Microbiological Analysis of Plaque and Its Composition in Three Patient Groups under Different Orthodontic Treatments
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Size
2.2. Bleeding Indices
2.3. Plaque Indices
2.4. Microbiological Analysis of Bacterial Plaque
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Blatz, M.B.; Chiche, G.; Bahat, O.; Roblee, R.; Coachman, C.; Heymann, H.O. Evolution of Aesthetic Dentistry. J. Dent. Res. 2019, 98, 1294–1304. [Google Scholar] [CrossRef] [PubMed]
- Campos, L.A.; Costa, M.A.; Bonafé, F.S.S.; Marôco, J.; Campos, J.A.D.B. Psychosocial impact of dental aesthetics on dental patients. Int. Dent. J. 2020, 70, 321–327. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kusy, R.P. Orthodontic biomechanics: Vistas from the top of a new century. Am. J. Orthod. Dentofac. Orthop. 2000, 117, 589–591. [Google Scholar] [CrossRef] [PubMed]
- Papageorgiou, S.N.; Koletsi, D.; Iliadi, A.; Peltomaki, T.; Eliades, T. Treatment outcome with orthodontic aligners and fixed appliances: A systematic review with meta-analyses. Eur. J. Orthod. 2020, 42, 331–343. [Google Scholar] [CrossRef] [PubMed]
- Jedliński, M.; Belfus, J.; Milona, M.; Mazur, M.; Grocholewicz, K.; Janiszewska-Olszowska, J. Orthodontic treatment demand for fixed treatment and aligners among young adults in middle Europe and South America—A questionnaire study. BMC Oral Health 2024, 24, 292. [Google Scholar] [CrossRef] [PubMed]
- Farronato, G.; Giannini, L.; Nolet, F.; Galbiati, G.; Garagiola, U.; Maspero, C. Qualitative and quantitative assessment of plaque bacteria in pediatric patients, patients undergoing orthodontic treatment, combined orthdontic-surgical treatment and implant-prosthetic rehabilitation. Minerva Stomatol. 2014, 63, 167–178. [Google Scholar] [PubMed]
- Giardino, L.; Savadori, P.; Generali, L.; Mohammadi, Z.; Del Fabbro, M.; De Vecchi, E.; Bidossi, A. Antimicrobial effectiveness of etidronate powder (Dual Rinse® HEDP) and two EDTA preparations against Enterococcus faecalis: A preliminary laboratory study. Odontology 2020, 108, 396–405. [Google Scholar] [CrossRef] [PubMed]
- Al-Dboush, R.E.; Al-Zawawi, E.; El-Bialy, T. Do orthodontic treatments using fixed appliances and clear aligner achieve comparable quality of occlusal contacts? Evid. Based Dent. 2022, 23, 160–161. [Google Scholar] [CrossRef] [PubMed]
- Kassam, S.K.; Stoops, F.R. Are clear aligners as effective as conventional fixed appliances? Evid. Based Dent. 2020, 21, 30–31. [Google Scholar] [CrossRef] [PubMed]
