Interaction between Per- and Polyfluorinated Substances (PFAS) and Acetaminophen in Disease Exacerbation—Focusing on Autism and the Gut–Liver–Brain Axis
Abstract
:1. Introduction
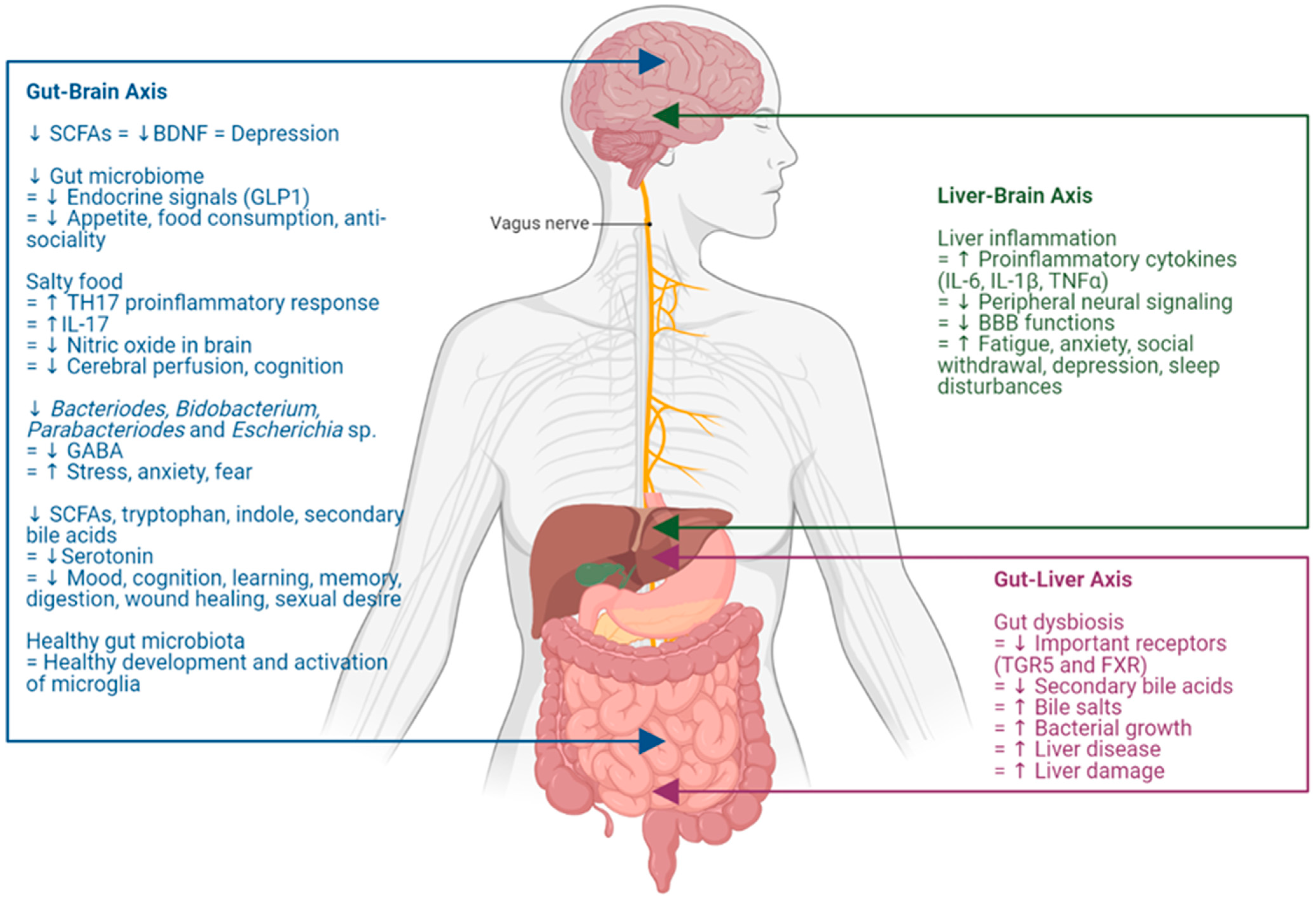
2. The Gut–Liver–Brain Axis
2.1. Gut–Brain Interactions
2.2. Gut–Liver Interactions
2.3. Liver–Brain Interactions
3. Polyfluoroalkyl Substances
3.1. Liver Inflammation and Polyfluoroalkyl Substances
| Organism | Sample Type | Sample Size | Age | Sex | Reagents | Exposure Dose | Exposure Time | Outcome | References |
|---|---|---|---|---|---|---|---|---|---|
| Humans (Cross-sectional) | Liver | 105 | 18 to 75 | M, F | PFAS | Population study | Environmental/ Lifestyle | ↓ Insulin resistance ↑ Liver fat content ↑ Histological liver lesions | [80] |
| Humans (Cross-sectional) | Blood serum | 46,452 | Adults | M, F | PFOS PFOA | Median (IQR) PFOA: 28.0 (13.5–70.8) ng/mL PFOS: 20.3 (13.7–29.4) ng/mL | 2005–2006 | ↑ Alanine aminotransferase (ALT) | [81] |
| Humans (Cross-sectional) | Plasma serum | 230 to 2288 | 20 to 74 | M, F | PFOS PFOA PFHxS PFNA | Population study | Environmental/ Lifestyle | ↑ Aspartate aminotransferase (AST) ↑ Gamma-glutamyltransferase (GGT) ↑ Alkaline phosphatase (ALP) | [82] |
| Humans (Retrospective) | Blood serum | 2883 | Adults (obesed) | M, F | PFOS PFOA PFHxS PFNA | Geometric mean (95% CI) PFOA: 2.0 (1.8–2.1) ng/mL PFOS: 5.5 (5.0–6.0) ng/mL PFNA: 0.73 (0.68–0.79) ng/mL PFHxSe: 1.24 (1.13–1.37) ng/mL | 2011–2014 | PFOA, PFHxS and PFNA: ↑ Alanine aminotransferase (ALT) PFOA and PFNA: ↑ Gamma-glutamyltransferase (GGT) | [83] |
| Rats | Plasma | 90 (3 doses × 3 expsoure period × 10/dose group) | 6–7 weeks | M | K+PFOS | 20 and 100 ppm | 1, 7 and 28 days | ↑ Persoxisome proliferator-activated receptor alpha (PPARa) ↑ Constitutive androstane receptor (CAR) ↑ Pregnane X receptor (PXR) | [85] |
| HepaRG and HepG2 cells | Liver cells | Not indicated | Not relevant | Not relevant | PFOA HFBA PFTA | 5 to 1000 μM | 24 h to 10 days | ↑ Cell apoptosis ↑ ROS production ↑ Pro-inflammatory cytokine (TNFα, IL6) ↑ UPR signalling pathway markers (IRE1α, ATF4, BIP) ↑ Fatty acid metabolic gene markers (SCD1, FASN, ACC) ↑ Transcription factors (SREBP1) ↑ Fibrosis signalling gene markers (TIMP2, p21, TGFβ) ↓ Nrf2 regulated antioxidant defense system | [86] |
| HepG2 cells | Liver cells | Not indicated | Not relevant | Not relevant | PFOA | 0, 0.1, 1, 10, 100 and 1000 ng/mL | 24 h | ↑ Impairment of insulin receptor (InsR) signalling pathway ↑ Altered glycogen synthesis ↓ Glucose uptake | [87] |
| Humans (Cross-sectional) | Blood serum | 74 | Children (with NAFLD) | M, F | PFOS PFOA PFHxS | Median (IQR) PFOA: 3.42 (1.65) ng/mL PFOS: 3.59 (4:46) ng/mL PFHxS: 1.53 (3:17) ng/mL | 2007–2015 | ↑ NAFLD ↑ NASH ↑ Fibrosis ↑ Lobular/portal inflammation ↑ NAFLD activity scire | [88] |
| HepG2 cells | Liver cells | Not indicated | Not relevant | Not relevant | PFOA PFOS PFNA PFDA PFHxS | 0.2, 2 and 20 μM | 24 h | ↓ Glutathione levels | [89] |
3.2. Neuroinflammation and Polyfluoroalkyl Substances
3.3. Other Neurological Diseases and Polyfluoroalkyl Substances
3.4. Gut Microbiome and Polyfluoroalkyl Substances
| Organism | Sample Type | Sample Size | Age | Sex | Reagents | Exposure Dose | Exposure Time | Disease/Disorder | Outcome | References |
|---|---|---|---|---|---|---|---|---|---|---|
| Rats | Brain (hippocamal neurons) | Not indicated | Not indicated | Not indicated | PFOA PFOS | 30, 100 and 300 µmol/L | 30 min | ADHD | ↑ Calcium concentration in neurons ↑ Synaptic transmission ↑ Neuronal excitement ↑ Cell apoptosis | [94] |
| Rats | Brain, (cortex and hippocampus) | 4 groups of 8 to 10 | Adult | M | PFOS | 1.7, 5.0, and 15.0 mg/L | 91 days | ADHD | ↑ Alteration of calcium-dependent signalling molecules expression (CaMKII, CREB, CaM) | [96] |
| Northern leopard frogs | Whole body | Not indicated | Larvae | M, F | PFOA PFOS | 10, 100, and 1000 ppb | 30 days | ADHD | ↓ Dopamine ↑ Glutamate | [97] |
| Rats | Brain (amgydala, prefrontal cortex and hippocampus) | 5 groups of 6 | 2 months | M | PFOS | 0.5; 1.0; 3.0 and 6.0 mg/kg | 28 days | ADHD | ↑ Dopamine | [97,99] |
| Mice | Brain (cerebral cortex and hippocampus) | Not indicated | 10 days | M | PFOS | 11.3 mg/kg | 24 h; 2 months post exposure | ADHD | ↓ Dopamine receptor-D5 ↓ Dopamine receptor-D2 | [98] |
| Mice | Brain and liver | Not indicated | Not indicated | M | PFOA PFAS mixtures | 0.5 and 2.5 mg/kg | 28 days | ADHD | Dopamine concentration:↑ PFOA | [100] |
| Mice | Brain and liver | Not indicated | Not indicated | M | PFOA | 2.5 mg/kg | 28 days | Impaired neurodevelopment | ↓ Glutamate | [100] |
| Mice | Brain (hippocampus) | 4 group of 15 | 2 months | M, F | PFOS | 10.75 mg/kg | 3 months | Impaired spatial learning and memory | ↑ Glutamate | [101] |
| Mice | Behaviourial test | Not indicated | Neonatal | M | PFOA PFOS | PFOA: 0.58 or 8.70 mg/kg PFOS: 0.75 or 11.3 mg/kg | 10 days | Associated with neurodevelopment | ↓ Cholinergic system | [102] |
| Mice | Lung | 3 group of 8 | Pregnant adults | F | PFOS | 0, 1 or 5 mg/kg | Gestational day 12 to 18 | Parkinson’s disease | ↑ Inflammasome activation in the brain ↑ NOD-, LRR- and pyrin domain-containing protein 3 (NLRP3) | [103] |
| Mice | Dopaminergic primary cultured neurons | 2 groups of 6 | 2 months | M | PFOS | 10 mg/kg | 14 days | Parkinson’s disease | ↑ Synuclein aggregation ↑ Dopaminergic degeneration | [104] |
| Humans | Epidemiological database | 369,826 | 0 to > 74 | M, F | PFAS | Ecological mortality study | 1980 to 2013 | Cerebrovascular diseases Alzheimer’s diseases Parkinson’s disease | Ecological mortality study ↑ Significant relative risk | [105] |
