Occlusal Plane, Mandibular Position and Dentoalveolar Changes during the Orthodontic Treatment with the Use of Mini-Screws
Abstract
:1. Introduction
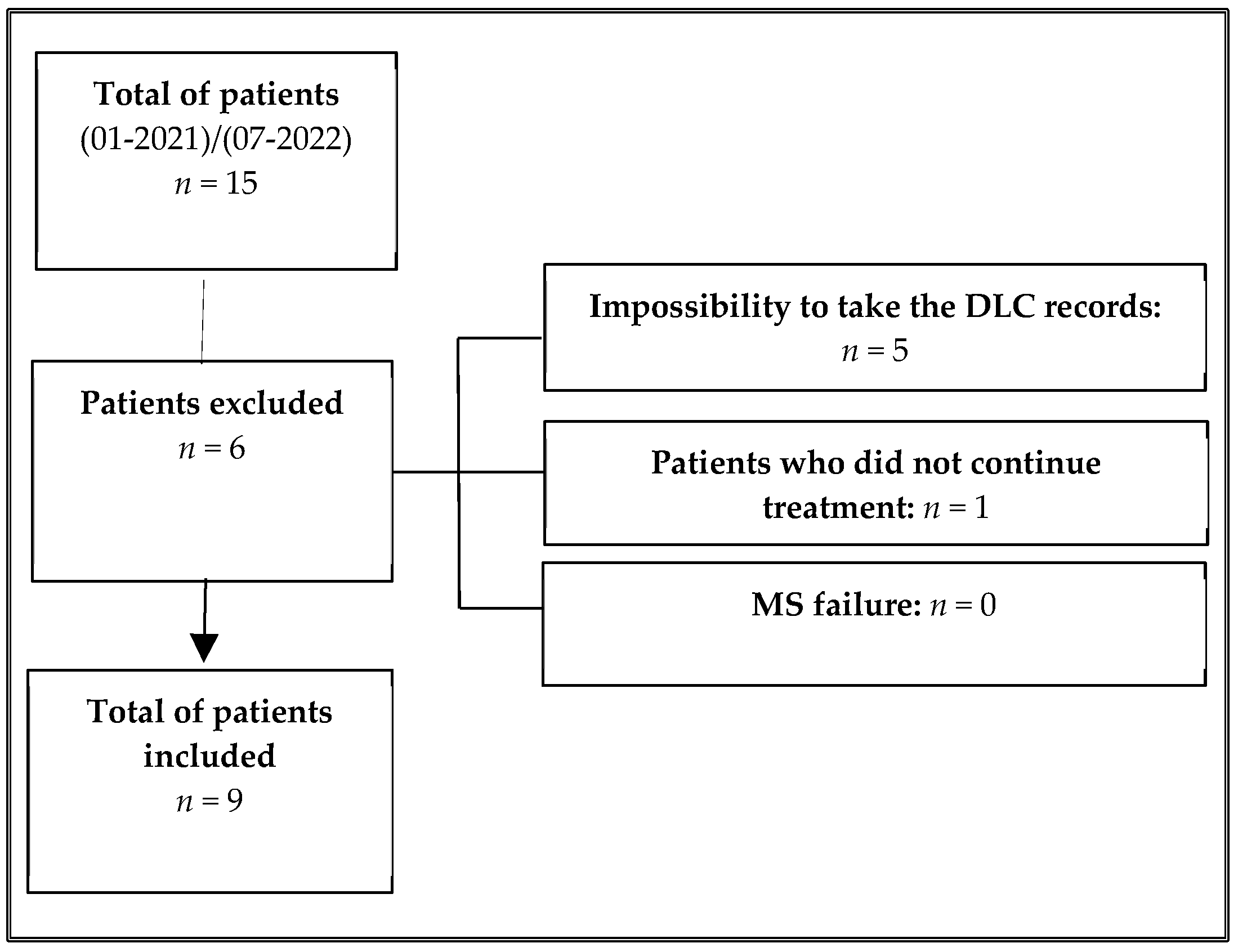
2. Materials and Methods
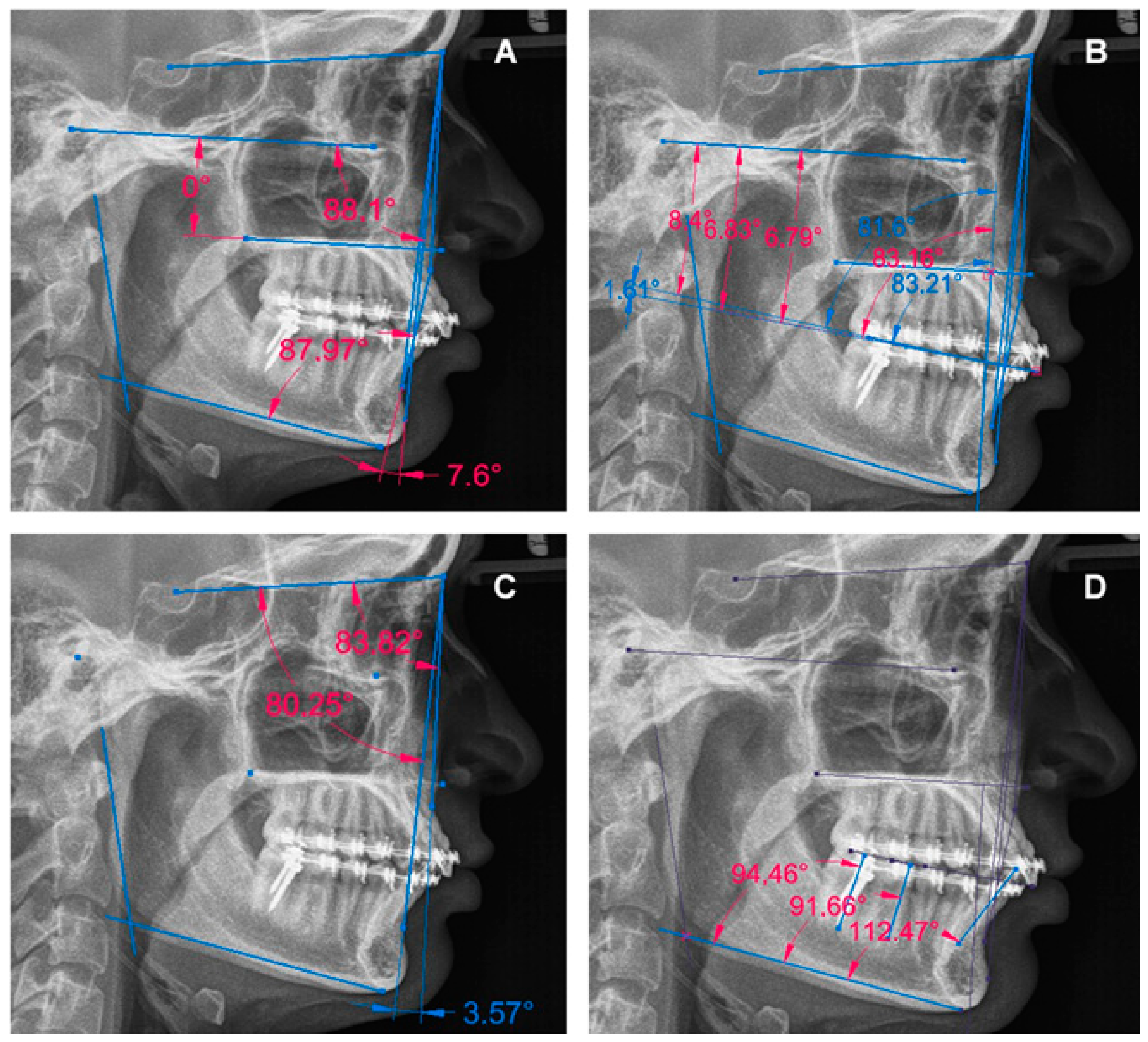
2.1. Design, Data Collection Techniques and Study Variables
2.2. Bias Control
2.3. Statistical and Other Analyses
2.4. Ethical Considerations
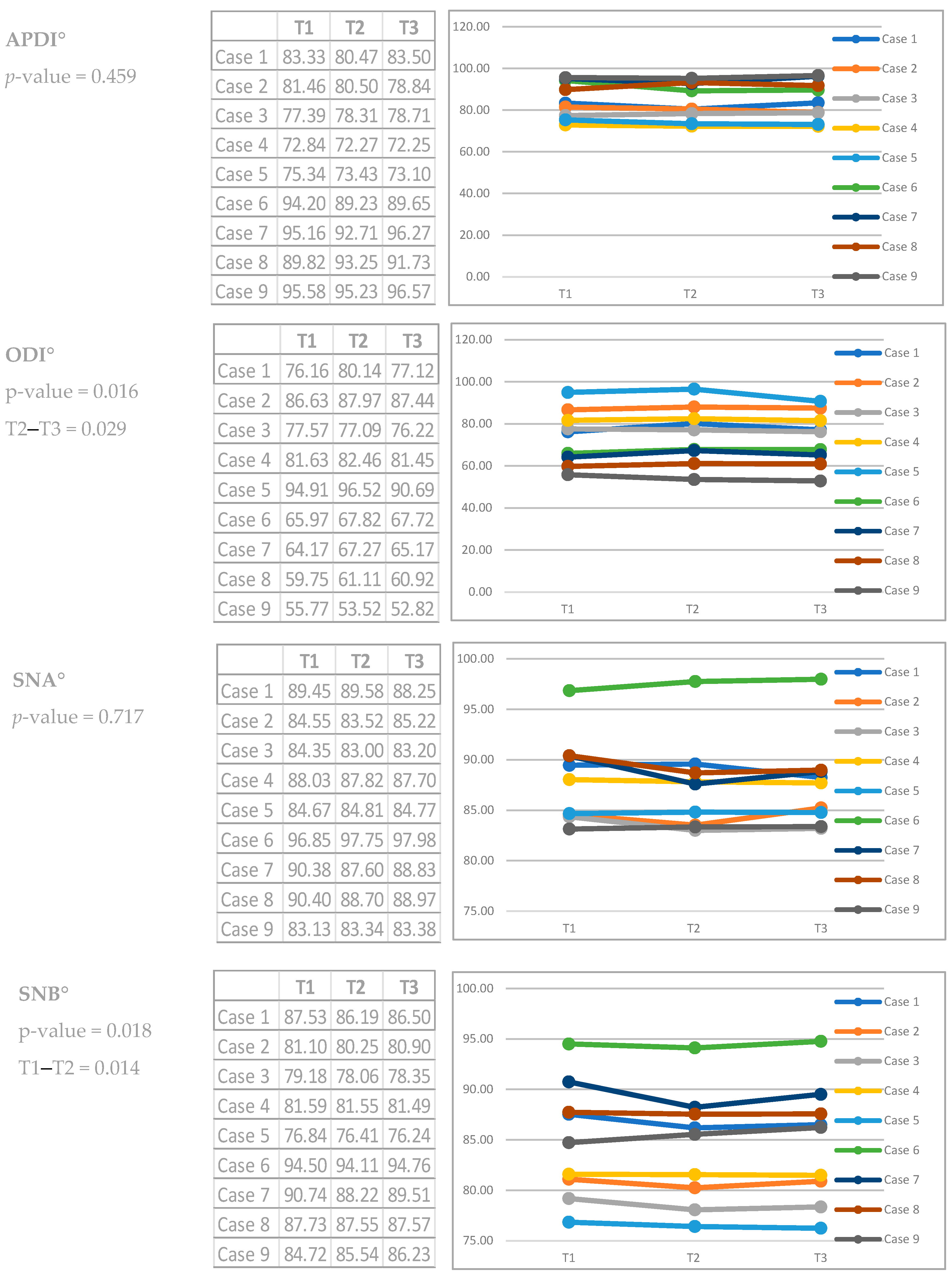
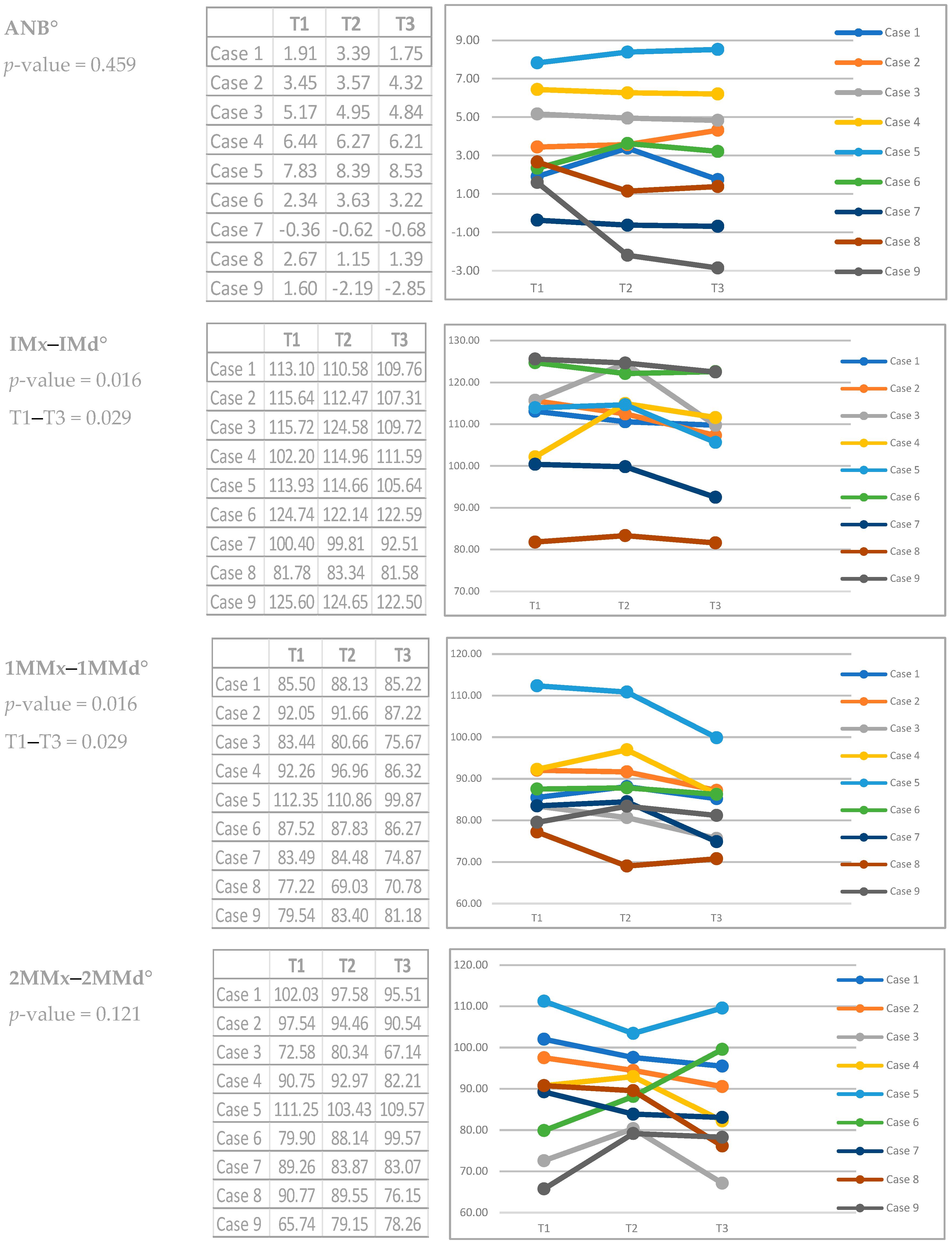
3. Results
3.1. General Characteristics of the Sample
3.2. Report of the Specific Characteristics of the Cases
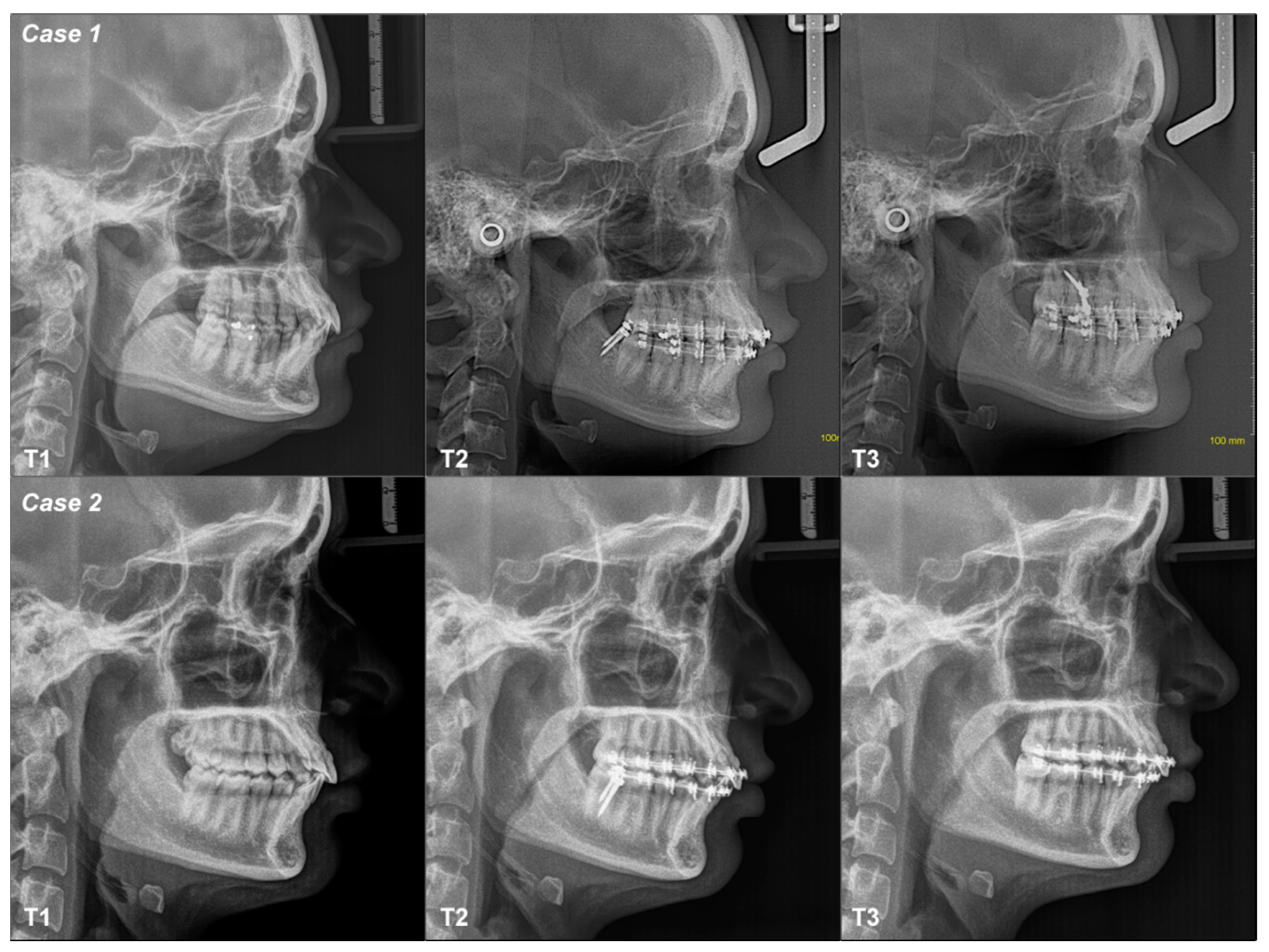
3.2.1. Case 1
3.2.2. Case 2
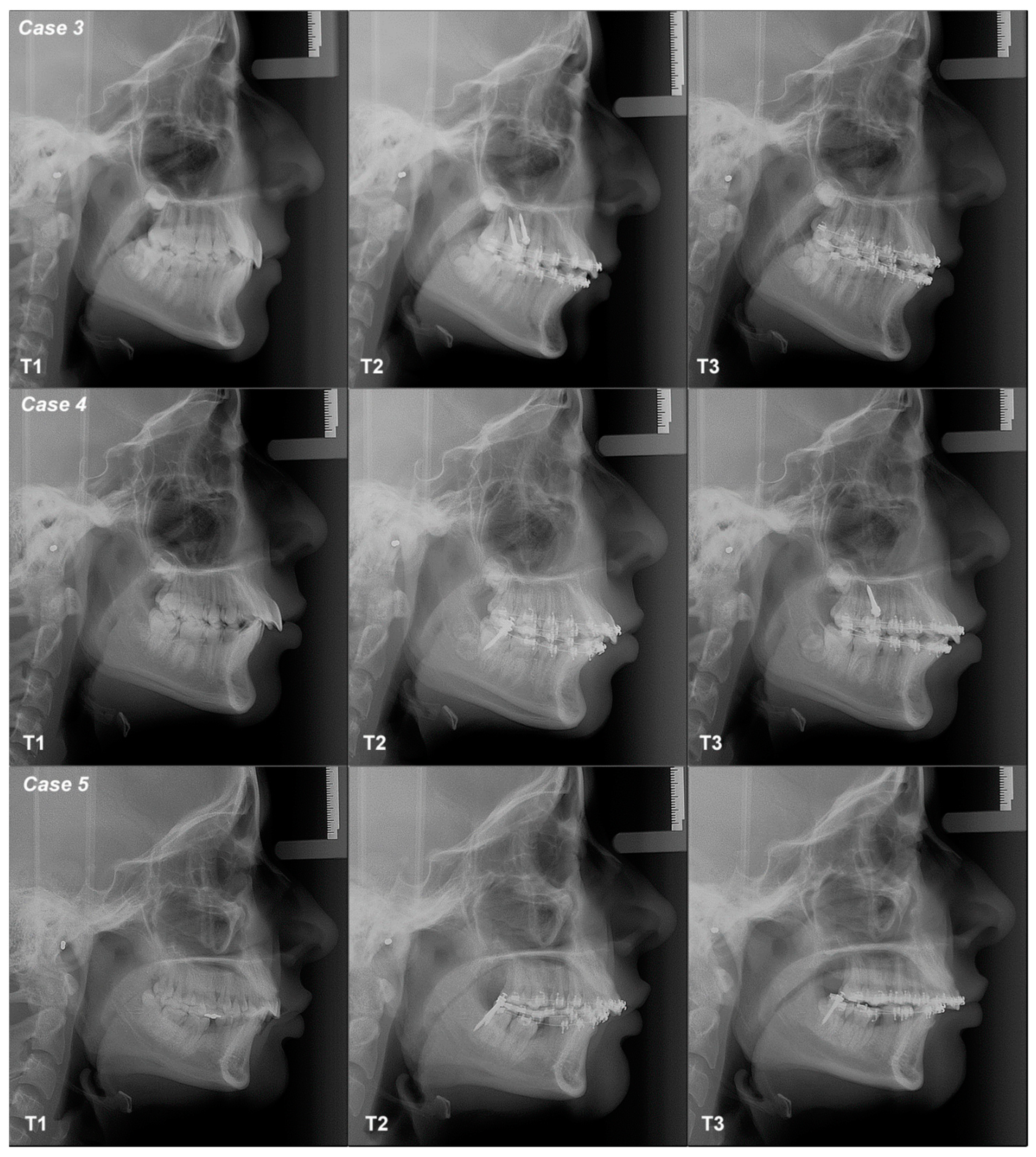
3.2.3. Case 3
3.2.4. Case 4
3.2.5. Case 5
3.2.6. Case 6
3.2.7. Case 7
3.2.8. Case 8
3.2.9. Case 9
4. Discussion
5. Conclusions
- Distalization mechanics with MS steep the COP and the AOP but flatten the POP, which can be positive for managing patients with a class II skeletal pattern;
- The anteroposterior position of the maxilla and the mandible, and the sagittal and vertical relationships, do not change with the biomechanics of distalization with MS;
- The changes in the OP were associated with dentoalveolar inclination of incisors and molars;
- New methodological approaches should be considered, such as the use of clinical trials with statistical power and the incorporation of new variables and control groups.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sato, S. A Treatment Approach to Malocclusions under the Consideration of Craniofacial Dynamics; Meaw Publishing House: Yokosuka, Japan, 2001. [Google Scholar]