- Socransky, S.S.; Haffajee, A.D. Periodontal microbial ecology. Periodontol. 2000 2005, 38, 135–187. [Google Scholar] [CrossRef] [PubMed]
- Socransky, S.S.; Haffajee, A.D. Dental biofilms: Difficult therapeutic targets. Periodontol. 2000 2002, 28, 12–55. [Google Scholar] [CrossRef] [PubMed]
- Lovegrove, J.M. Dental plaque revisited: Bacteria associated with periodontal disease. J. N. Z. Soc. Periodontol. 2004, 87, 7–21. [Google Scholar] [PubMed]
- Bosshardt, D.D. The periodontal pocket: Pathogenesis, histopathology and consequences. Periodontol. 2000 2018, 76, 43–50. [Google Scholar] [CrossRef] [PubMed]
- Fine, D.H.; Patil, A.G.; Velusamy, S.K. Aggregatibacter actinomycetemcomitans (Aa) Under the Radar: Myths and Misunderstandings of Aa and Its Role in Aggressive Periodontitis. Front. Immunol. 2019, 10, 728. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shokeen, B.; Viloria, E.; Duong, E.; Rizvi, M.; Murillo, G.; Mullen, J.; Shi, B.; Dinis, M.; Li, H.; Tran, N.C.; et al. The impact of fixed orthodontic appliances and clear aligners on the oral microbiome and the association with clinical parameters: A longitudinal comparative study. Am. J. Orthod. Dentofac. Orthop. 2022, 161, e475–e485. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Ma, J.B.; Wang, B.; Zhang, X.; Yin, Y.L.; Bai, H. Alterations of the oral microbiome in patients treated with the Invisalign system or with fixed appliances. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 633–640, Erratum in: Am. J. Orthod. Dentofac. Orthop. 2020, 157, 4. [Google Scholar] [CrossRef] [PubMed]
- Baybekov, O.; Stanishevskiy, Y.; Sachivkina, N.; Bobunova, A.; Zhabo, N.; Avdonina, M. Isolation of Clinical Microbial Isolates during Orthodontic Aligner Therapy and Their Ability to Form Biofilm. Dent. J. 2023, 11, 13. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Quinzi, V.; Carli, E.; Mummolo, A.; De Benedictis, F.; Salvati, S.E.; Mampieri, G. Fixed and removable orthodontic retainers, effects on periodontal health compared: A systematic review. J. Oral. Biol. Craniofac. Res. 2023, 13, 337–346. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Giardino, L.; Grande, N.M.; Savadori, P.; Fabbro, M.D.; Plotino, G. Clinical and Histological Findings of Post-Treatment Infection in the Presence of Vertical Root Fracture and Apical Periodontitis: Case Reports. Eur. Endod. J. 2019, 4, 45–48. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cenzato, N.; Nobili, A.; Maspero, C. Prevalence of Dental Malocclusions in Different Geographical Areas: Scoping Review. Dent. J. 2021, 9, 117. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ferreira, S.B., Jr.; Figueiredo, C.M.; Almeida, A.L.; Assis, G.F.; Dionísio, T.J.; Santos, C.F. Clinical, histological, and microbiological findings in peri-implant disease: A pilot study. Implant. Dent. 2009, 18, 334–344. [Google Scholar] [CrossRef] [PubMed]
- Dyer, G.S.; Harris, E.F.; Vaden, J.L. Age effects on orthodontic treatment: Adolescents contrasted with adults. Am. J. Orthod. Dentofac. Orthop. 1991, 100, 523–530. [Google Scholar] [CrossRef] [PubMed]
- Khocht, A.; Zohn, H.; Deasy, M.; Chang, K.M. Assessment of periodontal status with PSR and traditional clinical periodontal examination. J. Am. Dent. Assoc. 1995, 126, 1658–1665. [Google Scholar] [CrossRef] [PubMed]
- Alasiri, M.M.; Almalki, A.; Alotaibi, S.; Alshehri, A.; Alkhuraiji, A.A.; Thomas, J.T. Association between Gingival Phenotype and Periodontal Disease Severity-A Comparative Longitudinal Study among Patients Undergoing Fixed Orthodontic Therapy and Invisalign Treatment. Healthcare 2024, 12, 656. [Google Scholar] [CrossRef] [PubMed]
- Bertoldi, C.; Forabosco, A.; Lalla, M.; Generali, L.; Zaffe, D.; Cortellini, P. How Intraday Index Changes Influence Periodontal Assessment: A Preliminary Study. Int. J. Dent. 2017, 2017, 7912158. [Google Scholar] [CrossRef] [PubMed]
- He, T.; Qu, L.; Chang, J.; Wang, J. Gingivitis Models—Relevant Approaches to Assess Oral Hygiene Products. J. Clin. Dent. 2018, 29, 45–51. [Google Scholar] [PubMed]
- Savadori, P.; Dalfino, S.; Piazzoni, M.; Parrini, M.; Del Fabbro, M.; Tartaglia, G.M.; Giardino, L. A simplified method for detecting Gram-positive and Gram-negative bacteria in dental histological samples: A preliminary and comparative study. Acta Histochem. 2023, 125, 151992, Erratum in: Acta Histochem. 2023, 151995. [Google Scholar] [CrossRef] [PubMed]
- Cerroni, S.; Pasquantonio, G.; Condò, R.; Cerroni, L. Orthodontic Fixed Appliance and Periodontal Status: An Updated Systematic Review. Open Dent. J. 2018, 12, 614–622. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Contaldo, M.; Lucchese, A.; Lajolo, C.; Rupe, C.; Di Stasio, D.; Romano, A.; Petruzzi, M.; Serpico, R. The Oral Microbiota Changes in Orthodontic Patients and Effects on Oral Health: An Overview. J. Clin. Med. 2021, 10, 780. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kinane, D.F.; Stathopoulou, P.G.; Papapanou, P.N. Periodontal diseases. Nat. Rev. Dis. Primers 2017, 3, 17038. [Google Scholar] [CrossRef] [PubMed]
