Abstract
This in vitro study assessed the effect of different primers on the shear bond strength (SBS) and adhesive remnant index (ARI) of orthodontic brackets bonded to reinforced polyetheretherketone (PEEK) substrate. A total of 40 specimens were randomly distributed to two groups based on the primer used for orthodontic bonding: group 1 (control)—Transbond XT adhesive with Visio.link primer and group 2 (test)—orthodontic adhesive (Transbond XT) with traditional orthodontic primer. After bonding, specimens were thermocycled followed by SBS testing and ARI scoring of debonded specimens. Data were analyzed using the unpaired independent t-test and the Chi-square test. Group 1 specimens showed significantly higher SBS values (21.38 ± 1.48 MPa) compared to group 2 specimens (18.63 ± 1.29 MPa) (p < 0.0001). Adhesive remnant index scores showed no significant variations in bond failure modes and distributions between groups. The SBS obtained by the tested primers exceeded the clinically recommended value. Consequently, there is a comparable clinical application for both tested primers in orthodontic bonding, especially the traditional orthodontic primer, where the availability of Visio.link in clinical practice is not ensured.
1. Introduction
Bonding orthodontic brackets clinically is of paramount importance for the overall effectiveness of orthodontic treatment [1]. In the past few years, adult orthodontic treatment has gained popularity [1,2,3]. Accordingly, there may be clinical scenarios in which orthodontic brackets are bonded to prosthetic or restorative surfaces. When a fixed dental prosthesis is planned for an orthodontic patient, it is typically recommended that the insertion of the final prosthetic restoration be delayed until the completion of orthodontic therapy [1]. This delay permits the tooth to be repositioned to its final position after orthodontic treatment is completed before placing the final restoration [2,3]. In addition, any surface damage to the fixed restoration upon removal of bonded orthodontic brackets may necessitate replacement of the fixed dental restoration [3]. Therefore, interim restorations are placed between the completion of orthodontic therapy and the placement of the final prosthetic restoration. Furthermore, they prevent tooth decay and fracture while protecting the pulp and periodontal tissues [2,4].
Computer-aided design and computer-aided manufacturing (CAD/CAM) technology have facilitated using pre-polymerized materials to fabricate long-term temporary restorations with lower liability for fracture and marginal discrepancy than the direct method [3]. Polymethylmethacrylate (PMMA) is a widely utilized material for fabricating interim crowns using CAD/CAM technology [5]. However, polyetherether-ketone (PEEK), a high performance polymer (HPP), has emerged as a potential material for indirect long-term interim restoration fabrication in recent years. PEEK is a thermoplastic, aromatic, semi-crystalline material with a linear structure resulting from the binding of ether and ketone groups around aryl rings [6,7]. The growing popularity of PEEK among dental practitioners is due to its low modulus of elasticity, which closely resembles natural bone, high resistance to chemical wear hydrolysis, superior mechanical properties, and high temperature resistance [8,9]. Nevertheless, the inherent hydrophobic nature of unmodified PEEK limits its clinical use, and wetting the material with hydrophobic resin is challenging [10].
Reinforced PEEK is known as bioactive PEEK, and contains ceramic fillers or Bio-HPP, 20% of which contains ceramic fillers [7,8]. The white shade and excellent polishability of Bio-HPP makes it a potential alternative to other restorative materials for the fabrication of fixed dental restorations [8]. Bio-HPP has emerged as an alternative for tooth-colored crowns [10,11], especially for people with parafunctions such as bruxism, because it does not abrade antagonist teeth [7]. It can also be used to fabricate endo-crowns to manage endodontically treated teeth in young adolescents and adults [7].
However, bonding to reinforced PEEK has been an area of interest for recent research [11] in which air-borne particle abrasion or sandblasting using aluminum oxide (Al2O3) particles with or without silica coating has been proposed as a suitable method for the surface modification of PEEK. This creates micro-roughness for micro-mechanical interlocking with resin and makes it more prone to moisture, allowing for better wetting with more hydrophobic resins [11,12]. Chemical modifications have also been proposed to enhance bonding to PEEK-based materials, including the application of adhesive primers such as Visio.link® (Bredent, Germany) or Signum PEEK Bond® (Kulzer GmbH, Hanau, Germany) [12]. Combined mechanical surface roughening and chemical adhesive treatments are recommended to improve material adhesiveness to a wetting hydrophobic resin by diversifying functional groups and creating a micromechanical interlock [12].
In the literature, combining mechanical surface pretreatment with adhesive primers, namely PEEK’s adhesive primer Visio.link, is proposed to increase shear bond strength (SBS) [12]. As a routine surface treatment, it is recommended that Visio.link be used as the adhesive primer when bonding to PEEK [6,12]. However, in a systematic review of adhesion to HPP in dentistry, Gama et al. [12] concluded that only a few studies had been conducted to compare SBS among specimens using various bonding adhesives, which was insufficient for them to conduct a meta-analysis. Nonetheless, in a study by Lee et al. [13] different dental adhesives and primers were applied to surface-treated PEEK, and it was concluded that a self-etching universal primer containing both MDP and a silane coupling agent is a suitable alternative to the manufacturer’s recommended primer. During orthodontic bonding, Visio.link is often less readily available to orthodontists than orthodontic primers. Nonetheless, the recommendation to use different dental adhesive primers when bonding to PEEK in clinical practice is unclear.
Therefore, the aim of this study was to assess the effect of different primers (the manufacturer’s recommended primer or an orthodontic primer) on the shear bond strength and adhesive remnant index (ARI) of orthodontic brackets bonded to reinforced PEEK. The null hypothesis of the current study was that the SBS of metallic orthodontic brackets bonded to reinforced PEEK using two adhesive primers would not vary significantly.
