Investigating the Dietary Impact on Trans-Vaccenic Acid (Trans-C18:1 n-7) and Other Beneficial Fatty Acids in Breast Milk and Infant Formulas
Abstract
:1. Introduction
2. Materials and Methods
2.1. Samples
- Cohort 1: Women consuming conventional dairy products.
- Cohort 2: Women consuming improved dairy products.
- Infant formula.
2.2. Fatty Acid Determination
2.3. Statistics
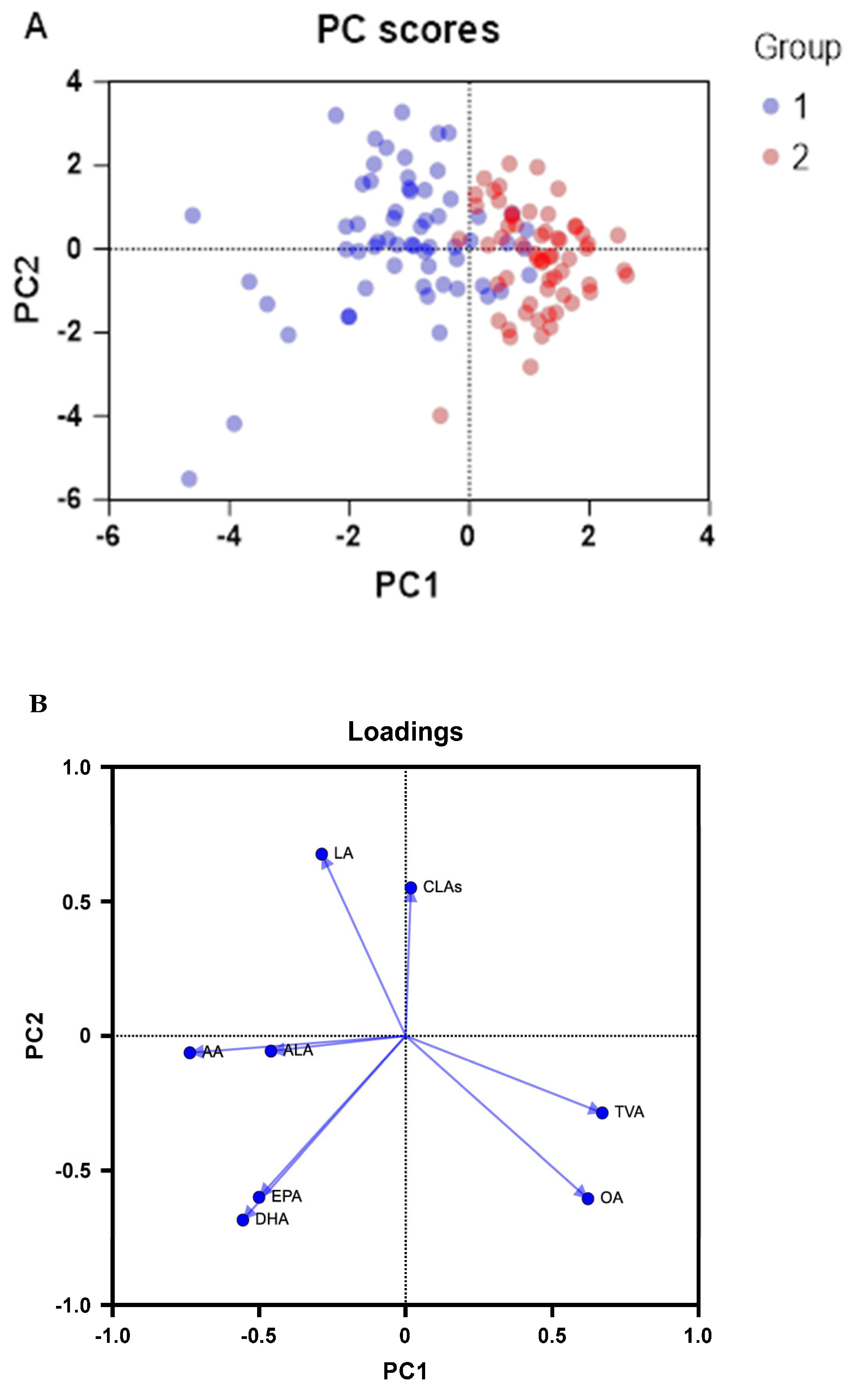
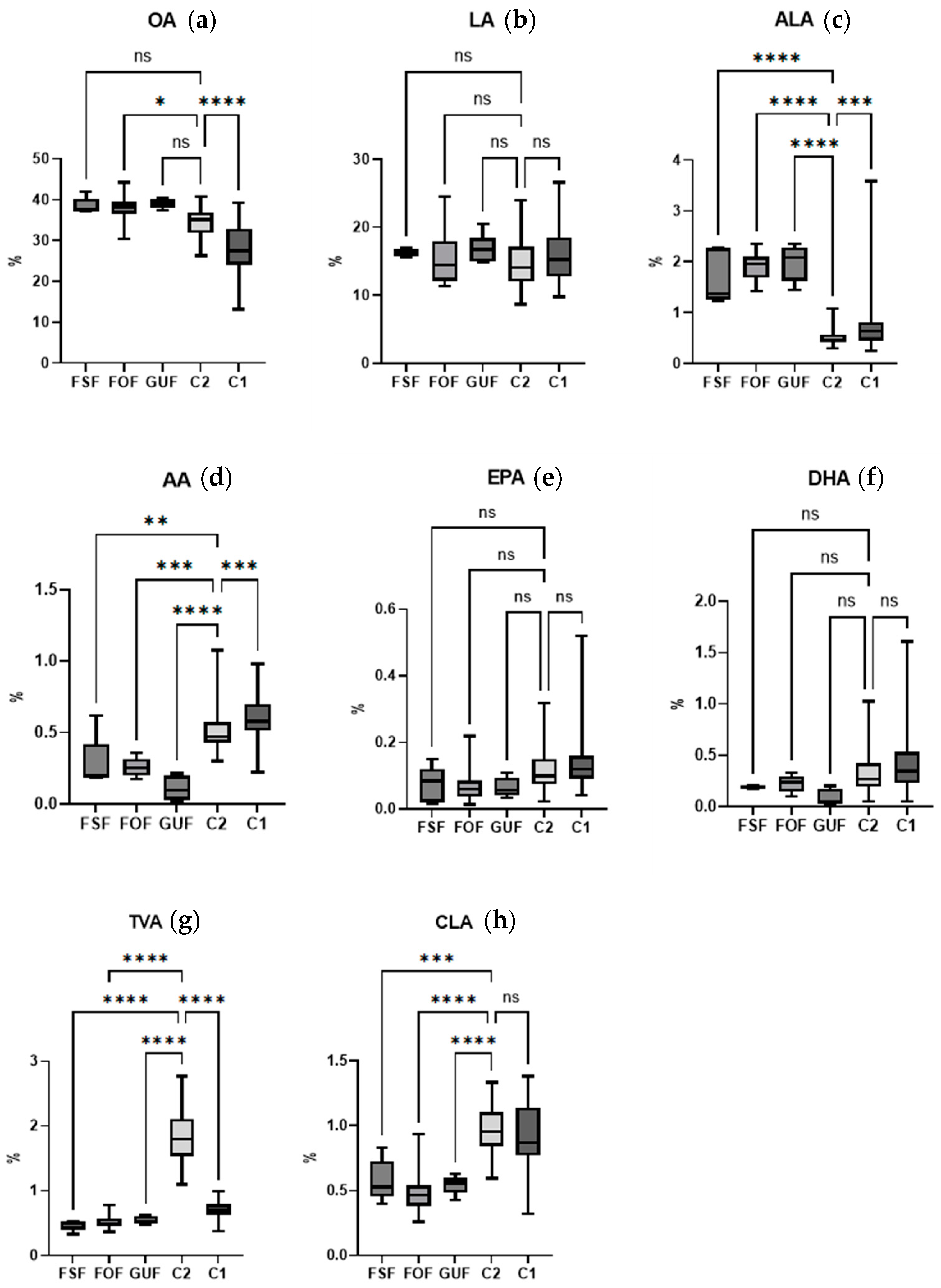
3. Results and Discussion
3.1. Samples Data
3.1.1. TFA, Diet, and Lactation Characteristics
- Cohort 1
- Cohort 2
3.1.2. TFA across Samples
- Cohort 1
- Cohort 1 versus cohort 2
- Breast milk vs. infant formula
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hennet, T.; Borsig, L. Breastfed at Tiffany’s. Trends Biochem. Sci. 2016, 41, 508–518. [Google Scholar] [CrossRef] [PubMed]
- Grote, V.; Verduci, E.; Scaglioni, S.; Vecchi, F.; Contarini, G.; Giovannini, M.; Koletzko, B.; Agostoni, C. Breast Milk Composition and Infant Nutrient Intakes during the First 12 Months of Life. Eur. J. Clin. Nutr. 2016, 70, 250–256. [Google Scholar] [CrossRef] [PubMed]
- Barreiro, R.; Díaz-Bao, M.; Cepeda, A.; Regal, P.; Fente, C.A. Fatty Acid Composition of Breast Milk in Galicia (NW Spain): A Cross-Country Comparison. Prostaglandins Leukot. Essent. Fatty Acids 2018, 135, 102–114. [Google Scholar] [CrossRef] [PubMed]
- Keikha, M.; Bahreynian, M.; Saleki, M.; Kelishadi, R. Macro- and Micronutrients of Human Milk Composition: Are They Related to Maternal Diet? A Comprehensive Systematic Review. Breastfeed. Med. 2017, 12, 517–527. [Google Scholar] [CrossRef] [PubMed]
- Craig-Schmidt, M.C. World-Wide Consumption of Trans Fatty Acids. Atheroscler. Suppl. 2006, 7, 1–4. [Google Scholar] [CrossRef]
- Ganguly, R.; Pierce, G.N. The Toxicity of Dietary Trans Fats. Food Chem. Toxicol. 2015, 78, 170–176. [Google Scholar] [CrossRef]
