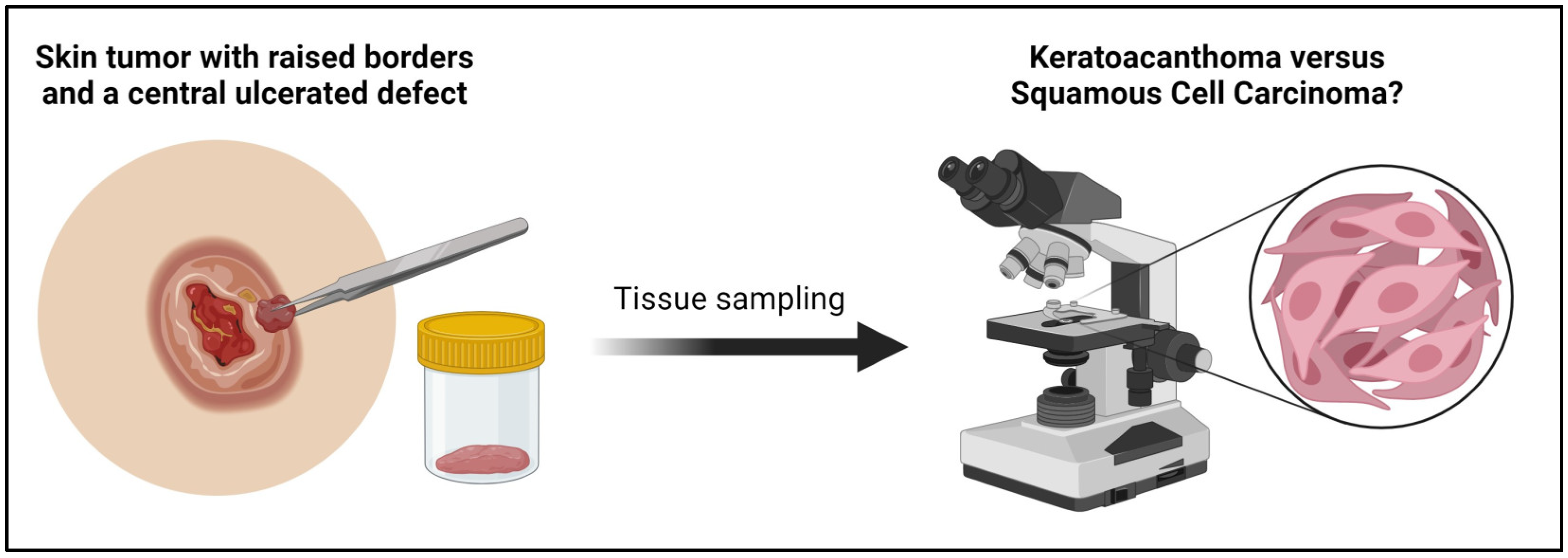
Keratoacanthoma versus Squamous-Cell Carcinoma: Histopathological Features and Molecular Markers
Abstract
1. Introduction: Definition and Epidemiology
1.1. Basic Histopathologic Features of Keratoacanthoma
1.2. Histologic Phases of Keratoacanthoma
1.2.1. Proliferation Phase
1.2.2. Maturation Phase
1.2.3. Regression Phase
1.3. Regression of Keratoacanthoma
1.4. Molecular Pathways Contributing to the Formation of Keratoacanthoma
1.5. Pitfalls in the Diagnosis of Keratoacanthoma
2. Differential Diagnosis of Keratoacanthoma
3. Distinguishing Keratoacanthoma from Squamous-Cell Carcinoma
3.1. Histologic Features and Key Criteria of Keratoacanthoma and Squamous-Cell Carcinoma
3.2. Immunohistologic and Immunocytologic Markers Distinguishing Keratoacanthoma and Squamous-Cell Carcinoma
3.2.1. CK17 and Ki67
3.2.2. Anti-P2X7
3.2.3. CD123
3.3. Genetics and Molecular Alterations in Keratoacanthoma versus Squamous-Cell Carcinoma
3.4. Malignant Transformation of Keratoacanthoma to Squamous-Cell Carcinoma
3.5. Keratoacanthoma versus Squamous-Cell Carcinoma in CAP Protocols and WHO Books
4. Treatment of Keratoacanthoma versus Squamous-Cell Carcinoma
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kwiek, B.; Schwartz, R.A. Keratoacanthoma (KA): An update and review. J. Am. Acad. Dermatol. 2016, 74, 1220–1233. [Google Scholar] [CrossRef] [PubMed]
- Hutchinson, J. The crateriform ulcer of the face: A form of epithelial cancer. Trans. Pathol. Soc. Lond. 1889, 40, 275–281. [Google Scholar]
- Carr, R.A.; Houghton, J.P. Histopathologists’ approach to keratoacanthoma: A multisite survey of regional variation in Great Britain and Ireland. J. Clin. Pathol. 2014, 67, 637–638. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, R.A. The keratoacanthoma: A review. J. Surg. Oncol. 1979, 12, 305–317. [Google Scholar] [CrossRef]
- Vergilis-Kalner, I.J.; Kriseman, Y.; Goldberg, L.H. Keratoacanthomas: Overview and comparison between Houston and minneapolis experiences. J. Drugs Dermatol. 2010, 9, 117–121. [Google Scholar]
- Misago, N.; Inoue, T.; Koba, S.; Narisawa, Y. Keratoacanthoma and other types of squamous cell carcinoma with crateriform architecture: Classification and identification. J. Dermatol. 2013, 40, 443–452. [Google Scholar] [CrossRef]
- Takai, T. Advances in histopathological diagnosis of keratoacanthoma. J. Dermatol. 2017, 44, 304–314. [Google Scholar] [CrossRef]
- Mandrell, J.C.; Santa Cruz, D.J. Keratoacanthoma: Hyperplasia, benign neoplasm, or a type of squamous cell carcinoma? Semin. Diagn. Pathol. 2009, 26, 150–163. [Google Scholar] [CrossRef]
- Calonje, E.; Jones, E.W. Intravascular Spread of Keratoacanthoma an Alarming but Benign Phenomenon. Am. J. Dermatopathol. 1992, 14, 414–417. [Google Scholar] [CrossRef]