- Do Ho, H.; Akimoto, S.; Sato, S. Relationship between the occlusal plane inclination and mandibular posture in the hyperdivergent type of skeletal frame. Bull. Kanagawa Dent. Coll. 2003, 31, 39–50. [Google Scholar]
- Tanaka, E.M.; Sato, S. Longitudinal alteration of the occlusal plane and development of different dentoskeletal frames during growth. Am. J. Orthod. Dentofac. Orthop. 2008, 134, 602.e1–602.e11; discussion 602–603. [Google Scholar] [CrossRef]
- Kanomi, R. Mini-implant for orthodontic anchorage. J. Clin. Orthod. 1997, 31, 763–767. [Google Scholar] [PubMed]
- Mizrahi, E.; Mizrahi, B. Mini-screw implants (temporary anchorage devices): Orthodontic and pre-prosthetic applications. J. Orthod. 2007, 34, 80–94. [Google Scholar] [CrossRef] [PubMed]
- Jones, J.P.; Elnagar, M.H.; Perez, D.E. Temporary Skeletal Anchorage Techniques. Oral Maxillofac. Surg. Clin. N. Am. 2020, 32, 27–37. [Google Scholar] [CrossRef]
- Ishikawa, H.; Nakamura, S.; Iwasaki, H.; Kitazawa, S.; Tsukada, H.; Sato, Y. Dentoalveolar compensation related to variations in sagittal jaw relationships. Angle Orthod. 1999, 69, 534–538. [Google Scholar]
- Lee, K.J.; Park, Y.C.; Hwang, C.J.; Kim, Y.J.; Choi, T.H.; Yoo, H.M.; Kyung, S.H. Displacement pattern of the maxillary arch depending on miniscrew position in sliding mechanics. Am. J. Orthod. Dentofac. Orthop. 2011, 140, 224–232. [Google Scholar] [CrossRef]