- Mennitti, L.V.; Oliveira, J.L.; Morais, C.A.; Estadella, D.; Oyama, L.M.; do Nascimento, C.M.O.; Pisani, L.P. Type of Fatty Acids in Maternal Diets during Pregnancy and/or Lactation and Metabolic Consequences of the Offspring. J. Nutr. Biochem. 2015, 26, 99–111. [Google Scholar] [CrossRef] [PubMed]
- Valenzuela, C.A.; Baker, E.J.; De Souza, C.O.; Miles, E.A.; Calder, P.C. Differential Effects of Ruminant and Industrial 18-Carbon Trans-Monounsaturated Fatty Acids (Trans Vaccenic and Elaidic) on the Inflammatory Responses of an Endothelial Cell Line. Molecules 2021, 26, 5834. [Google Scholar] [CrossRef]
- Fan, H.; Xia, S.; Xiang, J.; Li, Y.; Ross, M.O.; Lim, S.A.; Yang, F.; Tu, J.; Xie, L.; Dougherty, U. Trans-Vaccenic Acid Reprograms CD8+ T Cells and Anti-Tumour Immunity. Nature 2023, 623, 1034–1043. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Cao, H.; King, I.B.; Lemaitre, R.N.; Song, X.; Siscovick, D.S.; Hotamisligil, G.S. Trans-Palmitoleic Acid, Metabolic Risk Factors, and New-Onset Diabetes in US Adults: A Cohort Study. Ann. Intern. Med. 2010, 153, 790–799. [Google Scholar] [CrossRef]
- Imamura, F.; Fretts, A.; Marklund, M.; Ardisson Korat, A.V.; Yang, W.-S.; Lankinen, M.; Qureshi, W.; Helmer, C.; Chen, T.-A.; Wong, K. Fatty Acid Biomarkers of Dairy Fat Consumption and Incidence of Type 2 Diabetes: A Pooled Analysis of Prospective Cohort Studies. PLoS Med. 2018, 15, e1002670. [Google Scholar] [CrossRef]
- Guillocheau, E.; Penhoat, C.; Drouin, G.; Godet, A.; Catheline, D.; Legrand, P.; Rioux, V. Current Intakes of Trans-Palmitoleic (Trans-C16: 1 n-7) and Trans-Vaccenic (Trans-C18: 1 n-7) Acids in France Are Exclusively Ensured by Ruminant Milk and Ruminant Meat: A Market Basket Investigation. Food Chem. X 2020, 5, 100081. [Google Scholar] [CrossRef]
- Wolff, R.L. Content and Distribution of Trans-18: 1 Acids in Ruminant Milk and Meat Fats. Their Importance in European Diets and Their Effect on Human Milk. J. Am. Oil Chem. Soc. 1995, 72, 259–272. [Google Scholar] [CrossRef]
- Varela, G.; Moreiras, O.; Ansón, R. Consumo de Alimentos En Galicia-La Dieta Atlántica; Fundación Española de Nutrición: Madrid, Spain, 2004. [Google Scholar]