- Ko, C.J. Keratoacanthoma: Facts and controversies. Clin. Dermatol. 2010, 28, 254–261. [Google Scholar] [CrossRef]
- Rinker, M.H.; Fenske, N.A.; Scalf, L.A.; Glass, L.F. Histologic variants of squamous cell carcinoma of the skin. Cancer Control 2001, 8, 354–363. [Google Scholar] [CrossRef] [PubMed]
- Miedzinski, F.; Kozakiewicz, J. Keratoacanthoma centrifugum—A special variety of keratoacanthoma. Der Hautarzt Z. fur Dermatol. Venerol. und Verwandte Geb. 1962, 13, 348–352. [Google Scholar]
- Ra, S.H.; Su, A.; Li, X.; Zhou, J.; Cochran, A.J.; Kulkarni, R.P.; Binder, S.W. Keratoacanthoma and squamous cell carcinoma are distinct from a molecular perspective. Mod. Pathol. 2015, 28, 799–806. [Google Scholar] [CrossRef]
- Georgescu, T.-A.; Oproiu, A.M.; Rădăşan, M.G.; Dumitru, A.V.; Costache, D.; Pătraşcu, O.M.; Lăzăroiu, A.M.; Chefani, A.E.; Sajin, M.; Costache, M. Keratoacanthoma centrifugum marginatum: An unusual clinical and histopathological diagnostic pitfall. Rom. J. Morphol. Embryol. 2017, 58, 561–565. [Google Scholar] [PubMed]
- Liu, J.; Xiao, Q.; Xiao, J.; Niu, C.; Li, Y.; Zhang, X.; Zhou, Z.; Shu, G.; Yin, G. Wnt/β-catenin signalling: Function, biological mechanisms, and therapeutic opportunities. Signal Transduct. Target. Ther. 2022, 7, 3. [Google Scholar] [CrossRef]
- Zito, G.; Saotome, I.; Liu, Z.; Ferro, E.G.; Sun, T.Y.; Nguyen, D.X.; Bilguvar, K.; Ko, C.J.; Greco, V. Spontaneous tumour regression in keratoacanthomas is driven by Wnt/retinoic acid signalling cross-talk. Nat. Commun. 2014, 5, 3543. [Google Scholar] [CrossRef]
- Williams, R.; Westgate, G.E.; Pawlus, A.D.; Sikkink, S.K.; Thornton, M.J. Age-related changes in female scalp dermal sheath and dermal fibroblasts: How the hair follicle environment impacts hair aging. J. Investig. Dermatol. 2021, 141, 1041–1051. [Google Scholar] [CrossRef]
- Hu, W.; Cook, T.; Oh, C.W.; Penneys, N.S. Expression of the cyclin-dependent kinase inhibitor p27 in keratoacanthoma. J. Am. Acad. Dermatol. 2000, 42, 473–475. [Google Scholar] [CrossRef]
- Li, W.-R.; Lin, L. Seborrheic keratosis in a young woman: A mimicker of keratoacanthoma. Int. J. Dermatol. Venereol. 2020, 3, 116–117. [Google Scholar] [CrossRef]
- Gleich, T.; Chiticariu, E.; Huber, M.; Hohl, D. Keratoacanthoma: A distinct entity? Exp. Dermatol. 2016, 25, 85–91. [Google Scholar] [CrossRef]