| Humans | Maternal plasma and fetal physical features | 656 | 5 | M, F | PFAS | Birth Cohort Study | Prenatal exposure | Down syndrome | Shorter palpebral fissure length Lower IQ scores Behavioural impairment | [106] |
| Mice | Brain, liver, intestines, blood and faeces | 5 groups of 10 | 8 weeks | M | PFOA | 0, 0.5, 1, and 3 mg/kg | 35 days | Associated with brain inflammation and impairment | ↑ LPS content and TNF- α levels in the cortex ↑ Cognitive deficits and dysbiosis with the gut and brain | [116] |
| Humans | Plasma serum and cord blood | 725 | Maternal and fetal | M, F | PFHxS | Birth Cohort Study | Prenatal exposure | Associated with fetal neurodevelopment | ↑ Brain-derived neurotrophic factor (BDNF) expression | [117] |
| Organism | Sample Type | Sample Size | Age | Sex | Reagents | Exposure Dose | Exposure Time | Outcome | References |
|---|---|---|---|---|---|---|---|---|---|
| Human | Blood, urine and faeces | 79 | Nil | M, F | PFAS | Population study | Nil | ↓ genus: Thermogemmatisporales, Stigonematales, and Legionellales | [109] |
| Humans | Breast milk and infant faeces | Breastmilk: 333 mothers and 328 children Faeces: 535 mothers and 552 children | Not indicated | M, F | PFOS PFOA | Cohort study PFOS: 0.12 ng/mL PFOA: 0.05 ng/mL | 2002 to 2005 | ↓ microbiome α-diversity and Lactobacillus ↑ Enterococcus in breast milk | [110] |
| Human | Maternal blood, cord blood and and infant faeces | Nil | Nil | M, F | PFOS PFOA | Cohort study Maternal blood: 2.4 ng/mL Cord blood: 1.14 ng/mL | Nil | ↓ genus: Faecalibacterium ↑ genus: Clostridium, Streptococcus, Gemella and Bifidobacterium | [111,112] |
| Mice | Liver, faeces | 8 groups of 6 | 2 months | M | PFOS | 5, 10 and 20 mg/kg | 14 days | ↓ genus: Lactobacillus, Limosilactobacillus, Neglecta, Ligilactobacillus, Ihubacter, Parasutterella, ↑ genus: Escherichia/Shigella, Bilophila, Parabacteroides | [113] |
| Humans | Whole blood, cord blood, postnatal serum and faeces | Nil | 7, 14, 22 and 28 years | M, F | PFOS PFOA | Cohort study | Nil | PFOS: ↑ species: Bilophila wadsworthia, Faecalibacterium prautzii, Dorea longicatena and Sutterella wadsworthensis PFOA: ↑ species: Bacteroidetes and Odoribacter splanchnicus | [114] |
| Mice | Liver and faeces | 4 groups of 5 | 8 to 10 weeks | M | PFOS | 0, 0.003%, 0.006%, and 0.012% | 21 days | ↓ phylum: Firmicutes and Bacteroidetes ↓ genus: Flavonifractor and Alistipes ↑ phylum: Firmicutes ↑ genus: Clostridium and Streptococcus | [115] |
| Mice | Brain, blood, liver, intestine and faeces | 5 groups of 10 | 8 weeks | M | PFOA | 0, 0.5, 1, and 3 mg/kg | 5 weeks | ↓ phylum: Firmicutes, Verrucomicrobia, Actinobacteria and Bacteroidetes ↓ genus: Ruminococcus, Anoxybacillus, Gemmiger, Akkermansia, Bifidobacterium and Parabacteroides ↓ integrity of their intestinal barrier ↓ concentrations of SCFA ↓ capability in spatial memory and learning ↑ phylum: Bacteroidetes | [116] |
4. Acetaminophen
4.1. Autism Epidemic and Acetaminophen
4.2. Liver Inflammation and Acetaminophen
4.3. Neuroinflammation and Acetaminophen
4.4. Gut Microbiome and Acetaminophen
| Organism | Sample Type | Sample Size | Age | Sex | Reagents | Exposure Dose | Exposure Time | Effects | Outcome | References |
|---|---|---|---|---|---|---|---|---|---|---|
| Rats | Brain endothelial cells | Not indicated | Not indicated | Not indicated | APAP | 100 μM | 8 h | Protective | ↓ SOD activity ↓ Inflammatory proteins ↓ Superoxide-generating compound menadione ↑ Cell survival | [56] |
| Rats | Plasma and cerebrospinal fluid | 2 groups of 6–8 | Not indicated | F | APAP | 250 and 500 mg/kg | 1, 3 and 6 h | Toxic | ↑ Neuronal death in cortex | [127] |
| Rats | Testes (ex vivo organotypic culture) | Not indicated | Gestation day 14.5 | M | APAP | 0.1 μM to 100 Μm | 24, 48 and 72 h | Toxic | ↓ Testoesterone production ↓ Brain development | [128] |
| Rats | Brain | 70 | Adult | M | APAP | 5 to 100 mg/kg | 24 h | Protective | ↓ ROS ↓ Mitochondrial redox impairment ↓ Lipid peroxidation level ↓ Ca2+- ATPase activity ↑ Reduced glutathione (GSH) ↑ Glutathione peroxidase (GSH-Px) ↑ Vitamin E | [129] |
| Rats | Hippocampal neurons and PC12 cell line | Not indicated | Not relevant | Not relevant | APAP | 10 mM | 24 h | Protective | ↓ Lipid peroxidation level ↓ Amyloid-beta peptide-induced oxidative stress | [130] |
| Guinea pigs | Heart | 2 groups of 4 | Not indicated | M | APAP | 0.35 mM | 1 time | Protective | ↓ Protein oxidation ↓ Damaging effects of hydrogen peroxide and peroxynitrite in the heart | [131] |
| Rats | Brain | 24 | Adult | M | APAP | 100 mg/kg | 3 h (injection/hour) | Protective | ↓ 1-methyl-4-phenylpyridinium induced toxicity in mitochondria; Protected dopaminergic neurons | [132] |
| Rats | Brain (hippocampus) | 5 groups of 5 | Adult | M | APAP | 100 mg/kg | 7 days | Protective | ↓ Superoxide generation caused by quinolinic acid | [133] |
| Rats | Whole brain Frontal cortex and hippocampal proteins | 60 | Adult | M | APAP | 200 mg/kg | 1, 15 and 30 days | Toxic | ↑ Brain-derived neurotrophic factor (BDNF) expression ↓ Learning and memory (cognitive impairment) | [137] |
5. Potential Interactions between PFAS and Acetaminophen in Exacerbating Autism Spectrum Disorder
6. Conclusions and Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Volkmar, F.R.; Paul, R.; Klin, A.; Cohen, D.E. Handbook of Sutism and Pervasive Developmental Disorders, Volume 1: Diagnosis, Development, Neurobiology, and Behavior; John Wiley & Sons Inc.: Hoboken, NJ, USA, 2005. [Google Scholar]
- CDC. Per- and Polyfluorinated Substances (PFAS) Factsheet. Centers for Disease Control and Prevention. National Biomonitoring Program. 2022. Available online: https://www.cdc.gov/biomonitoring/PFAS_FactSheet.html (accessed on 9 August 2023).
