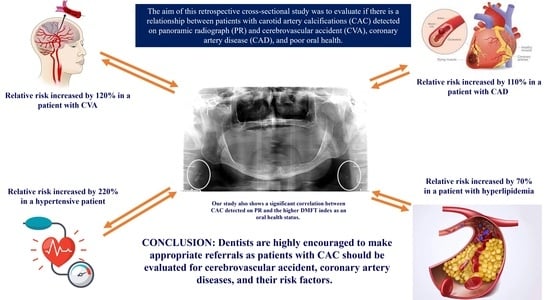
Carotid Artery Calcification Detected on Panoramic Radiography Is Significantly Related to Cerebrovascular Accident, Coronary Artery Disease, and Poor Oral Health: A Retrospective Cross-Sectional Study
Abstract
1. Introduction
2. Methods
2.1. Control Group
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Friedlander, A.H.; Lande, A. Panoramic radiographic identification of carotid arterial plaques. Oral Surg. Oral Med. Oral Pathol. 1981, 52, 102–104. [Google Scholar] [CrossRef] [PubMed]
- Kwon, Y.E.; An, C.H.; Choi, K.S.; An, S.Y. Comparison of carotid artery calcification between stroke and nonstroke patients using CT angiographic and panoramic images. Dentomaxillofac. Radiol. 2022, 51, 20210500. [Google Scholar] [CrossRef] [PubMed]
- Most, T.; Winter, L.; Ballheimer, Y.E.; Kappler, C.; Schmid, M.; Adler, W.; Weber, M.; Kesting, M.R.; Lutz, R. Prevalence of carotid artery calcification detected by different dental imaging techniques and their relationship with cardiovascular risk factors, age and gender. BMC Oral Health 2023, 23, 949. [Google Scholar] [CrossRef] [PubMed]
- Almog, D.M.; Horev, T.; Illig, K.A.; Green, R.M.; Carter, L.C. Correlating carotid artery stenosis detected by panoramic radiography with clinically relevant carotid artery stenosis determined by duplex ultrasound. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2002, 94, 768–773. [Google Scholar] [CrossRef] [PubMed]
- Smoljan-Basuga, M.; Marelic, M.; Badel, T.; Skrinjar, I.; Loncar-Brzak, B.; Klemencic, A.; Flegaric-Bradic, M.; Prenc, M.; Zadravec, D. Significance of Calcifications in Projection of Carotid Arteries on Orthopantomography for Detection of Carotid Artery Stenosis. Acta Stomatol. Croat. 2022, 56, 257–266. [Google Scholar] [CrossRef] [PubMed]
- Ross, R. Atherosclerosis—An inflammatory disease. N. Engl. J. Med. 1999, 340, 115–126. [Google Scholar] [CrossRef] [PubMed]
- Lusis, A.J. Atherosclerosis. Nature 2000, 407, 233–241. [Google Scholar] [CrossRef] [PubMed]
- Tsao, C.W.; Aday, A.W.; Almarzooq, Z.I.; Anderson, C.A.M.; Arora, P.; Avery, C.L.; Baker-Smith, C.M.; Beaton, A.Z.; Boehme, A.K.; Buxton, A.E.; et al. Heart Disease and Stroke Statistics-2023 Update: A Report from the American Heart Association. Circulation 2023, 147, e93–e621. [Google Scholar] [CrossRef] [PubMed]
- Assmann, G.; Cullen, P.; Jossa, F.; Lewis, B.; Mancini, M. Coronary heart disease: Reducing the risk: The scientific background to primary and secondary prevention of coronary heart disease. A worldwide view. International Task force for the Prevention of Coronary Heart disease. Arterioscler. Thromb. Vasc. Biol. 1999, 19, 1819–1824. [Google Scholar] [CrossRef]
- Kugiyama, K.; Ota, Y.; Takazoe, K.; Moriyama, Y.; Kawano, H.; Miyao, Y.; Sakamoto, T.; Soejima, H.; Ogawa, H.; Doi, H.; et al. Circulating levels of secretory type II phospholipase A(2) predict coronary events in patients with coronary artery disease. Circulation 1999, 100, 1280–1284. [Google Scholar] [CrossRef]
- Nathan, L.; Chaudhuri, G. Estrogens and atherosclerosis. Annu. Rev. Pharmacol. Toxicol. 1997, 37, 477–515. [Google Scholar] [CrossRef] [PubMed]
- Goldbourt, U.; Neufeld, H.N. Genetic aspects of arteriosclerosis. Arteriosclerosis 1986, 6, 357–377. [Google Scholar] [CrossRef] [PubMed]