2. Materials and Methods
2.1. Specimen Preparation
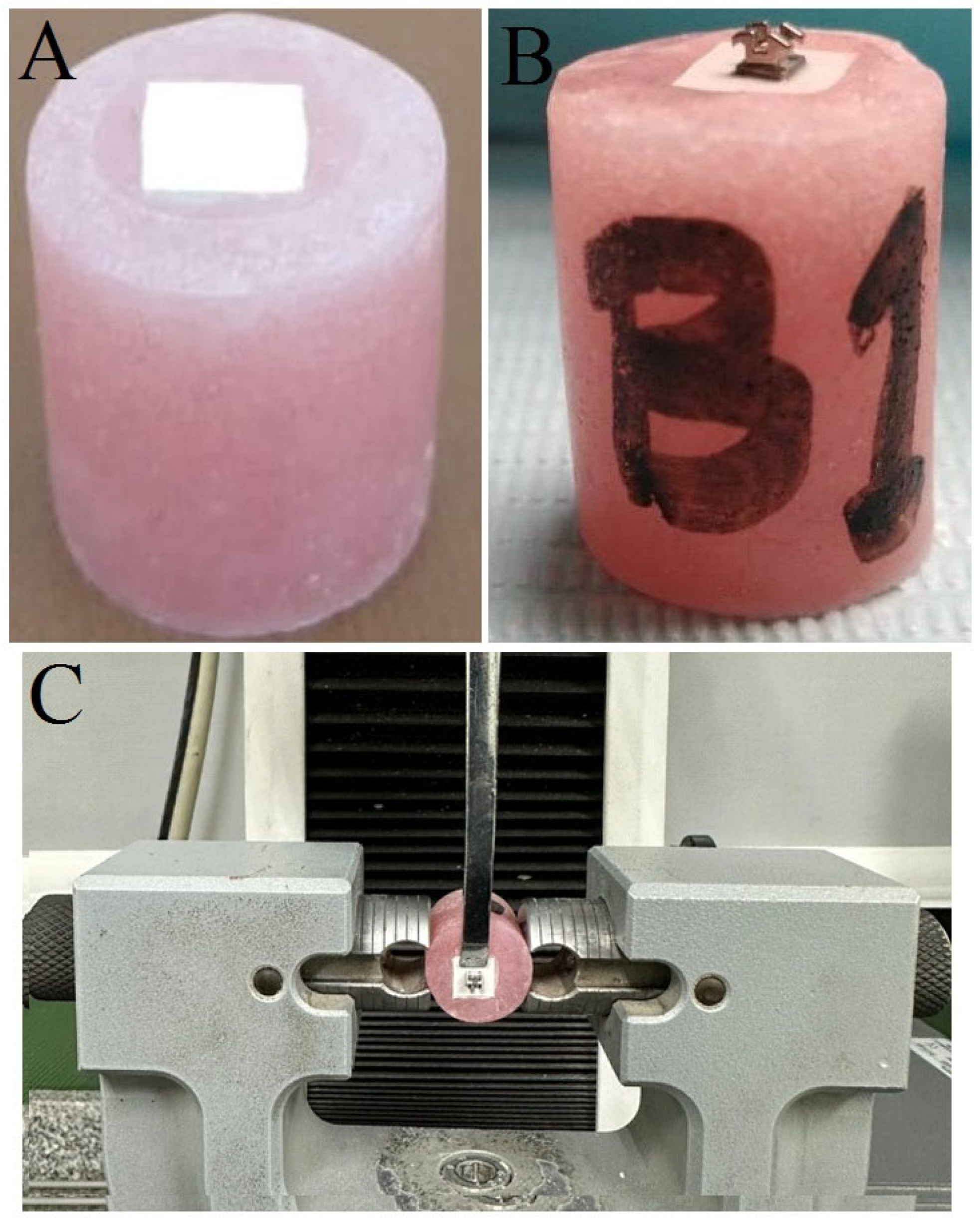
According to a prior investigation [14], 40 specimens (n = 20 for each group) were adequate to show significant differences in SBS between groups. Forty rectangular specimens (5 × 7 × 2 mm3) were sectioned from prefabricated PEEK blanks (breCAM, Bio-HPP; Bredent GmbH, Senden, Germany). PEEK blanks were sectioned as per the required dimensions utilizing an automated precision saw (Isomet® 4000, Buehler, Lake Bluff, IL, USA) using a diamond cut-off wheel saw at 2500 rpm and a continuous water coolant [15]. Next, sectioned specimens were contained in individual acrylic cylinders using self-curing acrylic resin (Acrostone Dental and Medical Supplies, Cairo, Egypt) (Figure 1A). The bonding surfaces of all specimens were ground and polished with sequential use of P600 and P800 grit silicon carbide paper (3M™, St. Paul, MN, USA) at 300 rpm under water coolant using an automated LaboPol-25 grinding and polishing machine (LaboPol, Struers GmbH, Copenhagen, Denmark). To standardize the polishing process, all specimens were finished and polished by a single operator (H.R.M). Polished specimens were cleaned for 10 min in an ultrasonic cleaner (Krisbow CD4862, Shenzhen, China) containing distilled water, followed by air-drying prior to surface treatment [5,16,17,18].
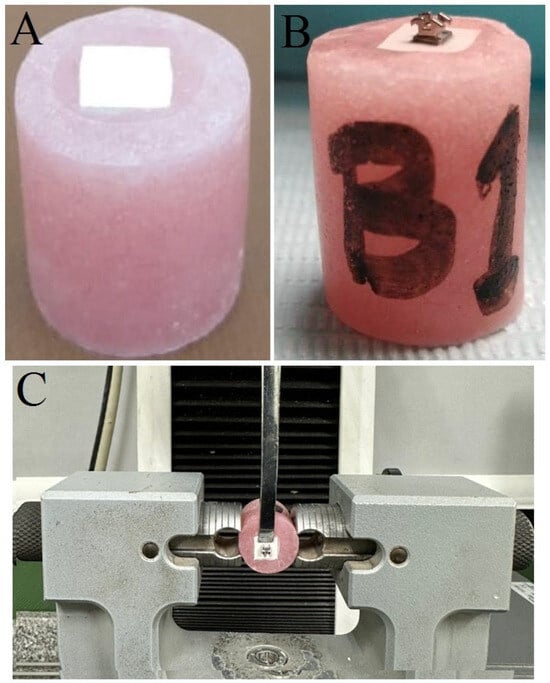
Figure 1.