- Bjørklund, G.; Skalny, A.V.; Rahman, M.; Dadar, M.; Yassa, H.A.; Aaseth, J.; Chirumbolo, S.; Skalnaya, M.G.; Tinkov, A.A. Toxic metal(loid)-based pollutants and their possible role in autism spectrum disorder. Environ. Res. 2018, 166, 234–250. [Google Scholar] [CrossRef]
- Bölte, S.; Girdler, S.; Marschik, P.B. The contribution of environmental exposure to the etiology of autism spectrum disorder. Cell. Mol. Life Sci. 2019, 76, 1275–1297. [Google Scholar] [CrossRef]
- Cattane, N.; Richetto, J.; Cattaneo, A. Prenatal exposure to environmental insults and enhanced risk of developing Schizophrenia and Autism Spectrum Disorder: Focus on biological pathways and epigenetic mechanisms. Neurosci. Biobehav. Rev. 2020, 117, 253–278. [Google Scholar] [CrossRef]
- Cheroni, C.; Caporale, N.; Testa, G. Autism spectrum disorder at the crossroad between genes and environment: Contributions, convergences, and interactions in ASD developmental pathophysiology. Mol. Autism 2020, 11, 69. [Google Scholar] [CrossRef]
- Ijomone, O.M.; Olung, N.F.; Akingbade, G.T.; Okoh, C.O.; Aschner, M. Environmental influence on neurodevelopmental disorders: Potential association of heavy metal exposure and autism. J. Trace Elem. Med. Biol. 2020, 62, 126638. [Google Scholar] [CrossRef]
- Roberts, J.R.; Dawley, E.H.; Reigart, J.R. Children’s low-level pesticide exposure and associations with autism and ADHD: A review. Pediatr. Res. 2019, 85, 234–241. [Google Scholar] [CrossRef]
- Aktar, R.; Parkar, N.; Stentz, R.; Baumard, L.; Parker, A.; Goldson, A.; Brion, A.; Carding, S.; Blackshaw, A.; Peiris, M. Human resident gut microbe Bacteroides thetaiotaomicron regulates colonic neuronal innervation and neurogenic function. Gut Microbes 2020, 11, 1745–1757. [Google Scholar] [CrossRef]
- Balaguer-Trias, J.; Deepika, D.; Schuhmacher, M.; Kumar, V. Impact of Contaminants on Microbiota: Linking the Gut–Brain Axis with Neurotoxicity. Int. J. Environ. Res. Public Health 2022, 19, 1368. [Google Scholar] [CrossRef] [PubMed]
- Clarke, G.; Grenham, S.; Scully, P.; Fitzgerald, P.; Moloney, R.D.; Shanahan, F.; Dinan, T.G.; Cryan, J.F. The microbiome-gut-brain axis during early life regulates the hippocampal serotonergic system in a sex-dependent manner. Mol. Psychiatry 2013, 18, 666–673. [Google Scholar] [CrossRef] [PubMed]
- Erny, D.; Hrabě de Angelis, A.L.; Jaitin, D.; Wieghofer, P.; Staszewski, O.; David, E.; Keren-Shaul, H.; Mahlakoiv, T.; Jakobshagen, K.; Buch, T.; et al. Host microbiota constantly control maturation and function of microglia in the CNS. Nat. Neurosci. 2015, 18, 965–977. [Google Scholar] [CrossRef] [PubMed]
- Guo, T.L.; Chen, Y.; Xu, H.S.; McDonough, C.M.; Huang, G. Gut microbiome in neuroendocrine and neuroimmune interactions: The case of genistein. Toxicol. Appl. Pharmacol. 2020, 402, 115130. [Google Scholar] [CrossRef] [PubMed]
- Luck, B.; Engevik, M.A.; Ganesh, B.P.; Lackey, E.P.; Lin, T.; Balderas, M.; Major, A.; Runge, J.; Luna, R.A.; Sillitoe, R.V.; et al. Bifidobacteria shape host neural circuits during postnatal development by promoting synapse formation and microglial function. Sci. Rep. 2020, 10, e54176. [Google Scholar] [CrossRef] [PubMed]
- Yao, Y.; Uddin, M.N.; Manley, K.; Lawrence, D.A. Improvements of autism-like behaviors but limited effects on immune cell metabolism after mitochondrial replacement in BTBR T+ Itpr3tf/J mice. J. Neuroimmunol. 2022, 368, 577893. [Google Scholar] [CrossRef] [PubMed]
- Abdelmohcine, A.; El Amine, S.; Warda, K.; El Baz, S.; Khanouchi, M.; El-Mansoury, B.; Agnaou, M.; Smimih, K.; Zouhairi, N.; Chatoui, H.; et al. Hyperammonemia induces gut microbiota dysbiosis and motor coordination disturbances in mice: New insight into gut-brain axis involvement in hepatic encephalopathy. Acta Neurobiol. Exp. 2023, 83, 203–215. [Google Scholar] [CrossRef] [PubMed]
- Bajaj, J.S.; Shamsaddini, A.; Fagan, A.; McGeorge, S.; Gavis, E.; Sikaroodi, M.; Brenner, L.A.; Wade, J.B.; Gillevet, P.M. Distinct gut microbial compositional and functional changes associated with impaired inhibitory control in patients with cirrhosis. Gut Microbes 2021, 13, 1953247. [Google Scholar] [CrossRef] [PubMed]
- Camara-Lemarroy, C.R.; Silva, C.; Greenfield, J.; Liu, W.-Q.; Metz, L.M.; Yong, V.W. Biomarkers of intestinal barrier function in multiple sclerosis are associated with disease activity. Mult. Scler. J. 2020, 26, 1340–1350. [Google Scholar] [CrossRef]
- Lv, W.-J.; Wu, X.-L.; Chen, W.-Q.; Li, Y.-F.; Zhang, G.-F.; Chao, L.-M.; Zhou, J.-H.; Guo, A.; Liu, C.; Guo, S.-N. The Gut Microbiome Modulates the Changes in Liver Metabolism and in Inflammatory Processes in the Brain of Chronic Unpredictable Mild Stress Rats. Oxidative Med. Cell. Longev. 2019, 2019, 7902874. [Google Scholar] [CrossRef]
- Mahmoudian Dehkordi, S.; Arnold, M.; Nho, K.; Ahmad, S.; Jia, W.; Xie, G. Alzheimer Disease Metabolomics Consortium. Altered bile acid profile associates with cognitive impairment in Alzheimer’s disease—An emerging role for gut microbiome. Alzheimers Dement. 2019, 15, 76–92. [Google Scholar] [CrossRef]
- Nho, K.; Kueider-Paisley, A.; MahmoudianDehkordi, S.; Arnold, M.; Risacher, S.L.; Louie, G. Alzheimer Disease Metabolomics Consortium. Altered bile acid profile in mild cognitive impairment and Alzheimer’s disease: Relationship to neuroimaging and CSF biomarkers. Alzheimers Dement. 2019, 15, 232–244. [Google Scholar] [CrossRef]
- Pu, Z.; Liu, S.; Guo, Z.; Zhang, X.; Yan, J.; Tang, Y.; Bai, Q. Casein Reactivates Dopaminergic Nerve Injury and Intestinal Inflammation with Disturbing Intestinal Microflora and Fecal Metabolites in a Convalescent Parkinson’s Disease Mouse Model. Neuroscience 2023, 524, 120–136. [Google Scholar] [CrossRef]
- Veniaminova, E.; Oplatchikova, M.; Bettendorff, L.; Kotenkova, E.; Lysko, A.; Vasilevskaya, E.; Kalueff, A.V.; Fedulova, L.; Umriukhin, A.; Lesch, K.-P.; et al. Prefrontal cortex inflammation and liver pathologies accompany cognitive and motor deficits following Western diet consumption in non-obese female mice. Life Sci. 2019, 241, 117163. [Google Scholar] [CrossRef] [PubMed]
- Zhang, A.; Matsushita, M.; Zhang, L.; Wang, H.; Shi, X.; Gu, H.; Xia, Z.; Cui, J.Y. Cadmium exposure modulates the gut-liver axis in an Alzheimer’s disease mouse model. Commun. Biol. 2021, 4, 1398. [Google Scholar] [CrossRef] [PubMed]
- Cryan, J.F.; O’Riordan, K.J.; Cowan, C.S.; Sandhu, K.V.; Bastiaanssen, T.F.; Boehme, M.; Codagnone, M.G.; Cussotto, S.; Fulling, C.; Golubeva, A.V.; et al. The microbiota-gut-brain axis. Physiol. Rev. 2019, 99, 1877–2013. [Google Scholar] [CrossRef] [PubMed]
- Martin, C.R.; Osadchiy, V.; Kalani, A.; Mayer, E.A. The brain-gut-microbiome axis. Cell. Mol. Gastroenterol. Hepatol. 2018, 6, 133–148. [Google Scholar] [CrossRef]