- Karampinis, E.; Kostopoulou, C.; Toli, O.; Marinos, L.; Papadimitriou, G.; Roussaki Schulze, A.V.; Zafiriou, E. Multiple Keratoacanthoma-like Syndromes: Case Report and Literature Review. Medicina 2024, 60, 371. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Wang, K.; Gao, F.; Jensen, T.D.; Li, S.T.; DeAngelis, P.M.; Kølvraa, S.; Proby, C.; Forslund, O.; Bolund, L.; et al. Array comparative genomic hybridization of keratoacanthomas and squamous cell carcinomas: Different patterns of genetic aberrations suggest two distinct entities. J. Investig. Dermatol. 2012, 132, 2060–2066. [Google Scholar] [CrossRef] [PubMed]
- Prieto-Granada, C.; Rodriguez-Waitkus, P. Cutaneous squamous cell carcinoma and related entities: Epidemiology, clinical and histological features, and basic science overview. Curr. Probl. Cancer 2015, 39, 206–215. [Google Scholar] [CrossRef]
- Arnault, J.P.; Wechsler, J.; Escudier, B.; Spatz, A.; Tomasic, G.; Sibaud, V.; Aractingi, S.; Grange, J.-D.; Poirier-Colame, V.; Malka, D.; et al. Keratoacanthomas and Squamous Cell Carcinomas in Patients Receiving Sorafenib. J. Clin. Oncol. 2009, 27, e59–e61. [Google Scholar] [CrossRef]
- Dubauskas, Z.; Kunishige, J.; Prieto, V.G.; Jonasch, E.; Hwu, P.; Tannir, N.M. Cutaneous Squamous Cell Carcinoma and Inflammation of Actinic Keratoses Associated with Sorafenib. Clin. Genitourin. Cancer 2009, 7, 20–23. [Google Scholar] [CrossRef] [PubMed]
- Kent, R.; Glorioso, S.; Nordberg, M.L. A model for cutaneous squamous cell carcinoma in vemurafenib therapy. J. La. State Med. Soc. 2012, 164, 311–313. [Google Scholar]
- Callahan, M.K.; Rampal, R.; Harding, J.J.; Klimek, V.M.; Chung, Y.R.; Merghoub, T.; Wolchok, J.D.; Solit, D.B.; Rosen, N.; Abdel-Wahab, O.; et al. Progression of RAS-mutant leukemia during RAF inhibitor treatment. N. Engl. J. Med. 2012, 367, 2316–2321. [Google Scholar] [CrossRef]
- Nagarajan, P. Differentiating keratoacanthoma from squamous cell carcinoma—In quest of the holy grail. J. Cutan. Pathol. 2020, 47, 418–420. [Google Scholar] [CrossRef] [PubMed]
- Misago, N.; Takai, T.; Toda, S.; Narisawa, Y. The changes in the expression levels of follicular markers in keratoacanthoma depend on the stage: Keratoacanthoma is a follicular neoplasm exhibiting infundibular/isthmic differentiation without expression of CK15. J. Cutan. Pathol. 2014, 41, 437–446. [Google Scholar] [CrossRef]
- Ranglani, H.; Pai, V.V.; Shukla, P. Keratoacanthoma-like cutaneous metastases in a case of squamous cell carcinoma of the tongue. Indian J. Dermatol. Venereol. Leprol. 2019, 85, 568. [Google Scholar] [CrossRef]
- Magalhães, R.F.; Cruvinel, G.T.; Cintra, G.F.; Cintra, M.L.; Palu, A.P.; Ismael, B.; de Moraes, A.M. Diagnosis and follow-up of Keratoacanthoma-like lesions: Clinical-histologic study of 43 cases. J. Cutan. Med. Surg. 2008, 12, 163–173. [Google Scholar] [CrossRef] [PubMed]
