Multi-Walled Carbon Nanotubes Accelerate Leukaemia Development in a Mouse Model
Abstract
1. Introduction
2. Materials and Methods
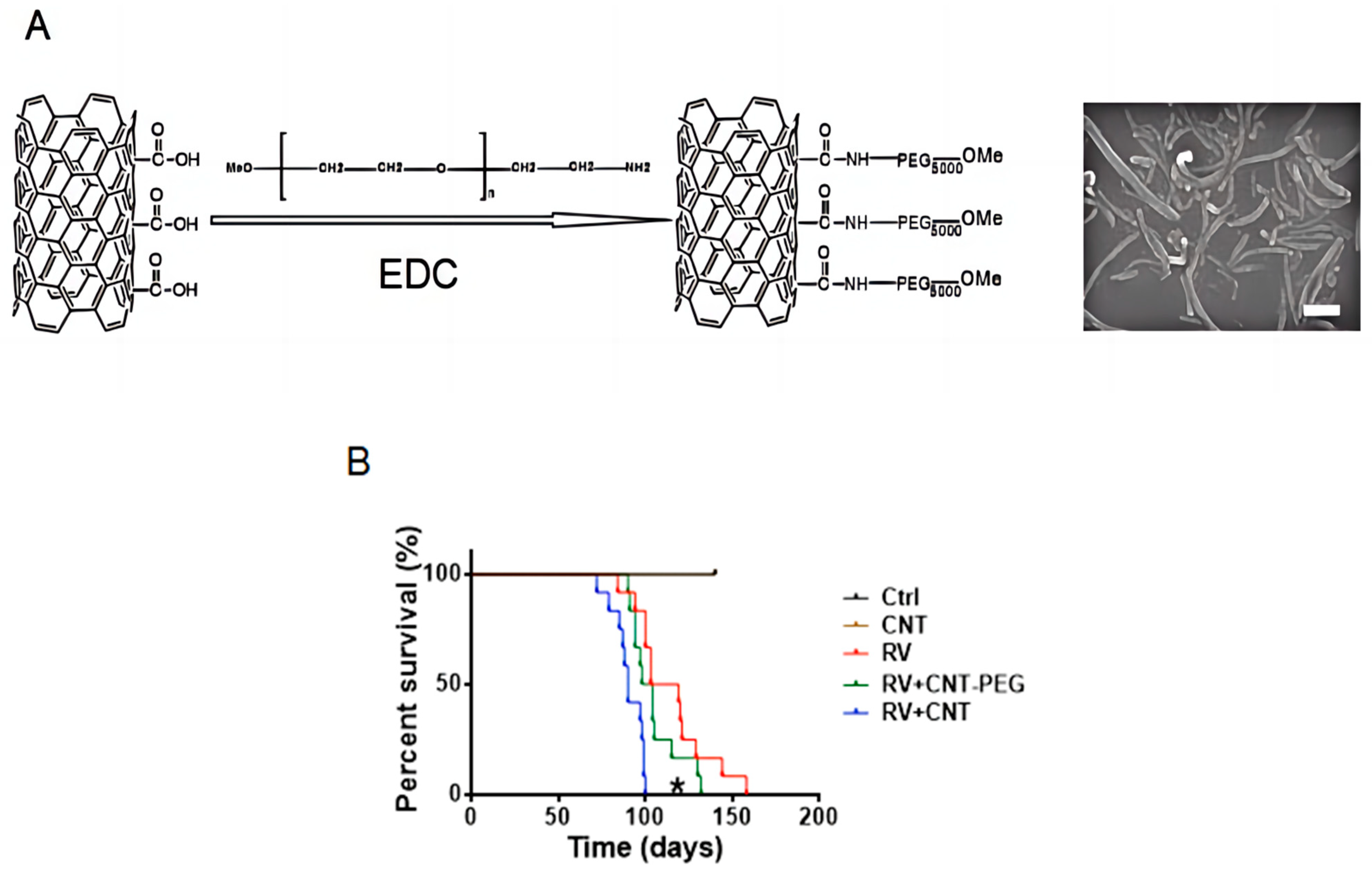
2.1. Preparation of Acidified MWCNTs and PEG-Modified MWCNTs
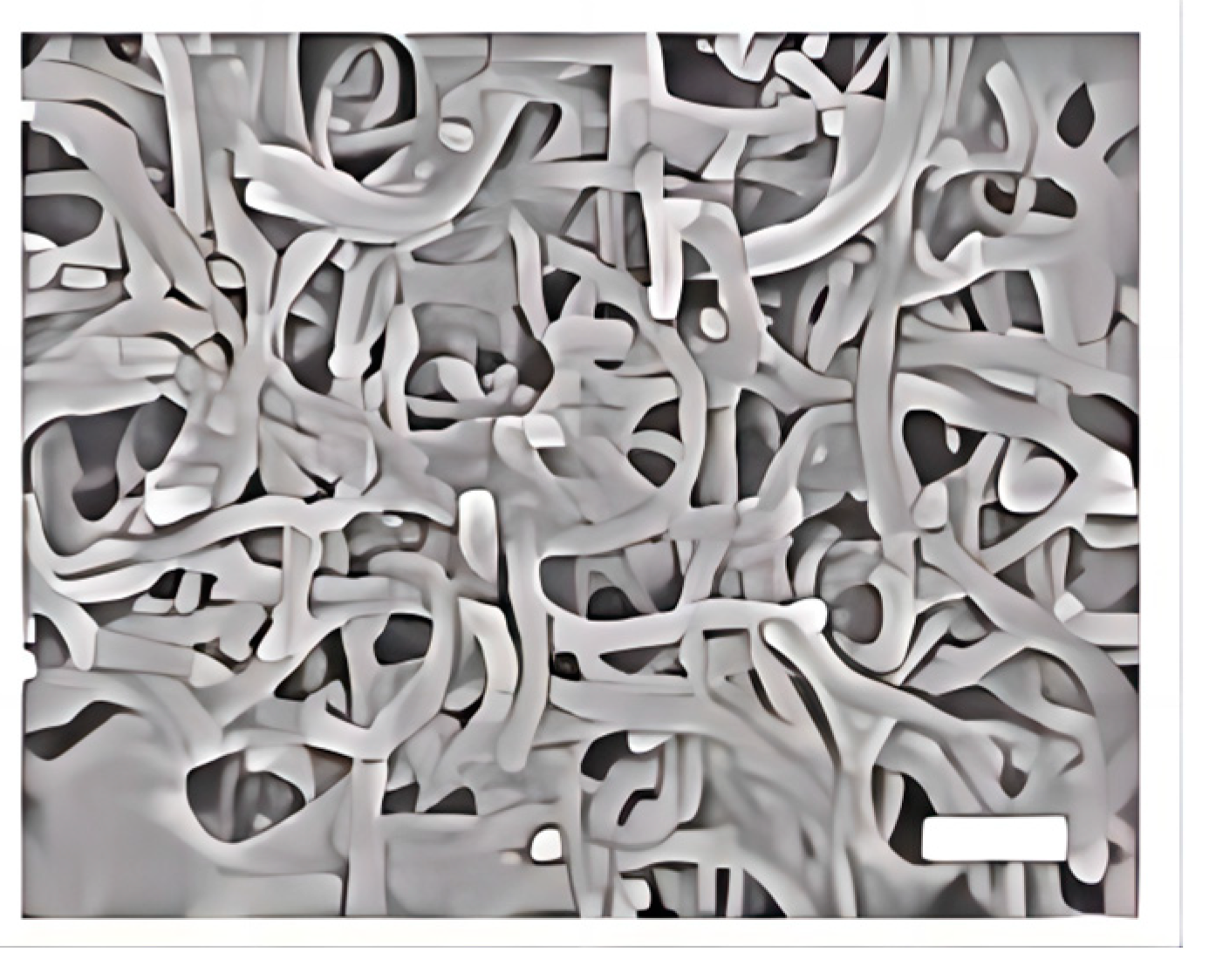
2.2. Scanning Electron Microscopy (SEM)
2.3. Cell Culture and Mice
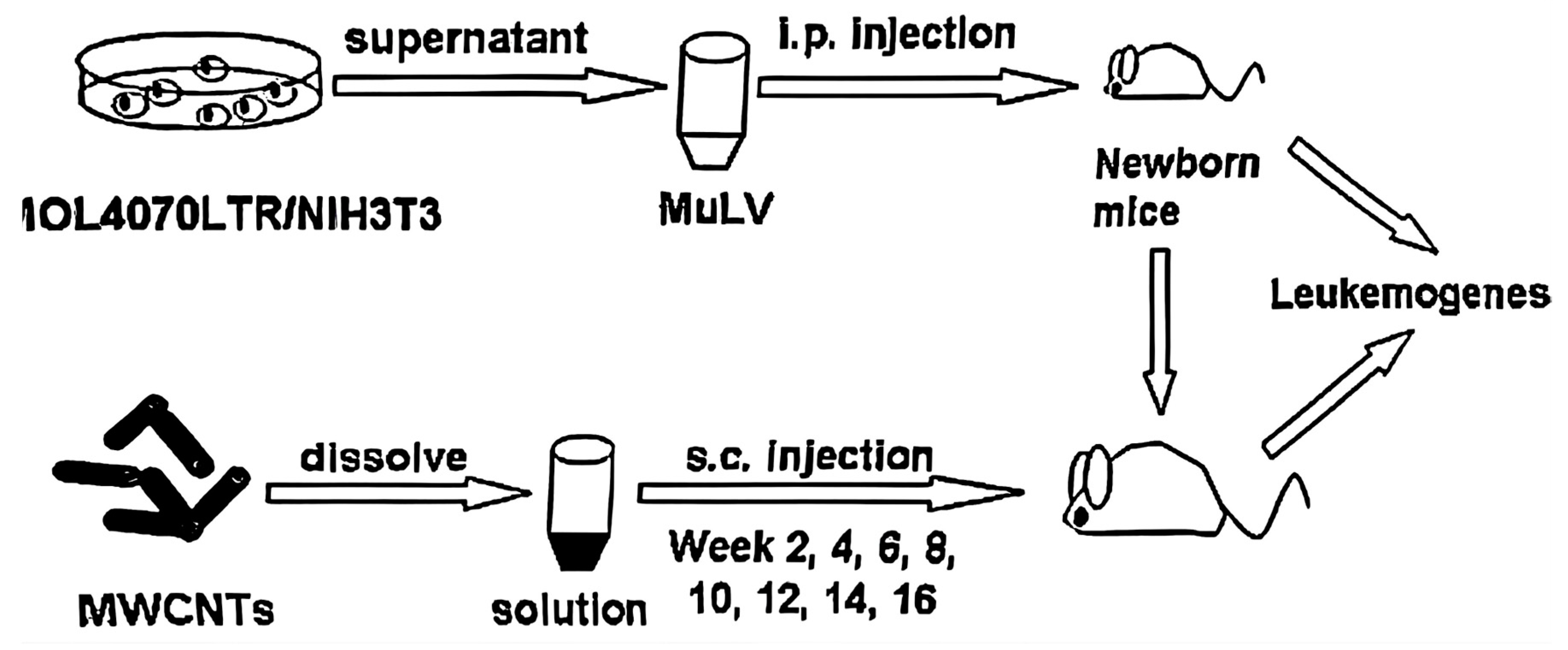
2.4. Murine Leukemia Virus (MuLV)-Induced Leukemia Mouse Model
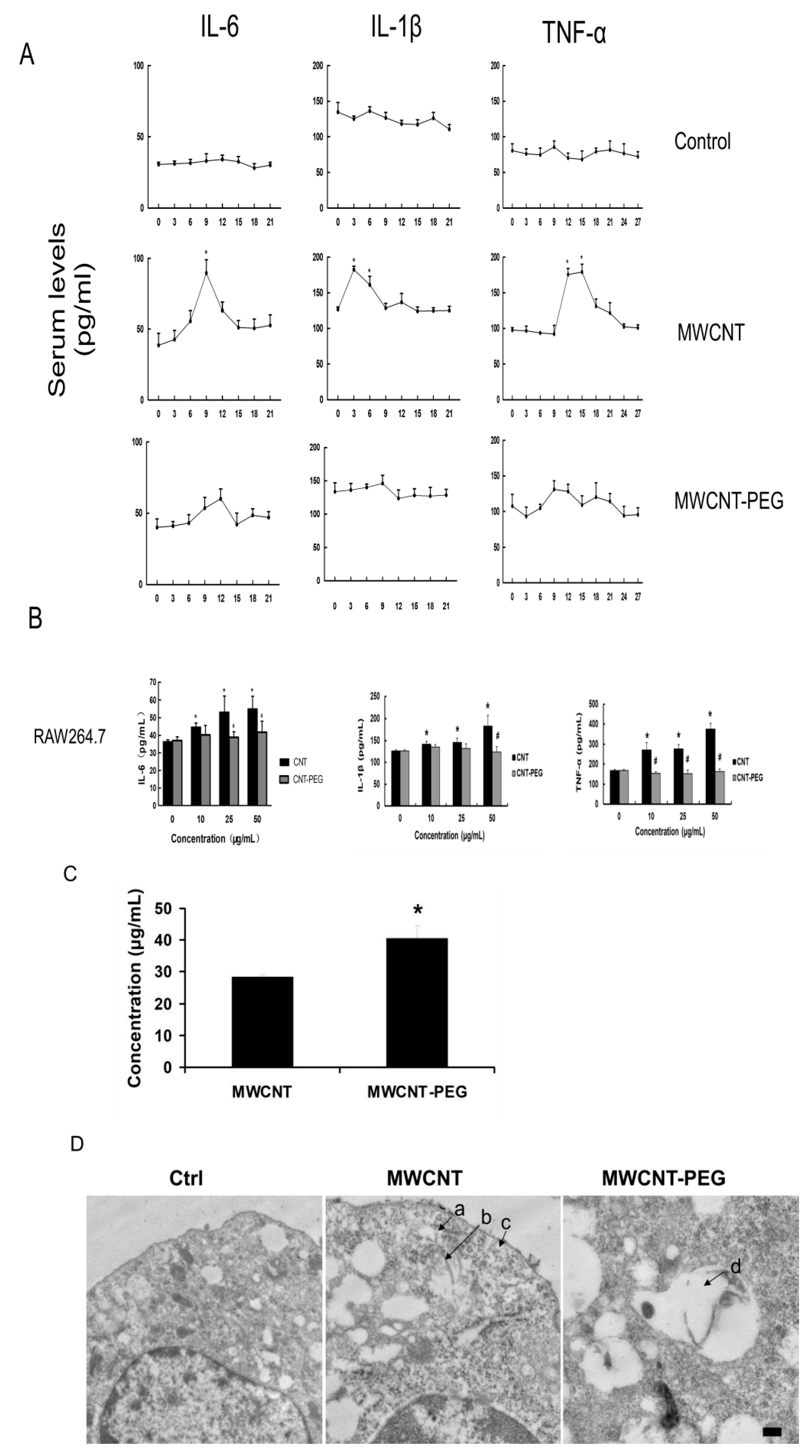
2.5. Detection of Pro-Inflammatory Cytokines by Enzyme-Linked Immunosorbent Assay (ELISA)
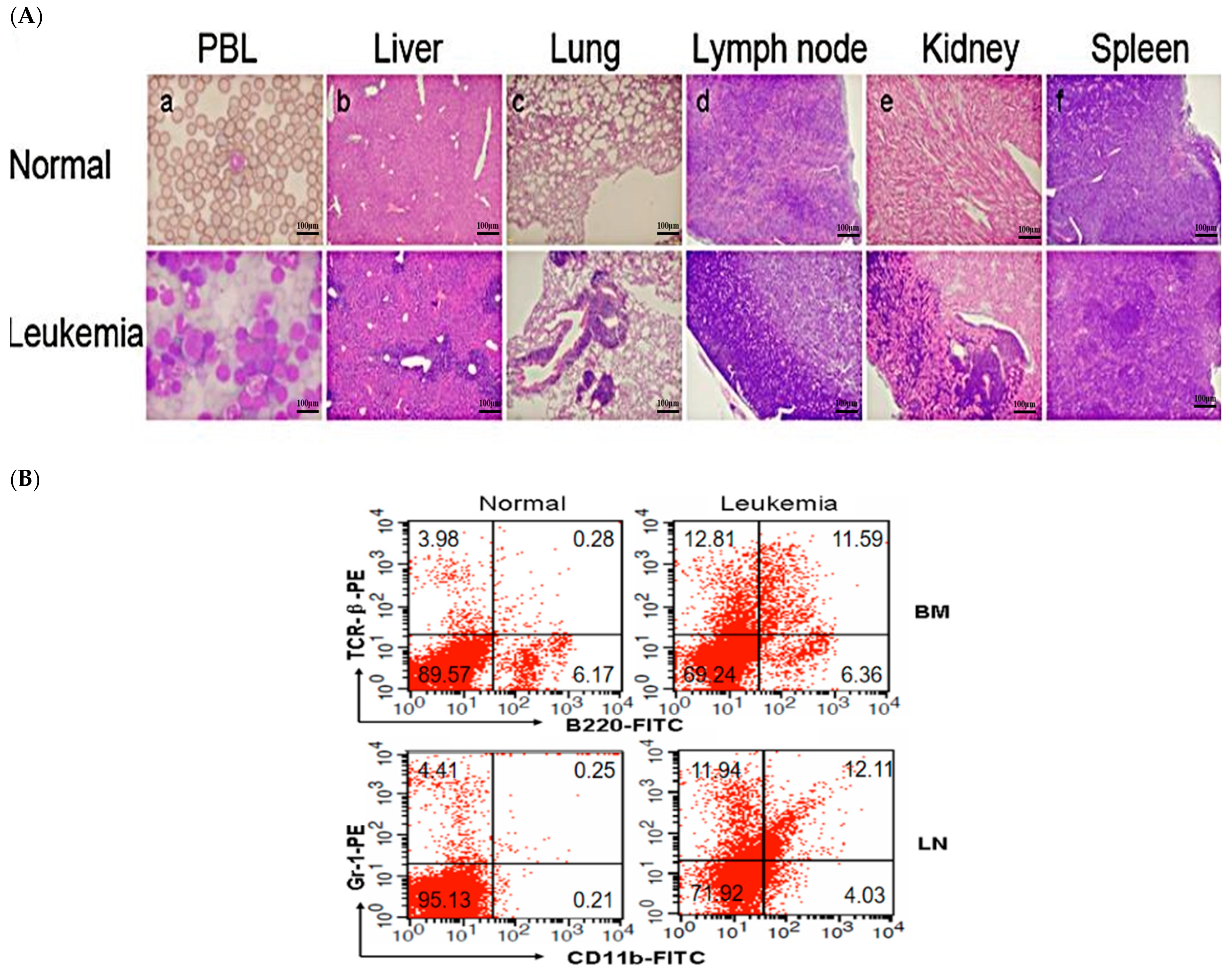
2.6. Histopathology
2.7. Uptake of MWCNTs and MWCNTs-PEG by Transmission Electron Microscopy (TEM) and Concentration Determinations
2.8. Flow Cytometry Analysis of Mouse Leukemic Cell Lineage