- Baccetti, T.; Franchi, L.; McNamara, J.A., Jr. The cervical vertebral maturation (CVM) method for the assessment of optimal treatment diming in dentofacial orthopedics. Semin. Orthod. 2005, 11, 119–129. [Google Scholar] [CrossRef]
- Frykholm, A.; Malmgren, O.; Sämfors, K.A.; Welander, U. Angular measurements in orthopantomography. Dentomaxillofac. Radiol. 1977, 6, 77–81. [Google Scholar] [CrossRef]
- Kim, Y.H. Overbite depth indicator with particular reference to anterior open-bite. Am. J. Orthod. 1974, 65, 586–611. [Google Scholar] [CrossRef]
- Kim, Y.H.; Vietas, J.J. Anteroposterior dysplasia indicator: An adjunct to cephalometric differential diagnosis. Am. J. Orthod. 1978, 73, 619–633. [Google Scholar] [CrossRef] [PubMed]
- Riedel, R.A. The relation of maxillary structures to cranium in malocclusion and in normal occlusion. Angle Orthod. 1952, 22, 142–145. [Google Scholar]
- Kim, H.Y. Statistical notes for clinical researchers: Evaluation of measurement error 2: Dahlberg’s error, Bland-Altman method, and Kappa coefficient. Restor. Dent. Endod. 2013, 38, 182–185. [Google Scholar] [CrossRef] [PubMed]
- Jing, Y.; Han, X.; Guo, Y.; Li, J.; Bai, D. Nonsurgical correction of a Class III malocclusion in an adult by miniscrew-assisted mandibular dentition distalization. Am. J. Orthod. Dentofac. Orthop. 2013, 143, 877–887. [Google Scholar] [CrossRef] [PubMed]
