression of kidney fibrosis, and is associated with poorer prognosis [
9,
10]. To date, treatment of proteinuric kidney disease is restricted to use of drugs developed for cardiovascular and metabolic disorders including antihypertensives and blood sugar reducing agents. These regimens are only partially effective, which is evidenced by the increasing incidence of renal replacement therapy. In contrast to a disease such as diabetic nephropathy characterized by both heterogeneity and comorbidities, a pathology in diseases such as collagenofibrotic glomerulopathy is more homogenous. Understanding the qualitative and quantitative changes in collagen type III accumulation in such a disease might spur development of targeted and effective therapeutics.
Administration of puromycin aminonucleoside (PAN) to rats is associated with proteinuria and changes in glomerular microarchitecture that mimics to some extent human proteinuric kidney disease [
11,
12,
13,
14]. Although rodent models are largely resistant to glomerular insult and at most demonstrate a transient increase in urine protein in response to toxins such as PAN, they remain the model of choice for nonclinical screening of therapeutic modalities [
11,
12]. The present study evaluates the relation between proteinuria and glomerular collagen type III accumulation, and compartmental differences in collagen type III signaling in the rat model of PAN nephropathy.
2. Materials and Methods
2.1. Animal Model
This study was conducted after obtaining approval (2019-013-R) from Angion’s institutional animal care and use committee.
Adult male Wistar rats (~6 weeks old, ~75 g) were provided standard lab diet (5001, LabDiet, St. Louis, MO, USA, calories provided by protein 28.5%, by fat 13.5%, by carbohydrate 58%) and water ad libitum. After an acclimatization period of 5 days, animals were administered PAN (100 mg/kg in saline, intaperitoneally, n = 8) and this continued out to 21 days when they were sacrificed. A sham cohort (n = 4) was injected with an equivalent volume of saline. The number of animals to be entered into the study was determined by assuming a minimum effect size of a 10-fold increase in PAN-associated proteinuria, 80% power, and a false positive rate of 0.05. The sample size was doubled in the PAN cohort to accommodate noise typically associated with transcriptomic analysis. Twenty-four urine samples were obtained on Days 4, 8, 14 and 21 after PAN administration. Urine protein was determined using the Bradford assay. Urine protein obtained from the sham cohort on Days 1 and 21 were averaged. The left kidney was retrieved at sacrifice under ketamine/xylazine (25/5 mg/kg, intraperitoneal) and submitted to histopathologic and transcriptomic analysis.
2.2. Glomerular Morphometry
Ten randomly selected glomeruli per kidney stained with periodic acid–Schiff (PAS) stains were photographed under a light microscope at 40× magnification by an observer (ML) blinded to the groups. Areas of the glomerulus, Bowman space, and Bowman’s capsule were determined using ImageJ and expressed as μm2. Glomerular morphometric measurements for each kidney represented the average of 10 measurements within that kidney.
2.3. Collagen Analysis
At sacrifice, the left kidney was retrieved for transcriptomic and histopathologic analyses. RNA was isolated from renal tissue using the RNeasy® Mini Kit by Qiagen (Hilden, Germany) following manufacturer protocol for tissue RNA isolation. Homogenization was performed by a Next-Advance (Rensselaer, New York, NY, USA) Bullet-Blender Storm 24 bead homogenizer with sterile Next-Advance 1.0 mm diameter zirconium-oxide beads. RNA concentration and quality assured with a thermo-scientific (ThermoFisher Scientific, Waltham, MA, USA) NanoDrop Lite spectrophotometer. Samples were diluted to the same approximate concentration and converted into cDNA with the Applied Biosystems (ThermoFisher Scientific, Waltham, MA, USA) High Capacity cDNA Reverse Transcription Kit following manufacturer protocol. Quantitative polymerase chain reaction (qPCR) was performed on sample cDNA in triplicate with the Applied Biosystems (ThermoFisher Scientific, Waltham, MA, USA) TaqManTM Fast Advanced Master Mix following manufacturer’s protocol. Analysis was performed for collagen type 1 alpha chain 1 (COL1A1) and collagen type 3 alpha 1 chain (COL3A1) and were normalized by the housekeeping gene peptidylprolyl isomerase A (PPIA). Commercially available and validated TaqManTM probes were used for COL1A1 (Thermofisher, Waltham, MA, USA; Mm00801666_g1), COL3A1 (Thermofisher, Waltham, MA, USA, Mm00802300_m1), and PPIA (Thermofisher, Waltham, MA, USA, Mm02342430_g1). All qPCR was run on an Applied Biosystems QuantStudio 3 Real-Time PCR system. Renal homogenates were subjected to analysis for COL1A1, COL3A1 and peptidylprolyl isomerase A (housekeeping gene) mRNA. qPCR was performed on a Thermofisher Quant-Studio 3 Real-Time PCR system, each sample was diluted three-fold, and qPCR reaction was performed in triplicate for all tissue samples.