- Schroder, A.G.D.; de Araujo, C.M.; Guariza-Filho, O.; Flores-Mir, C.; de Luca Canto, G.; Porporatti, A.L. Diagnostic accuracy of panoramic radiography in the detection of calcified carotid artery atheroma: A meta-analysis. Clin. Oral Investig. 2019, 23, 2021–2040. [Google Scholar] [CrossRef] [PubMed]
- Garoff, M.; Ahlqvist, J.; Levring Jaghagen, E.; Johansson, E.; Wester, P. Carotid calcification in panoramic radiographs: Radiographic appearance and the degree of carotid stenosis. Dentomaxillofac. Radiol. 2016, 45, 20160147. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.N.; Friedlander, A.H.; Jolly, D.A.; Date, L. Carotid calcification on panoramic radiographs: An important marker for vascular risk. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2002, 94, 510–514. [Google Scholar] [CrossRef] [PubMed]
- Constantine, S.; Roach, D.; Liberali, S.; Kiermeier, A.; Sarkar, P.; Jannes, J.; Sambrook, P.; Anderson, P.; Beltrame, J. Carotid Artery Calcification on Orthopantomograms (CACO Study)—Is it indicative of carotid stenosis? Aust. Dent. J. 2019, 64, 4–10. [Google Scholar] [CrossRef] [PubMed]
- Goncalves, J.R.; Yamada, J.L.; Berrocal, C.; Westphalen, F.H.; Franco, A.; Fernandes, A. Prevalence of Pathologic Findings in Panoramic Radiographs: Calcified Carotid Artery Atheroma. Acta Stomatol. Croat. 2016, 50, 230–234. [Google Scholar] [CrossRef] [PubMed]
- Maia, P.R.L.; Tomaz, A.F.G.; Maia, E.F.T.; Lima, K.C.; Oliveira, P.T. Prevalence of soft tissue calcifications in panoramic radiographs of the maxillofacial region of older adults. Gerodontology 2022, 39, 266–272. [Google Scholar] [CrossRef] [PubMed]
- Ghassemzadeh, S.; Sbricoli, L.; Frigo, A.C.; Bacci, C. Incidental findings detected with panoramic radiography: Prevalence calculated on a sample of 2017 cases treated at a major Italian trauma and cancer centre. Oral Radiol. 2021, 37, 507–517. [Google Scholar] [CrossRef]
- Janiszewska-Olszowska, J.; Jakubowska, A.; Gieruszczak, E.; Jakubowski, K.; Wawrzyniak, P.; Grocholewicz, K. Carotid Artery Calcifications on Panoramic Radiographs. Int. J. Environ. Res. Public Health 2022, 19, 14056. [Google Scholar] [CrossRef]
- Aghazadehsanai, N.; Chang, T.I.; Garrett, N.R.; Friedlander, A.H. Prevalence of calcified carotid artery atheromas on digital panoramic images among perimenopausal and postmenopausal African American women. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2017, 123, 621–625. [Google Scholar] [CrossRef] [PubMed]
- Mehdizadeh, M.; Shahbazi, S.; Taheri, H.; Eslami, A. Evaluation of Using Panoramic Radiography and Ultrasonography for Diagnosing Carotid Artery Calcifications. Adv. BioMed Res. 2023, 12, 226. [Google Scholar] [CrossRef]
- Ozkan, G.; Kose, E.; Yesiltepe, S. Ultrasonographic Evaluation of Soft Tissue Calcifications in the Head and Neck Region Detected on Panoramic Radiographs. J. Ultrasound. Med. 2023, 42, 1057–1064. [Google Scholar] [CrossRef] [PubMed]
- Garoff, M.; Johansson, E.; Ahlqvist, J.; Jaghagen, E.L.; Arnerlov, C.; Wester, P. Detection of calcifications in panoramic radiographs in patients with carotid stenoses >/=50%. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2014, 117, 385–391. [Google Scholar] [CrossRef] [PubMed]
