Ectopic Permanent Molars: A Review
Abstract
:1. Introduction
2. Prevalence
3. Etiology and Associated Dentoskeletal Features
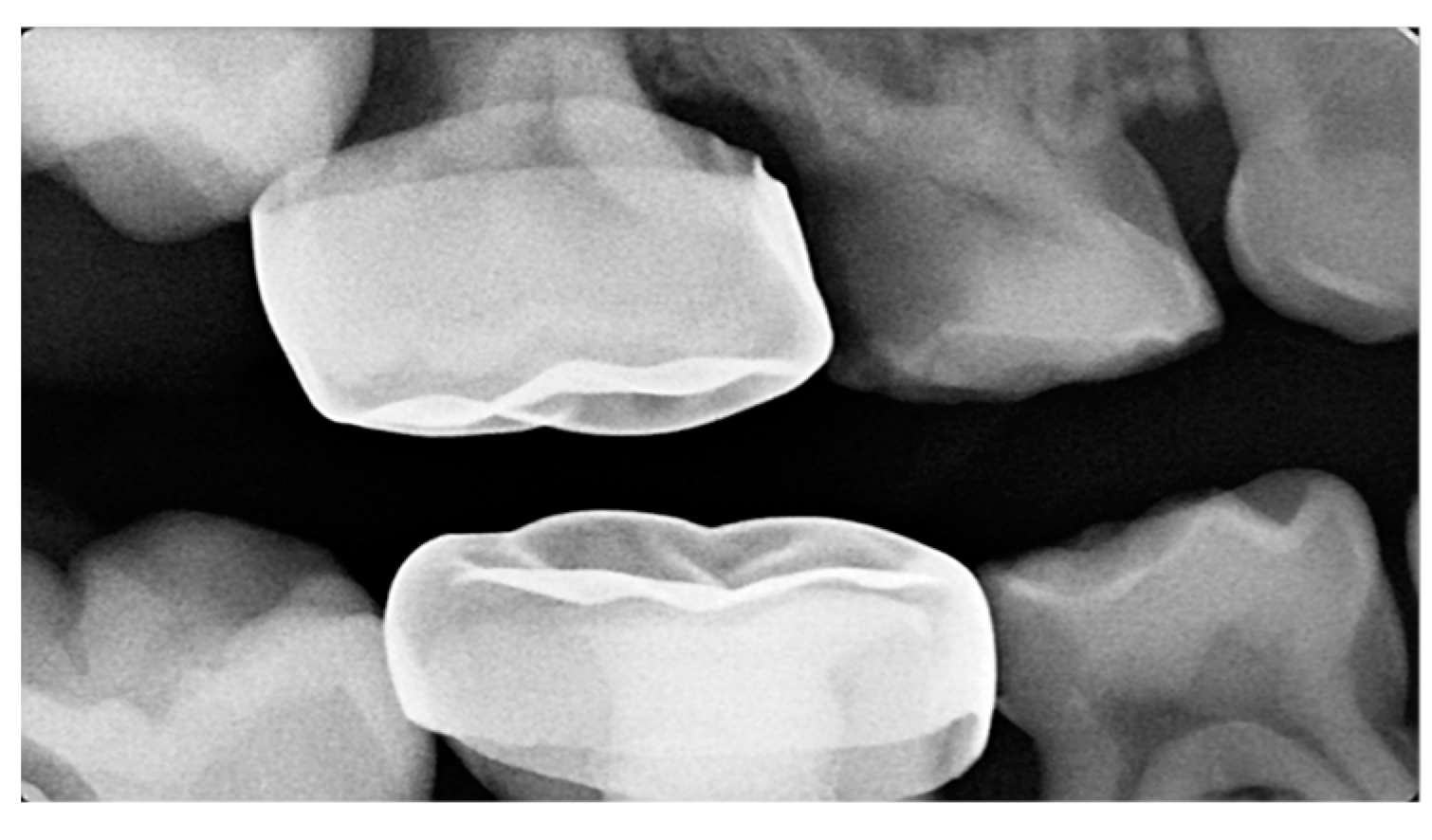
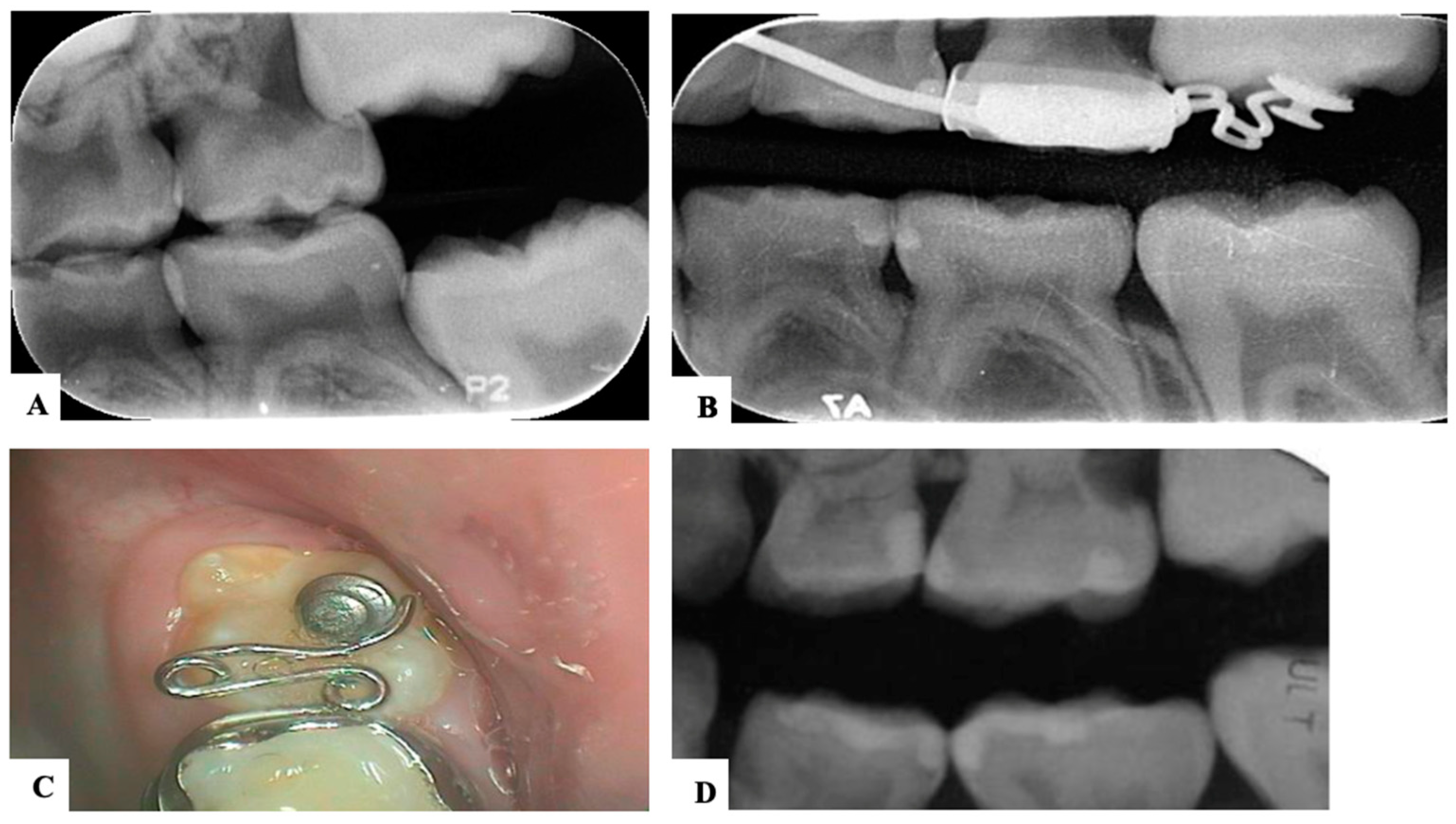
4. Classification
5. Diagnosis
6. Complications and Rationale for Treatment
7. Prognosis
8. Treatment
9. Ectopic First Permanent Molars
9.1. Interproximal Wedging
9.2. Distal Tipping
10. Ectopic Second Permanent Molars
11. Novel Devices
12. Maintenance
13. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nikiforuk, G. Ectopic eruption: Discussion and clinical report. J. Ont. Dent. Assoc. 1948, 25, 243–246. [Google Scholar]
- Kim, W.S.; Kim, Y.; Cho, J.H.; Oh, H.; Hwang, H.S. Unlocking ectopically erupting permanent first molars using light wires. J. Am. Dent. Assoc. 2020, 151, 857–862. [Google Scholar] [CrossRef] [PubMed]
- Nam, O.H.; Ahn, H.J.; Kim, M.S.; Park, J.H. Treatment of Ectopic Permanent Maxillary First Molar Using a K-loop. J. Clin. Pediatr. Dent. 2015, 39, 387–391. [Google Scholar] [CrossRef] [PubMed]
- Noueiri, B.; Ambriss, B.; Moukarzel, C. Management of Bilateral Ectopically Erupting Maxillary Molars: A Case Report. Int. J. Clin. Pediatr. Dent. 2019, 12, 153–156. [Google Scholar] [CrossRef]
- Bondemark, L.; Tsiopa, J.; Tsiopab, L.B.A.J.; Fu, P.S.; Wang, J.C.; Wu, Y.M.; Huang, T.K.; Chen, W.C.; Tseng, Y.C.; Tseng, C.H.; et al. Prevalence of Ectopic Eruption, Impaction, Retention and Agenesis of the Permanent Second Molar. Angle Orthod. 2007, 77, 773–778. [Google Scholar] [CrossRef] [PubMed]
- Güven, Y. Prevalence of ectopic eruption of first permanent molars in a Turkish population. Eur. Oral Res. 2018, 52, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Hennessy, J.; Al-Awadhi, E.; Dwyer, L.O.; Leith, R.; Sian, J.S.; Sivakumar, A.; Sholapurkar, A.; Muthukrishnan, V.; Valiathan, A.; Pai, K.M.; et al. Treatment of ectopic first permanent molar teeth. Dent. Updat. 2012, 39, 656–661. [Google Scholar] [CrossRef] [PubMed]
- Magnussona, C.; Kjellbergb, H. Impaction and Retention of Second Molars: Diagnosis, Treatment and Outcome. A Retro-spective Follow-up Study. Angle Orthod. 2009, 79, 422–427. [Google Scholar] [CrossRef] [PubMed]
