Use of Orthodontic Methods in the Treatment of Dental Luxations: A Scoping Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Research Questions
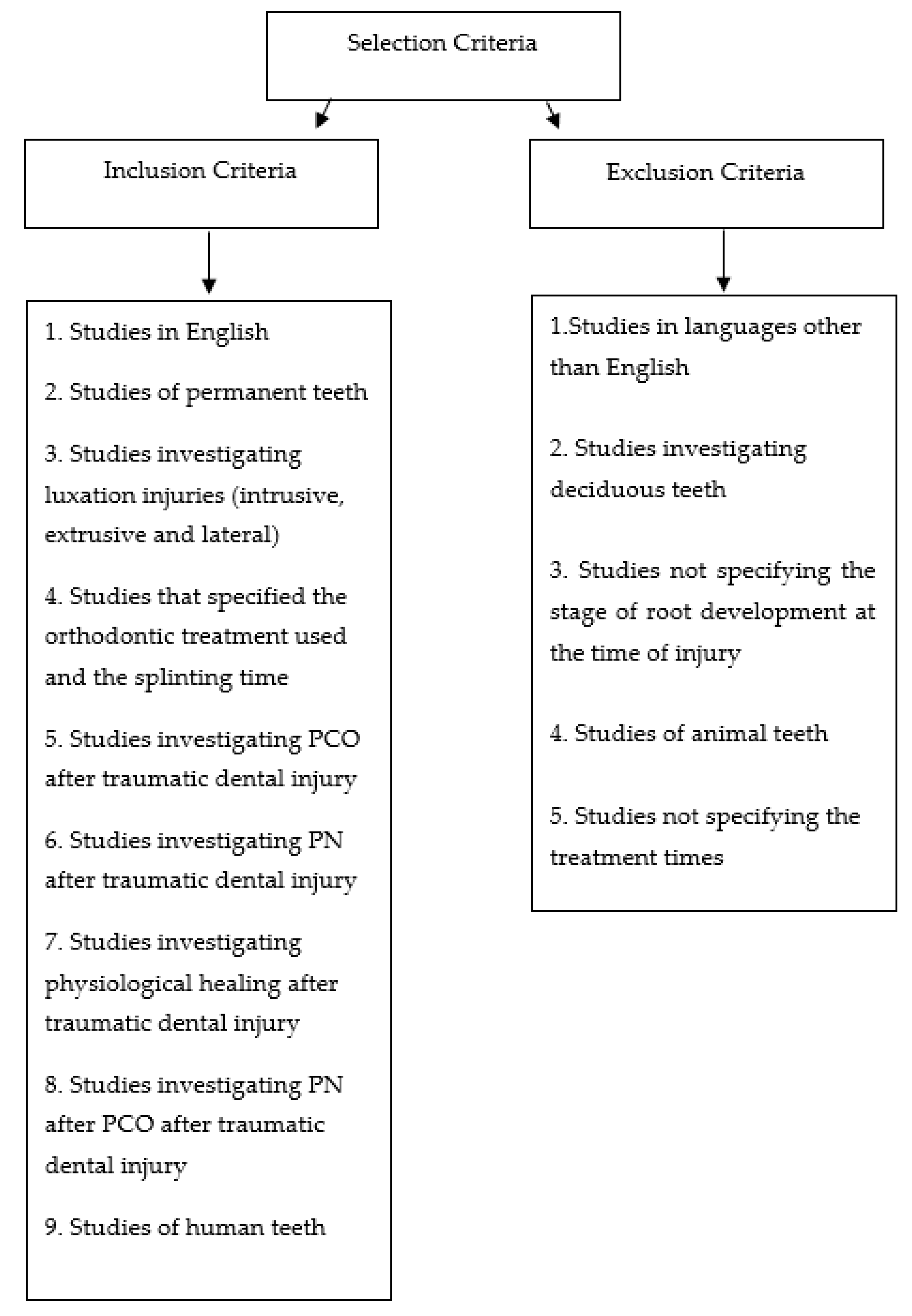
2.2. Selection Criteria
- Population. We considered studies in humans presenting permanent dentition and one or more teeth affected by intrusive, extrusive, or lateral luxation injuries.
- Intervention. We considered patients treated with orthodontic repositioning and stabilization splinting, with the use of flexible, semi-rigid, or rigid splints.
- Comparison. We compared patients presenting with intrusive, extrusive, and lateral luxation injuries.