- Tai, K.; Park, J.H.; Tatamiya, M.; Kojima, Y. Distal movement of the mandibular dentition with temporary skeletal anchorage devices to correct a Class III malocclusion. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 715–725. [Google Scholar] [CrossRef] [PubMed]
- Nishimura, M.; Sannohe, M.; Nagasaka, H.; Igarashi, K.; Sugawara, J. Nonextraction treatment with temporary skeletal anchorage devices to correct a Class II Division 2 malocclusion with excessive gingival display. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 85–94. [Google Scholar] [CrossRef] [PubMed]
- Kawamura, J.; Park, J.H.; Kojima, Y.; Tamaya, N.; Kook, Y.A.; Kyung, H.M.; Chae, J.M. Biomechanical analysis for total distalization of the maxillary dentition: A finite element study. Am. J. Orthod. Dentofac. Orthop. 2021, 160, 259–265. [Google Scholar] [CrossRef] [PubMed]
- Chae, J.M.; Park, J.H.; Kojima, Y.; Tai, K.; Kook, Y.A.; Kyung, H.M. Biomechanical analysis for total distalization of the mandibular dentition: A finite element study. Am. J. Orthod. Dentofac. Orthop. 2019, 155, 388–397. [Google Scholar] [CrossRef]
- Jaramillo-Bedoya, D.; Villegas-Giraldo, G.; Agudelo-Suárez, A.A.; Ramírez-Ossa, D.M. A Scoping Review about the Characteristics and Success-Failure Rates of Temporary Anchorage Devices in Orthodontics. Dent. J. 2022, 10, 78. [Google Scholar] [CrossRef]
- Thilander, B. Basic mechanisms in craniofacial growth. Acta Odontol. Scand. 1995, 53, 144–151. [Google Scholar] [CrossRef]