- Kumagai, M.; Yamagishi, T.; Fukui, N.; Chiba, M. Carotid artery calcification seen on panoramic dental radiographs in the Asian population in Japan. Dentomaxillofac. Radiol. 2007, 36, 92–96. [Google Scholar] [CrossRef] [PubMed]
- Moshfeghi, M.; Taheri, J.B.; Bahemmat, N.; Evazzadeh, M.E.; Hadian, H. Relationship between carotid artery calcification detected in dental panoramic images and hypertension and myocardial infarction. Iran. J. Radiol. 2014, 11, e8714. [Google Scholar] [CrossRef] [PubMed]
- Kumagai, M.; Yamagishi, T.; Fukui, N.; Chiba, M. Long-term cigarette smoking increases the prevalence of carotid artery calcification seen on panoramic dental radiographs in male patients. Tohoku J. Exp. Med. 2007, 212, 21–25. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Akkemik, O.; Kazaz, H.; Tamsel, S.; Dundar, N.; Sahinalp, S.; Ellidokuz, H. A 5 years follow-up for ischemic cardiac outcomes in patients with carotid artery calcification on panoramic radiographs confirmed by doppler ultrasonography in Turkish population. Dentomaxillofac. Radiol. 2020, 49, 20190440. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Yang, Z.; Wang, Y.; Gao, H.; Wang, Y.; Zhang, Q. Association between Periodontitis and Carotid Artery Calcification: A Systematic Review and Meta-Analysis. BioMed Res. Int. 2021, 2021, 3278351. [Google Scholar] [CrossRef]
- Garoff, M.; Ahlqvist, J.; Edin, L.T.; Jensen, S.; Levring Jaghagen, E.; Petajaniemi, F.; Wester, P.; Johansson, E. Bilateral vessel-outlining carotid artery calcifications in panoramic radiographs: An independent risk marker for vascular events. BMC Cardiovasc. Disord. 2019, 19, 225. [Google Scholar] [CrossRef]
- Bladh, M.; Gustafsson, N.; Engstrom, G.; Kennback, C.; Klinge, B.; Nilsson, P.M.; Jonsson, D.; Levring Jaghagen, E. Defined shapes of carotid artery calcifications on panoramic radiographs correlate with specific signs of cardiovascular disease on ultrasound examination. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2023. [Google Scholar] [CrossRef] [PubMed]
- Song, I.S.; Han, K.; Ryu, J.J.; Park, J.B. Obesity is inversely related to the risks of dental caries in Korean adults. Oral Dis. 2017, 23, 1080–1086. [Google Scholar] [CrossRef] [PubMed]
- Desvarieux, M.; Demmer, R.T.; Rundek, T.; Boden-Albala, B.; Jacobs, D.R., Jr.; Papapanou, P.N.; Sacco, R.L.; Oral, I.; Vascular Disease Epidemiology, S. Relationship between periodontal disease, tooth loss, and carotid artery plaque: The Oral Infections and Vascular Disease Epidemiology Study (INVEST). Stroke 2003, 34, 2120–2125. [Google Scholar] [CrossRef] [PubMed]
- Schillinger, T.; Kluger, W.; Exner, M.; Mlekusch, W.; Sabeti, S.; Amighi, J.; Wagner, O.; Minar, E.; Schillinger, M. Dental and periodontal status and risk for progression of carotid atherosclerosis: The inflammation and carotid artery risk for atherosclerosis study dental substudy. Stroke 2006, 37, 2271–2276. [Google Scholar] [CrossRef] [PubMed]
- Abecasis, P.; Chimenos-Kustner, E.; Lopez-Lopez, O. Orthopantomography contribution to prevent isquemic stroke. J. Clin. Exp. Dent. 2014, 6, e127. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Johansson, E.P.; Ahlqvist, J.; Garoff, M.; Karp, K.; Jaghagen, E.L.; Wester, P. Ultrasound screening for asymptomatic carotid stenosis in subjects with calcifications in the area of the carotid arteries on panoramic radiographs: A cross-sectional study. BMC Cardiovasc. Disord. 2011, 11, 44. [Google Scholar] [CrossRef] [PubMed]