- Cabibi, D.; Conway de Macario, E.; Ingrao, S.; Porcasi, R.; Zucco, F.; Macario, A.J.L.; Cappello, F.; Rappa, F. CD1A-positive cells and HSP60 (HSPD1) levels in keratoacanthoma and squamous cell carcinoma. Cell Stress Chaperones 2016, 21, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Leblebici, C.; Pasaoglu, E.; Kelten, C.; Darakci, S.; Dursun, N. Cytokeratin 17 and Ki-67: Immunohistochemical markers for the differential diagnosis of keratoacanthoma and squamous cell carcinoma. Oncol. Lett. 2017, 13, 2539–2548. [Google Scholar] [CrossRef] [PubMed]
- Kalaimani, G.; Rao, U.D.K.; Joshua, E.; Ranganathan, K. E-cadherin Expression in Premalignant Lesions, Premalignant Conditions, Oral Squamous Cell Carcinoma, and Normal Mucosa: An Immunohistochemical Study. Cureus 2023, 15, e44266. [Google Scholar] [CrossRef]
- Puizina-Ivić, N.; Sapunar, D.; Marasović, D.; Mirić, L. An overview of Bcl-2 expression in histopathological variants of basal cell carcinoma, squamous cell carcinoma, actinic keratosis and seborrheic keratosis. Coll. Antropol. 2008, 32 (Suppl. S2), 61–65. [Google Scholar]
- Gaballah, M.A.; Ahmed, R.-A. Diagnostic value of CD10 and Bcl2 expression in distinguishing cutaneous basal cell carcinoma from squamous cell carcinoma and seborrheic keratosis. Pathol. Res. Pract. 2015, 211, 931–938. [Google Scholar] [CrossRef]
- Vasiljevic, N.; Andersson, K.; Bjelkenkrantz, K.; Kjellstrom, C.; Mansson, H.; Nilsson, E.; Landberg, G.; Dillner, J.; Forslund, O. The Bcl-xL inhibitor of apoptosis is preferentially expressed in cutaneous squamous cell carcinoma compared with that in keratoacanthoma. Int. J. Cancer 2009, 124, 2361–2366. [Google Scholar] [CrossRef]
- Scola, N.; Segert, H.M.; Stucker, M.; Altmeyer, P.; Gambichler, T.; Kreuter, A. Ki-67 may be useful in differentiating between keratoacanthoma and cutaneous squamous cell carcinoma. Clin. Exp. Dermatol. 2014, 39, 216–218. [Google Scholar] [CrossRef]
- Connolly, M.; Narayan, S.; Oxley, J.; de Berker, D.A. Immunohistochemical staining for the differentiation of subungual keratoacanthoma from subungual squamous cell carcinoma. Clin. Exp. Dermatol. 2008, 33, 625–628. [Google Scholar] [CrossRef]
- Lammoglia-Ordiales, L.; Toussaint-Caire, S.; Contreras-Barrera, M.; Fonte-Avalos, V.; Rodriguez-Carreon, A.A.; Rivera-Macias, S.; Dominguez-Cherit, J. Assessment of syndecan-1 (CD138) and Ki-67 expression for differentiating keratoacanthoma and squamous cell carcinoma. J. Drugs Dermatol. 2013, 12, e53–e58. [Google Scholar]
- Basta-Juzbasic, A.; Klenkar, S.; Jakic-Razumovic, J.; Pasic, A.; Loncaric, D. Cytokeratin 10 and Ki-67 nuclear marker expression in keratoacanthoma and squamous cell carcinoma. Acta Dermatovenerol. Croat. 2004, 12, 251–256. [Google Scholar] [PubMed]