- Oliveira, A.; Lopes, C.; Rodríguez-Artalejo, F. Adherence to the Southern European Atlantic Diet and Occurrence of Nonfatal Acute Myocardial Infarction. Am. J. Clin. Nutr. 2010, 92, 211–217. [Google Scholar] [CrossRef]
- Guallar-Castillón, P.; Oliveira, A.; Lopes, C.; López-García, E.; Rodríguez-Artalejo, F. The Southern European Atlantic Diet Is Associated with Lower Concentrations of Markers of Coronary Risk. Atherosclerosis 2013, 226, 502–509. [Google Scholar] [CrossRef] [PubMed]
- Nasser, R.; Stephen, A.M.; Goh, Y.K.; Clandinin, M.T. The Effect of a Controlled Manipulation of Maternal Dietary Fat Intake on Medium and Long Chain Fatty Acids in Human Breast Milk in Saskatoon, Canada. Int. Breastfeed. J. 2010, 5, 3. [Google Scholar] [CrossRef] [PubMed]
- Mosley, E.E.; McGuire, M.K.; Williams, J.E.; McGuire, M.A. Cis-9, Trans-11 Conjugated Linoleic Acid Is Synthesized from Vaccenic Acid in Lactating Women. J. Nutr. 2006, 136, 2297–2301. [Google Scholar] [CrossRef]
- Aumeistere, L.; Beluško, A.; Ciproviča, I.; Zavadska, D. Trans Fatty Acids in Human Milk in Latvia: Association with Dietary Habits during the Lactation Period. Nutrients 2021, 13, 2967. [Google Scholar] [CrossRef]
- Thijs, C.; Müller, A.; Rist, L.; Kummeling, I.; Snijders, B.E.P.; Huber, M.; Van Ree, R.; Simões-Wüst, A.P.; Dagnelie, P.C.; Van Den Brandt, P.A. Fatty Acids in Breast Milk and Development of Atopic Eczema and Allergic Sensitisation in Infancy. Allergy 2011, 66, 58–67. [Google Scholar] [CrossRef]
- Chisaguano, A.M.; Montes, R.; Castellote, A.I.; Morales, E.; Júlvez, J.; Vioque, J.; Sunyer, J.; López-Sabater, M.C. Elaidic, Vaccenic, and Rumenic Acid Status during Pregnancy: Association with Maternal Plasmatic LC-PUFAs and Atopic Manifestations in Infants. Pediatr. Res. 2014, 76, 470–476. [Google Scholar] [CrossRef]
- Sánchez, C.; Fente, C.; Barreiro, R.; López-Racamonde, O.; Cepeda, A.; Regal, P. Association between Breast Milk Mineral Content and Maternal Adherence to Healthy Dietary Patterns in Spain: A Transversal Study. Foods 2020, 9, 659. [Google Scholar] [CrossRef] [PubMed]
