Physiotherapists and Osteopaths’ Attitudes: Training in Management of Temporomandibular Disorders
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lavangie, P.; Norkin, C. Joint Structure and Function: A Comprehensive Analysis; F. A. Davis Company: Philadelphia, PA, USA, 2010. [Google Scholar]
- de Toledo, E.G., Jr.; Silva, D.P.; de Toledo, J.A.; Salgado, I.O. The interrelationship between dentistry and physiotherapy in the treatment of temporomandibular disorders. J. Contemp. Dent. Pract. 2012, 13, 579–583. [Google Scholar] [CrossRef] [PubMed]
- de Leeuw, R.; Glasser, G. Orofacial Pain: Guidelines for Classification, Assessment, and Management, 5th ed.; Quintessence Publ. Co.: Chicago, IL, USA, 2013. [Google Scholar]
- Wright, E.F.; North, S.L. Management and treatment of temporomandibular disorders: A clinical perspective. J. Man Manip. Ther. 2009, 17, 247–254. [Google Scholar] [CrossRef] [PubMed]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group†. J. Oral Facial Pain Headache 2014, 28, 6–27. [Google Scholar] [CrossRef]
- Farooq, M.N.; Malik, M.; Khalid, F.; Raja, I.; Shah, A.U. Awareness of dental consultants about physiotherapy management of temporomandibular joint disorders. Rehman J. Health Sci. 2021, 3, 72–76. [Google Scholar] [CrossRef]
- Chang, S.W.; Chuang, C.Y.; Li, J.R.; Lin, C.Y.; Chiu, C.T. Treatment effects of maxillary flat occlusal splints for painful clicking of the temporomandibular joint. Kaohsiung J. Med. Sci. 2010, 26, 299–307. [Google Scholar] [CrossRef]
- Kraus, S. Temporomandibular disorders, head and orofacial pain: Cervical spine considerations. Dent. Clin. N. Am. 2007, 51, 161–193. [Google Scholar] [CrossRef]
- de Leeuw, R. Orofacial Pain-Giudelines for the Assessment, Diagnosis, and Management, 4th ed.; Quintessence: Berlin, Germany, 2008. [Google Scholar]
- Zieliński, G.; Suwała, M.; Ginszt, M.; Szkutnik, J.; Majcher, P. Bioelectric activity of mastication muscles and the functional impairment risk groups concerning the masticatory muscles. Acta Bioeng. Biomech. 2018, 20, 161–166. [Google Scholar] [CrossRef]
- Saccomanno, S.; Laganà, D.; Mastrapasqua, R.; Giancaspro, S.; Manenti, R.J.; Saran, S. The relationship between TMJ symptoms and orthodontic treatments: A survey on 236 orthodontic patients. J. Biol. Regul. Homeost. Agents 2021, 35 (Suppl. S1), 197–204. [Google Scholar] [CrossRef]
- Armijo-Olivo, S.L.; Gadotti, I.C. Chapter 4: Temporomandibular disorders. In Pathology and Intervention in musculoskeletal Rehabilitation, 2nd ed.; Magee, D.J., Zachazewski, J.E., Quillen, W.S., Manske, R.C., Eds.; Elsevier: Maryland Heights, MO, USA, 2016; pp. 119–156. [Google Scholar]
- Saccomanno, S.; Saran, S.; Vanella, V.; Mastrapasqua, R.F.; Capogreco, M.; Carretta, G.; Pirino, A.; Scoppa, F. Is there any correlation between malocclusion, temporomandibular disorders, and systemic disease? The importance of differential diagnosis. J. Biol. Regul. Homeost. Agents 2022, 36 (Suppl. S1), 149–156. [Google Scholar]