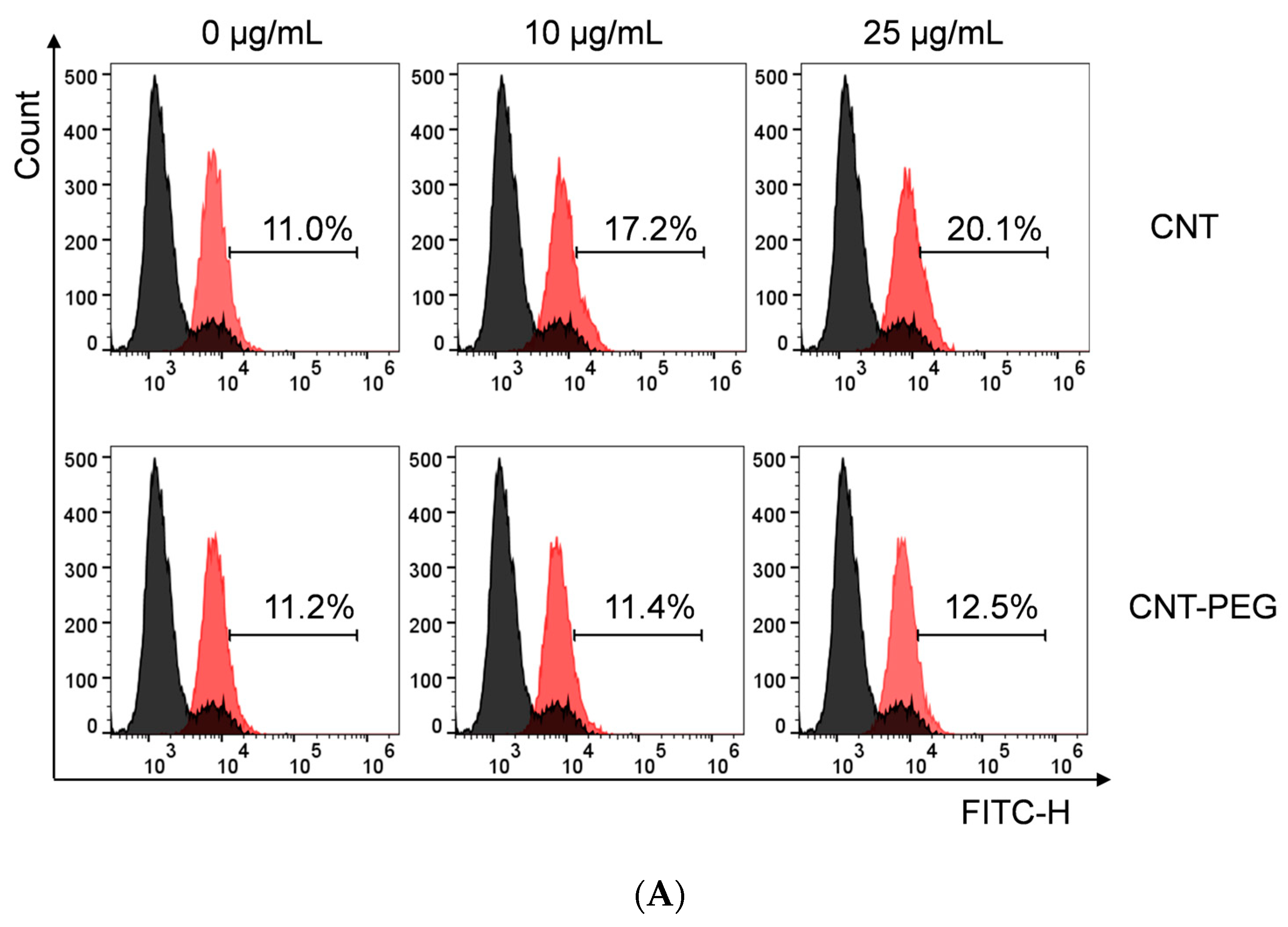
2.9. ROS Detection
2.10. Statistical Analyses
3. Results
3.1. Characterization of MWCNTs
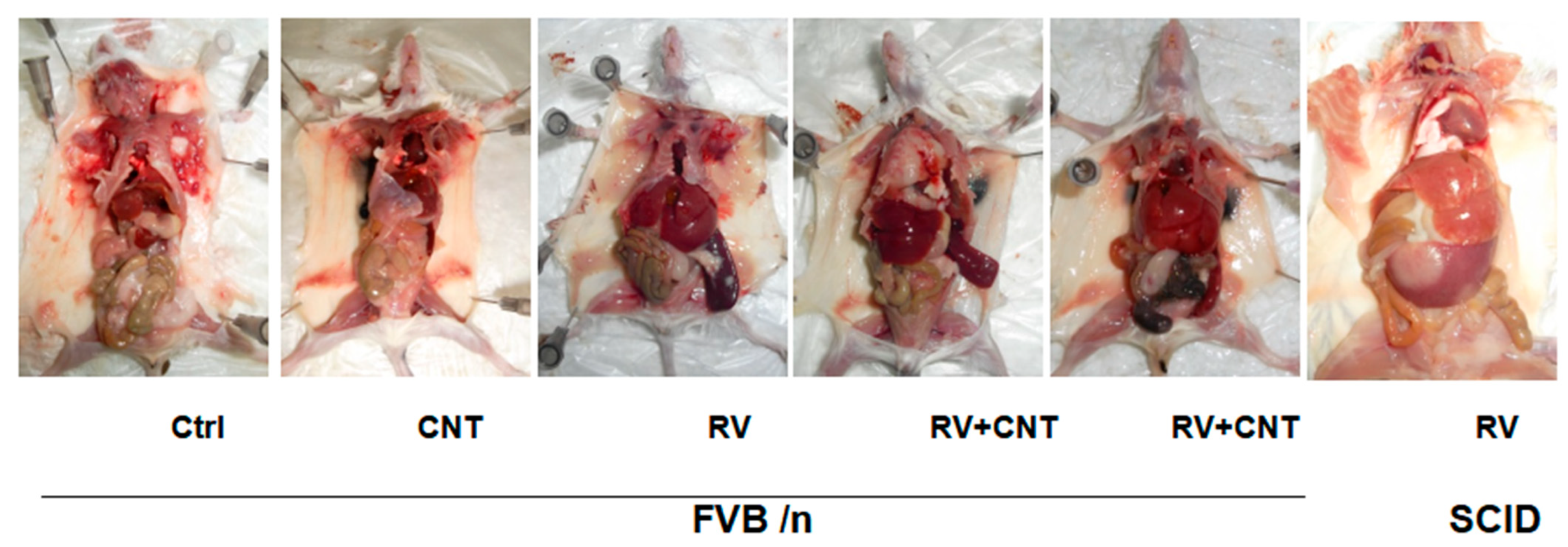
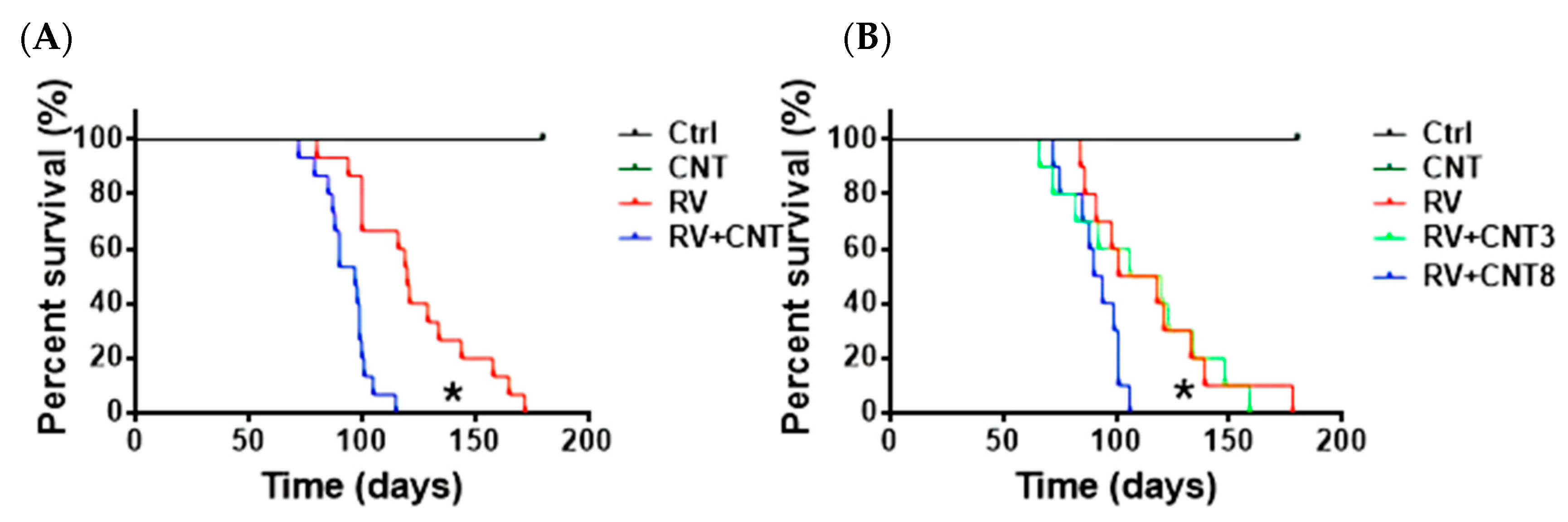
3.2. Mouse Model Data
3.3. Effect of PEG Modification of MWCNTs
3.4. Effects of MWCNTs in Immune Deficient Mice
3.5. Pro-Inflammatory Cytokines in Mice Exposed to MWCNTs
3.6. Effects of MWCNTs on Macrophages
3.7. ROS Levels
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yang, M.M.; Alexe, M. Sunlight harvested by nanotubes. Nature 2019, 570, 310–311. [Google Scholar] [CrossRef]
- Tunuguntla, R.H.; Henley, R.Y.; Yao, Y.C.; Pham, T.A.; Wanunu, M.; Noy, A. Enhanced water permeability and tunable ion selectivity in subnanometer carbon nanotube porins. Science 2017, 357, 792–796. [Google Scholar] [CrossRef] [PubMed]