- Barreiro, R.; Regal, P.; López-Racamonde, O.; Cepeda, A.; Fente, C. Evolution of Breast Milk Fatty Acids in Spanish Mothers after One Year of Uninterrupted Lactation. Prostaglandins Leukot. Essent. Fatty Acids 2020, 159, 102141. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Martín, C.; Garcia-Ortiz, L.; Rodriguez-Sanchez, E.; Martin-Cantera, C.; Soriano-Cano, A.; Arietaleanizbeaskoa, M.S.; Magdalena-Belio, J.F.; Menendez-Suarez, M.; Maderuelo-Fernandez, J.A.; Lugones-Sanchez, C. The Relationship of the Atlantic Diet with Cardiovascular Risk Factors and Markers of Arterial Stiffness in Adults without Cardiovascular Disease. Nutrients 2019, 11, 742. [Google Scholar] [CrossRef] [PubMed]
- Roibás, L.; Martínez, I.; Goris, A.; Barreiro, R.; Hospido, A. An Analysis on How Switching to a More Balanced and Naturally Improved Milk Would Affect Consumer Health and the Environment. Sci. Total Environ. 2016, 566, 685–697. [Google Scholar] [CrossRef] [PubMed]
- Guadarrama-Flores, B.; Matencio, A.; Navarro-Orcajada, S.; Martínez-Lede, I.; Conesa, I.; Vidal-Sánchez, F.J.; García-Carmona, F.; López-Nicolás, J.M. Development if Healthy Milk and Yogurt Products for Reducing Metabolic Diseases Using Cyclodextrin and Omega-3 Fatty Acids from Fish Oil. Food Funct. 2022, 13, 5528–5535. [Google Scholar] [CrossRef] [PubMed]
- Sanjulián, L.; Lamas, A.; Barreiro, R.; Cepeda, A.; Fente, C.A.; Regal, P. Bacterial Diversity of Breast Milk in Healthy Spanish Women: Evolution from Birth to Five Years Postpartum. Nutrients 2021, 13, 2414. [Google Scholar] [CrossRef]
- Jahreis, G.; Pritsche, J.; Steinhart, H. Conjugated Linoleic Acid in Milk Fat: High Variation Depending on Production System. Nutr. Res. 1997, 17, 1479–1484. [Google Scholar] [CrossRef]
- Bergamo, P.; Fedele, E.; Iannibelli, L.; Marzillo, G. Fat-Soluble Vitamin Contents and Fatty Acid Composition in Organic and Conventional Italian Dairy Products. Food Chem. 2003, 82, 625–631. [Google Scholar] [CrossRef]