- Outcomes. We considered the number of cases of PCO and of PN in teeth affected by intrusive, extrusive, and lateral luxations; we also considered the number of teeth that showed physiological healing (pulp survival) and the appearance of PN after PCO in the three types of trauma.
2.3. The Search Strategy
2.4. Study Quality Assessment
2.5. Data Extraction
3. Results
4. Discussion
- (1)
- The stabilization splinting technique is a fundamental part of the management of luxated teeth that have undergone dental repositioning, regardless of the dental movement method used. Orthodontic repositioning of an intruded tooth is, in fact, a treatment approach that has been widely validated in the literature and it can also be considered, in certain situations, for the treatment of extrusively and laterally luxated teeth. However, even though it does not seem to aggravate pathological pulp responses in these cases and does not necessarily have to applied immediately after the trauma, orthodontic repositioning is rarely considered in the treatment of these injuries. Further observational and retrospective studies are needed to validate this protocol.
- (2)
- Compliance with the guidelines in the early diagnostic and follow-up phases, and in relation to splinting times, was found to be poor. The lack of data on the timing of treatments and the severity of the luxation (e.g., mild, moderate, and severe), which to an extent justifies the choice of treatment, did not allow us to obtain conclusive information.
- (3)
- Pulp necrosis is the most frequent pathological pulp reaction in teeth that have sustained an intrusive or lateral luxation injury, showing a higher prevalence, of approximately 66% and 93% respectively, in CA teeth.
- (4)
- Pulp canal obliteration is a physiological response to luxation injuries, particularly dental extrusions (in which it is seen in around 42% of cases); it occurs mainly in OA teeth (approximately 83%).
- (5)
- The literature confirmed that the appearance of PN in a tooth showing PCO is a rare occurrence. Furthermore, since physiological healing (pulp survival) is always one of the possible outcomes, it should be more extensively investigated by clinicians. The present review showed that this outcome was not reported by all authors, and even when it was reported, the information provided was unclear.
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Soriano, E.P.; Caldas, A.F., Jr.; Carvalho, M.V.D.; Amorim Filho, H.A. Prevalence and risk factors related to traumatic dental injuries. Dent. Traumatol. 2007, 23, 232–240. [Google Scholar] [CrossRef]
- Traebert, J.; Bittencourt, D.D.; Peres, K.G.; Peres, M.A.; De Lacerda, J.T.; Marcenes, W. Aetiology and rates of treatment of traumatic dental injuries among 12-year-old school children in a town in southern Brazil. Dent. Traumatol. 2006, 22, 173–178. [Google Scholar] [CrossRef]
- Bauss, O.; Röhling, J.; Schwestka-Polly, R. Prevalence of traumatic injuries to the permanent incisors in candidates for orthodontic treatment. Dent. Traumatol. 2004, 20, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Schatz, J.-P.; Hakeberg, M.; Ostini, E.; Kiliaridis, S. Prevalence of traumatic injuries to permanent dentition and its association with overjet in a Swiss child population. Dent. Traumatol. 2012, 29, 110–114. [Google Scholar] [CrossRef] [PubMed]
- Glendor, U.; Halling, A.; Andersson, L.; Eilert-Petersson, E. Incidence of traumatic tooth injuries in children and adolescents in the county of Västmanland, Sweden. Swed. Dent. J. 1996, 20, 15–28. [Google Scholar] [PubMed]