- Dalile, B.; Van Oudenhove, L.; Vervliet, B.; Verbeke, K. The role of short-chain fatty acids in microbiota–gut–brain communication. Nat. Rev. Gastroenterol. Hepatol. 2019, 16, 461–478. [Google Scholar] [CrossRef] [PubMed]
- Clemmensen, C.; Müller, T.D.; Woods, S.C.; Berthoud, H.-R.; Seeley, R.J.; Tschöp, M.H. Gut-Brain Cross-Talk in Metabolic Control. Cell 2017, 168, 758–774. [Google Scholar] [CrossRef]
- Bäckhed, F.; Ding, H.; Wang, T.; Hooper, L.V.; Koh, G.Y.; Nagy, A.; Semenkovich, C.F.; Gordon, J.I. The Gut Microbiota as an Environmental Factor That Regulates Fat Storage. Proc. Natl. Acad. Sci. USA 2004, 101, 15718–15723. [Google Scholar] [CrossRef]
- Desbonnet, L.; Clarke, G.; Shanahan, F.; Dinan, T.G.; Cryan, J.F. Microbiota is essential for social development in the mouse. Mol. Psychiatry 2014, 19, 146–148. [Google Scholar] [CrossRef]
- Faraco, G.; Brea, D.; Garcia-Bonilla, L.; Wang, G.; Racchumi, G.; Chang, H.; Buendia, I.; Santisteban, M.M.; Segarra, S.G.; Koizumi, K.; et al. Dietary salt promotes neurovascular and cognitive dysfunction through a gut-initiated TH17 response. Nat. Neurosci. 2018, 21, 240–249. [Google Scholar] [CrossRef]
- Duranti, S.; Ruiz, L.; Lugli, G.A.; Tames, H.; Milani, C.; Mancabelli, L.; Mancino, W.; Longhi, G.; Carnevali, L.; Sgoifo, A.; et al. Bifidobacterium adolescentis as a key member of the human gut microbiota in the production of GABA. Sci. Rep. 2020, 10, 14112. [Google Scholar] [CrossRef]
- Otaru, N.; Ye, K.; Mujezinovic, D.; Berchtold, L.; Constancias, F.; Cornejo, F.A.; Pugin, B. GABA production by human intestinal Bacteroides spp.: Prevalence, regulation, and role in acid stress tolerance. Front. Microbiol. 2021, 12, 656895. [Google Scholar] [CrossRef] [PubMed]
- Strandwitz, P.; Kim, K.H.; Terekhova, D.; Liu, J.K.; Sharma, A.; Levering, J.; McDonald, D.; Dietrich, D.; Ramadhar, T.R.; Lekbua, A.; et al. GABA-modulating bacteria of the human gut microbiota. Nat. Microbiol. 2019, 4, 396–403. [Google Scholar] [CrossRef] [PubMed]
- Pokusaeva, K.; Johnson, C.; Luk, B.; Uribe, G.; Fu, Y.; Oezguen, N.; Matsunami, R.K.; Lugo, M.; Major, A.; Mori-Akiyama, Y.; et al. GABA-producing Bifidobacterium dentium modulates visceral sensitivity in the intestine. Neurogastroenterol. Motil. 2016, 29, e12904. [Google Scholar] [CrossRef] [PubMed]
- Morris, G.; Berk, M.; Carvalho, A.; Caso, J.R.; Sanz, Y.; Walder, K.; Maes, M. The Role of the Microbial Metabolites Including Tryptophan Catabolites and Short Chain Fatty Acids in the Pathophysiology of Immune-Inflammatory and Neuroimmune Disease. Mol. Neurobiol. 2017, 54, 4432–4451. [Google Scholar] [CrossRef] [PubMed]
- Yano, J.M.; Yu, K.; Donaldson, G.P.; Shastri, G.G.; Ann, P.; Ma, L.; Nagler, C.R.; Ismagilov, R.F.; Mazmanian, S.K.; Hsiao, E.Y. Indigenous Bacteria from the Gut Microbiota Regulate Host Serotonin Biosynthesis. Cell 2015, 161, 264–276. [Google Scholar] [CrossRef] [PubMed]
- Fernstrom, J.D.; Coppola, A.; Wenner, B.R.; Ilkayeva, O.; Stevens, R.D.; Maggioni, M.; Slotkin, T.A.; Levin, E.D.; Newgard, C.B.; O’Kane, R.L.; et al. Role of precursor availability in control of monoamine biosynthesis in brain. Physiol. Rev. 1983, 63, 484–546. [Google Scholar] [CrossRef] [PubMed]
- Banks, W.A. Characteristics of compounds that cross the blood-brain barrier. BMC Neurol. 2009, 9, S3. [Google Scholar] [CrossRef]
- Ding, J.-H.; Jin, Z.; Yang, X.-X.; Lou, J.; Shan, W.-X.; Hu, Y.-X.; Du, Q.; Liao, Q.-S.; Xie, R.; Xu, J.-Y. Role of gut microbiota via the gut-liver-brain axis in digestive diseases. World J. Gastroenterol. 2020, 26, 6141–6162. [Google Scholar] [CrossRef]
- Johnson, K.V.-A.; Foster, K.R. Why does the microbiome affect behaviour? Nat. Rev. Genet. 2018, 16, 647–655. [Google Scholar] [CrossRef]
- Bosi, A.; Banfi, D.; Bistoletti, M.; Giaroni, C.; Baj, A. Tryptophan Metabolites Along the Microbiota-Gut-Brain Axis: An Interkingdom Communication System Influencing the Gut in Health and Disease. Int. J. Tryptophan Res. 2020, 13, 1178646920928984. [Google Scholar] [CrossRef]
- Morais, L.H.; Schreiber, H.L., IV; Mazmanian, S.K. The gut microbiota–brain axis in behaviour and brain disorders. Nat. Rev. Microbio. 2021, 19, 241–255. [Google Scholar] [CrossRef] [PubMed]
- Bellono, N.W.; Bayrer, J.R.; Leitch, D.B.; Castro, J.; Zhang, C.; O’Donnell, T.A.; Brierley, S.M.; Ingraham, H.A.; Julius, D. Enterochromaffin Cells Are Gut Chemosensors that Couple to Sensory Neural Pathways. Cell 2017, 170, 185–198. [Google Scholar] [CrossRef]
- Kabouridis, P.S.; Lasrado, R.; McCallum, S.; Chng, S.H.; Snippert, H.J.; Clevers, H.; Pettersson, S.; Pachnis, V. Microbiota Controls the Homeostasis of Glial Cells in the Gut Lamina Propria. Neuron 2015, 85, 289–295. [Google Scholar] [CrossRef] [PubMed]
- Bajaj, J.S.; Heuman, D.M.; Hylemon, P.B.; Sanyal, A.J.; White, M.B.; Monteith, P.; Noble, N.A.; Unser, A.B.; Daita, K.; Fisher, A.R.; et al. Altered profile of human gut microbiome is associated with cirrhosis and its complications. J. Hepatol. 2014, 60, 940–947. [Google Scholar] [CrossRef] [PubMed]
- Behary, J.; Amorim, N.; Jiang, X.-T.; Raposo, A.; Gong, L.; McGovern, E.; Ibrahim, R.; Chu, F.; Stephens, C.; Jebeili, H.; et al. Gut microbiota impact on the peripheral immune response in non-alcoholic fatty liver disease related hepatocellular carcinoma. Nat. Commun. 2021, 12, 187. [Google Scholar] [CrossRef] [PubMed]
- Kang, K.; Sun, Y.; Pan, D.; Sang, L.-X.; Sun, M.-J.; Li, Y.-L.; Chang, B. Distinctive gut microbial dysbiosis between chronic alcoholic fatty liver disease and metabolic-associated fatty liver disease in mice. Exp. Ther. Med. 2021, 21, 418. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.-N.; Joo, E.-J.; Cheong, H.S.; Kim, Y.; Kim, H.-L.; Shin, H.; Chang, Y.; Ryu, S. Gut Microbiota and Risk of Persistent Nonalcoholic Fatty Liver Diseases. J. Clin. Med. 2019, 8, 1089. [Google Scholar] [CrossRef]
- Lang, S.; Demir, M.; Martin, A.; Jiang, L.; Zhang, X.; Duan, Y.; Gao, B.; Wisplinghoff, H.; Kasper, P.; Roderburg, C.; et al. Intestinal Virome Signature Associated With Severity of Nonalcoholic Fatty Liver Disease. Gastroenterology 2020, 159, 1839–1852. [Google Scholar] [CrossRef]
- Lapidot, Y.; Amir, A.; Nosenko, R.; Uzan-Yulzari, A.; Veitsman, E.; Cohen-Ezra, O.; Davidov, Y.; Weiss, P.; Bradichevski, T.; Segev, S.; et al. Alterations in the Gut Microbiome in the Progression of Cirrhosis to Hepatocellular Carcinoma. mSystems 2020, 5, 10–1128. [Google Scholar] [CrossRef]
- Liao, L.; Schneider, K.M.; Galvez, E.J.C.; Frissen, M.; Marschall, H.-U.; Su, H.; Hatting, M.; Wahlström, A.; Haybaeck, J.; Puchas, P.; et al. Intestinal dysbiosis augments liver disease progression via NLRP3 in a murine model of primary sclerosing cholangitis. Gut 2019, 68, 1477–1492. [Google Scholar] [CrossRef]