- van Wijlen, R.P.J.; Colombani, P.C. Grass-Based Ruminant Production Methods and Human Bioconversion of Vaccenic Acid with Estimations of Maximal Dietary Intake of Conjugated Linoleic Acids. Int. Dairy. J. 2010, 20, 433–448. [Google Scholar] [CrossRef]
- Rist, L.; Mueller, A.; Barthel, C.; Snijders, B.; Jansen, M.; Simões-Wüst, A.P.; Huber, M.; Kummeling, I.; von Mandach, U.; Steinhart, H.; et al. Influence of Organic Diet on the Amount of Conjugated Linoleic Acids in Breast Milk of Lactating Women in the Netherlands. Br. J. Nutr. 2007, 97, 735–743. [Google Scholar] [CrossRef]
- Simões-Wüst, A.P.; Rist, L.; Mueller, A.; Huber, M.; Steinhart, H.; Thijs, C. Consumption of Dairy Products of Biodynamic Origin Is Correlated with Increased Contents of Rumenic and Trans-Vaccenic Acid in the Breast Milk of Lactating Women. Org. Agric. 2011, 1, 161–166. [Google Scholar] [CrossRef]
- Turpeinen, A.M.; Mutanen, M.; Aro, A.; Salminen, I.; Basu, S.; Palmquist, D.L.; Griinari, J.M. Bioconversion of Vaccenic Acid to Conjugated Linoleic Acid in Humans. Am. J. Clin. Nutr. 2002, 76, 504–510. [Google Scholar] [CrossRef] [PubMed]
- Hatem, O.; Kaçar, Ö.F.; Kaçar, H.K.; Szentpéteri, J.L.; Marosvölgyi, T.; Szabó, É. Trans Isomeric Fatty Acids in Human Milk and Their Role in Infant Health and Development. Front. Nutr. 2024, 11, 1379772. [Google Scholar] [CrossRef] [PubMed]
- Barreiro, R.; Regal, P.; López-Racamonde, O.; Cepeda, A.; Fente, C.A. Comparison of the Fatty Acid Profile of Spanish Infant Formulas and Galician Women Breast Milk. J. Physiol. Biochem. 2018, 74, 127–138. [Google Scholar] [CrossRef] [PubMed]
- Crawford, M.A.; Wang, Y.; Forsyth, S.; Brenna, J.T. The European Food Safety Authority Recommendation for Polyunsaturated Fatty Acid Composition of Infant Formula Overrules Breast Milk, Puts Infants at Risk, and Should Be Revised. Prostaglandins Leukot. Essent. Fatty Acids 2015, 102, 1–3. [Google Scholar] [CrossRef]
| Maternal Data | Mean | Median | Min | Max | |
|---|---|---|---|---|---|