- McClanahan, S.B.; Crepps, J.T., III; Maranga, M.C.; Worrel, E.D.; Behnia, A. American Association of Endodontists. Glossary of Endodontic Terms; American Association of Endodontists: Chicago, IL, USA, 2020; p. 31. [Google Scholar]
- Bourguignon, C.; Cohenca, N.; Lauridsen, E.; Flores, M.T.; O’Connell, A.C.; Day, P.F.; Tsilingaridis, G.; Abbott, P.V.; Fouad, A.; Hicks, L.; et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 1. Fractures and luxations. Dent. Traumatol. 2020, 36, 314–330. [Google Scholar] [CrossRef]
- Andreasen, J.O.; Andreasen, F.M.; Bakland, L.K.; Flores, M.T. Traumatic Dental Injuries—A Manual, 1st ed.; Munksgaard: Copenhagen, Denmark, 1999. [Google Scholar]
- Andreasen, J.; Andreasen, F.; Skeie, A.; Hjørting-Hansen, E.; Schwartz, O. Effect of treatment delay upon pulp and periodontal healing of traumatic dental injuries—A review article. Dent. Traumatol. 2002, 18, 116–128. [Google Scholar] [CrossRef]
- Andreasen, F.M.; Zhijie, Y.; Thomsen, B.L.; Andersen, P.K. Occurrence of pulp canal obliteration after luxation injuries in the permanent dentition. Endod. Dent. Traumatol. 1987, 3, 103–115. [Google Scholar] [CrossRef]
- Andreasen, J.O. Luxation of permanent teeth due to trauma A clinical and radiographic follow-up study of 189 injured teeth. Eur. J. Oral Sci. 1970, 78, 273–286. [Google Scholar] [CrossRef]
- Hermann, N.V.; Lauridsen, E.; Ahrensburg, S.S.; Gerds, T.A.; Andreasen, J.O. Periodontal healing complications following extrusive and lateral luxation in the permanent dentition: A longitudinal cohort study. Dent. Traumatol. 2012, 28, 394–402. [Google Scholar] [CrossRef] [PubMed]
- Lauridsen, E.; Hermann, N.V.; Gerds, T.A.; Ahrensburg, S.S.; Kreiborg, S.; Andreasen, J.O. Combination injuries 3. The risk of pulp necrosis in permanent teeth with extrusion or lateral luxation and concomitant crown fractures without pulp exposure. Dent. Traumatol. 2012, 28, 379–385. [Google Scholar] [CrossRef]
- Grossman, L.I. Intentional replantation of teeth. J. Am. Dent. Assoc. 1966, 72, 1111–1118. [Google Scholar] [CrossRef]
- Weine, F.S. The Case Against Intentional Replantation. J. Am. Dent. Assoc. 1980, 100, 664–668. [Google Scholar] [CrossRef]
- Spinas, E.; Generali, L.; Mameli, A.; Demontis, C.; Martinelli, D.; Giannetti, L. Delayed tooth replantation and inflammatory root resorption in childhood and adolescence. J. Biol. Regul. Homeost. Agents 2019, 33, 623–627. [Google Scholar]
- Okamoto, R.; De Faria, L.P.; Amaral, M.F.; De Almeida, M.M.; Brandini, D.A.; Poi, W.R. Treatment of Extrusive Luxation in Permanent Teeth: Literature Review with Systematic Criteria. J. Contemp. Dent. Pract. 2017, 18, 241–245. [Google Scholar] [CrossRef] [Green Version]
- Jafarzadeh, H.; Rouhani, A.; Javidi, B.; Habibi, M. Intentional Replantation: A Procedure as a Last Resort. J. Contemp. Dent. Pr. 2011, 12, 486–492. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Kratchman, S.; Kim, S. Intentional Replantation; Wiley: Hoboken, NJ, USA, 2017; Volume 41, pp. 179–191. [Google Scholar]
- Lu, D.P. Intentional replantation of periodontally involved and endodontically mistreated tooth. Oral Surg. Oral Med. Oral Pathol. 1986, 61, 508–513. [Google Scholar] [CrossRef]
- Andreasen, J.O.; Hjorting-Hansen, E. Replantation of teeth. I. Radiographic and clinical study of 110 human teeth replanted after accidental loss. Acta Odontol. Scand. 1966, 24, 263–286. [Google Scholar] [CrossRef]