- Ponziani, F.R.; Bhoori, S.; Castelli, C.; Putignani, L.; Rivoltini, L.; Del Chierico, F.; Sanguinetti, M.; Morelli, D.; Sterbini, F.P.; Petito, V.; et al. Hepatocellular Carcinoma Is Associated With Gut Microbiota Profile and Inflammation in Nonalcoholic Fatty Liver Disease. Hepatology 2019, 69, 107–120. [Google Scholar] [CrossRef] [PubMed]
- Almeida, J.I.; Tenreiro, M.F.; Martinez-Santamaria, L.; Guerrero-Aspizua, S.; Gisbert, J.P.; Alves, P.M.; Serra, M.; Baptista, P.M. Hallmarks of the human intestinal microbiome on liver maturation and function. J. Hepatol. 2021, 76, 694–725. [Google Scholar] [CrossRef]
- Stärkel, P.; Schnabl, B. Bidirectional Communication between Liver and Gut during Alcoholic Liver Disease. Semin. Liver Dis. 2016, 36, 331–339. [Google Scholar] [CrossRef]
- Tripathy, D.; Grammas, P. Acetaminophen protects brain endothelial cells against oxidative stress. Microvasc. Res. 2009, 77, 289–296. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira, M.C.; Gilglioni, E.H.; de Boer, B.A.; Runge, J.H.; de Waart, D.R.; Salgueiro, C.L.; Gaemers, I.C. Bile acid receptor agonists INT747 and INT777 decrease oestrogen deficiency-related postmenopausal obesity and hepatic steatosis in mice. Biochim. Et Biophys. Acta (BBA) Mol. Basis Dis. 2016, 1862, 2054–2062. [Google Scholar] [CrossRef] [PubMed]
- Sinal, C.J.; Tohkin, M.; Miyata, M.; Ward, J.M.; Lambert, G.; Gonzalez, F.J. Targeted Disruption of the Nuclear Receptor FXR/BAR Impairs Bile Acid and Lipid Homeostasis. Cell 2000, 102, 731–744. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Chen, K.; Li, F.; Gu, Z.; Liu, Q.; He, L.; Shao, T.; Song, Q.; Zhu, F.; Zhang, L.; et al. Probiotic Lactobacillus rhamnosus GG Prevents Liver Fibrosis Through Inhibiting Hepatic Bile Acid Synthesis and Enhancing Bile Acid Excretion in Mice. Hepatology 2019, 71, 2050–2066. [Google Scholar] [CrossRef] [PubMed]
- Zhong, W.; Wei, X.; Hao, L.; Lin, T.-D.; Yue, R.; Sun, X.; Guo, W.; Dong, H.; Li, T.; Ahmadi, A.R.; et al. Paneth Cell Dysfunction Mediates Alcohol-related Steatohepatitis Through Promoting Bacterial Translocation in Mice: Role of Zinc Deficiency. Hepatology 2019, 71, 1575–1591. [Google Scholar] [CrossRef]
- Zhou, D.; Pan, Q.; Shen, F.; Cao, H.-X.; Ding, W.-J.; Chen, Y.-W.; Fan, J.-G. Total fecal microbiota transplantation alleviates high-fat diet-induced steatohepatitis in mice via beneficial regulation of gut microbiota. Sci. Rep. 2017, 7, 1529. [Google Scholar] [CrossRef]
- Spadoni, I.; Zagato, E.; Bertocchi, A.; Paolinelli, R.; Hot, E.; Di Sabatino, A.; Caprioli, F.; Bottiglieri, L.; Oldani, A.; Viale, G.; et al. A gut-vascular barrier controls the systemic dissemination of bacteria. Science 2015, 350, 830–834. [Google Scholar] [CrossRef]
- Claeys, W.; Van Hoecke, L.; Geerts, A.; Van Vlierberghe, H.; Lefere, S.; Van Imschoot, G.; Van Wonterghem, E.; Ghesquière, B.; Vandenbroucke, R.E.; Van Steenkiste, C. A mouse model of hepatic encephalopathy: Bile duct ligation induces brain ammonia overload, glial cell activation and neuroinflammation. Sci. Rep. 2022, 12, 17558. [Google Scholar] [CrossRef] [PubMed]
- Deng, P.; Barney, J.; Petriello, M.C.; Morris, A.J.; Wahlang, B.; Hennig, B. Hepatic metabolomics reveals that liver injury increases PCB 126-induced oxidative stress and metabolic dysfunction. Chemosphere 2019, 217, 140–149. [Google Scholar] [CrossRef]
- Xie, G.; Wang, X.; Jiang, R.; Zhao, A.; Yan, J.; Zheng, X.; Huang, F.; Liu, X.; Panee, J.; Rajani, C.; et al. Dysregulated bile acid signaling contributes to the neurological impairment in murine models of acute and chronic liver failure. EBioMedicine 2018, 37, 294–306. [Google Scholar] [CrossRef] [PubMed]
- D’mello, C.; Swain, M.G. Liver–brain interactions in inflammatory liver diseases: Implications for fatigue and mood disorders. Brain Behav. Immun. 2014, 35, 9–20. [Google Scholar] [CrossRef] [PubMed]
- De Vadder, F.; Kovatcheva-Datchary, P.; Goncalves, D.; Vinera, J.; Zitoun, C.; Duchampt, A.; Bäckhed, F.; Mithieux, G. Microbiota-Generated Metabolites Promote Metabolic Benefits via Gut-Brain Neural Circuits. Cell 2014, 156, 84–96. [Google Scholar] [CrossRef] [PubMed]
- Haghikia, A.; Jörg, S.; Duscha, A.; Berg, J.; Manzel, A.; Waschbisch, A.; Hammer, A.; Lee, D.-H.; May, C.; Wilck, N.; et al. Dietary Fatty Acids Directly Impact Central Nervous System Autoimmunity via the Small Intestine. Immunity 2015, 43, 817–829. [Google Scholar] [CrossRef] [PubMed]
- Hollingsworth, K.G.; Jones, D.E.J.; Taylor, R.; Frith, J.; Blamire, A.M.; Newton, J.L. Impaired cerebral autoregulation in primary biliary cirrhosis: Implications for the pathogenesis of cognitive decline. Liver Int. 2010, 30, 878–885. [Google Scholar] [CrossRef]
- McDonald, C.; Newton, J.; Lai, H.M.; Baker, S.N.; Jones, D.E. Central nervous system dysfunction in primary biliary cirrhosis and its relationship to symptoms. J. Hepatol. 2010, 53, 1095–1100. [Google Scholar] [CrossRef]
- Newton, J.L.; Hollingsworth, K.G.; Taylor, R.; El-Sharkawy, A.M.; Khan, Z.U.; Pearce, R.; Sutcliffe, K.; Okonkwo, O.; Davidson, A.; Burt, J.; et al. Cognitive impairment in primary biliary cirrhosis: Symptom impact and potential etiology. Hepatology 2008, 48, 541–549. [Google Scholar] [CrossRef]
- Sanmarco, L.M.; Wheeler, M.A.; Gutiérrez-Vázquez, C.; Polonio, C.M.; Linnerbauer, M.; Pinho-Ribeiro, F.A.; Li, Z.; Giovannoni, F.; Batterman, K.V.; Scalisi, G.; et al. Gut-licensed IFNγ+ NK cells drive LAMP1+TRAIL+ anti-inflammatory astrocytes. Nature 2021, 590, 473–479. [Google Scholar] [CrossRef]
- Nguyen, H.H.; Swain, M.G. Avenues within the gut-liver-brain axis linking chronic liver disease and symptoms. Front. Neurosci. 2023, 17, 1171253. [Google Scholar] [CrossRef] [PubMed]
- Matsubara, Y.; Kiyohara, H.; Teratani, T.; Mikami, Y.; Kanai, T. Organ and brain crosstalk: The liver-brain axis in gastrointestinal, liver, and pancreatic diseases. Neuropharmacology 2022, 205, 108915. [Google Scholar] [CrossRef] [PubMed]
- Teratani, T.; Mikami, Y.; Nakamoto, N.; Suzuki, T.; Harada, Y.; Okabayashi, K.; Hagihara, Y.; Taniki, N.; Kohno, K.; Shibata, S.; et al. The liver–brain–gut neural arc maintains the Treg cell niche in the gut. Nature 2020, 585, 591–596. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Environmental Health Sciences. Perfluoroalkyl and Polyfluoroalkyl Substances (PFAS). Available online: https://www.niehs.nih.gov/health/topics/agents/pfc/index.cfm#:~:text=PFAS%20are%20a%20group%20of,the%20U.S.%20Environmental%20Protection%20Agency (accessed on 1 July 2023).