Specimen preparation and SBS set-up. (A) PEEK specimens embedded in acrylic; (B) orthodontic bracket bonded to surface-treated specimen, and (C) specimen mounted in universal testing machine for SBS test.
2.2. Surface Treatment and Specimen Grouping
Surfaces of PEEK specimens were sandblasted using 110 µm Al2O3 particles for 30 s using a pressure of 0.25 MPa from a distance of 10 mm, followed by 10 min cleaning using distilled water in an ultrasonic unit and air-drying for 30 s [5,17,18,19]. Surface-treated specimens were randomly assigned to one of two groups (n = 20) based on the primer application of the bonding surface, as follows:
- Group 1 (control): Visio.link (Lot#: 210802, Expiry: 02/24, Bredent GmbH & Co. KG, Senden, Germany).
- Group 2 (test): traditional orthodontic primer (Transbond XT, Lot#: MB4GA, Expiry: 05/24, 3M Unitek, Monrovia, CA, USA).
2.3. Bracket Bonding
Group 1 (control): A thin film of Visio.link primer was applied onto the surface-treated PEEK surface, distributed via gentle air spray from a distance of 15 mm, and light-cured for 90 s using a hand-held unit (1000 mW/cm2, Woodpecker Guilin, Guangxi, China) [17]. Metal mandibular incisor brackets (0.022-inch, Gemini series, 3M Unitek, Monrovia, CA, USA) with a 10.5 mm2 average bonding area were bonded to the PEEK surface. The bracket base was covered with a small amount of orthodontic adhesive (Transbond XT, Lot#: MB4GA, Expiry: 05/24, 3M Unitek, Monrovia, CA, USA) and pressed against the specimen’s surface. Excess adhesive was removed (Figure 1B) and bracket surfaces were light-cured for 40 s [20,21].
Group 2 (test): The treated surface was coated with a thin film of Transbond XT primer, distributed onto the specimen surface via gentle air spray at a distance of 15 mm, and light-cured for 10 s. Bracket bonding was identical to the procedure detailed for group 1 specimens.
Bonded specimens were thermocycled to replicate the oral environment after being stored in distilled water at 37 °C for 24 h. The thermocycler apparatus (SD Mechatronik, Feldkirchen-Westerham, Germany) operated for 1500 cycles, between 5 to 55 °C, with a dwell time of 20 s and a transfer time of 10 s [22,23,24].
2.4. Shear Bond Strength Testing
A random number was allotted to each specimen before testing to avoid bias during testing. SBS tests were performed by a universal testing machine (Model 2710-113, Instron, Norwood, MA, USA). A vertical shear load was applied to each bracket’s base parallel to the PEEK/adhesive/bracket interface at a crosshead speed of 1 ± 0.1 mm/min until fracture (Figure 1C) [25,26,27]. The debonding load was recorded in Newtons (N) and then divided by the bracket base area (10.5 mm2) to obtain the SBS in megapascals (MPa) [28].
2.5. Adhesive Remnant Index (ARI)
Specimens’ surfaces after debonding were examined utilizing a stereomicroscope under ×20 magnification (Nikon SMZ745T, Tokyo, Japan) to quantify the remaining adhesive amount on the surface. Each debonded specimen was assigned a score based on the adhesive remnant index (ARI), as detailed below [29]:
Score 0 = no Transbond XT adhesive left on the PEEK surface;
Score 1 ≤ 50% of the Transbond XT adhesive left on the PEEK surface;
Score 2 ≥ 50% of the Transbond XT adhesive left on the PEEK surface;
Score 3 = all of the Transbond XT adhesive left on the PEEK surface.
2.6. Scanning Electron Microscopy (SEM) Analysis
A representative PEEK substrate was examined under SEM (TESCAN VEGA, Brno-Kohoutovice, Czech Republic) to evaluate sandblasting’s effects on the PEEK surface. Furthermore, a representative specimen was also examined under SEM after debonding to examine adhesive remains on the PEEK surface.
2.7. Statistical Analysis
Data analysis was performed with a statistical software package (v.24, IBM SPSS, Armonk, NY, USA). Descriptive statistics were generated for the studied groups. The unpaired independent t-test was applied to compare groups, preceded by assessment of normality through Shapiro–Wilk and Kolmogorov–Smirnov tests. These test results indicated a normal distribution of the parametric data under consideration. The Chi-square test was used to compare ARI scores between the studied groups (α ≤ 0.05).
3. Results
3.1. Shear Bond Strength
Table 1 presents descriptive statistics of the studied groups. The SBS of group 1 (Visio.link primer) ranged between 18.70 MPa and 23.50 MPa. On the contrary, the SBS of group 2 (Transbond XT traditional primer) ranged between 16.75 MPa and 21.10 MPa. The 95% confidence intervals show the range of reasonable values for the true mean SBS in the underlying population, ranging from 20.68 to 22.07 for group 1 and from 18.03 to 19.24 for group 2. Overall, the descriptive statistics indicate that group 1 specimens resulted in higher SBS on average, with more variability, compared to group 2 specimens.

Table 1.
Descriptive statistics of SBS values of the studied groups.