- Spinas, E.; Aresu, M.; Canargiu, F.; Giannetti, L. Preventive treatment of post-traumatic dental infraocclusion: Study on the knowledge of dental decoronation in a sample of Italian dental students and dentists. Eur. J. Paediatr. Dent. 2015, 16, 279–283. [Google Scholar] [PubMed]
- Dryden, J.A.; Arens, D.E. Intentional replantation. A viable alternative for selected cases. Dent. Clin. N. Am. 1994, 38, 325–353. [Google Scholar]
- Messkoub, M. Intentional replantation: A successful alternative for hopeless teeth. Oral Surg. Oral Med. Oral Pathol. 1991, 71, 743–747. [Google Scholar] [CrossRef]
- Spinas, E. A biological conservative approach to complex traumatic dento-alveolar lesions. J. Clin. Pediatr. Dent. 2004, 28, 1–10. [Google Scholar] [CrossRef]
- Spinas, E.; Pipi, L.; Dettori, C. Extrusive Luxation Injuries in Young Patients: A Retrospective Study with 5-Year Follow-Up. Dent. J. 2020, 8, 136. [Google Scholar] [CrossRef] [PubMed]
- Elbay, Ü.Ş.; Baysal, A.; Elbay, M.; Saridag, S.; Sarıdağ, S. Multidisciplinary Approach to Delayed Treatment of Traumatic Teeth Injuries Involving Extrusive Luxation, Avulsion and Crown Fracture. Oper. Dent. 2014, 39, 566–571. [Google Scholar] [CrossRef]
- Ebrahim, F.-H.; Kulkarni, G. Fixed orthodontic appliances in the management of severe dental trauma in mixed dentition: A case report. J. Can. Dent. Assoc. 2013, 79, d131. [Google Scholar]
- Sübay, R.K.; Kayatas, M.; Caniklioğlu, C. Delayed multidisciplinary management of an extrusively luxated maxillary central incisor. Dent. Traumatol. 2007, 23, 82–84. [Google Scholar] [CrossRef]
- Nikoui, M.; Kenny, D.J.; Barrett, E.J. Clinical outcomes for permanent incisor luxations in a pediatric population. III. Lateral luxations. Dent. Traumatol. 2003, 19, 208–285. [Google Scholar]
- Ferrazzini Pozzi, E.C.; von Arx, T. Pulp and periodontal healing of laterally luxated permanent teeth: Results after 4 years. Dent. Traumatol. 2008, 24, 658–662. [Google Scholar] [CrossRef] [PubMed]
- Kahler, B.; Heithersay, G.S. An evidence-based appraisal of splinting luxated, avulsed and root-fractured teeth. Dent. Traumatol. 2008, 24, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Andreasen, J.O.; Andreasen, F.M.; Mejare, I.; Cvek, M. Healing of 400 intra-alveolar root fractures 2. Effect of treatment factors such as treatment delay, repositioning, splinting type and period and antibiotics. Dent. Traumatol. 2004, 20, 203–211. [Google Scholar] [CrossRef]
- Cengiz, S.B.; Atac, A.S.; Cehreli, Z.C. Biomechanical effects of splint types on traumatized tooth: A photoelastic stress analysis. Dent. Traumatol. 2006, 22, 133–138. [Google Scholar] [CrossRef]
- Andreasen, F.M.; Pedersen, B.V. Prognosis of luxated permanent teeth—The development of pulp necrosis. Dent. Traumatol. 1985, 1, 207–220. [Google Scholar] [CrossRef]
- Andreasen, J.O. Etiology and pathogenesis of traumatic dental injuries A clinical study of 1,298 cases. Eur. J. Oral Sci. 1970, 78, 329–342. [Google Scholar] [CrossRef] [PubMed]
- Fields, H.W.; Christensen, J.R. Orthodontic Procedures after Trauma. J. Endod. 2013, 39, S78–S87. [Google Scholar] [CrossRef]
- Arskey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. 2005, 8, 19–32. [Google Scholar]
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018, 18, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [Green Version]
- Cumpston, M.; Li, T.; Page, M.J.; Chandler, J.; Welch, V.A.; Higgins, J.P.; Thomas, J. Updated guidance for trusted systematic reviews: A new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst. Rev. 2019, 10, ED000142. [Google Scholar] [CrossRef] [Green Version]