| Pregnancy Time (weeks) | 39.77 ± 1.34 | 40.00 | 36.00 | 42.29 | |
| Maternal Age (years) | 35.43 ± 4.06 | 35.00 | 26.00 | 46.00 | |
| Maternal BMI (kg/m2) | 24.47 ± 3.83 | 24.36 | 17.85 | 35.03 | |
| Lactating time (months) | 7.77 ± 11.12 | 3.00 | 0.5 | 58.97 | |
| AD adherence (score) | 3.80 ± 1.48 | 4.00 | 0.00 | 7.00 | |
| Infant gender: n♂ (%)/n♀ (%) | 43 (46.73)/49 (53.26) | C-section delivery (%) | 11.96 | Parity number 1st child (%) | 60.87 |
| Cohort 1 | Cohort 2 | Infant Formula | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fatty Acid (%wt/wt of Total Fatty Acids) | LT < 6 | LT ≥ 6 | BMI < 25 | BMI ≥ 25 | Infant 0 | Infant 1 | SEAD < 5 | SEAD ≥ 5 | Milk < 3 | Milk ≥ 3 | Meat < 3 | Meat ≥ 3 | LT < 6 | FSF | FOF | GUF | |
| n = 67 | n = 26 | n = 47 | n = 46 | n = 41 | n = 52 | n = 64 | n = 29 | n = 39 | n = 41 | n = 63 | n = 18 | n = 16 | n = 5 | n = 13 | n = 5 | ||
| 18:1 (n-9) OA | Mean | 28.35 * | 29.38 | 30.02 | 27.34 | 30.12 | 27.47 | 28.17 | 29.67 | 28.41 | 29.49 | 27.74 | 31.88 | 34.49 * | 38.49 | 38.06 * | 39.07 |
| SD | 5.87 | 8.37 | 6.85 | 6.20 | 6.81 | 6.30 | 6.86 | 6.05 | 6.96 | 6.00 | 6.20 | 6.58 | 3.22 | 2.06 | 3.44 | 1.18 | |
| Min | 13.11 | 14.52 | 14.52 | 13.11 | 19.76 | 13.11 | 13.11 | 20.03 | 13.11 | 20.15 | 13.11 | 22.50 | 26.21 | 37.10 | 36.45 | 37.32 | |
| Max | 39.28 | 43.19 | 42.57 | 43.19 | 43.19 | 41.58 | 43.19 | 42.11 | 42.11 | 43.19 | 43.19 | 42.11 | 40.67 | 42.04 | 44.20 | 40.43 | |
| 18:2 (n-6) LA | Mean | 15.96 | 15.78 | 15.63 | 16.18 | 15.68 | 16.10 | 15.84 | 16.08 | 16.64 | 15.23 | 16.50 | 14.53 | 14.60 | 16.26 | 15.64 | 16.96 |
| SD | 3.84 | 4.17 | 4.13 | 3.73 | 4.03 | 3.85 | 3.77 | 4.27 | 4.10 | 3.85 | 3.99 | 2.44 | 3.41 | 0.58 | 3.91 | 2.32 | |
| Min | 9.75 | 8.73 | 8.73 | 9.42 | 8.73 | 9.75 | 8.73 | 9.42 | 9.42 | 8.73 | 8.73 | 9.42 | 8.66 | 15.50 | 11.54 | 14.90 | |
| Max | 26.64 | 23.86 | 26.64 | 24.80 | 24.80 | 26.64 | 24.80 | 26.64 | 26.64 | 22.68 | 26.64 | 19.62 | 23.97 | 16.94 | 24.53 | 20.51 | |