- Shi, H.K.; Carter, S.; Haines, N.L. Harvesting electrical energy from carbon nanotube yarn twist. Science 2017, 357, 773–778. [Google Scholar]
- De Volder, M.F.; Tawfick, S.H.; Baughman, R.H.; Hart, A.J. Carbon Nanotubes: Present and Future Commercial Applications. Science 2013, 339, 535–539. [Google Scholar] [CrossRef]
- Lima, M.D.; Li, N.; Jung de Andrade, M.; Fang, S.; Oh, J.; Spinks, G.M.; Kozlov, M.E.; Haines, C.S.; Suh, D.; Foroughi, J.; et al. Electrically, Chemically, and Photonically Powered Torsional and Tensile Actuation of Hybrid Carbon Nanotube Yarn Muscles. Science 2012, 338, 928–932. [Google Scholar] [CrossRef]
- Balani, K.; Anderson, R.; Laha, T. Plasma-sprayed carbon nanotube reinforced hydroxyapatite coatings and their interaction with human osteoblasts in vitro. Biomaterials 2007, 28, 618–624. [Google Scholar] [CrossRef]
- Kam, N.W.S.; Jessop, T.C.; Wender, P.A.; Dai, H. Nanotube molecular transporters: Internalization of carbon nanotube-protein conjugates into Mammalian cells. J. Am. Chem. Soc. 2004, 126, 6850–6851. [Google Scholar] [CrossRef]
- Pan, B.; Cui, D.; Xu, P. Synthesis and characterization of polyamidoamine dendrimer-coated multi-walled carbon nanotubes and their application in gene delivery systems. Nanotechnology 2009, 20, 125101. [Google Scholar] [CrossRef] [PubMed]
- Kam, N.W.S.; Liu, Z.; Dai, H. Functionalization of carbon nanotubes via cleavable disulfide bonds for efficient intracellular delivery of siRNA and potent gene silencing. J. Am. Chem. Soc. 2005, 127, 12492–12493. [Google Scholar] [CrossRef]