- Lamarque, S. The importance of occlusal plane control during orthodontic mechanotherapy. Am. J. Orthod. Dentofac. Orthop. 1995, 107, 548–558. [Google Scholar] [CrossRef] [PubMed]
- Fushima, K.; Kitamura, Y.; Mita, H.; Sato, S.; Suzuki, Y.; Kim, Y.H. Significance of the cant of the posterior occlusal plane in class II division 1 malocclusions. Eur. J. Orthod. 1996, 18, 27–40. [Google Scholar] [CrossRef]
- Almeida, M.R. Biomechanics of extra-alveolar mini-implants. Dent. Press J. Orthod. 2019, 24, 93–109. [Google Scholar] [CrossRef] [PubMed]
- Coro, J.C.; Velasquez, R.L.; Coro, I.M.; Wheeler, T.T.; McGorray, S.P.; Sato, S. Relationship of maxillary 3-dimensional posterior occlusal plane to mandibular spatial position and morphology. Am. J. Orthod. Dentofac. Orthop. 2016, 150, 140–152. [Google Scholar] [CrossRef]
- Čelar, A.; Tafaj, E.; Graf, A.; Lettner, S. Association of anterior and posterior occlusal planes with different Angle and skeletal classes in permanent dentitions: A lateral cephalometric radiograph study. J. Orofac. Orthop. 2018, 79, 267–276. [Google Scholar] [CrossRef] [PubMed]
- Del Santo, M., Jr. Influence of occlusal plane inclination on ANB and Wits assessments of anteroposterior jaw relationships. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 641–648. [Google Scholar] [CrossRef]
- Greven, M.; Cazacu, I.; Piehslinger, E. Correlation of occlusal-plane-inclination with functional condylar displacement in different skeletal classes. Int. J. Dent. Oral Health 2020, 6, 321. [Google Scholar]