- Giardino, L.; Bidossi, A.; Del Fabbro, M.; Savadori, P.; Maddalone, M.; Ferrari, L.; Ballal, N.V.; Das, S.; Rao, B.S.S. Antimicrobial activity, toxicity and accumulated hard-tissue debris (AHTD) removal efficacy of several chelating agents. Int. Endod. J. 2020, 53, 1093–1110. [Google Scholar] [CrossRef] [PubMed]
- Kozak, U.; Lasota, A.; Chałas, R. Changes in Distribution of Dental Biofilm after Insertion of Fixed Orthodontic Appliances. J. Clin. Med. 2021, 10, 5638. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Farronato, M.; Baselli, G.; Baldini, B.; Favia, G.; Tartaglia, G.M. 3D Cephalometric Normality Range: Auto Contractive Maps (ACM) Analysis in Selected Caucasian Skeletal Class I Age Groups. Bioengineering 2022, 9, 216. [Google Scholar] [CrossRef] [PubMed]
- Buccino, F.; Zagra, L.; Savadori, P.; Galluzzo, A.; Colombo, C.; Grossi, G.; Banfi, G.; Vergani, L. Mapping local mechanical properties of human healthy and osteoporotic femoral heads. Materialia 2021, 20, 101229. [Google Scholar] [CrossRef]
- Ren, Y.; Jongsma, M.A.; Mei, L.; van der Mei, H.C.; Busscher, H.J. Orthodontic treatment with fixed appliances and biofilm formation--a potential public health threat? Clin. Oral Investig. 2014, 18, 1711–1718. [Google Scholar] [CrossRef] [PubMed]
- Rivera-Yoshida, N.; Bottagisio, M.; Attanasi, D.; Savadori, P.; De Vecchi, E.; Bidossi, A.; Franci, A. Host Environment Shapes S. aureus Social Behavior as Revealed by Microscopy Pattern Formation and Dynamic Aggregation Analysis. Microorganisms 2022, 10, 526. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bidossi, A.; Bottagisio, M.; Savadori, P.; De Vecchi, E. Identification and Characterization of Planktonic Biofilm-Like Aggregates in Infected Synovial Fluids From Joint Infections. Front. Microbiol. 2020, 11, 1368. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gu, W.; Deng, X.; Lee, M.; Sucu, Y.D.; Arevalo, S.; Stryke, D.; Federman, S.; Gopez, A.; Reyes, K.; Zorn, K.; et al. Rapid pathogen detection by metagenomic next-generation sequencing of infected body fluids. Nat. Med. 2021, 27, 115–124. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Murakami, S.; Mealey, B.L.; Mariotti, A.; Chapple, I.L.C. Dental plaque-induced gingival conditions. J. Periodontol. 2018, 89 (Suppl. S1), S17–S27. [Google Scholar] [CrossRef] [PubMed]