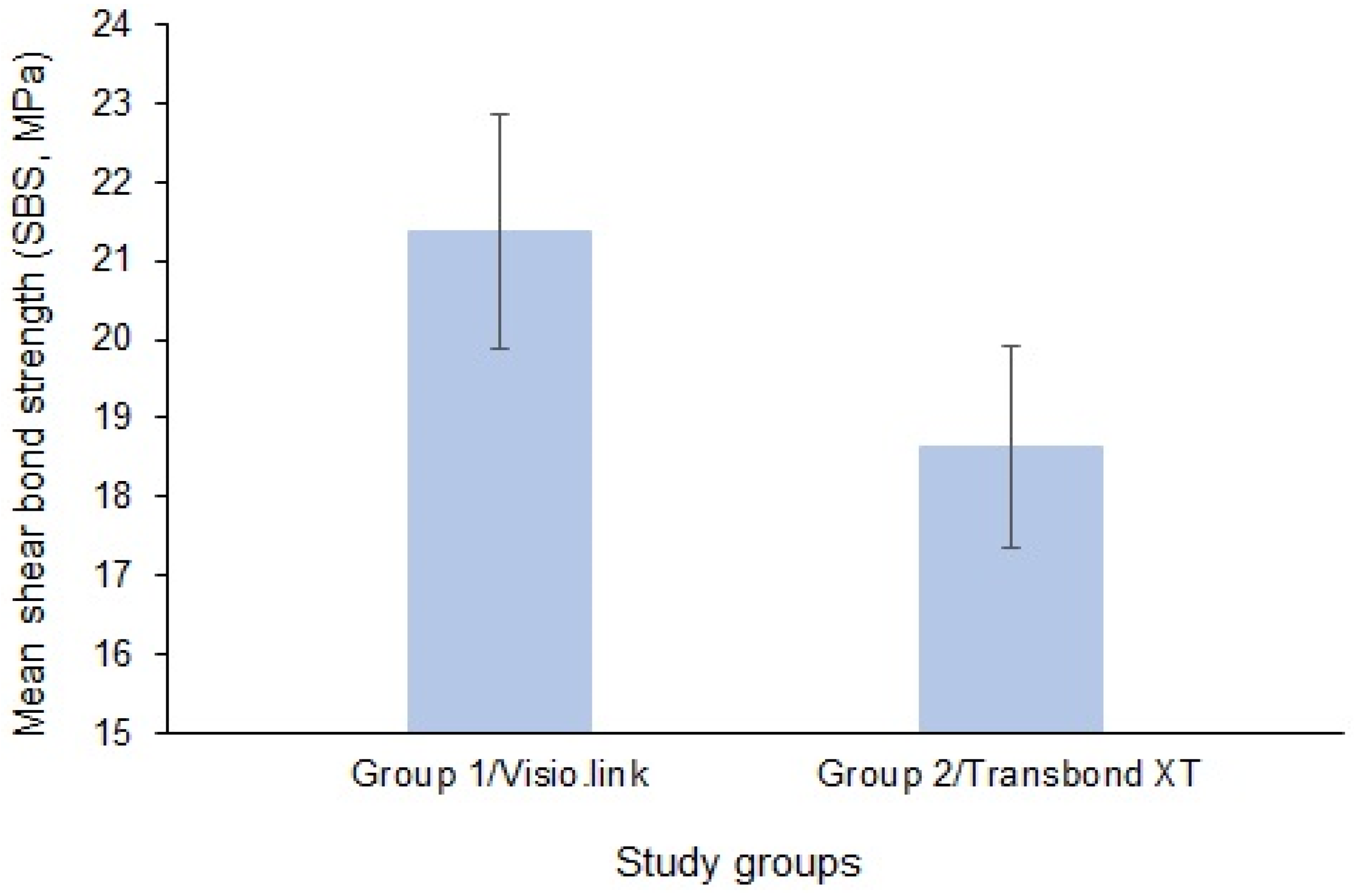
The mean ± SD of SBS values of the studied groups are presented in Figure 1. The mean SBS of group 1 PEEK specimens was 21.38 ± 1.48 compared to 18.63 ± 1.29 for group 2 PEEK specimens.
Table 2 presents results of an unpaired t-test comparing the mean SBS between the two groups. With a p-value less than 0.0001, the difference in mean SBS was statistically significant. The two-tailed p-value indicates this was a non-directional hypothesis test. The large t-value of 6.237 with 38 degrees of freedom also reflects the highly significant difference between groups.

Table 2.
Comparative statistics of SBS between groups using unpaired independent t-test.
3.2. Adhesive Remnant Index (ARI)
Table 3 presents a comparative analysis of ARI scores between groups using a Chi-square test. In group 1, there were no specimens with a score of 0, 3 specimens (15%) scored 1, 11 specimens (55%) scored 2, and 6 specimens (30%) scored 3. For group 2, there were no specimens with an ARI score of 0, 5 specimens (25%) scored 1, 10 specimens (50%) scored 2, and 5 specimens (25%) scored 3. Chi-square p-values comparing the distributions of scores 1, 2, and 3 individually between the two groups were not statistically significant. This indicates a non-significant difference in the bond failure modes and distribution of ARI scores of Visio.link primer versus Transbond XT orthodontic primer.

Table 3.
Comparative statistics of adhesive remnant index (ARI) scores between groups using Chi-square test.