| Case | Skeletal Diagnosis | Distalization Arch | Time | COP | AOP | POP | I | 1M | 2M | SMP | VMP |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Class I Neutral Angle | Mandible | T1–T2 | Flattened | Tipped | Flattened | Decreased | Increased | Decreased | Not changed | Not changed |
| T2–T3 | Tipped | Tipped | Flattened | Decreased | Decreased | Decreased | Not changed | Not changed | |||
| T1–T3 | Flattened | Tipped | Flattened | Decreased | Decreased | Decreased | Not changed | Not changed | |||
| 2 | Class I Low Angle | Mandible | T1–T2 | Tipped | Tipped | Flattened | Decreased | Decreased | Decreased | Not changed | Not changed |
| T2–T3 | Tipped | Tipped | Flattened | Decreased | Decreased | Decreased | Not changed | Not changed | |||
| T1–T3 | Tipped | Tipped | Flattened | Decreased | Decreased | Decreased | Not changed | Not changed | |||
| 3 | Class II Neutral Angle | Maxilla | T1–T2 | Flattened | Flattened | Flattened | Increased | Decreased | Increased | Not changed | Not changed |
| T2–T3 | Tipped | Tipped | Tipped | Decreased | Decreased | Decreased | Changed | Not changed | |||
| T1–T3 | Tipped | Tipped | Flattened | Decreased | Decreased | Decreased | Changed | Not changed | |||
| 4 | Class II Low Angle | Mandible | T1–T2 | Flattened | Flattened | Flattened | Increased | Increased | Increased | Not changed | Not changed |
| T2–T3 | Tipped | Tipped | Tipped | Decreased | Decreased | Decreased | Not changed | Not changed | |||