Picrosirius red (PSR)-stained renal sections were analyzed (25×) under circular-polarized microscopy to observe accumulation of collagen and to identify subtype based on birefringence pattern [
15,
16]. Peroxidase 3, 3′-diaminobenzidine (DAB) immunohistochemistry was performed with a rabbit anti collagen type 3 primary antibody from MyBioSource (San Diego, CA, USA) and SignalStain
® Boost IHC Detection Reagent (HRP, Rabbit) #8114 by Cell Signaling (Danvers, MA, USA) acting as a secondary antibody. All Images (25×) were taken with a Leitz (Leica-Microsystems; Wetzlar, Germany) Laborlux D light microscope and AmScope (Irvine, CA, USA) FMA050 camera.
2.4. Gene Ontology Network Analysis
HumanBase [
17] was used to build glomerular (G) and tubular (T)
COL3A1 transcriptomic networks. Network analysis was restricted to 51 elements each, inclusive of
COL3A1, with a minimum interaction confidence of 0.01. The Jaccard–Tanimoto similarity index was used to calculate common elements within the two compartments:
Data are expressed as average ± standard error of mean. Between group (sham vs. PAN) differences were calculated using analysis of variance followed by Tukey’s post-hoc test. A p-value < 0.05 was assumed to be significant. A Pearson product moment (r) was calculated as the square root of the correlation coefficient.
3. Results
Consistent with previous reports [
11,
12], administration of PAN was associated with a robust increase in urine protein with an observed peaked at ~Day 14 (
Figure 1). In fact, Day 14 urine protein levels were ~236-fold greater than that of the sham cohort (
p < 0.01). By Day 21, the urine protein level had decreased although it was still significantly elevated (~10-fold,
p = 0.016) compared to the sham cohort.
As described previously by Liu and colleagues [
12], histopathological analysis of the kidney showed hypertrophy of the glomerulus in the PAN cohort. Accompanying the increase in glomerular area was the expansion of the Bowman’s capsule. The area of the Bowman’s space, calculated as the difference in areas between the Bowman’s capsule and glomerulus, was also increased in the PAN cohort (
Figure 2).
Levels of
COL1A1 and
COL3A1 mRNA, which code for collagen type I and collagen type III, respectively, were evaluated in renal homogenates on Day 21. There was no difference (
p = 0.74) in renal
COL1A1 mRNA levels between the sham and the PAN cohort (data not shown). By contrast, renal
COL3A1 mRNA level was elevated ~4-fold (
p < 0.05 vs. sham) in the PAN cohort (
Figure 3). Correlation between Day 21 renal
COL3A1 mRNA level and urine protein returned a significant (
p < 0.01) and direct (r = 0.8) association (
Figure 3).
Next, it was determined whether the increased transcriptomic
COL3A1 level was associated with collagen type III deposition, and, if so, whether the deposition was glomerular, tubulointerstitial, or both. Polarized light microscopy was utilized in PSR-stained renal sections to identify the type and location of collagen. As seen in
Figure 4, a yellow-green birefringence pattern largely confined to the glomerulus was observed in the PSR-stained renal sections. This pattern is consistent with the presence of collagen type III [
15,
16].