- Shimizu, T.; Muto, M.; Murakami, T.; Furumoto, H.; Mogami, S.; Asagami, C. Overexpression of p53 protein associated with proliferative activity as evaluated by Ki-67 immunostaining in well-differentiated squamous cell carcinoma of the skin. Dermatology 1997, 195, 224–227. [Google Scholar] [CrossRef] [PubMed]
- Slater, M.; Barden, J.A. Differentiating keratoacanthoma from squamous cell carcinoma by the use of apoptotic and cell adhesion markers. Histopathology 2005, 47, 170–178. [Google Scholar] [CrossRef]
- Fraga, G.R.; Chow, P. Plasmacytoid dendritic cells in keratoacanthoma and squamous cell carcinoma: A blinded study of CD123 as a diagnostic marker. J. Cutan. Pathol. 2020, 47, 17–21. [Google Scholar] [CrossRef] [PubMed]
- Batinac, T.; Zamolo, G.; Coklo, M.; Hadzisejdic, I.; Stemberger, C.; Zauhar, G. Expression of cell cycle and apoptosis regulatory proteins in keratoacanthoma and squamous cell carcinoma. Pathol. Res. Pract. 2006, 202, 599–607. [Google Scholar] [CrossRef]
- Clausen, O.P.; Beigi, M.; Bolund, L.; Kølvraa, S.; Gjersvik, P.J.; Mørk, G.; de Angelis, P.M. Keratoacanthomas frequently show chromosomal aberrations as assessed by comparative genomic hybridization. J. Investig. Dermatol. 2002, 119, 1367–1372. [Google Scholar] [CrossRef]
- Fan, X.; Niu, X.; Wu, Z.; Yao, L.; Chen, S.; Wan, W.; Huang, B.; Qi, R.Q.; Zhang, T. Computer Image Analysis Reveals C-Myc as a Potential Biomarker for Discriminating between Keratoacanthoma and Cutaneous Squamous Cell Carcinoma. BioMed Res. Int. 2022, 2022, 3168503. [Google Scholar] [CrossRef]
- Wrone-Smith, T.; Bergstrom, J.; Quevedo, M.E.; Reddy, V.; Gutierrez-Steil, C.; Nickoloff, B.J. Differential expression of cell survival and cell cycle regulatory proteins in cutaneous squamoproliferative lesions. J. Dermatol. Sci. 1999, 19, 53–67. [Google Scholar] [CrossRef]
- Forslund, O.; Iftner, T.; Andersson, K.; Lindelof, B.; Hradil, E.; Nordin, P.; Stenquist, B.; Kirnbauer, R.; Dillner, J.; de Villiers, E.M.; et al. Cutaneous human papillomaviruses found in sun-exposed skin: Beta-papillomavirus species 2 predominates in squamous cell carcinoma. J. Infect. Dis. 2007, 196, 876–883. [Google Scholar] [CrossRef]
- Bouwes Bavinck, J.N.; Plasmeijer, E.I.; Feltkamp, M.C. Beta-papillomavirus infection and skin cancer. J. Investig. Dermatol. 2008, 128, 1355–1358. [Google Scholar] [CrossRef]
- Ascierto, P.A.; Kirkwood, J.M.; Grob, J.J.; Simeone, E.; Grimaldi, A.M.; Maio, M.; Palmieri, G.; Testori, A.; Marincola, F.M.; Mozzillo, N. The role of BRAF V600 mutation in melanoma. J. Transl. Med. 2012, 10, 85. [Google Scholar] [CrossRef] [PubMed]
- Selmer, J.; Skov, T.; Spelman, L.; Weedon, D. Squamous cell carcinoma and keratoacanthomas are biologically distinct and can be diagnosed by light microscopy: A review. Histopathology 2016, 69, 535–541. [Google Scholar] [CrossRef]