| 18:3 (n-3) ALA | Mean | 0.75 * | 0.91 | 0.91 | 0.68 | 0.66 | 0.89 | 0.83 | 0.70 | 0.94 | 0.71 | 0.79 | 0.70 | 0.50 * | 1.69 * | 1.88 * | 1.98 * |
| SD | 0.49 | 0.75 | 0.74 | 0.33 | 0.29 | 0.71 | 0.66 | 0.31 | 0.69 | 0.37 | 0.52 | 0.29 | 0.13 | 0.54 | 0.28 | 0.36 | |
| Min | 0.25 | 0.31 | 0.31 | 0.25 | 0.25 | 0.31 | 0.31 | 0.25 | 0.31 | 0.25 | 0.25 | 0.40 | 0.30 | 1.23 | 1.69 | 1.45 | |
| Max | 3.59 | 4.12 | 4.12 | 1.69 | 1.55 | 4.12 | 4.12 | 1.54 | 4.12 | 1.67 | 3.59 | 1.54 | 1.08 | 2.27 | 2.35 | 2.35 | |
| 20:4 (n-6) AA | Mean | 0.60 * | 0.60 | 0.58 | 0.61 | 0.59 | 0.60 | 0.59 | 0.61 | 0.58 | 0.60 | 0.59 | 0.56 | 0.45 * | 0.28 * | 0.26 * | 0.11 * |
| SD | 0.14 | 0.19 | 0.16 | 0.16 | 0.16 | 0.15 | 0.16 | 0.15 | 0.15 | 0.18 | 0.15 | 0.15 | 0.11 | 0.19 | 0.07 | 0.09 | |
| Min | 0.22 | 0.30 | 0.30 | 0.22 | 0.22 | 0.31 | 0.30 | 0.22 | 0.30 | 0.22 | 0.22 | 0.35 | 0.28 | 0.18 | 0.28 | 0.02 | |
| Max | 0.98 | 1.00 | 0.98 | 1.00 | 1.00 | 0.98 | 1.00 | 0.98 | 1.00 | 0.98 | 1.00 | 0.88 | 0.72 | 0.62 | 0.36 | 0.21 | |
| 20:5 (n-3) EPA | Mean | 0.14 | 0.12 | 0.15 | 0.13 | 0.12 | 0.15 | 0.14 | 0.13 | 0.14 | 0.15 | 0.14 | 0.10 | 0.11 | 0.07 | 0.07 | 0.06 |
| SD | 0.09 | 0.08 | 0.09 | 0.09 | 0.08 | 0.09 | 0.09 | 0.09 | 0.07 | 0.12 | 0.08 | 0.05 | 0.06 | 0.05 | 0.05 | 0.03 | |
| Min | 0.04 | 0.05 | 0.06 | 0.04 | 0.04 | 0.05 | 0.05 | 0.04 | 0.05 | 0.04 | 0.04 | 0.05 | 0.02 | 0.02 | 0.01 | 0.03 | |
| Max | 0.52 | 0.35 | 0.51 | 0.52 | 0.52 | 0.51 | 0.52 | 0.51 | 0.35 | 0.52 | 0.52 | 0.29 | 0.32 | 0.15 | 0.22 | 0.11 | |
| 22:6 (n-3) DHA | Mean | 0.42 | 0.50 | 0.48 | 0.40 | 0.39 | 0.48 | 0.44 | 0.43 | 0.44 | 0.47 | 0.41 | 0.37 | 0.32 | 0.21 | 0.22 | 0.09 |
| SD | 0.32 | 0.30 | 0.33 | 0.29 | 0.27 | 0.34 | 0.30 | 0.34 | 0.28 | 0.37 | 0.29 | 0.24 | 0.18 | 0.05 | 0.08 | 0.08 | |
| Min | 0.05 | 0.17 | 0.05 | 0.05 | 0.05 | 0.05 | 0.05 | 0.05 | 0.05 | 0.05 | 0.05 | 0.05 | 0.05 | 0.18 | 0.28 | 0.01 | |
| Max | 1.61 | 1.23 | 1.61 | 1.41 | 1.41 | 1.61 | 1.41 | 1.61 | 1.23 | 1.61 | 1.41 | 0.96 | 1.03 | 0.30 | 0.33 | 0.20 | |