- Pelch, K.E.; Reade, A.; Wolffe, T.A.; Kwiatkowski, C.F. PFAS health effects database: Protocol for a systematic evidence map. Environ. Int. 2019, 130, 104851. [Google Scholar] [CrossRef] [PubMed]
- Domingo, J.L.; Nadal, M. Human exposure to per- and polyfluoroalkyl substances (PFAS) through drinking water: A review of the recent scientific literature. Environ. Res. 2019, 177, 108648. [Google Scholar] [CrossRef] [PubMed]
- ATSDR. PFAS in the U.S. Population. Agency for Toxic Substances and Disease Registry; Per- and Polyfluoroalkyl Substances (PFAS) and Your Health. 2022. Available online: https://www.atsdr.cdc.gov/pfas/health-effects/us-population.html (accessed on 9 August 2023).
- Sen, P.; Qadri, S.; Luukkonen, P.K.; Ragnarsdottir, O.; McGlinchey, A.; Jäntti, S.; Juuti, A.; Arola, J.; Schlezinger, J.J.; Webster, T.F.; et al. Exposure to environmental contaminants is associated with altered hepatic lipid metabolism in non-alcoholic fatty liver disease. J. Hepatol. 2022, 76, 283–293. [Google Scholar] [CrossRef] [PubMed]
- Gallo, V.; Leonardi, G.; Genser, B.; Lopez-Espinosa, M.-J.; Frisbee, S.J.; Karlsson, L.; Ducatman, A.M.; Fletcher, T. Serum Perfluorooctanoate (PFOA) and Perfluorooctane Sulfonate (PFOS) Concentrations and Liver Function Biomarkers in a Population with Elevated PFOA Exposure. Environ. Health Perspect. 2012, 120, 655–660. [Google Scholar] [CrossRef]
- Borghese, M.M.; Liang, C.L.; Owen, J.; Fisher, M. Individual and mixture associations of perfluoroalkyl substances on liver function biomarkers in the Canadian Health Measures Survey. Environ. Health 2022, 21, 85. [Google Scholar] [CrossRef]
- Jain, R.B.; Ducatman, A. Selective associations of recent low concentrations of perfluoroalkyl substances with liver function biomarkers: NHANES 2011 to 2014 data on US adults aged ≥ 20 years. J. Occup. Environ. Med. 2019, 6, 293–302. [Google Scholar] [CrossRef]
- Costello, E.; Rock, S.; Stratakis, N.; Eckel, S.P.; Walker, D.I.; Valvi, D.; Cserbik, D.; Jenkins, T.; Xanthakos, S.A.; Kohli, R.; et al. Exposure to per- and Polyfluoroalkyl Substances and Markers of Liver Injury: A Systematic Review and Meta-Analysis. Environ. Health Perspect. 2022, 130, 46001. [Google Scholar] [CrossRef]
- Elcombe, C.R.; Elcombe, B.M.; Foster, J.R.; Chang, S.-C.; Ehresman, D.J.; Butenhoff, J.L. Hepatocellular hypertrophy and cell proliferation in Sprague–Dawley rats from dietary exposure to potassium perfluorooctanesulfonate results from increased expression of xenosensor nuclear receptors PPARα and CAR/PXR. Toxicology 2012, 293, 16–29. [Google Scholar] [CrossRef] [PubMed]
- Qi, Q.; Niture, S.; Gadi, S.; Arthur, E.; Moore, J.; Levine, K.E.; Kumar, D. Per-and polyfluoroalkyl substances activate UPR pathway, induce steatosis and fibrosis in liver cells. Environ. Toxicol. 2023, 38, 225–242. [Google Scholar] [CrossRef] [PubMed]
- De Toni, L.; Di Nisio, A.; Rocca, M.S.; Guidolin, D.; Della Marina, A.; Bertazza, L.; Sut, S.; Purpura, E.; Pannella, M.; Garolla, A.; et al. Exposure to Perfluoro-Octanoic Acid Associated with Upstream Uncoupling of the Insulin Signaling in Human Hepatocyte Cell Line. Front. Endocrinol. 2021, 12, 632927. [Google Scholar] [CrossRef] [PubMed]
- Jin, R.; McConnell, R.; Catherine, C.; Xu, S.; Walker, D.I.; Stratakis, N.; Jones, D.P.; Miller, G.W.; Peng, C.; Conti, D.V.; et al. Perfluoroalkyl substances and severity of nonalcoholic fatty liver in Children: An untargeted metabolomics approach. Environ. Int. 2019, 134, 105220. [Google Scholar] [CrossRef]
- Ojo, A.F.; Xia, Q.; Peng, C.; Ng, J.C. Evaluation of the individual and combined toxicity of perfluoroalkyl substances to human liver cells using biomarkers of oxidative stress. Chemosphere 2021, 281, 130808. [Google Scholar] [CrossRef]
- Skogheim, T.S.; Weyde, K.V.F.; Aase, H.; Engel, S.M.; Surén, P.; Øie, M.G.; Biele, G.; Reichborn-Kjennerud, T.; Brantsæter, A.L.; Haug, L.S.; et al. Prenatal exposure to per- and polyfluoroalkyl substances (PFAS) and associations with attention-deficit/hyperactivity disorder and autism spectrum disorder in children. Environ. Res. 2021, 202, 111692. [Google Scholar] [CrossRef]
- Zodrow, J.; Vedagiri, U.; Sorell, T.; McIntosh, L.; Larson, E.; Hall, L.; Dourson, M.; Dell, L.; Cox, D.; Barfoot, K.; et al. PFAS Experts Symposium 2: PFAS Toxicology and Risk Assessment in 2021—Contemporary issues in human and ecological risk assessment of PFAS. Remediat. J. 2022, 32, 29–44. [Google Scholar] [CrossRef]
- Albajara Sáenz, A.; Septier, M.; Van Schuerbeek, P.; Baijot, S.; Deconinck, N.; Defresne, P.; Delvenne, V.; Passeri, G.; Raeymaekers, H.; Salvesen, L.; et al. ADHD and ASD: Distinct brain patterns of inhibition-related activation? Transl. Psychiatry 2020, 10, 203–215. [Google Scholar] [CrossRef]
- Cao, Y.; Ng, C. Absorption, distribution, and toxicity of per-and polyfluoroalkyl substances (PFAS) in the brain: A review. Environ. Sci. Process. Impacts 2021, 23, 1623–1640. [Google Scholar] [CrossRef]
- Liu, X.; Jin, Y.; Liu, W.; Wang, F.; Hao, S. Possible mechanism of perfluorooctane sulfonate and perfluorooctanoate on the release of calcium ion from calcium stores in primary cultures of rat hippocampal neurons. Toxicol. Vitr. 2011, 25, 1294–1301. [Google Scholar] [CrossRef]
- Liu, X.; Liu, W.; Jin, Y.; Yu, W.; Liu, L.; Yu, H. Effects of subchronic perfluorooctane sulfonate exposure of rats on calcium-dependent signaling molecules in the brain tissue. Arch. Toxicol. 2010, 84, 471–479. [Google Scholar] [CrossRef] [PubMed]
- Brown-Leung, J.M.; Cannon, J.R. Neurotransmission Targets of Per- and Polyfluoroalkyl Substance Neurotoxicity: Mechanisms and Potential Implications for Adverse Neurological Outcomes. Chem. Res. Toxicol. 2022, 35, 1312–1333. [Google Scholar] [CrossRef] [PubMed]