- Saccomanno, S.; Saran, S.; Carretta, G.; Mastrapasqua, R.F.; Vanella, V.; Pirino, A.; Scoppa, F. The relationship between TMJ symptoms and gut disease. J. Biol. Regul. Homeost. Agents 2022, 36, 175–182. [Google Scholar]
- Guarda-Nardini, L.; Pavan, C.; Arveda, N.; Ferronato, G.; Manfredini, D. Psychometric features of temporomandibular disorders patients in relation to pain diffusion, location, intensity and duration. J. Oral Rehabil. 2012, 39, 737–743. [Google Scholar] [CrossRef] [PubMed]
- Magnusson, T.; Egermark, I.; Carlsson, G.E. A longitudinal epidemiologic study of signs and symptoms of temporomandibular disorders from 15 to 35 years of age. J. Orofac. Pain 2000, 14, 310–319. [Google Scholar] [PubMed]
- Yu, S.; Xing, X.; Liang, S.; Ma, Z.; Li, F.; Wang, M.; Li, Y. Locally synthesized estrogen plays an important role in the development of TMD. Med. Hypotheses 2009, 72, 720–722. [Google Scholar] [CrossRef] [PubMed]
- Thilander, B.; Rubio, G.; Pena, L.; de Mayorga, C. Prevalence of temporomandibular dysfunction and its association with malocclusion in children and adolescents: An epidemiologic study related to specified stages of dental development. Angle Orthod. 2002, 72, 146–154. [Google Scholar] [CrossRef] [PubMed]
- Shedden Mora, M.; Weber, D.; Borkowski, S.; Rief, W. Nocturnal masseter muscle activity is related to symptoms and somatization in temporomandibular disorders. J. Psychosom. Res. 2012, 73, 307–312. [Google Scholar] [CrossRef]
- Perkins, J.A.; Sie, K.C.; Milczuk, H.; Richardson, M.A. Airway management in children with craniofacial anomalies. Cleft Palate Craniofac. J. 1997, 34, 135–140. [Google Scholar] [CrossRef]
- Cortese, S.; Mondello, A.; Galarza, R.; Biondi, A. Postural alterations as a risk factor for temporomandibular disorders. Acta Odontol. Lat. 2017, 30, 57–61. [Google Scholar]
- Gungormus, Z.; Erciyas, K. Evaluation of the relationship between anxiety and depression and bruxism. J. Int. Med. Res. 2009, 37, 547–550. [Google Scholar] [CrossRef]
- Robinson, J.L.; Johnson, P.M.; Kister, K.; Yin, M.T.; Chen, J.; Wadhwa, S. Estrogen signaling impacts temporomandibular joint and periodontal disease pathology. Odontology 2020, 108, 153–165. [Google Scholar] [CrossRef]
- Ryan, J.; Akhter, R.; Hassan, N.; Glen Hilton, G.; Wickham, J.; Ibaragi, S. Epidemiology of Temporomandibular Disorder in the General Population: A Systematic Review. Adv. Dent. Oral Health 2019, 10, 555787. [Google Scholar] [CrossRef]
- Dalanon, J.; Ugalde, R.B.; Catibod, L.D.; Macaso, J.M.L.; Okura, K.; Matsuka, Y. Comparative analysis of education, awareness, and knowledge of dentists and physical therapists in the treatment of temporomandibular disorders. Cranio 2020, 28, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Silveira, A.; Gadotti, I.C.; Armijo-Olivo, S.; Biasotto-Gonzalez, D.A.; Magee, D. Jaw dysfunction is associated with neck disability and muscle tenderness in subjects with and without chronic temporomandibular disorders. Biomed. Res. Int. 2015, 2015, 512792. [Google Scholar] [CrossRef] [PubMed]