Indeed, immunohistochemical analysis indicated deposition of collagen type III restricted to the glomerular mesangium (
Figure 5).
Since the tubulointerstitial space was largely free of collagen type III deposition, a gene ontology-based network analysis was conducted to determine the relative strengths of the
COL3A1 glomerular and tubulointerstitial transcriptomic networks. As seen in
Figure 6, the glomerular
COL3A1 transcriptome is relatively strong with an average strength of 0.8 ± 0.08, whereas the tubulointerstitial
COL3A1 interactome is relatively weak with an average strength of 0.56 ± 0.01. Furthermore, the Jaccard–Tannimoto similarity index between the glomerular (G) and tubular (T)
COL3A1 signaling elements was 5.1%, suggesting a relatively small overlap between elements within these compartments.
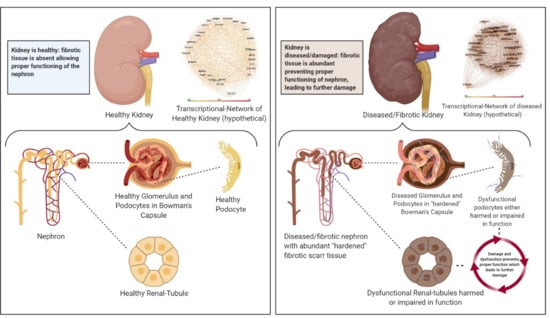
4. Discussion
The PAN model of proteinuric kidney disease is associated with a robust increase in in urine protein and glomerular remodeling including glomerular hypertrophy and expansion of both the Bowman’s capsule and the Bowman’s space. The increase in renal COL3A1 mRNA is directly associated with the increase in urine protein. Collagen type III deposition is restricted to the glomerulus which may be explained at least in part by a robust COL3A1 transcriptomic network in that compartment.
Proteinuria, a marker of renal dysfunction, can occur secondary to diabetes, metabolic syndrome, and other diseases including minimal change disease, FSGS, membraneous nephropathy, and immunoglobulin A nephropathy [
1,
2,
4,
5,
6]. Ultra-rare diseases such as collagenofibrotic glomerulopathy, also known as a collagen type III kidney disease, and nail-patella syndrome are also accompanied by proteinuria [
7,
8]. The typical sequence of renal pathophysiology in proteinuric kidney disease is proteinuria, glomerulosclerosis, tubular injury followed by deposition of matrix within the tubulointerstitial space [
18]. Glomerular and tubulointerstitial matrix components typically comprise collagens with the isoform depending on the disease type [
4,
5,
6,
7,
8]. Collagen type III disorders are fortunately ultra-rare but most often present in childhood. Proteinuria is the typical manifestation, with progression to ESRD in approximately 10 years. The serum precursor collagen type III protein is elevated in the circulation, albeit the gold-standard for diagnosis remains renal biopsy. Collagenofibrotic glomerulopathy is characterized by collagen type III accumulation in subendothelial aspects of capillary walls and the mesangial matrix. On the other hand, nail-patella syndrome, also accompanied by proteinuria, is accompanied by collagen type III accumulation within the glomerular basement membrane. While matrix deposition within the glomerulus does suggest significant pathology, a number of studies [
9,
10] suggests that deposition of matrix in the extraglomerular space i.e., the tubulointerstititum is associated with worse prognosis and an accelerated path toward the need for renal replacement therapy. This is most likely at least in part due to the pivotal nature of tubules in maintaining ionic homeostasis and fluid balance.