- Landis, J.R.; Koch, G.G. An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers. Biometrics 1977, 33, 363–374. [Google Scholar] [CrossRef]
- Higgins, P.T.J.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for systematic Reviews of Interventions, 2nd ed.; The Cochrane Collaboration and John Wiley and Sons Ltd.: Chichester, UK, 2019. [Google Scholar]
- Alaçam, A.; Üçüncü, N. Combined apexification and orthodontic intrusion of a traumatically extruded immature permanent incisor. Dent. Traumatol. 2002, 18, 37–41. [Google Scholar] [CrossRef] [PubMed]
- Spinas, E.; Giannetti, L.; Mameli, A.; Re, D. Dental injuries in young athletes, a five-year follow-up study. Eur. J. Paediatr. Dent. 2018, 19, 187–193. [Google Scholar]
- Ebeleseder, K.A.; Glockner, K.; Pertl, C.; Stadtler, P. Splints made of wire and composite: An investigation of lateral tooth mobility in vivo. Dent. Traumatol. 1995, 11, 288–293. [Google Scholar] [CrossRef]
- von Arx, T. Splinting of traumatized teeth with focus on adhesive techniques. J. Calif. Dent. Assoc. 2005, 33, 409–414. [Google Scholar]
- Andreasen, F.M.; Andreasen, J.O. Diagnosis of luxation injuries: The importance of standardized clinical, radiographic and photographic techniques in clinical investigations. Dent. Traumatol. 1985, 1, 160–169. [Google Scholar] [CrossRef]
- Andreasen, F.M.; Kahler, B. Diagnosis of acute dental trauma: The importance of standardized documentation: A review. Dent. Traumatol. 2015, 31, 340–349. [Google Scholar] [CrossRef]
- Spinas, E.; Mameli, A.; Giannetti, L. Traumatic Dental Injuries Resulting from Sports Activities; Immediate Treatment and Five Years Follow-Up: An Observational Study. Open Dent. J. 2018, 12, 1–10. [Google Scholar] [CrossRef]
- Wigen, T.I.; Agnalt, R.; Jacobsen, I. Intrusive luxation of permanent incisors in Norwegians aged 6-17 years: A retrospective study of treatment and outcome. Dent. Traumatol. 2008, 24, 612–618. [Google Scholar] [CrossRef] [PubMed]
- Tsilingaridis, G.; Malmgren, B.; Andreasen, J.O.; Malmgren, O. Intrusive luxation of 60 permanent incisors: A retrospective study of treatment and outcome. Dent. Traumatol. 2012, 28, 416–422. [Google Scholar] [CrossRef]
- Lee, R.; Barrett, E.J.; Kenny, D.J. Clinical outcomes for permanent incisor luxations in a pediatric population. II. Extrusions. Dent. Traumatol. 2003, 19, 274–279. [Google Scholar] [CrossRef]
- Ramírez, A.V.; Strenger, S.K.; López, M.S.; Cortes, P.M.; Núñez, C.C. A 4-year follow-up case of extrusive luxation in a patient with cerebral palsy. Spéc. Care Dent. 2019, 39, 225–230. [Google Scholar] [CrossRef]
- Cehreli, Z.C.; Sara, S.; Aksoy, B. Revascularization of immature permanent incisors after severe extrusive luxation injury. J. Can. Dent. Assoc. 2012, 78, 4. [Google Scholar]
- Hecová, H.; Tzigkounakis, V.; Merglova, V.; Netolický, J. A retrospective study of 889 injured permanent teeth. Dent. Traumatol. 2010, 26, 466–475. [Google Scholar] [CrossRef]
- Oikarinen, K.; Gundlach, K.K.H.; Pfeifer, G. Late complications of luxation injuries to teeth. Dent. Traumatol. 1987, 3, 296–303. [Google Scholar] [CrossRef]
- Spinas, E.; Deias, M.; Mameli, A.; Giannetti, L. Pulp canal obliteration after extrusive and lateral luxation in young permanent teeth: A scoping review. Eur. J. Paediatr. Dent. 2021, 22. in press. [Google Scholar]
- McCabe, P.S.; Dummer, P.M.H. Pulp canal obliteration: An endodontic diagnosis and treatment challenge. Int. Endod. J. 2012, 45, 177–197. [Google Scholar] [CrossRef] [PubMed]