- Helm, A.; Martín-Vacas, A.; Molinero-Mourelle, P.; Caleya, A.; Gallardo, N.; Mourelle-Martínez, M. Ectopic Eruption of Maxillary First Permanent Molars: Preliminary Results of Prevalence and Dentoskeletal Characteristics in Spanish Paediatric Population. Children 2021, 8, 479. [Google Scholar] [CrossRef]
- Aldowsari, M.K.; Alsaidan, M.; Alaqil, M.; BinAjian, A.; Albeialy, J.; Alraawi, M.; Al Moaleem, M.M. Ectopic Eruption of First Permanent Molars for Pediatric Patients Attended King Saud University, Riyadh, Saudi Arabia: A Radiographic Study. Clin. Cosmet. Investig. Dent. 2021, 13, 325–333. [Google Scholar] [CrossRef]
- Cohn, C. Diagnosis and Treatment of Ectopic Eruption of Permanent Molars—Oral Health Group. 2014. Available online: https://www.oralhealthgroup.com/features/diagnosis-and-treatment-of-ectopic-eruption-of-permanent-molars/ (accessed on 20 July 2023).
- Kurol, J.; Bjerklin, K. Ectopic eruption of maxillary first permanent molars: A review. ASDC J. Dent. Child. 1986, 53, 209–214. [Google Scholar]
- Dalben, G.d.S.; das Neves, L.T.; Gomide, M.R. Oral findings in patients with Apert Syndrome. J. Appl. Oral Sci. 2006, 14, 465–469. [Google Scholar] [CrossRef]
- Ahiko, N.; Baba, Y.; Tsuji, M.; Horikawa, R.; Moriyama, K. Investigation of maxillofacial morphology and oral characteristics with Turner syndrome and early mixed dentition. Congenit. Anomalies 2018, 59, 11–17. [Google Scholar] [CrossRef]
- Giancotti, A.; Maselli, A. Orthodontic correction of an ectopic mandibular first permanent molar: A case report. J. Clin. Pediatr. Dent. 2001, 25, 119–121. [Google Scholar] [CrossRef] [PubMed]
- Mucedero, M.; Rozzi, M.; Cardoni, G.; Ricchiuti, M.R.; Cozza, P. Dentoskeletal features in individuals with ectopic eruption of the permanent maxillary first molar. Korean J. Orthod. 2015, 45, 190–197. [Google Scholar] [CrossRef]
- Bjerklin, K.; Kurol, J. Ectopic eruption of the maxillary first permanent molar: Etiologic factors. Am. J. Orthod. 1983, 84, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Garrocho-Rangel, A.; Benavídez-Valadez, P.; Rosales-Berber, M.Á.; Pozos-Guillén, A. Treatment of ectopic eruption of the max-illary first permanent molar in children and adolescents: A scoping review. Eur. J. Paediatr. Dent. 2022, 23, 94–100. [Google Scholar] [CrossRef] [PubMed]
- Croll, T.P.; Epstein, D.W.; Castaldi, C.R. Marginal adaptation of stainless steel crowns. Pediatr. Dent. 2003, 25, 249–252. [Google Scholar] [PubMed]