In the present study, administration of PAN to the sensitive Wistar rat [
11,
12] was associated with a robust increase in proteinuria and profound remodeling of the glomerulus. Indeed, these data are consistent with previous findings from this laboratory reporting a direct correlation between an expanding Bowman’s space and both proteinuria and albuminuria [
12]. Although delineating the exact mechanism of PAN-induced nephropathy was not the goal of this study, previous reports [
19,
20] that PAN administration is associated with glomerular epithelial cell (GEC) toxicity [
19,
20]. Patchy detachment of the GEC layer from the glomerular basement membrane has been demonstrated after PAN treatment, which is accompanied by diffuse leakage of serum proteins [
11,
19,
20]. Surviving GECs undergo an epithelial to mesenchymal transition. Repeat sampling of renal tissue from PAN-administered rats demonstrates abnormal expression and deposition of fibronectin, laminin and collagen, matrix components, in the glomerulus leading to glomerulosclerosis. [
21].
The salient feature of this study is the finding that PAN-induced proteinuria correlates with increasing
COL3A1 mRNA expression level. To the best of our knowledge, this is the first study describing a relation between proteinuria and transcriptomic upregulation of
COL3A1 which codes for collagen type III. Although this is a finding made in a nonclinical PAN model of proteinuric kidney disease, if clinically translatable, it assumes significance in that urine protein level becomes a noninvasive biomarker of renal
COL3A1 mRNA and perhaps renal collagen type III deposition. Identification of such a non-invasive biomarker can inform disease status without the need for a biopsy. Consistent with the transcriptomic data, both PSR polarized microscopy and immunohistochemical analysis showed collagen type III expression. In fact, the use of polarized microscopy pointed to the presence of thin fiber collagen type III which appears yellow-green [
15,
16]. Consistent with the absence of increased
COL1A1 mRNA expression level, no red-yellow birefringence indicative collagen type I was observed.
A second salient observation in this model was the localization of collagen type III within the glomerulus. Expression was focal with not all glomeruli exhibiting collagen deposition. There was little if any collagen type III deposition within the tubulointerstitium. This is significant in that tubulointerstitial scarring in proteinuric kidney disease is associated with poorer prognosis [
9,
10,
18]. A potential explanation for this phenomenon could lie within transcriptomic differences in the
COL3A1 network with these compartments. Indeed, gene ontology-based network analysis using HumanBase spoke to the differential strengths of the
COL3A1 network within the glomerular and tubular compartments. HumanBase [
15] constructs maps of interacting signaling networks specific based on cell- or tissue-type and based on empirical data collated from a large body of published literature. Gene ontology-driven transcriptomic network analysis revealed a relatively strong
COL3A1 network within the glomerulus but a relatively weaker one within the tubulointerstitium potentially restricting matrix deposition to the glomerular compartment.
The Jaccard index is estimates the similarity or diversity of sample sets [
22]. The Jaccard coefficient is the ratio of the intersection set to the union set. Of significance was the finding of only a 5% overlap between the
COL3A1 signaling components within these two compartments. These data might have ramifications for development of drugs that neutralize this network in that they may be effective against glomerular scarring only.
This study does have several weaknesses. First, rodent models of proteinuric kidney disease do not fully replicate the human syndrome. Unlike rodent models, left untreated, humans with proteinuric kidney disease do not typically exhibit spontaneous decrease in urine protein. Second glomerular morphometry and collagen expression were measured only at sacrifice on Day 21 and may not reflect pathology at earlier timepoints. Additional studies would be required to profile the time-dependent nature of glomerular remodeling. A common feature between rodent models and human proteinuric kidney disease is that glomerular filtration rate is not the most sensitive marker of disease progression with most clinical trials therefore using proteinuria or urine protein to urine creatinine ratios as a measure of renal dysfunction or therapeutic benefit [
2].
This report serves to highlight the potential of urine protein as a noninvasive biomarker of glomerular COL3A1 upregulation. Furthermore, the PAN model of proteinuric kidney disease mimics in part renal collagen type III disorders and can serve as a potential platform for screening of prospective therapies. Results from this study also inform the therapeutic potential of drugs targeting the glomerular COL3A1 network.