| T1–T3 | Tipped | Flattened | Flattened | Increased | Decreased | Decreased | Not changed | Not changed | |||
| 5 | Class II Low Angle | Mandible | T1–T2 | Tipped | Tipped | Flattened | Increased | Decreased | Decreased | Not changed | Not changed |
| T2–T3 | Flattened | Flattened | Tipped | Decreased | Decreased | Increased | Not changed | Not changed | |||
| T1–T3 | Tipped | Tipped | Flattened | Decreased | Decreased | Decreased | Not changed | Not changed | |||
| 6 | Class III High Angle | Maxilla | T1–T2 | Flattened | Flattened | Flattened | Increased | Decreased | Decreased | Not changed | Not changed |
| T2–T3 | Flattened | Flattened | Tipped | Decreased | Increased | Decreased | Not changed | Not changed | |||
| T1–T3 | Flattened | Flattened | Flattened | Decreased | Decreased | Increased | Not changed | Not changed | |||
| 7 | Class III High Angle | Mandible | T1–T2 | Flattened | Flattened | Tipped | Decreased | Decreased | Decreased | Not changed | Not changed |
| T2–T3 | Tipped | Tipped | Flattened | Decreased | Increased | Decreased | Not changed | Not changed | |||
| T1–T3 | Flattened | Tipped | Flattened | Decreased | Decreased | Decreased | Not changed | Not changed | |||
| 8 | Class III High Angle | Mandible | T1–T2 | Tipped | Flattened | Flattened | Decreased | Increased | Increased | Not changed | Not changed |
| T2–T3 | Flattened | Tipped | Flattened | Increased | Decreased | Increased | Not changed | Not changed | |||