- Borger, M.A.; Fremes, S.E.; Weisel, R.D.; Cohen, G.; Rao, V.; Lindsay, T.F.; Naylor, C.D. Coronary bypass and carotid endarterectomy: Does a combined approach increase risk? A metaanalysis. Ann. Thorac. Surg. 1999, 68, 14–20; discussion 21. [Google Scholar] [CrossRef] [PubMed]
- Jashari, F.; Ibrahimi, P.; Nicoll, R.; Bajraktari, G.; Wester, P.; Henein, M.Y. Coronary and carotid atherosclerosis: Similarities and differences. Atherosclerosis 2013, 227, 193–200. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, T.; Morimoto, Y.; Ansai, T.; Okabe, S.; Yamada, K.; Taguchi, A.; Awano, S.; Kito, S.; Takata, Y.; Takehara, T.; et al. Can the presence of carotid artery calcification on panoramic radiographs predict the risk of vascular diseases among 80-year-olds? Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2006, 101, 777–783. [Google Scholar] [CrossRef]
- Bengtsson, V.W.; Persson, G.R.; Berglund, J.; Renvert, S. Carotid calcifications in panoramic radiographs are associated with future stroke or ischemic heart diseases: A long-term follow-up study. Clin. Oral Investig. 2019, 23, 1171–1179. [Google Scholar] [CrossRef]
- Griniatsos, J.; Damaskos, S.; Tsekouras, N.; Klonaris, C.; Georgopoulos, S. Correlation of calcified carotid plaques detected by panoramic radiograph with risk factors for stroke development. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2009, 108, 600–603. [Google Scholar] [CrossRef] [PubMed]
- Gustafsson, N.; Ahlqvist, J.B.; Naslund, U.; Wester, P.; Buhlin, K.; Gustafsson, A.; Levring Jaghagen, E. Calcified carotid artery atheromas in panoramic radiographs are associated with a first myocardial infarction: A case-control study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2018, 125, 199–204 e191. [Google Scholar] [CrossRef] [PubMed]
- Lim, L.Z.; Koh, P.S.F.; Cao, S.; Wong, R.C.W. Can carotid artery calcifications on dental radiographs predict adverse vascular events? A systematic review. Clin. Oral Investig. 2021, 25, 37–53. [Google Scholar] [CrossRef] [PubMed]
- Carasso, S.; Porat Ben Amy, D.; Issawy, M.; Kusniec, F.; Ghanim, D.; Sudarsky, D.; Elbaz-Greener, G.; Kinany, W.; Shmuel, C.; Abu El-Naaj, I.; et al. The association between carotid calcium on dental panoramic radiographs and coronary calcium score on chest computerized tomography. Dentomaxillofac. Radiol. 2021, 50, 20200174. [Google Scholar] [CrossRef]
- Donders, H.C.M.; LM, I.J.; Soffner, M.; van ’t Hof, A.W.J.; Loos, B.G.; de Lange, J. Elevated Coronary Artery Calcium scores are associated with tooth loss. PLoS ONE 2020, 15, e0243232. [Google Scholar] [CrossRef]





| Characteristics | N (%) |
|---|---|
| Sex | |
| Female | 168 (53.5) |
| Male | 146 (46.5) |
| Age (years) | |
| Range | 29–92 |
| Median | 68 |
| Age distribution | |
| 0–29 | 1 (0.3) |
| 30–39 | 2 (0.6) |
| 40–49 | 3 (1) |
| 50–59 | 40 (12.7) |
| 60–69 | 124 (39.5) |
| 70–79 | 109 (34.7) |
| 80–89 | 32 (10.2) |
| 90–99 | 3 (1) |
| Location | |
| One side | 168 (53.5) |
| Both sides | 146 (46.5) |
| DMFT | |
| Range | 8–32 |
| Average | 26.6 |
| Hypertension | |
| Yes | 268 (86.2) |
| No | 43 (13.8) |
| Hyperlipidemia | |
| Yes | 178 (57.6) |
| No | 131 (42.4) |
| Diabetes mellitus | |
| Yes | 95 (30.7) |
| No | 214 (69.3) |
| Cerebrovascular accident | |