- Kurgan, S.; Kantarci, A. Molecular basis for immunohistochemical and inflammatory changes during progression of gingivitis to periodontitis. Periodontol. 2000 2018, 76, 51–67. [Google Scholar] [CrossRef] [PubMed]
- Farronato, D.; Pasini, P.M.; Orsina, A.A.; Manfredini, M.; Azzi, L.; Farronato, M. Correlation between Buccal Bone Thickness at Implant Placement in Healed Sites and Buccal Soft Tissue Maturation Pattern: A Prospective Three-Year Study. Materials 2020, 13, 511. [Google Scholar] [CrossRef]
- Frank, D.; Cser, A.; Kolarovszki, B.; Farkas, N.; Miseta, A.; Nagy, T. Mechanical stress alters protein O-GlcNAc in human periodontal ligament cells. J. Cell. Mol. Med. 2019, 23, 6251–6259. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yudaev, P.; Chuev, V.; Klyukin, B.; Kuskov, A.; Mezhuev, Y.; Chistyakov, E. Polymeric Dental Nanomaterials: Antimicrobial Action. Polymers 2022, 14, 864. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kazarina, A.; Kuzmicka, J.; Bortkevica, S.; Zayakin, P.; Kimsis, J.; Igumnova, V.; Sadovska, D.; Freimane, L.; Kivrane, A.; Namina, A.; et al. Oral microbiome variations related to ageing: Possible implications beyond oral health. Arch. Microbiol. 2023, 205, 116. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cenzato, N.; Marcolongo, L.; Sanchez, S.; Maspero, C.M.N. Qualitative Microbiological Evaluation of Dental Plaque in Patients with Fixed Appliances and Clear Aligners J. Biol. Regul. Homeost. Agents 2022, 36, 647–653. [Google Scholar]

| FMPS | PI | FMBS | mSBI | PSR | |
|---|---|---|---|---|---|
| p-value | 0.006 * | 0.000 * | 0.860 | 0.712 | 0.010 * |
| Group Comparison | FMPS | PI | PSR |
|---|---|---|---|
| Aligners–Control | 0.006 * | 0.001 * | 0.029 * |
| Aligner–Fixed Appliance | 0.356 | 0.686 | 0.045 * |
| Fixed Appliance–Control | 0.159 | 0.002 * | 2.630 |
| Control | Aligners | Fixed Appliance | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| FMPS | PI | FMBS | mSBI | FMPS | PI | FMBS | mSBI | FMPS | PI | FMBS | mSBI | |
| 25% perc | 100 | 72 | 3 | 1 | 76 | 37 | 0 | 0 | 91 | 53 | 0 | 0 |
| Median | 100 | 84 | 9 | 3 | 93 | 55 | 8 | 3 | 100 | 64 | 7 | 3 |
| 75% perc | 100 | 92 | 23 | 10 | 100 | 69 | 18 | 6 | 100 | 73 | 23 | 14 |
| Lilliefors p-value | 0.001 * | 0.201 | 0.046 * | 0.005 * | 0.002 * | 0.834 | 0.017 * | 0.011 * | 0.001 * | 0.564 | 0.001 * | 0.001 * |
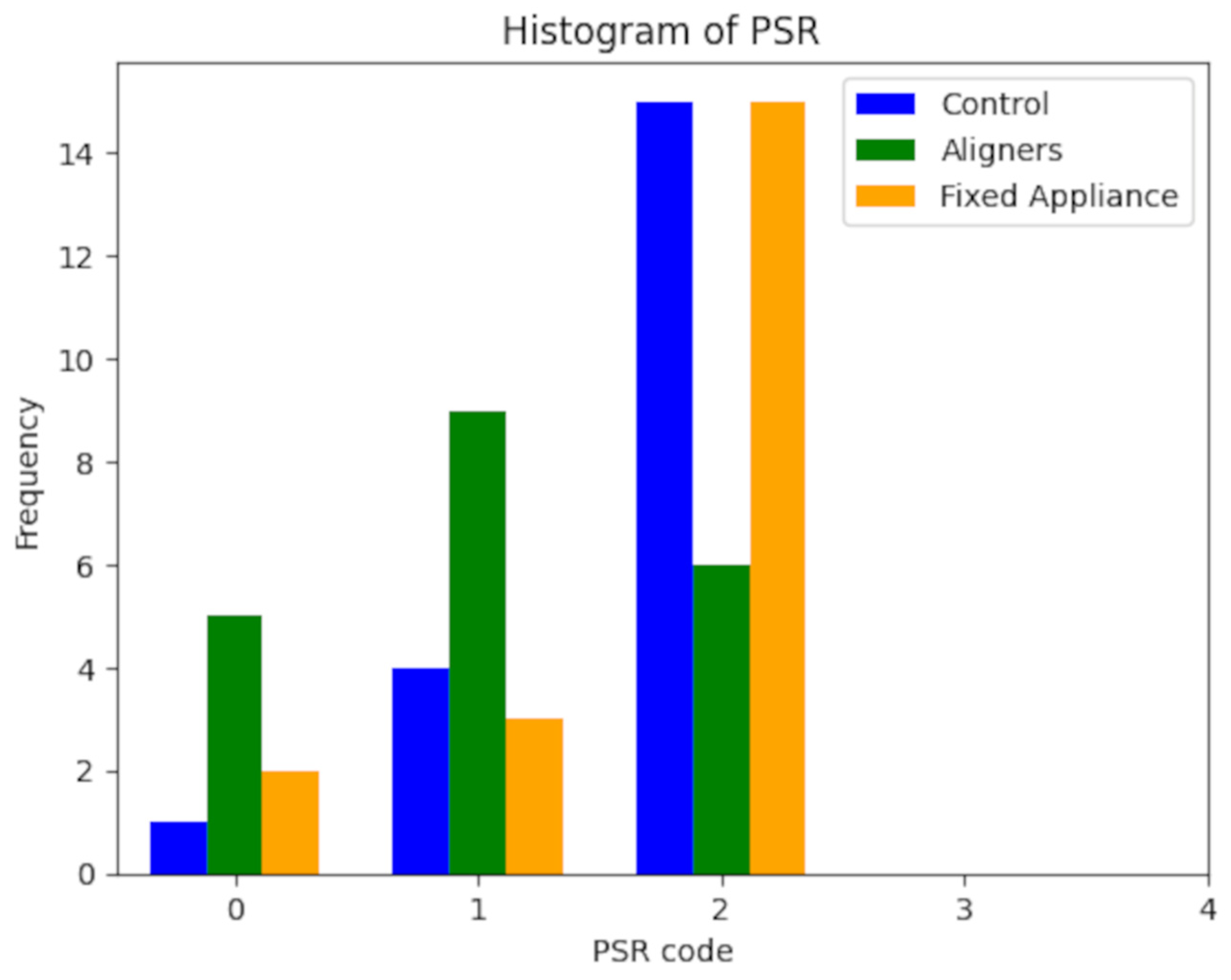
| PSR | |||
|---|---|---|---|
| Code | Control | Aligners | Fixed A. |
| 0 | 1 | 5 | 2 |
| 1 | 4 | 9 | 3 |