- Baccetti, T. Tooth anomalies associated with failure of eruption of first and second permanent molars. Am. J. Orthod. Dentofac. Orthop. 2000, 118, 608–610. [Google Scholar] [CrossRef]
- Becktor, K.B.; Steiniche, K.; Kjær, I. Association between ectopic eruption of maxillary canines and first molars. Eur. J. Orthod. 2005, 27, 186–189. [Google Scholar] [CrossRef]
- Bjerklin, K.; Kurol, J.; Valentin, J. Ectopic eruption of maxillary first permanent molars and association with other tooth and developmental disturbances. Eur. J. Orthod. 1992, 14, 369–375. [Google Scholar] [CrossRef]
- Young, D.H. Ectopic eruption of the first permanent molar. J. Dent. Child. 1980, 24, 153–162. [Google Scholar]
- Barberia-Leache, E.; Suarez-Clúa, M.C.; Saavedra-Ontiveros, D. Ectopic eruption of the maxillary first permanent molar: Char-acteristics and occurrence in growing children. Angle Orthodontist. 2005, 75, 610–615. [Google Scholar] [CrossRef]
- Harrison, L.; Michal, B.C. Treatment of Ectopically Erupting Permanent Molars. Dent. Clin. N. Am. 1984, 28, 57–67. [Google Scholar] [CrossRef]
- Chen, X.; Huo, Y.; Peng, Y.; Zhang, Q.; Zou, J. Ectopic eruption of the first permanent molar: Predictive factors for irreversible outcome. Am. J. Orthod. Dentofac. Orthop. 2021, 159, 169–177. [Google Scholar] [CrossRef] [PubMed]
- Dean, J. McDonald’s and Avery’s Dentistry for the Child and Adolescent, 10th ed.; Mosby/Elsevier: St. Louis, MO, USA, 2011. [Google Scholar]
- Dabbagh, B.; Sigal, M.J.; Tompson, B.D.; Titley, K.; Andrews, P. Ectopic Eruption of the Permanent Maxillary First Molar: Predictive Factors for Irreversible Outcome. Int. J. Clin. Pediatr. Dent. 2017, 39, 215–218. [Google Scholar]
- Song, M.S.; Kang, C.M.; Song, J.S.; Choi, H.J.; Lee, J.; Kim, S.O. Modifications of Rect-Spring to Enhance the Engagement of Ectopically Entrapped Molars with 2 Case Reports. Children 2021, 8, 823. [Google Scholar] [CrossRef]
- Kupietzky, A.; Soxman, J.A. Ectopic Eruption of Maxillary First Permanent Molars. In Handbook of Clinical Techniques in Pe-diatric Dentistry; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2021; Volume 5, pp. 201–215. [Google Scholar] [CrossRef]