- Bauss, O.; Röhling, J.; Rahman, A.; Kiliaridis, S. The Effect of Pulp Obliteration on Pulpal Vitality of Orthodontically Intruded Traumatized Teeth. J. Endod. 2008, 34, 417–420. [Google Scholar] [CrossRef]
- Kvinnsland, S.; Heyeraas, K.; Ofjord, E.S. Effect of experimental tooth movement on periodontal and pulpal blood flow. Eur. J. Orthod. 1989, 11, 200–205. [Google Scholar] [CrossRef]
- Derringer, K.A.; Jaggers, D.C.; Linden, R.W.A. Angiogenesis in human dental pulp following orthodontic tooth movement. J. Dent. Res. 1996, 75, 1761–1766. [Google Scholar] [CrossRef]
- Vandevska-Radunovic, V.; Kristiansen, A.B.; Heyeraas, K.J.; Kvinnsland, S. Changes in blood circulation in teeth and supporting tissues incident to experimental tooth movement. Eur. J. Orthod. 1994, 16, 361–369. [Google Scholar] [CrossRef]
- Yu, C.Y.; Abbott, P.V. Responses of the pulp, periradicular and soft tissues following trauma to the permanent teeth. Aust. Dent. J. 2016, 61, 39–58. [Google Scholar] [CrossRef] [PubMed]
- Feiglin, B. Dental pulp response to traumatic injuries—A retrospective analysis with case reports. Dent. Traumatol. 1996, 12, 1–8. [Google Scholar] [CrossRef]


| Author and Year | N° of Samples | N° of Intr. Lux. | N° of Extr. Lux. | N° of Lat. Lux | Mm of lux | PCO in IL | PCO in EL | PCO in LL | PN in IL | PN in EL | PN in LL | PS | PN after PCO | First Clinical Examination | Follow-Up |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Lee, 2003 | 55 | / | 55 (24 OA 31 CA) | / | <2 mm >2 mm n° NS | / | 19 (16 OA 3 CA) | / | / | 23 (11 OA 12 CA) | / | NS | 2 | Clinical examination, X-ray (Periapical+ Occlusal) | 2 wk-3 mo-6 mo-early |
| Nikoui, 2003 | 58 | / | / | 58 (35 OA 23 CA) | <2 mm >2 mm n° NS | / | / | 23 (6 OA 17 CA) | / | / | 23 (3 OA 20 CA) | NS | 0 | Clinical examination, X-ray (Periapical+ Occlusal) | 2 wk-3 mo-6 mo-early |
| Wigen, 2008 | 51 | 51 (31 OA 20 CA) | / | / | <2 mm (8) >2 mm (22) | 18 (13 OA 5 CA) | / | / | 29 (14 OA 15 CA) | / | / | 4 | NS | Clinical examination, X-ray (Periapical) | 1–12 yr |
| Tsilingaridis, 2011 | 60 | 60 (27 OA 33 CA) | / | / | 1–3 mm (16) 4–6 mm (22) >7 mm (22) | 17 (16 OA 1 CA) | / | / | 23 (4 OA 19 CA) | / | / | 17 | NS | Clinical examination, X-ray (Periapical) | 6–130 mo |
| Cehreli, 2012 | 2 | / | 2 (2 OA) | / | NS | / | / | / | / | 2 (2 OA) | / | 0 | 0 | Clinical examination, X-ray (Periapical) | 1–2-3 wk- 3 mo-12 mo-18 mo |
| Ferrazzini Pozzi, 2008 | 47 | / | / | 47 (10 OA 37 CA) | NS | / | / | 9 (2 OA 7 CA) | / | / | 19 (0 OA 19 CA) | 19 | NS | Clinical examination, DPT, X-ray | 2 wk- 4 wk- 6/8 wk-6 mo-directly at 4 yr |
| Ramirez, 2018 | 2 | / | 2 (2 OA) | / | NS | / | 2 (2 OA) | / | / | 0 | / | 0 | 0 | Clinical examination, X-ray (periapical), photo | 2 wk-3-4-5 mo-1–3-4 yr |
| Spinas, 2020 | 13 | / | 13 (8 OA 5 CA) | / | 0–2 mm (4) 3–5 mm (7) >6 mm (2) | / | 9 (7 OA 2 CA) | / | / | 3 (1 OA 2 CA) | / | 1 | 0 | Clinical examination, DPT, X-ray (Periapical+ Occlusal), photo | 2 wk- 4 wk- 6/8 wk-6 mo-yearly for 5 yr |
| Author and Year | N° of Samples | Age (Years) | N° of Intr. Lux. | N° of Extr. Lux. | N° of Lat. Lux | Manual Repositioning | Surgical Repositioning | Orthodontic Repositioning | Time of Splinting | Type of Splinting |
|---|---|---|---|---|---|---|---|---|---|---|
| Lee, 2003 | 55 | 7.1–17.8 | / | 55 (24 OA 31 CA) | / | 55 | 0 | 0 | 7–14 days | SS 0.016 wire composite |
| Nikoui, 2003 | 58 | 6.3–17.8 | / | / | 58 (35 OA 23 CA) | 58 | 0 | 0 | 14–21 days | SS 0.014/0.016 wire composite |