- Garrigós-Pedrón, M.; Elizagaray-García, I.; Domínguez-Gordillo, A.A.; Del-Castillo-Pardo-de-Vera, J.L.; Gil-Martínez, A. Temporomandibular disorders: Improving outcomes using a multidisciplinary approach. J. Multidiscip. Healthc. 2019, 3, 733–747, Erratum in J. Multidiscip. Healthc. 2019, 12. [Google Scholar] [CrossRef] [PubMed]
- Gil-Martínez, A.; Paris-Alemany, A.; López-de-Uralde-Villanueva, I.; La Touche, R. Management of pain in patients with temporomandibular disorder (TMD): Challenges and solutions. J. Pain Res. 2018, 16, 571–587. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira Viana, M.; da Cunha Olegario, N.B.; de Oliveira Viana, M.; da Silva, G.P.F.; Santos, J.L.F.; de Carvalho, S.T.R.F. Effect of physical theraphy protocol on the health-related quality of life of patients with temporomandibular disorder. Fisioter. Em Mov. 2016, 29, 507–514. [Google Scholar] [CrossRef]
- Armijo-Olivo, S.; Pitance, L.; Singh, V.; Neto, F.; Thie, N.; Michelotti, A. Effectiveness of Manual Therapy and Therapeutic Exercise for Temporomandibular Disorders: Systematic Review and Meta-Analysis. Phys. Ther. 2016, 96, 9–25. [Google Scholar] [CrossRef]
- Snyder, M.J.; Hawks, M.K.; Moss, D.A.; Crawford, P.F., 3rd. Integrative Medicine: Manual Therapy. FP Essent. 2021, 505, 11–17. [Google Scholar]
- Brantingham, J.W.; Cassa, T.K.; Bonnefin, D.; Pribicevic, M.; Robb, A.; Pollard, H.; Tong, V.; Korporaal, C. Manipulative and multimodal therapy for upper extremity and temporomandibular disorders: A systematic review. J. Manip. Physiol. Ther. 2013, 36, 143–201. [Google Scholar] [CrossRef]
- Degenhardt, B.F.; Darmani, N.A.; Johnson, J.C.; Towns, L.C.; Rhodes, D.C.; Trinh, C.; McClanahan, B.; DiMarzo, V. Role of osteopathic manipulative treatment in altering pain biomarkers: A pilot study. J. Am. Osteopath. Assoc. 2007, 107, 387–400. [Google Scholar]
- Kimos, P.; Biggs, C.; Mah, J.; Heo, G.; Rashiq, S.; Thie, N.M.; Major, P.W. Analgesic action of gabapentin on chronic pain in the masticatory muscles: A randomized controlled trial. Pain 2007, 127, 151–160. [Google Scholar] [CrossRef]
- Ouanounou, A.; Goldberg, M.; Haas, D.A. Pharmacotherapy in Temporomandibular Disorders: A Review. J. Can. Dent. Assoc. 2017, 83, h7. [Google Scholar] [PubMed]
- Melis, M. The role of physical therapy for the treatment of temporomandibular disorders. J. Orthod. Sci. 2013, 2, 113–114. [Google Scholar] [CrossRef] [PubMed]
- Gesslbauer, C.; Vavti, N.; Keilani, M.; Mickel, M.; Crevenna, R. Effectiveness of osteopathic manipulative treatment versus osteopathy in the cranial field in temporomandibular disorders—A pilot study. Disabil. Rehabil. 2018, 40, 631–636. [Google Scholar] [CrossRef]
- Jäkel, A.; von Hauenschild, P. Therapeutic effects of cranial osteopathic manipulative medicine: A systematic review. J. Am. Osteopath. Assoc. 2011, 111, 685–693. [Google Scholar]
- Easterbrook, S.; Keys, J.; Talsma, J.; Pierce-Talsma, S. Osteopathic Manipulative Treatment for Temporomandibular Disorders. J. Am. Osteopath. Assoc. 2019, 119, e29–e30. [Google Scholar] [CrossRef] [PubMed]
- Gauer, R.L.; Semidey, M.J. Diagnosis and treatment of temporomandibular disorders. Am. Fam. Physician. 2015, 91, 378–386. [Google Scholar] [PubMed]