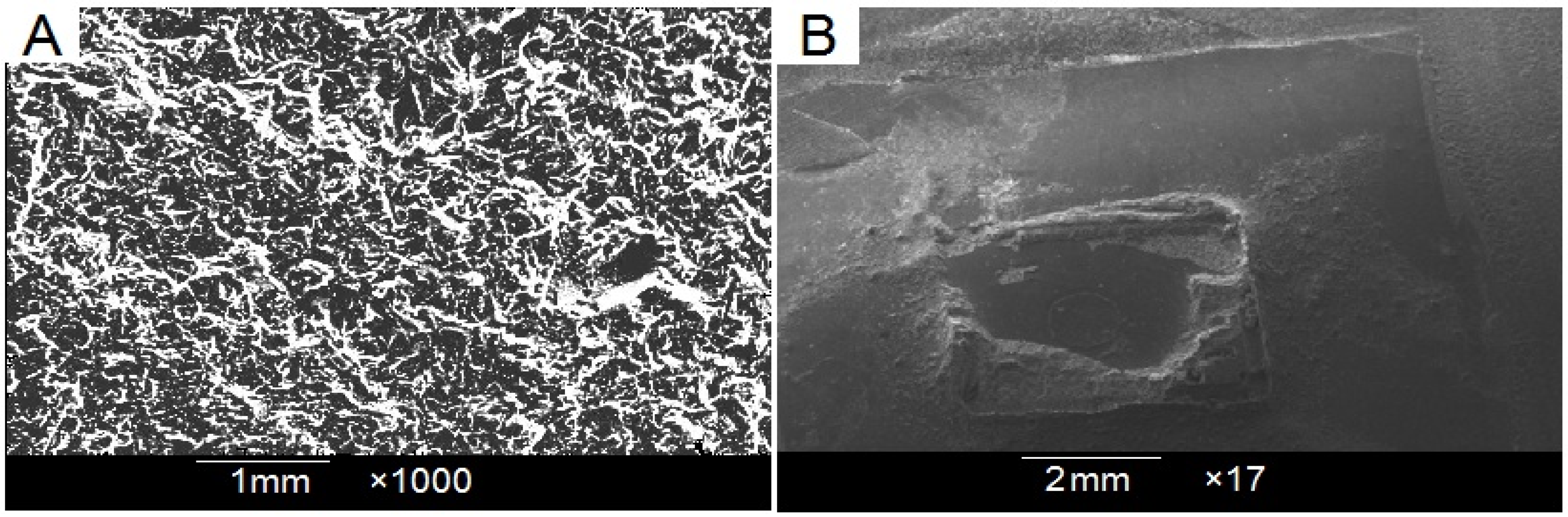
3.3. Scanning Electron Microscopy (SEM) Observation
A SEM micrograph of the surface-treated and debonded PEEK specimen is presented in Figure 2. The surface-treated PEEK surface (Figure 3A) showed an irregularly speckled pattern with deep grooves and craters. The PEEK specimen, after debonding (Figure 3B), showed a significant amount of adhesive remaining on most bracket base surface areas (representing an ARI score > 2).
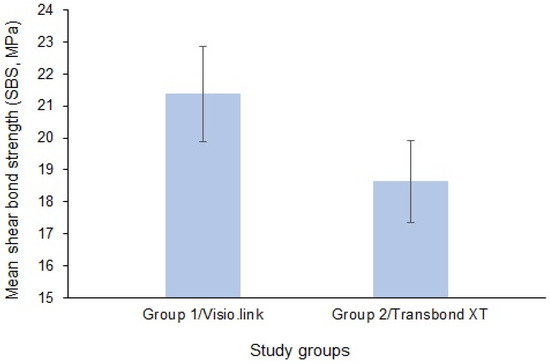
Figure 2.
Shear bond strengths of the studied groups.
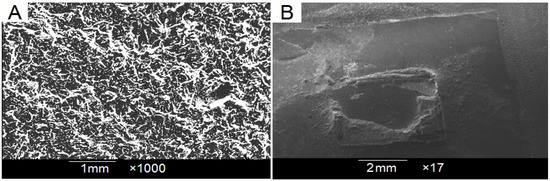
Figure 3.
(A) Surface-treated PEEK specimen; (B) PEEK surface after debonding showing significant amount of remaining adhesive material.
4. Discussion
The current study assessed the SBS of orthodontic brackets bonded to PEEK surfaces using either manufacturer-recommended adhesive primer or traditional orthodontic primer. To the best of the authors’ knowledge, this is the first study to assess the SBS of orthodontic brackets bonded to reinforced PEEK. It was hypothesized that the SBS of orthodontic brackets bonded to reinforced PEEK using two adhesive primers would not significantly vary. The data analysis outcome recommends rejecting the hypothesis, as there was a significant difference in SBS values between the two studied groups.
The literature recommends that the minimum SBS be in the range of 6–8 MPa, and the maximum SBS must be lower than the fracture threshold of enamel, which is around 14 MPa [23,30]. However, it must be remembered that SBS obtained in vitro are typically 40% higher than those obtained in vivo owing to the complexity of the oral environment, where moisture contamination can noticeably reduce the SBS [31]. The current study demonstrated that the SBS of brackets bonded using Visio.link primer and traditional orthodontic primers were 21.38 ± 1.486 MPa and 18.63 ± 1.291 MPa, respectively. The difference in SBS between the primer groups was statistically significant; however, the difference seemed clinically irrelevant, as both these values exceeded the recommended optimal SBS values. In orthodontic practice, obtaining optimal SBS rather than the maximum possible SBS is preferable [32]. Brackets bonded to fixed prosthodontic surfaces should be compatible to resist the oral biomechanics, masticatory forces, and functional activities of the patient, but also adequate enough to facilitate debonding upon treatment completion without any deleterious effect on the bonded surface of the restoration [33].
In this study, PEEK specimens were surface-treated using sandblasting, as it is a simple and safe intraoral method for surface pretreatment that increases the micro-roughness and bonding area of PEEK material, subsequently improving the micromechanical interlocking of bonding agents. Additionally, it eliminates all organic contaminants from the material’s surface with surface activation [16,33]. Visio.link adhesive primer is the recommended standard primer for bonding to PEEK surfaces, as it provides a reliable bond between PEEK and resin regardless of the surface treatment [16,17]. However, this primer may not be readily available, and an orthodontist may be compelled to use traditional orthodontic primer. Although different primers were used, Transbond XT adhesive was used to bond the brackets in both groups, as it is regarded as the gold standard light-cured orthodontic adhesive [21]. Previous studies have predominantly used premolar brackets in their SBS studies; however, in the current study, mandibular incisors metal brackets were used, as their flat base provided maximum adaptation to the flat surface of PEEK specimens [34].
The oral environment undergoes temperature fluctuations (between 0 and 65 °C) that can impact the bond strength of adhesives and restorations. The International Organization for Standardization (ISO) recommends a minimum of 500 cycles at 5–55 °C, 20 s of dwell time, and 5–10 s transfer time to simulate an oral environment [35]. These 500 cycles, which mimic less than two months, are insufficient compared to the average orthodontic treatment time, which extends over one year. Conversely, specimens in this study underwent 1500 thermocycles at 5–55 °C to more accurately replicate oral and clinical thermal stress conditions.