| 18:1 (n-7) TVA | Mean | 0.71 * | 0.69 | 0.70 | 0.71 | 0.70 | 0.71 | 0.71 | 0.70 | 0.69 | 0.75 | 0.70 | 0.72 | 1.84 * | 0.47 * | 0.53 * | 0.54 * |
| SD | 0.13 | 0.13 | 0.12 | 0.13 | 0.14 | 0.12 | 0.12 | 0.14 | 0.12 | 0.15 | 0.12 | 0.14 | 0.41 | 0.08 | 0.11 | 0.06 | |
| Min | 0.38 | 0.41 | 0.43 | 0.38 | 0.38 | 0.42 | 0.42 | 0.38 | 0.41 | 0.38 | 0.38 | 0.41 | 1.10 | 0.33 | 0.45 | 0.48 | |
| Max | 0.99 | 0.87 | 0.99 | 0.94 | 0.95 | 0.99 | 0.95 | 0.99 | 0.94 | 0.99 | 0.95 | 0.94 | 2.77 | 0.53 | 0.79 | 0.63 | |
| CLAs | Mean | 0.93 | 0.86 | 0.89 | 0.93 | 0.88 | 0.93 | 0.93 | 0.85 | 0.96 | 0.85 | 0.94 | 0.85 | 0.97 * | 0.58 * | 0.50 * | 0.54 * |
| SD | 0.23 | 0.30 | 0.26 | 0.24 | 0.26 | 0.24 | 0.25 | 0.24 | 0.26 | 0.25 | 0.26 | 0.23 | 0.19 | 0.16 | 0.19 | 0.07 | |
| Min | 0.32 | 0.50 | 0.41 | 0.32 | 0.32 | 0.59 | 0.41 | 0.32 | 0.41 | 0.32 | 0.32 | 0.57 | 0.60 | 0.40 | 0.42 | 0.43 | |
| Max | 1.38 | 1.42 | 1.42 | 1.38 | 1.42 | 1.38 | 1.42 | 1.31 | 1.42 | 1.29 | 1.42 | 1.33 | 1.33 | 0.83 | 0.94 | 0.63 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sanjulian, L.; Lamas, A.; Barreiro, R.; Martínez, I.; García-Alonso, L.; Cepeda, A.; Fente, C.; Regal, P. Investigating the Dietary Impact on Trans-Vaccenic Acid (Trans-C18:1 n-7) and Other Beneficial Fatty Acids in Breast Milk and Infant Formulas. Foods 2024, 13, 2164. https://doi.org/10.3390/foods13142164
Sanjulian L, Lamas A, Barreiro R, Martínez I, García-Alonso L, Cepeda A, Fente C, Regal P. Investigating the Dietary Impact on Trans-Vaccenic Acid (Trans-C18:1 n-7) and Other Beneficial Fatty Acids in Breast Milk and Infant Formulas. Foods. 2024; 13(14):2164. https://doi.org/10.3390/foods13142164
Chicago/Turabian StyleSanjulian, Laura, Alexandre Lamas, Rocío Barreiro, Ismael Martínez, Leopoldo García-Alonso, Alberto Cepeda, Cristina Fente, and Patricia Regal. 2024. "Investigating the Dietary Impact on Trans-Vaccenic Acid (Trans-C18:1 n-7) and Other Beneficial Fatty Acids in Breast Milk and Infant Formulas" Foods 13, no. 14: 2164. https://doi.org/10.3390/foods13142164