| Wigen, 2008 | 51 | 6–17 | 51 (31 OA 20 CA) | / | / | 37 | 7 | 7 | 2–6 wk | Wire composite |
| Tsilingaridis, 2011 | 60 | 6–16 | 60 (27 OA 33 CA) | / | / | 17 | 12 | 31 | 6–80 days (mean 28.9) | Kevlar + wire |
| Cehreli, 2012 | 2 | 8.5 | / | 2 (2 OA) | / | 2 | 0 | 0 | 3 wk | Fishing line + composite |
| Ferrazzini Pozzi, 2008 | 47 | 7–59 | / | / | 47 (10 OA 37 CA) | 47 | 0 | 0 | 7–28 days (mean 22) | TTS composite |
| Ramirez, 2018 | 2 | 9 | / | 2 (2 OA) | / | 2 | 0 | 0 | 3 mo | SS wire composite 0.4 mm |
| Spinas, 2020 | 13 | 8–16 | / | 13 (8 OA 5 CA) | / | 3 | 9 | 0 | 14–21 days | Bracket–NiTi wire |
| Author, Years | Title | Type of Study |
|---|---|---|
| Lee, 2003 | Clinical outcomes for permanent incisor luxations in a pediatric population. II. Extrusion | Longitudinal study |
| Nikoui, 2003 | Clinical outcomes for permanent incisor luxations in a pediatric population. III. Lateral Luxations | Longitudinal study |
| Wigen, 2008 | Intrusive luxation of permanent incisors in Norwegians aged 6–17 years: a retrospective study of treatment and outcome | Retrospective study |
| Ferrazzini Pozzi, 2008 | Pulp and periodontal healing of laterally luxated permanent teeth: results after 4 years | Retrospective study |
| Tsilingaridis, 2011 | Intrusive luxation of 60 permanent incisors: a retrospective study of treatment and outcome | Retrospective study |
| Cehreli, 2012 | Revascularization of Immature Permanent Incisors after Severe Extrusive Luxation Injury | Case report |
| Ramirez, 2018 | A 4-year follow-up case of extrusive luxation in a patient with cerebral palsy | Case report |
| Spinas, 2020 | Extrusive luxations in young patients: Retrospective study with 5-year follow-up | Retrospective study |
| Intrusive Luxation | ||||
| Total | PCO | PN | PS | PN after PCO |
| 111 58 OA–53 CA | 35 29 OA–6 CA | 52 18 OA–34 CA | 19 | - |
| Extrusive Luxation | ||||
| Total | PCO | PN | PS | PN after PCO |
| 72 36 OA–36 CA | 30 25 OA–5 CA | 28 14 OA–14 CA | 1 | 2 |
| Lateral Luxation | ||||
| Total | PCO | PN | PS | PN after PCO |
| 105 45 OA–60 CA | 32 8 OA–24 CA | 42 3 OA–39 CA | 19 | 0 |
| Intrusive Luxation | ||||
| Total | Manual repositioning | Orthodontic repositioning | Surgical repositioning | |
| 111 58 OA–53 CA | 54 | 19 | 38 | |
| Extrusive Luxation | ||||
| Total | Manual repositioning | Orthodontic repositioning | Surgical repositioning | |
| 72 36 OA–36 CA | 62 | 12 | 0 | |
| Lateral Luxation | ||||
| Total | Manual repositioning | Orthodontic repositioning | Surgical repositioning | |
| 105 45 OA–60 CA | 105 | 0 | 0 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Spinas, E.; Pipi, L.; Mezzena, S.; Giannetti, L. Use of Orthodontic Methods in the Treatment of Dental Luxations: A Scoping Review. Dent. J. 2021, 9, 18. https://doi.org/10.3390/dj9020018
Spinas E, Pipi L, Mezzena S, Giannetti L. Use of Orthodontic Methods in the Treatment of Dental Luxations: A Scoping Review. Dentistry Journal. 2021; 9(2):18. https://doi.org/10.3390/dj9020018
Chicago/Turabian StyleSpinas, Enrico, Laura Pipi, Silvia Mezzena, and Luca Giannetti. 2021. "Use of Orthodontic Methods in the Treatment of Dental Luxations: A Scoping Review" Dentistry Journal 9, no. 2: 18. https://doi.org/10.3390/dj9020018
APA StyleSpinas, E., Pipi, L., Mezzena, S., & Giannetti, L. (2021). Use of Orthodontic Methods in the Treatment of Dental Luxations: A Scoping Review. Dentistry Journal, 9(2), 18. https://doi.org/10.3390/dj9020018