- Guo, Y.J.; Pan, W.W.; Liu, S.B.; Shen, Z.F.; Xu, Y.; Hu, L.L. ERK/MAPK signalling pathway and tumorigenesis. Exp. Ther. Med. 2020, 19, 1997–2007. [Google Scholar] [CrossRef]
- Sharma, P.; Narwal, A.; Kamboj, M. Myriad facades of keratocanthoma: Benignity VS malignancy. J. Oral Biol. Craniofac. Res. 2019, 9, 352–354. [Google Scholar] [CrossRef] [PubMed]
- Burns, C.; Kubicki, S.; Nguyen, Q.-B.; Aboul-Fettouh, N.; Wilmas, K.M.; Chen, O.M.; Doan, H.Q.; Silapunt, S.; Migden, M.R. Advances in Cutaneous Squamous Cell Carcinoma Management. Cancers 2022, 14, 3653. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, E.S.; Karia, P.S.; Besaw, R.; Schmults, C.D. Performance of the American Joint Committee on Cancer Staging Manual, vs the Brigham and Women’s Hospital tumor classification system for cutaneous squamous cell carcinoma. JAMA Dermatol. 2019, 155, 819–825. [Google Scholar] [CrossRef]
- Seethala, R.; Shon, W.; Balzer, B.; Duvvuri, U.; Gharavi, N.; Lydiatt, W. Protocol for the Examination of Specimens from Patients with Cutaneous Squamous Cell Carcinoma of the Head and Neck; College of American Pathologists: New Orleans, LA, USA, 2022. [Google Scholar]
- Carr, R.A.; Zalaudek, I.; Craig, P. Keratoacanthoma. In Skin Tumours; Scolyer, R., Messina, J., Eds.; International Agency for Research on Cancer: Lyon, France, 2023. [Google Scholar]
- Ambur, A.; Clark, A.; Nathoo, R. An Updated Review of the Therapeutic Management of Keratoacanthomas. J. Clin. Aesthetic Dermatol. 2022, 15, S16. [Google Scholar]
- Di Lernia, V.; Ricci, C.; Albertini, G. Spontaneous regression of keratoacanthoma can be promoted by topical treatment with imiquimod cream. J. Eur. Acad. Dermatol. Venereol. 2004, 18, 626–629. [Google Scholar] [CrossRef]
- Plachouri, K.M.; Mulita, F.; Bousis, D.; Tchabashvili, L.; Liolis, E.; Kaplanis, C.; Perdikaris, I.; Iliopoulos, F.; Verras, G.I.; Tolias, V. Successful treatment of a keratoacanthoma in a young patient with the application of topical 5% imiquimod cream. Clin. Case Rep. 2021, 9, e04920. [Google Scholar] [CrossRef]
- Winge, M.C.G.; Kellman, L.N.; Guo, K.; Tang, J.Y.; Swetter, S.M.; Aasi, S.Z.; Sarin, K.Y.; Chang, A.L.S.; Khavari, P.A. Advances in cutaneous squamous cell carcinoma. Nat. Rev. Cancer 2023, 23, 430–449. [Google Scholar] [CrossRef]
- Tisack, A.; Fotouhi, A.; Fidai, C.; Friedman, B.J.; Ozog, D.; Veenstra, J. A clinical and biological review of keratoacanthoma*. Br. J. Dermatol. 2021, 185, 487–498. [Google Scholar] [CrossRef] [PubMed]