The SBS test is frequently employed to assess the adhesion of dental materials. Conventional shear tests are preferred because they are easy to perform, require minimal tools and specimen preparation, and provide an extensive view of the adhesion strength—despite the SBS test being debatable, deemed unsatisfactory, and requiring that many variables be considered [35].
The adhesion remnant index (ARI) is the most popular and simplest method for assessing adhesion between the bonding substrate and bracket base. This qualitative and subjective index is used to evaluate adhesion quality by assessing adhesive remnants on the bonded surface and identifying the bond failure site after bracket removal [31,32,36]. It is a quick and easy procedure requiring no additional apparatus. Previous studies have shown no significant differences in ARI scores between qualitative visual scoring, elemental mapping, and SEM analysis [37,38]. On the contrary, the reliability of how magnification affects adhesive remnant interpretation has been questioned [39].
Surface damage or fracture at the interface may result from a robust adhesion between the bonding surface and the adhesive resin, which is indicated by an increased ARI score. Consequently, to lower the possibility of restoration damage or surface cracking during bracket removal, failure within the adhesive layer or between the bracket base and adhesive is desirable [31,40,41,42]. The current investigation showed a non-significant difference in bond failure types. Bond failures occurred frequently at the bracket–adhesive contact in both groups, leaving nearly all adhesive on the specimen surface (scores 2 and 3) (Figure 2B). Previous studies have indicated an association between failure mode and bond strength, with higher bond strengths associated with more mixed fractures. As indicated by scores 2 and 3, the bracket–adhesive interface can be considered the most advantageous failure site for safe debonding because most of the adhesive remains on the bonding surface [43]. However, the surface should be meticulously finished and polished to remove adhesive remnants.
The present study had a few limitations that are worth mentioning. Although care was taken to simulate the intra-oral environment as closely as possible, factors such as the presence of saliva, occlusal forces, diet, and oral hygiene methods were not considered. Secondly, the significant difference in SBS between primer groups was inconsistent with non-significant ARI values. Finally, the findings of this study could not be compared to other similar studies, as there were no data available on orthodontic bonding to PEEK surfaces at the time of this investigation. Future studies should focus on SBS in terms of PEEK crowns, aesthetic brackets, and different surface conditioning methods. Also, it would be compelling to evaluate the immediate SBS rather than the 24 h SBS, as archwires are ligated to brackets within 15 min of orthodontic bonding in clinical conditions.
5. Conclusions
Within this study’s limitations, the following conclusions were drawn from this laboratory study:
- (a)
- SBS values obtained with the use of both tested primers exceeded the clinically recommended value (6–8 MPa).
- (b)
- SBS values of Visio.link primer (21.38 ± 1.48) were statistically significant compared to those of traditional Transbond XT primer (18.63 ± 1.29) (p < 0.0001).
- (c)
- There was a non-significant difference in bond failure modes and the distribution of ARI scores between Visio.link and Transbond XT primers.
- (d)
- There is a comparable clinical application for both tested primers in the orthodontic bonding of metal brackets to a PEEK substrate.
- (e)
- The use of readily available traditional orthodontic primer in clinical orthodontic bonding to a PEEK surface is practical if there is no Visio.link available.
Author Contributions
Conceptualization, A.A.E.-A., A.E.E. and E.M.K.; Data curation, K.S.E., H.R.M. and M.A.A.; Formal analysis, H.R.M., A.E.E., M.A.A., E.M.K. and A.L.A.; Funding acquisition, A.E.E.; Investigation, K.S.E. and H.R.M.; Methodology, A.A.E.-A., K.S.E., H.R.M., K.S.A., M.A.A. and A.L.A.; Project administration, H.R.M., A.E.E., K.S.A. and E.M.K.; Resources, A.E.E., K.S.A. and E.M.K.; Software, K.S.A.; Supervision, A.A.E.-A.; Validation, K.S.E., K.S.A., M.A.A. and A.L.A.; Visualization, K.S.A. and E.M.K.; Writing—original draft, A.A.E.-A.; Writing—review and editing, A.A.E.-A., K.S.E., M.A.A. and A.L.A. All authors have read and agreed to the published version of the manuscript.
Funding
This study received no external funding.
Institutional Review Board Statement
Not applicable to this study.
Informed Consent Statement
Not applicable to this study.
Data Availability Statement
Available data are contained within the article.
Conflicts of Interest
The authors confirm no conflicts of interest.