- Marín, N.G. Corrective Treatment of Ectopic Eruption of Permanent First Molars: Case Report. Odovtos-Int. J. Dent. Sc. 2022, 23, 19–26. [Google Scholar] [CrossRef]
- Huang, W.J.; Childers, N.K. Clinical aid in placing brass wires to treat ectopically erupting permanent first molars. Pediatr. Dent. 1995, 17, 122. [Google Scholar] [PubMed]
- Levitas, T.C. A simple technique for correcting an ectopically erupting maxillary first permanent molar. J. Dent. Child. 1964, 31, 16–18. [Google Scholar]
- Gungor, H.C.; Altay, N. Ectopic eruption of maxillary first permanent molars: Treatment options and report of two cases. J. Clin. Pediatr. Dent. 1998, 22, 211–216. [Google Scholar]
- Abu-Hussein, M.; Watted, N.; Abdulgani, A. Halterman technique for the treatment of ectopically erupting permanent first molar. J. Dent. Med. Sci. 2015, 14, 72–78. [Google Scholar] [CrossRef]
- Yaseen, S.M.; Naik, S.; Uloopi, K. Ectopic eruption—A review and case report. Contemp. Clin. Dent. 2011, 2, 3–7. [Google Scholar] [CrossRef]
- Pogrel, M. The surgical uprighting of mandibular second molars. Am. J. Orthod. Dentofac. Orthop. 1995, 108, 180–183. [Google Scholar] [CrossRef]
- Rajesh, R.; Naveen, V.; Amit, S.; Baroudi, K.; Reddy, C.S.; Namineni, S. Treatment of Ectopic Mandibular Second Permanent Molar with Elastic Separators. Case Rep. Dent. 2014, 2014, 621568. [Google Scholar] [CrossRef]
- Giancotti, A.; Arcuri, C.; Barlattani, A. Treatment of ectopic mandibular second molar with titanium miniscrews. Am. J. Orthod. Dentofacial Orthop. 2004, 126, 113–117. [Google Scholar] [CrossRef]
- Kim, I.H.; Kang, C.M.; Song, J.S.; Lee, J.; Choi, H.J.; Kim, S.O. The Piston Elastic: A Novel Device for Treating Entrapped Ectopic Permanent Molars. Children 2021, 8, 652. [Google Scholar] [CrossRef] [PubMed]
- Jun, H.; Lee, H.S.; Song, J.S.; Lee, J.; Choi, B.J.; Kim, S.O. The Rect-spring: A new device for treating ectopically erupting permanent molars. Pediatr. Dent. 2014, 36, 143–147. [Google Scholar]
- Christensen, J.; Nowak, A.; Mabry, T.; Townsend, J.; Wells, M. Pediatric Dentistry: Infancy through Adolescence, 5th ed.; Elsevier Inc.: St. Louis, MO, USA, 2013; Chapter 35, Treatment Planning and Management of Orthodontic Problems; pp. 527–529. [Google Scholar]








| Barberia-Leache ’s Classification (Based on the effect on second primary molar) * | |||||