- Di Nardo, L.; Pellegrini, C.; Di Stefani, A.; Del Regno, L.; Sollena, P.; Piccerillo, A.; Longo, C.; Garbe, C.; Fargnoli, M.C.; Peris, K. Molecular genetics of cutaneous squamous cell carcinoma: Perspective for treatment strategies. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 932–941. [Google Scholar] [CrossRef] [PubMed]
- Gellrich, F.; Hüning, S.; Beissert, S.; Eigentler, T.; Stockfleth, E.; Gutzmer, R.; Meier, F. Medical treatment of advanced cutaneous squamous-cell carcinoma. J. Eur. Acad. Dermatol. Venereol. 2019, 33, 38–43. [Google Scholar] [CrossRef] [PubMed]

| Neoplastic Conditions | Infectious Diseases | Inflammatory Diseases |
|---|---|---|
| SCC (infundibular) Bowen disease Verrucous carcinoma Seborrheic keratosis Actinic keratosis KA-like SCC “KA with malignant transformation” Large-cell lymphomas Amelanotic melanoma | Sporotrichosis Cryptococcosis Blastomycosis Molluscum contagiosum | Hypertrophic form of discoid lupus erythematosus Lichen planus Halogenoderma Prurigo nodularis |
| IHC Marker | Squamous-Cell Carcinoma | Keratoacanthoma |
|---|---|---|
| Ki67 | High proliferation index (diffuse staining) | Low proliferation index (localized to the base) |
| CK17 [33] | Positive | Positive (central staining pattern) |
| E-cadherin [34] | Loss or reduced expression | Positive (retained) |
| BCL2 [35] | Typically, absent or weak | Positive |
| CD10 [36] | Negative | May be positive (localized to the base) |
| P16 | Frequently overexpressed (aberrant pattern) in HPV-related SCC | Patchy (mosaic pattern) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Published by MDPI on behalf of the European Society of Dermatopathology. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bahmad, H.F.; Stoyanov, K.; Mendez, T.; Trinh, S.; Terp, K.; Qian, L.; Alexis, J. Keratoacanthoma versus Squamous-Cell Carcinoma: Histopathological Features and Molecular Markers. Dermatopathology 2024, 11, 272-285. https://doi.org/10.3390/dermatopathology11040029
Bahmad HF, Stoyanov K, Mendez T, Trinh S, Terp K, Qian L, Alexis J. Keratoacanthoma versus Squamous-Cell Carcinoma: Histopathological Features and Molecular Markers. Dermatopathology. 2024; 11(4):272-285. https://doi.org/10.3390/dermatopathology11040029
Chicago/Turabian StyleBahmad, Hisham F., Kalin Stoyanov, Teresita Mendez, Sally Trinh, Kristy Terp, Linda Qian, and John Alexis. 2024. "Keratoacanthoma versus Squamous-Cell Carcinoma: Histopathological Features and Molecular Markers" Dermatopathology 11, no. 4: 272-285. https://doi.org/10.3390/dermatopathology11040029
APA StyleBahmad, H. F., Stoyanov, K., Mendez, T., Trinh, S., Terp, K., Qian, L., & Alexis, J. (2024). Keratoacanthoma versus Squamous-Cell Carcinoma: Histopathological Features and Molecular Markers. Dermatopathology, 11(4), 272-285. https://doi.org/10.3390/dermatopathology11040029