References
- Najafi, H.Z.; Moradi, M.; Torkan, S. Effect of different surface treatment methods on the shear bond strength of orthodontic brackets to temporary crowns. Int. Orthod. 2019, 17, 89–95. [Google Scholar] [CrossRef] [PubMed]
- Fotovat, F.; Shishehian, A.; Alijani, S.; Alafchi, B.; Parchami, P. Comparison of shear bond strength of orthodontic stainless-steel brackets on temporary crowns fabricated by three different methods: An in vitro study. Int. Orthod. 2022, 20, 100641. [Google Scholar] [CrossRef] [PubMed]
- Morales, K.; Garces, G.; Yagnam, S.; Bustos, V.; Belfus, J.; Rojas, V. Comparison of shear bond strength of metal orthodontic brackets bonded to a CAD/CAM prosthetic provisional material after the use of a self-adhesive resin cement versus a light adhesive paste and different surface conditioning protocols: An in vitro study. Int. Orthod. 2022, 20, 100661. [Google Scholar] [CrossRef] [PubMed]
- Goracci, C.; Ozcan, M.; Franchi, L.; Di Bello, G.; Louca, C.; Vichi, A. Bracket bonding to polymethylmethacrylate-based materials for computer-aided design/manufacture of temporary restorations: Influence of mechanical treatment and chemical treatment with universal adhesives. Korean J. Orthod. 2019, 49, 404–412. [Google Scholar] [CrossRef] [PubMed]
- Benli, M.; Eker-Gumus, B.; Kahraman, Y.; Huck, O.; Ozcan, M. Can polylactic acid be a CAD/CAM material for provisional crown restorations in terms of fit and fracture strength? Dent. Mater. J. 2021, 40, 772–780. [Google Scholar] [CrossRef] [PubMed]
- Akay, C.; Israfil, N.; Pat, S. Enhancement of adhesive bonding properties of polyetheretherketone-based materials using plasma surface modifications. J. Adhes. Dent. 2022, 24, 117–124. [Google Scholar] [PubMed]
- Georgiev, J.; Vlahova, A.; Kissov, H.; Aleksandrov, S.; Kazakova, R. Possible application of BioHPP in prosthetic dentistry: A literature review. J. IMAB–Annu. Proceeding Sci. Pap. 2018, 24, 1896–1898. [Google Scholar] [CrossRef]
- Skirbutis, G.; Dzingutė, A.; Masiliūnaitė, V.; Šulcaitė, G.; Žilinskas, J. PEEK polymer’s properties and its use in prosthodontics. A review. Stomatologija 2018, 20, 54–58. [Google Scholar] [PubMed]
- Tekin, S.; Cangül, S.; Adıgüzel, Ö.; Değer, Y. Areas for use of PEEK material in dentistry. Int. Dent. Res. 2018, 8, 84–92. [Google Scholar] [CrossRef]
- Bathala, L.; Majeti, V.; Rachuri, N.; Singh, N.; Gedela, S. The role of polyether ether ketone (PEEK) in dentistry—A review. J. Med. Life 2019, 12, 5. [Google Scholar] [CrossRef]
- Alexakou, E.; Damanaki, M.; Zoidis, P.; Bakiri, E.; Mouzis, N.; Smidt, G.; Kourtis, S. PEEK high performance polymers: A review of properties and clinical applications in prosthodontics and restorative dentistry. Eur. J. Prosthodont. Restor. Dent. 2019, 27, 113–121. [Google Scholar]
- Gama, L.T.; Duque, T.M.; Özcan, M.; Philippi, A.G.; Mezzomo, L.A.M.; Gonçalves, T.M.S.V. Adhesion to high-performance polymers applied in dentistry: A systematic review. Dent. Mater. 2020, 36, e93–e108. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.-S.; Shin, M.-S.; Lee, J.-Y.; Ryu, J.-J.; Shin, S.-W. Shear bond strength of composite resin to high performance polymer PEKK according to surface treatments and bonding materials. J. Adv. Prosthodont. 2017, 9, 350. [Google Scholar] [CrossRef] [PubMed]
- Rambhia, S.; Heshmati, R.; Dhuru, V.; Iacopino, A. Shear bond strength of orthodontic brackets bonded to provisional crown materials utilizing two different adhesives. Angle Orthod. 2009, 79, 784–789. [Google Scholar] [CrossRef] [PubMed]
- Fouda, A.M.; Atta, O.; Kassem, A.S.; Desoky, M.; Bourauel, C. Wear behavior and abrasiveness of monolithic CAD/CAM ceramics after simulated mastication. Clin. Oral Investig. 2022, 26, 6593–6605. [Google Scholar] [CrossRef] [PubMed]
- Caglar, I.; Ates, S.M.; Yesil Duymus, Z. An In Vitro Evaluation of the Effect of Various Adhesives and Surface Treatments on Bond Strength of Resin Cement to Polyetheretherketone. J. Prosthodont. 2019, 28, e342–e349. [Google Scholar] [CrossRef] [PubMed]
- Gouveia, D.; Razzoog, M.E.; Sierraalta, M.; Alfaro, M.F. Effect of surface treatment and manufacturing process on the shear bond strength of veneering composite resin to polyetherketoneketone (PEKK) and polyetheretherketone (PEEK). J. Prosthet. Dent. 2021, 128, 1061–1066. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Qian, Y.; Zhu, Y.; Liu, H.; Gan, K.; Guo, J. The effect of different surface treatments on the bond strength of PEEK composite materials. Dent. Mater. 2014, 30, e209–e215. [Google Scholar] [CrossRef] [PubMed]
- Eltombakshy, M.A.; Elattar, M.S.; Ahmed, D.M. Shear Bond Strength of different resin-based materials Processed on Poly-ether-ether ketone frameworks (In Vitro Study). Alex. Dent. J. 2019, 44, 93–98. [Google Scholar] [CrossRef]
- Behnaz, M.; Dalaie, K.; Mirmohammadsadeghi, H.; Salehi, H.; Rakhshan, V.; Aslani, F. Shear bond strength and adhesive remnant index of orthodontic brackets bonded to enamel using adhesive systems mixed with TiO2 nanoparticles. Dent. Press J. Orthod. 2018, 23, 43.e41–43.e47. [Google Scholar] [CrossRef]
- Sodagar, A.; Bahador, A.; Pourhajibagher, M.; Ahmadi, B.; Baghaeian, P. Effect of addition of curcumin nanoparticles on antimicrobial property and shear bond strength of orthodontic composite to bovine enamel. J. Dent. 2016, 13, 373. [Google Scholar]
- Chung, S.H.; Cho, S.; Kim, K.; Lim, B.S.; Ahn, S.J. Antimicrobial and physical characteristics of orthodontic primers containing antimicrobial agents. Angle Orthod. 2017, 87, 307–312. [Google Scholar] [CrossRef] [PubMed]