| Grade 1 Mild | Grade 2 Moderate | Grade 3 Severe | Grade 4 Very severe | ||
| Limited resorption to the cementum or with minimum dentine penetration | Resorption of the dentine without pulp exposure | Resorption of the distal root leading to pulp exposure | Resorption that affects the mesial root of the second primary molar | ||
 |  |  |  | ||
| Harrison and Michal’s Classification (based on severity of the lock using bitewing radiograph) * | |||||
| Normal | Minimal lock | Severe lock | |||
| No sign of impaction | Impacted less than half the width of the distal marginal ridge of the second primary molar | Impacted more than the width of the distal marginal ridge of the second primary molar | |||
 |  |  | |||
| Treatment Modalities | Severity of Impaction | Chair Side Time | Laboratory Work | Patient Discomfort | Cost | Treatment Duration |
|---|---|---|---|---|---|---|
| Elastic separator [35] | Mild to moderate | ↓ | ✕ | ↑ | ↓ | ↓ |
| Soft brass wire separator [37] | Mild to moderate | ↓ | ✕ | ↑ | ↓ | ↓ |
| Spring separator | Mild to moderate | ↓ | ✕ | ↑ | ↓ | ↓ |
| Humphrey appliance | Moderate to severe | ↑ | √ | ↓ | ↑ | ↓ |
| Halterman appliance [35] | Moderate to severe | ↑ | √ | ↓ | ↑ | ↓ |
| Croll’s appliance [4] | Moderate to severe | ↑ | √ | ↓ | ↑ | ↓ |
| Fixed edgewise appliance | Moderate to severe | ↑ | ✕ | ↓ | ↑ | ↓ |
| Surgical uprighting | Severe | ↑ | ✕ | ↑↑ | ↑↑ | ↑ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alfuriji, S.; Alamro, H.; Kentab, J.; Alosail, L.; Alali, L.; Altuwaijri, N.; Alalwan, R. Ectopic Permanent Molars: A Review. Dent. J. 2023, 11, 206. https://doi.org/10.3390/dj11090206
Alfuriji S, Alamro H, Kentab J, Alosail L, Alali L, Altuwaijri N, Alalwan R. Ectopic Permanent Molars: A Review. Dentistry Journal. 2023; 11(9):206. https://doi.org/10.3390/dj11090206
Chicago/Turabian StyleAlfuriji, Samah, Haifa Alamro, Jomanah Kentab, Lama Alosail, Linah Alali, Nada Altuwaijri, and Rahaf Alalwan. 2023. "Ectopic Permanent Molars: A Review" Dentistry Journal 11, no. 9: 206. https://doi.org/10.3390/dj11090206
APA StyleAlfuriji, S., Alamro, H., Kentab, J., Alosail, L., Alali, L., Altuwaijri, N., & Alalwan, R. (2023). Ectopic Permanent Molars: A Review. Dentistry Journal, 11(9), 206. https://doi.org/10.3390/dj11090206