- Foguth, R.M.; Flynn, R.W.; de Perre, C.; Iacchetta, M.; Lee, L.S.; Sepúlveda, M.S.; Cannon, J.R. Developmental exposure to perfluorooctane sulfonate (PFOS) and perfluorooctanoic acid (PFOA) selectively decreases brain dopamine levels in Northern leopard frogs. Toxicol. Appl. Pharmacol. 2019, 377, 114623. [Google Scholar] [CrossRef] [PubMed]
- Hallgren, S.; Viberg, H. Postnatal exposure to PFOS, but not PBDE 99, disturb dopaminergic gene transcription in the mouse CNS. Environ. Toxicol. Pharmacol. 2016, 41, 121–126. [Google Scholar] [CrossRef] [PubMed]
- Salgado, R.; López-Doval, S.; Pereiro, N.; Lafuente, A. Perfluorooctane sulfonate (PFOS) exposure could modify the dopaminergic system in several limbic brain regions. Toxicol. Lett. 2016, 240, 226–235. [Google Scholar] [CrossRef] [PubMed]
- Yu, N.; Wei, S.; Li, M.; Yang, J.; Li, K.; Jin, L.; Xie, Y.; Giesy, J.P.; Zhang, X.; Yu, H. Effects of Perfluorooctanoic Acid on Metabolic Profiles in Brain and Liver of Mouse Revealed by a High-throughput Targeted Metabolomics Approach. Sci. Rep. 2016, 6, 23963. [Google Scholar] [CrossRef] [PubMed]
- Long, Y.; Wang, Y.; Ji, G.; Yan, L.; Hu, F.; Gu, A. Neurotoxicity of Perfluorooctane Sulfonate to Hippocampal Cells in Adult Mice. PLoS ONE 2013, 8, e54176. [Google Scholar] [CrossRef]
- Johansson, N.; Fredriksson, A.; Eriksson, P. Neonatal exposure to perfluorooctane sulfonate (PFOS) and perfluorooctanoic acid (PFOA) causes neurobehavioural defects in adult mice. NeuroToxicology 2008, 29, 160–169. [Google Scholar] [CrossRef]
- Johnson, A.M.; Ou, Z.-Y.A.; Gordon, R.; Saminathan, H. Environmental neurotoxicants and inflammasome activation in Parkinson’s disease—A focus on the gut-brain axis. Int. J. Biochem. Cell Biol. 2022, 142, 106113. [Google Scholar] [CrossRef]
- Patel, R.; Bradner, J.M.; Stout, K.A.; Caudle, W.M. Alteration to Dopaminergic Synapses Following Exposure to Perfluorooctane Sulfonate (PFOS), in Vitro and in Vivo. Med. Sci. 2016, 4, 13. [Google Scholar] [CrossRef]
- Mastrantonio, M.; Bai, E.; Uccelli, R.; Cordiano, V.; Screpanti, A.; Crosignani, P. Drinking water contamination from perfluoroalkyl substances (PFAS): An ecological mortality study in the Veneto Region, Italy. Eur. J. Public Health 2018, 28, 180–185. [Google Scholar] [CrossRef] [PubMed]
- Luo, J.; Ramlau-Hansen, C.H.; Kesmodel, U.S.; Xiao, J.; Vasiliou, V.; Deziel, N.C.; Zhang, Y.; Olsen, J.; Liew, Z. Prenatal exposure to per-and polyfluoroalkyl substances and facial features at 5 years old. Environ. Health Perspect. 2022, 130, 17006. [Google Scholar] [CrossRef] [PubMed]
- Tillman, K.K.; Hakelius, M.; Höijer, J.; Ramklint, M.; Ekselius, L.; Nowinski, D.; Papadopoulos, F.C. Increased Risk for Neurodevelopmental Disorders in Children With Orofacial Clefts. J. Am. Acad. Child Adolesc. Psychiatry 2018, 57, 876–883. [Google Scholar] [CrossRef] [PubMed]
- Jandhyala, S.M.; Talukdar, R.; Subramanyam, C.; Vuyyuru, H.; Sasikala, M.; Reddy, D.N. Role of the normal gut microbiota. World J. Gastroenterol. WJG 2015, 21, 8787. [Google Scholar] [CrossRef] [PubMed]
- Gardner, C.M.; Hoffman, K.; Stapleton, H.M.; Gunsch, C.K. Exposures to Semivolatile Organic Compounds in Indoor Environments and Associations with the Gut Microbiomes of Children. Environ. Sci. Technol. Lett. 2020, 8, 73–79. [Google Scholar] [CrossRef]
- Iszatt, N.; Janssen, S.; Lenters, V.; Dahl, C.; Stigum, H.; Knight, R.; Mandal, S.; Peddada, S.; González, A.; Midtvedt, T.; et al. Environmental toxicants in breast milk of Norwegian mothers and gut bacteria composition and metabolites in their infants at 1 month. Microbiome 2019, 7, 34. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Wang, L.; Zhang, X.; Liu, P.; Deji, Z.; Xing, Y.; Zhou, Y.; Lin, X.; Huang, Z. Per- and polyfluoroalkyl substances exposure and its influence on the intestinal barrier: An overview on the advances. Sci. Total. Environ. 2022, 852, 158362. [Google Scholar] [CrossRef]
- Naspolini, N.F.; Meyer, A.; Moreira, J.C.; Sun, H.; Froes-Asmus, C.I.; Dominguez-Bello, M.G. Environmental pollutant exposure associated with altered early-life gut microbiome: Results from a birth cohort study. Environ. Res. 2021, 205, 112545. [Google Scholar] [CrossRef]
- Rashid, F.; Dubinkina, V.; Ahmad, S.; Maslov, S.; Irudayaraj, J.M.K. Gut Microbiome-Host Metabolome Homeostasis upon Exposure to PFOS and GenX in Male Mice. Toxics 2023, 11, 281. [Google Scholar] [CrossRef]
- Thompson, K.N.; Oulhote, Y.; Weihe, P.; Wilkinson, J.E.; Ma, S.; Zhong, H.; Li, J.; Kristiansen, K.; Huttenhower, C.; Grandjean, P. Effects of Lifetime Exposures to Environmental Contaminants on the Adult Gut Microbiome. Environ. Sci. Technol. 2022, 56, 16985–16995. [Google Scholar] [CrossRef]
- Zhang, L.; Rimal, B.; Nichols, R.G.; Tian, Y.; Smith, P.B.; Hatzakis, E.; Chang, S.-C.; Butenhoff, J.L.; Peters, J.M.; Patterson, A.D. Perfluorooctane sulfonate alters gut microbiota-host metabolic homeostasis in mice. Toxicology 2020, 431, 152365. [Google Scholar] [CrossRef] [PubMed]
- Shi, L.; Zheng, J.; Yan, S.; Li, Y.; Wang, Y.; Liu, X.; Xiao, C. Exposure to Perfluorooctanoic Acid Induces Cognitive Deficits via Altering Gut Microbiota Composition, Impairing Intestinal Barrier Integrity, and Causing Inflammation in Gut and Brain. J. Agric. Food Chem. 2020, 68, 13916–13928. [Google Scholar] [CrossRef] [PubMed]
- Yu, G.; Luo, F.; Nian, M.; Li, S.; Liu, B.; Feng, L.; Zhang, J. Exposure to Perfluoroalkyl Substances During Pregnancy and Fetal BDNF Level: A Prospective Cohort Study. Front. Endocrinol. 2021, 12, 653095. [Google Scholar] [CrossRef] [PubMed]
- National Library of Medicine, MedlinePlus. Acetaminophen. Available online: https://medlineplus.gov/druginfo/meds/a681004.html (accessed on 9 August 2023).