- Felemban, N.H.; Ebrahim, M.I. The influence of adding modified zirconium oxide-titanium dioxide nano-particles on mechanical properties of orthodontic adhesive: An in vitro study. BMC Oral Health 2017, 17, 43. [Google Scholar] [CrossRef] [PubMed]
- Toodehzaeim, M.H.; Zandi, H.; Meshkani, H.; Firouzabadi, A.H. The effect of CuO nanoparticles on antimicrobial effects and shear bond strength of orthodontic adhesives. J. Dent. 2018, 19, 1–5. [Google Scholar]
- Eslamian, L.; Borzabadi-Farahani, A.; Karimi, S.; Saadat, S.; Badiee, M.R. Evaluation of the Shear Bond Strength and Antibacterial Activity of Orthodontic Adhesive Containing Silver Nanoparticle, an In-Vitro Study. Nanomaterials 2020, 10, 1466. [Google Scholar] [CrossRef] [PubMed]
- Hammad, S.M.; El-Wassefy, N.; Maher, A.; Fawakerji, S.M. Effect of nanotechnology in self-etch bonding systems on the shear bond strength of stainless steel orthodontic brackets. Dent. Press J. Orthod. 2017, 22, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Pourhajibagher, M.; Salehi Vaziri, A.; Takzaree, N.; Ghorbanzadeh, R. Physico-mechanical and antimicrobial properties of an orthodontic adhesive containing cationic curcumin doped zinc oxide nanoparticles subjected to photodynamic therapy. Photodiagnosis Photodyn. Ther. 2019, 25, 239–246. [Google Scholar] [CrossRef] [PubMed]
- Haber, D.; Khoury, E.; Ghoubril, J.; Cirulli, N. Effect of Different Surface Treatments on the Shear Bond Strength of Metal Orthodontic Brackets Bonded to CAD/CAM Provisional Crowns. Dent. J. 2023, 11, 38. [Google Scholar] [CrossRef] [PubMed]
- Paolone, G.; Mandurino, M.; Baldani, S.; Paolone, M.G.; Goracci, C.; Scolavino, S.; Gherlone, E.; Cantatore, G.; Gastaldi, G. Quantitative Volumetric Enamel Loss after Orthodontic Debracketing/Debonding and Clean-Up Procedures: A Systematic Review. Appl. Sci. 2023, 13, 5369. [Google Scholar] [CrossRef]
- Bilal, R.; Arjumand, B. Shear bond strength and bonding properties of orthodontic and nano adhesives: A comparative In-Vitro study. Contemp. Clin. Dent. 2019, 10, 600. [Google Scholar] [CrossRef]
- EL-Awady, A.A.; Al-Khalifa, H.N.; Mohamed, R.E.; Ali, M.M.; Abdallah, K.F.; Hosny, M.M.; Mohamed, A.A.S.; ElHabbak, K.S.; Hussein, F.A. Shear bond strength and antibacterial efficacy of cinnamon and titanium dioxide nanoparticles incorporated experimental orthodontic adhesive—An in vitro comparative study. Appl. Sci. 2023, 13, 6294. [Google Scholar] [CrossRef]
- Hadrous, R.; Bouserhal, J.; Osman, E. Evaluation of shear bond strength of orthodontic molar tubes bonded using hydrophilic primers: An in vitro study. Int. Orthod. 2019, 17, 461–468. [Google Scholar] [CrossRef]
- Garces, G.A.; Rojas, V.H.; Bravo, C.; Sampaio, C.S. Shear bond strength evaluation of metallic brackets bonded to a CAD/CAM PMMA material compared to traditional prosthetic temporary materials: An in vitro study. Dent. Press J. Orthod. 2020, 25, 31–38. [Google Scholar] [CrossRef]
- Kwak, J.Y.; Jung, H.K.; Choi, I.K.; Kwon, T.Y. Orthodontic bracket bonding to glazed full-contour zirconia. Restor. Dent. Endod. 2016, 41, 106–113. [Google Scholar] [CrossRef]
- Martínez-Sabio, L.; Peñate, L.; Arregui, M.; Veloso Duran, A.; Blanco, J.R.; Guinot, F. Comparison of Shear Bond Strength and Microleakage between Activa™ Bioactive Restorative™ and Bulk-Fill Composites—An In Vitro Study. Polymers 2023, 15, 2840. [Google Scholar] [CrossRef] [PubMed]
- Montasser, M.A.; Drummond, J.L. Reliability of the Adhesive Remnant Index Score System with Different Magnifications. Angle Orthod. 2009, 79, 773–776. [Google Scholar] [CrossRef]
- Cehreli, S.B.; Polat-Ozsoy, O.; Sar, C.; Cubukcu, H.E.; Cehreli, Z.C. A comparative study of qualitative and quantitative methods for the assessment of adhesive remnant after bracket debonding. Eur. J. Orthod. 2012, 34, 188–192. [Google Scholar] [CrossRef] [PubMed]
- Kaneshima, E.N.; Berger, S.B.; Fernandes, T.M.F.; Navarro, M.F.L.; Oltramari, P.V.P. Using UV light for adhesive remnant removal after debonding of orthodontic accessories. Braz. Oral. Res. 2018, 32, e47. [Google Scholar] [CrossRef]
- Khan, A.; Suryadevaraya, S.S.; Rao, B.V.; Kattimani, S.; Sha, S.K.; Bhaskar, B.V. Appraisal of orthodontic brackets for Adhesive Remnant Index with and without primer: In vitro: Study. Int. J. Clin. Prev. Dent. 2018, 5, 68–70. [Google Scholar] [CrossRef]
- Alam, M.K.; Alsuwailem, R.; Alfawzan, A.A. Antibacterial activity and bond strength of silver nanoparticles modified orthodontic bracket adhesive: A systematic review and meta-analysis of in-vitro and in-vivo studies. Int. J. Adhes. Adhes. 2022, 113, 103040. [Google Scholar] [CrossRef]
- Assery, M.K.; Ajwa, N.; Alshamrani, A.; Alanazi, B.J.; Durgesh, B.H.; Matinlinna, J.P. Titanium dioxide nanoparticles reinforced experimental resin composite for orthodontic bonding. Mater. Res. Express 2019, 6, 125098. [Google Scholar] [CrossRef]
- Farzanegan, F.; Shafaee, H.; Darroudi, M.; Rangrazi, A. Effect of the incorporation of chitosan and TiO2 nanoparticles on the shear bond strength of an orthodontic adhesive: An in vitro study. J. Adv. Oral Res. 2021, 12, 261–266. [Google Scholar] [CrossRef]
- Henkin, F.S.; Macêdo, É.O.; Santos, K.D.; Schwarzbach, M.; Samuel, S.M.; Mundstock, K.S. In vitro analysis of shear bond strength and adhesive remnant index of different metal brackets. Dent. Press J. Orthod. 2016, 21, 67–73. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).