- Calixtre, L.B.; Moreira, R.F.; Franchini, G.H.; Alburquerque-Sendín, F.; Oliveira, A.B. Manual therapy for the management of pain and limited range of motion in subjects with signs and symptoms of temporomandibular disorder: A systematic review of randomised controlled trials. J. Oral Rehabil. 2015, 42, 847–861. [Google Scholar] [CrossRef]
- Nahian, A.; Ünal, M.; Mathew, J., Jr. Osteopathic Manipulative Treatment: Facial Muscle Energy, Direct MFR, and BLT Procedure—For TMJ Dysfunction. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Jiang, X.; Fan, S.; Cai, B.; Fang, Z.Y.; Xu, L.L.; Liu, L.K. Mandibular manipulation technique followed by exercise therapy and occlusal splint for treatment of acute anterior TMJ disk displacement without reduction. Shanghai Kou Qiang Yi Xue 2016, 25, 570–573. [Google Scholar]
- Klasser, G.D.; Greene, C.S. Oral appliances in the management of temporomandibular disorders. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2009, 107, 212–223. [Google Scholar] [CrossRef]
- Alajbeg, I.; Živković, K.; Gikić, M. Uloga Stabilizacijske Udlage U Liječenju Temporomandibularnih Poremećaja [The Role of Stabilization Splint In The Treatment of Temporomandibular Disorders]. Acta Med. Croat. 2015, 69, 33–43. [Google Scholar]
- Ginszt, M.; Zieliński, G.; Berger, M.; Szkutnik, J.; Bakalczuk, M.; Majcher, P. Acute Effect of the Compression Technique on the Electromyographic Activity of the Masticatory Muscles and Mouth Opening in Subjects with Active Myofascial Trigger Points. Appl. Sci. 2020, 10, 7750. [Google Scholar] [CrossRef]
- Ismail, F.; Demling, A.; Hessling, K.; Fink, M.; Stiesch-Scholz, M. Short-term efficacy of physical therapy compared to splint therapy in treatment of arthrogenous TMD. J. Oral Rehabil. 2007, 34, 807–813. [Google Scholar] [CrossRef] [PubMed]
- Breton-Torres, I.; Trichot, S.; Yachouh, J.; Jammet, P. Dysfonction de l’appareil manducateur: Approches rééducative et posturale [Temporomandibular joint disorders: Physiotherapy and postural approaches]. Rev. Stomatol. Chir. Maxillofac. Chir. Orale 2016, 117, 217–222. (In French) [Google Scholar] [CrossRef]
- Lee, B.K. Influence of proprioceptive neuromuscular facilitation therapeutic exercise on woman with temporomandibular joint disorder: A case study. J. Exerc. Rehabil. 2018, 14, 1074–1079. [Google Scholar] [CrossRef] [PubMed]
- Saccomanno, S.; Berretin-Felix, G.; Coceani Paskay, L.; Manenti, R.J.; Quinzi, V. Myofunctional Therapy Part 4: Prevention and treatment of dentofacial and oronasal disorders. Eur. J. Paediatr. Dent. 2021, 22, 332–334. [Google Scholar] [CrossRef] [PubMed]
- Saccomanno, S.; Antonini, G.; D’Alatri, L.; D’Angeloantonio, M.; Fiorita, A.; Deli, R. Case report of patients treated with an orthodontic and myofunctional protocol. Eur. J. Paediatr. Dent. 2014, 15 (Suppl. S2), 184–186. [Google Scholar] [PubMed]

| Frequency | Proportion | ||
|---|---|---|---|
| Assessment—[From the options below, what do you normally include in the evaluation of your patients with TMD?] | |||
| Jaw movements | 279 | 69.8 | |
| TMJ palpation | 269 | 67.3 | |