- Good, P. Evidence the U.S. autism epidemic initiated by acetaminophen (Tylenol) is aggravated by oral antibiotic amoxicillin/clavulanate (Augmentin) and now exponentially by herbicide glyphosate (Roundup). Clin. Nutr. ESPEN 2018, 23, 171–183. [Google Scholar] [CrossRef] [PubMed]
- Schultz, S.T.; Klonoff-Cohen, H.S.; Wingard, D.L.; A Akshoomoff, N.; A Macera, C.; Ji, M.; Bacher, C. Breastfeeding, infant formula supplementation, and Autistic Disorder: The results of a parent survey. Int. Breastfeed. J. 2006, 1, 16. [Google Scholar] [CrossRef] [PubMed]
- Von Ehrenstein, O.S.; Ling, C.; Cui, X.; Cockburn, M.; Park, A.S.; Yu, F.; Wu, J.; Ritz, B. Prenatal and infant exposure to ambient pesticides and autism spectrum disorder in children: Population based case-control study. BMJ 2019, 364, l962. [Google Scholar] [CrossRef]
- Hinson, J.A.; Roberts, D.W.; James, L.P. Mechanisms of Acetaminophen-Induced Liver Necrosis. Advers. Drug React. 2010, 196, 369–405. [Google Scholar] [CrossRef]
- Bajt, M.L.; Knight, T.R.; Lemasters, J.J.; Jaeschke, H. Acetaminophen-Induced Oxidant Stress and Cell Injury in Cultured Mouse Hepatocytes: Protection by N-Acetyl Cysteine. Toxicol. Sci. 2004, 80, 343–349. [Google Scholar] [CrossRef]
- Cover, C.; Mansouri, A.; Knight, T.R.; Bajt, M.L.; Lemasters, J.J.; Pessayre, D.; Jaeschke, H. Peroxynitrite-Induced Mitochondrial and Endonuclease-Mediated Nuclear DNA Damage in Acetaminophen Hepatotoxicity. J. Pharmacol. Exp. Ther. 2005, 315, 879–887. [Google Scholar] [CrossRef]
- Ghanem, C.I.; Pérez, M.J.; Manautou, J.E.; Mottino, A.D. Acetaminophen from liver to brain: New insights into drug pharmacological action and toxicity. Pharmacol. Res. 2016, 109, 119–131. [Google Scholar] [CrossRef]
- Masarwa, R.; Levine, H.; Gorelik, E.; Reif, S.; Perlman, A.; Matok, I. Prenatal Exposure to Acetaminophen and Risk for Attention Deficit Hyperactivity Disorder and Autistic Spectrum Disorder: A Systematic Review, Meta-Analysis, and Meta-Regression Analysis of Cohort Studies. Am. J. Epidemiol. 2018, 187, 1817–1827. [Google Scholar] [CrossRef] [PubMed]
- Posadas, I.; Santos, P.; Blanco, A.; Muñoz-Fernández, M.; Ceña, V. Acetaminophen Induces Apoptosis in Rat Cortical Neurons. PLoS ONE 2010, 5, e15360. [Google Scholar] [CrossRef] [PubMed]
- Kristensen, D.M.; Lesné, L.; Le Fol, V.; Desdoits-Lethimonier, C.; Dejucq-Rainsford, N.; Leffers, H.; Jégou, B. Paracetamol (acetaminophen), aspirin (acetylsalicylic acid) and indomethacin are anti-androgenic in the rat foetal testis. Int. J. Androl. 2012, 35, 377–384. [Google Scholar] [CrossRef] [PubMed]
- Nazıroğlu, M.; Uğuz, A.C.; Koçak, A.; Bal, R. Acetaminophen at Different Doses Protects Brain Microsomal Ca2+-ATPase and the Antioxidant Redox System in Rats. J. Membr. Biol. 2009, 231, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Bisaglia, M.; Venezia, V.; Piccioli, P.; Stanzione, S.; Porcile, C.; Russo, C.; Mancini, F.; Milanese, C.; Schettini, G. Acetaminophen protects hippocampal neurons and PC12 cultures from amyloid β-peptides induced oxidative stress and reduces NF-κB activation. Neurochem. Int. 2002, 41, 43–54. [Google Scholar] [CrossRef] [PubMed]
- Hadzimichalis, N.M.; Baliga, S.S.; Golfetti, R.; Jaques, K.M.; Firestein, B.L.; Merrill, G.F. Acetaminophen-mediated cardioprotection via inhibition of the mitochondrial permeability transition pore-induced apoptotic pathway. Am. J. Physiol. Circ. Physiol. 2007, 293, H3348–H3355. [Google Scholar] [CrossRef] [PubMed]
- Maharaj, H.; Maharaj, D.S.; Saravanan, K.S.; Mohanakumar, K.P.; Daya, S. Aspirin Curtails the Acetaminophen-Induced Rise in Brain Norepinephrine Levels. Metab. Brain Dis. 2004, 19, 71–77. [Google Scholar] [CrossRef]
- Maharaj, H.; Maharaj, D.S.; Daya, S. Acetylsalicylic acid and acetaminophen protect against oxidative neurotoxicity. Metab. Brain Dis. 2006, 21, 180–190. [Google Scholar] [CrossRef]
- Malfatti, M.A.; Kuhn, E.A.; Murugesh, D.K.; Mendez, M.E.; Hum, N.; Thissen, J.B.; Jaing, C.J.; Loots, G.G. Manipulation of the Gut Microbiome Alters Acetaminophen Biodisposition in Mice. Sci. Rep. 2020, 10, 4571. [Google Scholar] [CrossRef]
- Laue, H.E.; Shen, Y.; Bloomquist, T.R.; Wu, H.; Brennan, K.J.M.; Cassoulet, R.; Wilkie, E.; Gillet, V.; Desautels, A.-S.; Abdelouahab, N.; et al. In Utero Exposure to Caffeine and Acetaminophen, the Gut Microbiome, and Neurodevelopmental Outcomes: A Prospective Birth Cohort Study. Int. J. Environ. Res. Public Health 2022, 19, 9357. [Google Scholar] [CrossRef]
- Haws, S.A.; Yu, D.; Ye, C.; Wille, C.K.; Nguyen, L.C.; Krautkramer, K.A.; Tomasiewicz, J.L.; Yang, S.E.; Miller, B.R.; Liu, W.H.; et al. Methyl-Metabolite Depletion Elicits Adaptive Responses to Support Heterochromatin Stability and Epigenetic Persistence. Mol. Cell 2020, 78, 210–223.e8. [Google Scholar] [CrossRef] [PubMed]
- Lalert, L.; Tantarungsee, N.; Chotipinit, T.; Ji-Au, W.; Srikiatkhachorn, A.; Grand, S.M.-L. Long-Term Paracetamol Treatment Impairs Cognitive Function and Brain-Derived Neurotrophic Factor in Adult Rat Brain. Sci. Pharm. 2023, 91, 11. [Google Scholar] [CrossRef]
- Trinchese, G.; Cimmino, F.; Cavaliere, G.; Catapano, A.; Fogliano, C.; Lama, A.; Pirozzi, C.; Cristiano, C.; Russo, R.; Petrella, L.; et al. The Hepatic Mitochondrial Alterations Exacerbate Meta-Inflammation in Autism Spectrum Disorders. Antioxidants 2022, 11, 1990. [Google Scholar] [CrossRef] [PubMed]
| Organism | Sample Type | Sample Size | Age | Sex | Reagents | Exposure Dose | Exposure Time | Outcome | References |
|---|---|---|---|---|---|---|---|---|---|
| Mice | Liver cells | Not indicated | Not indicated | M | APAP | 5 mM | 0 to 12 h | ↓ Mitochondria function ↑ ROS production ↑ Glutathuone disulfide (GSSG) | [123] |
| Mice | Plasma, blood, and liver | 5 groups of 4–6 | Not indicated | M | APAP | 300 mg/kg | 12 h | ↑ Peroxynitrite in mitochondria ↑ Liver tissue necrosis | [124] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jiang, D.Q.Y.; Guo, T.L. Interaction between Per- and Polyfluorinated Substances (PFAS) and Acetaminophen in Disease Exacerbation—Focusing on Autism and the Gut–Liver–Brain Axis. Toxics 2024, 12, 39. https://doi.org/10.3390/toxics12010039
Jiang DQY, Guo TL. Interaction between Per- and Polyfluorinated Substances (PFAS) and Acetaminophen in Disease Exacerbation—Focusing on Autism and the Gut–Liver–Brain Axis. Toxics. 2024; 12(1):39. https://doi.org/10.3390/toxics12010039
Chicago/Turabian StyleJiang, Danielle Qiu Yun, and Tai Liang Guo. 2024. "Interaction between Per- and Polyfluorinated Substances (PFAS) and Acetaminophen in Disease Exacerbation—Focusing on Autism and the Gut–Liver–Brain Axis" Toxics 12, no. 1: 39. https://doi.org/10.3390/toxics12010039
APA StyleJiang, D. Q. Y., & Guo, T. L. (2024). Interaction between Per- and Polyfluorinated Substances (PFAS) and Acetaminophen in Disease Exacerbation—Focusing on Autism and the Gut–Liver–Brain Axis. Toxics, 12(1), 39. https://doi.org/10.3390/toxics12010039