| Yes | 48 (15.5) |
| No | 261 (84.5) |
| Coronary artery disease | |
| Yes | 89 (28.7) |
| No | 221 (71.3) |
| Unilateral | Bilateral | p-Value | |
|---|---|---|---|
| Age (mean ± SD) years | 67.8 ± 9.1 | 68.6 ± 9.2 | 0.465 * |
| Gender (F; M) | 0.734 | ||
| Female | 88 | 80 | |
| Male | 80 | 66 | |
| Hypertension | 0.622 | ||
| Yes | 142 | 126 | |
| No | 25 | 18 | |
| Hyperlipidemia | 1.00 | ||
| Yes | 96 | 82 | |
| No | 70 | 61 | |
| Diabetes mellitus | 0.387 | ||
| Yes | 55 | 40 | |
| No | 111 | 103 | |
| Cerebrovascular accident | 0.116 | ||
| Yes | 31 | 17 | |
| No | 135 | 126 | |
| Coronary artery disease | 0.802 | ||
| Yes | 49 | 40 | |
| No | 117 | 104 | |
| DMFT index (mean ± SD) | 26.96 ± 5.7 | 26.17 ± 6 | 0.234 * |
| CAC N = 276 | Control N = 276 | p-Value | |
|---|---|---|---|
| Age (mean ± SD; range) years | 68.5 ± 8.7; (34–92) | 68.5 ± 8.7; (34–92) | 1.00 * |
| Gender (F; M) | 1.00 | ||
| Female | 150 | 150 | |
| Male | 126 | 126 | |
| Hypertension | <0.001 | ||
| Yes | 237 | 159 | |
| No | 39 | 117 | |
| Hyperlipidemia | <0.001 | ||
| Yes | 161 | 93 | |
| No | 115 | 183 | |
| Diabetes mellitus | 0.007 | ||
| Yes | 90 | 61 | |
| No | 186 | 215 | |
| Cerebrovascular accident | <0.001 | ||
| Yes | 41 | 14 | |
| No | 235 | 262 | |
| Coronary artery disease | <0.001 | ||
| Yes | 72 | 27 | |
| No | 204 | 249 | |
| DMFT index (mean; range) | 26.3; (8–32) | 23.7; (2–32) | <0.001 * |
| aOR | 95% CI | p-Value | |
|---|---|---|---|
| Hypertension | 3.20 | 2.06–5.07 | <0.001 |
| Hyperlipidemia | 1.70 | 1.14–2.50 | 0.009 |
| Diabetes mellitus | 0.85 | 0.55–1.30 | 0.465 |
| CVA | 2.20 | 1.13–4.30 | 0.02 |
| CAD | 2.10 | 1.28–3.60 | 0.004 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brar, A.; DeColibus, K.; Rasner, D.S.; Haynes, A.R.; Pancratz, F.; Oladiran, O.; Gbadamosi, S.O.; Owosho, A.A. Carotid Artery Calcification Detected on Panoramic Radiography Is Significantly Related to Cerebrovascular Accident, Coronary Artery Disease, and Poor Oral Health: A Retrospective Cross-Sectional Study. Dent. J. 2024, 12, 99. https://doi.org/10.3390/dj12040099
Brar A, DeColibus K, Rasner DS, Haynes AR, Pancratz F, Oladiran O, Gbadamosi SO, Owosho AA. Carotid Artery Calcification Detected on Panoramic Radiography Is Significantly Related to Cerebrovascular Accident, Coronary Artery Disease, and Poor Oral Health: A Retrospective Cross-Sectional Study. Dentistry Journal. 2024; 12(4):99. https://doi.org/10.3390/dj12040099
Chicago/Turabian StyleBrar, Anmol, Katherine DeColibus, D. Shane Rasner, Angela R. Haynes, Frank Pancratz, Oreoluwa Oladiran, Semiu O. Gbadamosi, and Adepitan A. Owosho. 2024. "Carotid Artery Calcification Detected on Panoramic Radiography Is Significantly Related to Cerebrovascular Accident, Coronary Artery Disease, and Poor Oral Health: A Retrospective Cross-Sectional Study" Dentistry Journal 12, no. 4: 99. https://doi.org/10.3390/dj12040099
APA StyleBrar, A., DeColibus, K., Rasner, D. S., Haynes, A. R., Pancratz, F., Oladiran, O., Gbadamosi, S. O., & Owosho, A. A. (2024). Carotid Artery Calcification Detected on Panoramic Radiography Is Significantly Related to Cerebrovascular Accident, Coronary Artery Disease, and Poor Oral Health: A Retrospective Cross-Sectional Study. Dentistry Journal, 12(4), 99. https://doi.org/10.3390/dj12040099