| Masticatory muscles | 262 | 65.5 | |
| TMJ sound | 234 | 58.5 | |
| Cervical spine | 209 | 52.3 | |
| Occlusion | 196 | 49.0 | |
| Parafuncion | 167 | 41.8 | |
| History | 1 | 0.3 | |
| Problem—[What type of TMD have you evaluated and/or treated? (select all that applies)] | |||
| Muscle tightness | 246 | 61.5 | |
| Mouth opening limitation | 224 | 56.0 | |
| Dislocation | 174 | 43.5 | |
| Trigger points | 155 | 38.8 | |
| TMJ Degeneration | 135 | 33.8 | |
| Malocclusion | 128 | 32.0 | |
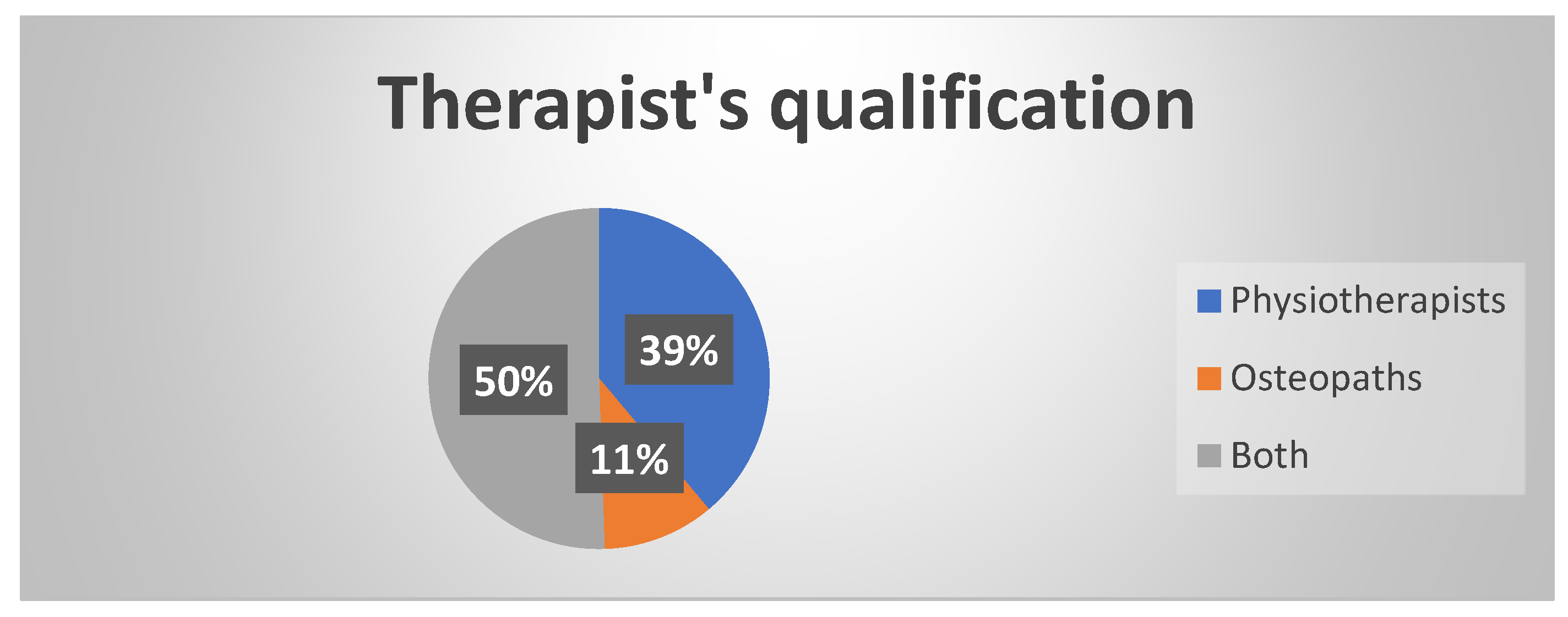
| Profession—[What is your profession?] | |||
| Physiotherapist | 155 | 38.8 | |
| Osteopath | 42 | 10.5 | |
| Both | 200 | 50 | |
| DId not respond | 3 | 0.8 | |
| Geograpical area—[Where do you live?] | |||
| Africa | 2 | 0.5 | |
| North America | 9 | 2.3 | |
| Central America | 2 | 0.5 | |
| South America | 2 | 0.5 | |
| Europe | 378 | 94.5 | |
| Asia and Middle east | 3 | 0.5 | |
| Oceania | 1 | 0.3 | |
| Did not respond | 3 | 0.8 | |
| Mean ± SD | Range | ||
| Age | 39.9 ± 10.8 | 21–69 | |
| years of Practice [How many years have you been practicing?] | 14.9 ± 10.2 | 0–47 | |
| Gender | |||
| Male | 214 | 53.8 | |
| Female | 184 | 46.0 | |
| Did not respond | 2 | 0.5 | |
| [Which healthcare provider/speciality do you refer to specifically?] Figure 2 | |||
| Orthodontist | 213 | 53.3 | |
| Physiotherapist | 159 | 39.8 | |
| Dentist | 154 | 38.5 | |
| Ostheopath | 121 | 30.3 | |
| Speech therapist | 112 | 28.0 | |
| Psychologist | 96 | 24.0 | |
| Oral surgeon | 89 | 22.3 | |
| [How much do you think you know about TMJ and its problems? (1–10)] | Physiotherapists | Osteopaths | Both |
| 4.81 ± 2.10 | 6.41 ± 1.55 | 4.02 ± 1.78 | |
| [Do you feel confident treating a patient with TMD? (1–10)] | |||
| p < 0.05 | 96/155 (61.9%) | 30/42 (71.4%) | 185/200 (92.5%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saran, S.; Saccomanno, S.; Petricca, M.T.; Carganico, A.; Bocchieri, S.; Mastrapasqua, R.F.; Caramaschi, E.; Levrini, L. Physiotherapists and Osteopaths’ Attitudes: Training in Management of Temporomandibular Disorders. Dent. J. 2022, 10, 210. https://doi.org/10.3390/dj10110210
Saran S, Saccomanno S, Petricca MT, Carganico A, Bocchieri S, Mastrapasqua RF, Caramaschi E, Levrini L. Physiotherapists and Osteopaths’ Attitudes: Training in Management of Temporomandibular Disorders. Dentistry Journal. 2022; 10(11):210. https://doi.org/10.3390/dj10110210
Chicago/Turabian StyleSaran, Stefano, Sabina Saccomanno, Maria Teresa Petricca, Andrea Carganico, Salvatore Bocchieri, Rodolfo Francesco Mastrapasqua, Elena Caramaschi, and Luca Levrini. 2022. "Physiotherapists and Osteopaths’ Attitudes: Training in Management of Temporomandibular Disorders" Dentistry Journal 10, no. 11: 210. https://doi.org/10.3390/dj10110210
APA StyleSaran, S., Saccomanno, S., Petricca, M. T., Carganico, A., Bocchieri, S., Mastrapasqua, R. F., Caramaschi, E., & Levrini, L. (2022). Physiotherapists and Osteopaths’ Attitudes: Training in Management of Temporomandibular Disorders. Dentistry Journal, 10(11), 210. https://doi.org/10.3390/dj10110210