| T1–T3 | Tipped | Flattened | Flattened | Decreased | Decreased | Decreased | Not changed | Not changed | |||
| 9 | Class III High Angle | Maxilla | T1–T2 | Tipped | Tipped | Flattened | Decreased | Increased | Increased | Not changed | Not changed |
| T2–T3 | Flattened | Tipped | Flattened | Decreased | Decreased | Decreased | Not changed | Not changed | |||
| T1–T3 | Tipped | Tipped | Flattened | Decreased | Increased | Increased | Not changed | Not changed |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gómez-Bedoya, J.D.; Escobar-Serna, P.A.; Tanaka-Lozano, E.M.; Agudelo-Suárez, A.A.; Ramírez-Ossa, D.M. Occlusal Plane, Mandibular Position and Dentoalveolar Changes during the Orthodontic Treatment with the Use of Mini-Screws. Dent. J. 2024, 12, 278. https://doi.org/10.3390/dj12090278
Gómez-Bedoya JD, Escobar-Serna PA, Tanaka-Lozano EM, Agudelo-Suárez AA, Ramírez-Ossa DM. Occlusal Plane, Mandibular Position and Dentoalveolar Changes during the Orthodontic Treatment with the Use of Mini-Screws. Dentistry Journal. 2024; 12(9):278. https://doi.org/10.3390/dj12090278
Chicago/Turabian StyleGómez-Bedoya, Julián David, Pablo Arley Escobar-Serna, Eliana Midori Tanaka-Lozano, Andrés A. Agudelo-Suárez, and Diana Milena Ramírez-Ossa. 2024. "Occlusal Plane, Mandibular Position and Dentoalveolar Changes during the Orthodontic Treatment with the Use of Mini-Screws" Dentistry Journal 12, no. 9: 278. https://doi.org/10.3390/dj12090278