| 2 | 15 | 6 | 15 |
| 3 | 0 | 0 | 0 |
| Control | Aligners | Fixed Appliance | ||||
|---|---|---|---|---|---|---|
| Bacterial Species | Absolute | Relative [%] | Absolute | Relative [%] | Absolute | Relative [%] |
| C | 16 | 21 | 13 | 20 | 18 | 24 |
| B | 12 | 17 | 8 | 15 | 16 | 22 |
| S | 0 | 5.3 | 2 | 9.1 | 1 | 6.6 |
| L/F | 9 | 14 | 7 | 14 | 8 | 14 |
| FU | 7 | 12 | 4 | 11 | 8 | 14 |
| FI | 15 | 20 | 9 | 16 | 12 | 18 |
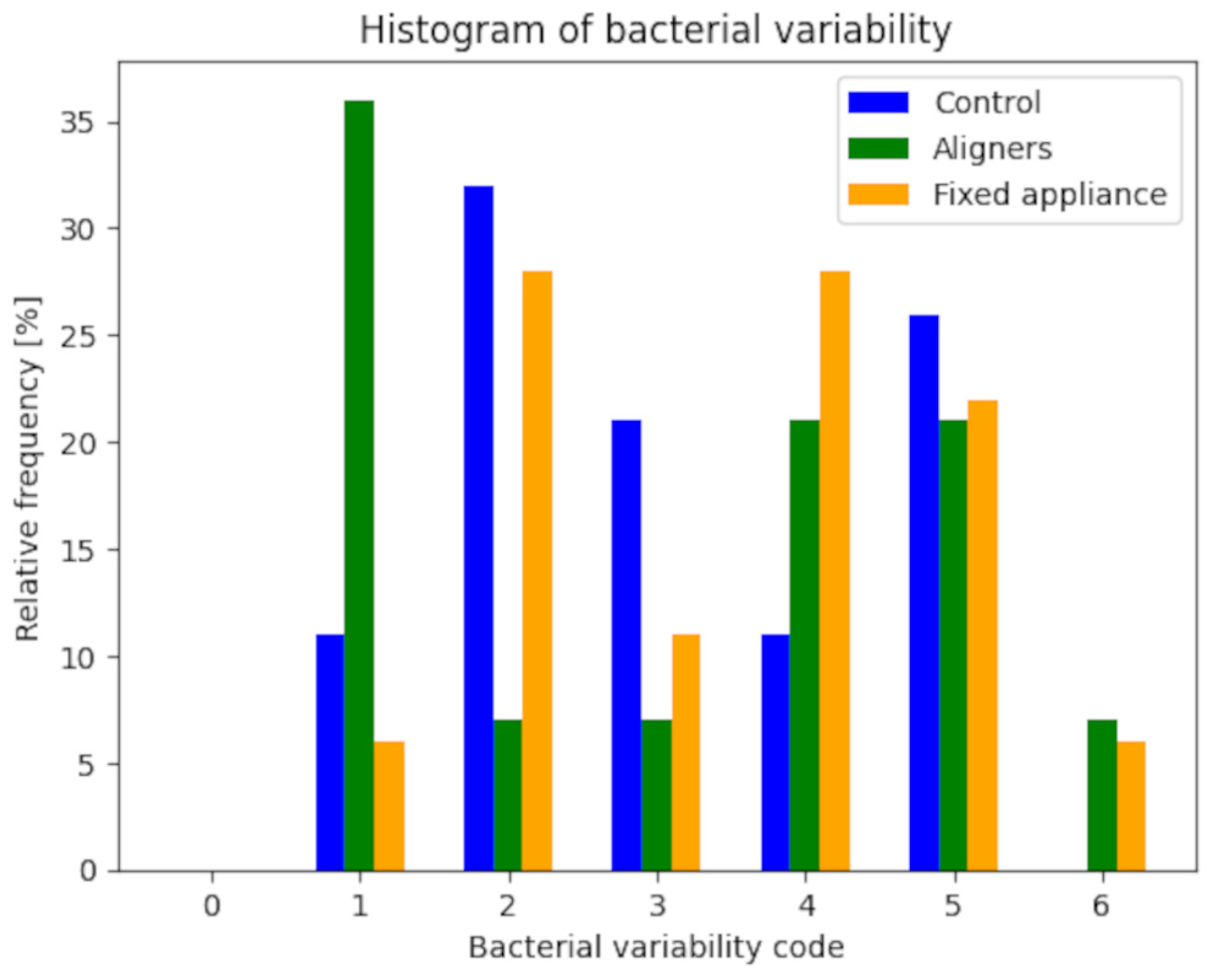
| Control | Aligners | Fixed Appliance | ||||
| Code | Absolute | Relative [%] | Absolute | Relative [%] | Absolute | Relative [%] |
| 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 1 | 2 | 11 | 5 | 36 | 1 | 6 |
| 2 | 6 | 32 | 1 | 7 | 5 | 28 |
| 3 | 4 | 21 | 1 | 7 | 2 | 11 |
| 4 | 2 | 11 | 3 | 21 | 5 | 28 |
| 5 | 5 | 26 | 3 | 21 | 4 | 22 |
| 6 | 0 | 0 | 1 | 7 | 1 | 6 |
| tot | 19 | 100 | 14 | 100 | 18 | 100 |
| Control | Aligners | Fixed Appliance | ||||
| Code | Absolute | Relative [%] | Absolute | Relative [%] | Absolute | Relative [%] |
| 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 1 | 2 | 11 | 5 | 36 | 1 | 6 |
| 2 | 6 | 32 | 1 | 7 | 5 | 28 |
| 3 | 4 | 21 | 1 | 7 | 2 | 11 |
| 4 | 2 | 11 | 3 | 21 | 5 | 28 |
| 5 | 5 | 26 | 3 | 21 | 4 | 22 |
| 6 | 0 | 0 | 1 | 7 | 1 | 6 |
| tot | 19 | 100 | 14 | 100 | 18 | 100 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cenzato, N.; Occhipinti, C.; D’amici, E.; Savadori, P.; Baldini, B.; Maspero, C. Microbiological Analysis of Plaque and Its Composition in Three Patient Groups under Different Orthodontic Treatments. Dent. J. 2024, 12, 168. https://doi.org/10.3390/dj12060168
Cenzato N, Occhipinti C, D’amici E, Savadori P, Baldini B, Maspero C. Microbiological Analysis of Plaque and Its Composition in Three Patient Groups under Different Orthodontic Treatments. Dentistry Journal. 2024; 12(6):168. https://doi.org/10.3390/dj12060168
Chicago/Turabian StyleCenzato, Niccolò, Chiara Occhipinti, Elena D’amici, Paolo Savadori, Benedetta Baldini, and Cinzia Maspero. 2024. "Microbiological Analysis of Plaque and Its Composition in Three Patient Groups under Different Orthodontic Treatments" Dentistry Journal 12, no. 6: 168. https://doi.org/10.3390/dj12060168
APA StyleCenzato, N., Occhipinti, C., D’amici, E., Savadori, P., Baldini, B., & Maspero, C. (2024). Microbiological Analysis of Plaque and Its Composition in Three Patient Groups under Different Orthodontic Treatments. Dentistry Journal, 12(6), 168. https://doi.org/10.3390/dj12060168