- Gannon, C.J.; Cherukuri, P.; Yakobson, B.I.; Cognet, L.; Kanzius, J.S.; Kittrell, C.; Weisman, R.B.; Pasquali, M.; Schmidt, H.K.; Smalley, R.E.; et al. Carbon nanotube-enhanced thermal destruction of cancer cells in a noninvasive radiofrequency field. Cancer 2007, 110, 2654–2665. [Google Scholar] [CrossRef]
- Meng, J.; Duan, J.; Kong, H.; Li, L.; Wang, C.; Xie, S.; Chen, S.; Gu, N.; Xu, H.; Yang, X. Carbon nanotubes conjugated to tumor lysate protein enhance the efficacy of an antitumor immunotherapy. Small 2008, 4, 1364–1370. [Google Scholar] [CrossRef]
- Meng, J.; Yang, M.; Jia, F.; Kong, H.; Zhang, W.; Wang, C.; Xing, J.; Xie, S.; Xu, H. Subcutaneous injection of water-soluble multi-walled carbon nanotubes in tumor-bearing mice boosts the host immune activity. Nanotechnology 2010, 21, 145104. [Google Scholar] [CrossRef]
- Zhao, S.; Liu, Z.; Meng, J.; Duan, J.; Xie, S.; Lu, X.; Zhu, Z.; Wang, C.; Chen, S.; Xu, H.; et al. Carbon nanotubes enhance cytotoxicity mediated by human lymphocytes in vitro. PLoS ONE 2017, 6, e21073. [Google Scholar]
- Ali-Boucetta, H.; Nunes, A.; Sainz, R.; Herrero, M.A.; Tian, B.; Prato, M.; Bianco, A.; Kostarelos, K. Asbestos-like pathogenicity of long carbon nanotubes alleviated by chemical functionalization. Angew. Chem. Int. Ed. Engl. 2013, 52, 2274–2278. [Google Scholar] [CrossRef]
- Ema, M.; Hougaard, K.S.; Kishimoto, A.; Honda, K. Reproductive and developmental toxicity of carbon-based nanomaterials: A literature review. Nanotoxicology 2016, 10, 391–412. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.V.; Laux, P.; Luch, A. Review of emerging concepts in nanotoxicology: Opportunities and challenges for safer nanomaterial design. Toxicol. Mech. Methods 2019, 29, 378–387. [Google Scholar] [CrossRef]
- Dong, J.; Ma, Q. Advances in mechanisms and signaling pathways of carbon nanotube toxicity. Nanotoxicology 2015, 9, 658–676. [Google Scholar] [CrossRef]
- Lindberg, H.K.; Falck, G.C.-M.; Singh, R. Genotoxicity of short single-wall and multi-wall carbon nanotubes in human bronchial epithelial and mesothelial cells in vitro. Toxicology 2013, 313, 24–37. [Google Scholar] [CrossRef]
- Murray, A.R.; Kisin, E.; Leonard, S.S.; Young, S.; Kommineni, C.; Kagan, V.; Castranova, V.; Shvedova, A. Oxidative stress and inflammatory response in dermal toxicity of single-walled carbon nanotubes. Toxicology 2008, 257, 161–171. [Google Scholar] [CrossRef]
- Nagai, H.; Okazaki, Y.; Chew, S.H.; Misawa, N.; Yamashita, Y.; Akatsuka, S.; Ishihara, T.; Yamashita, K.; Yoshikawa, Y.; Yasui, H.; et al. Diameter and rigidity of multiwalled carbon nanotubes are critical factors in mesothelial injury and carcinogenesis. Proc. Natl. Acad. Sci. USA 2011, 108, E1330–E1338. [Google Scholar] [CrossRef]
- Silva, R.M.; Doudrick, K.; Franzi, L.M.; TeeSy, C.; Anderson, D.S.; Wu, Z.; Mitra, S.; Vu, V.; Dutrow, G.; Evans, J.E.; et al. Instillation versus inhalation of multiwalled carbon nanotubes: Exposure-related health effects, clearance, and the role of particle characteristics. ACS Nano 2014, 8, 8911–8931. [Google Scholar] [CrossRef] [PubMed]
- Hindman, B.; Ma, Q. Carbon nanotubes and crystalline silica stimulate robust ROS production, inflammasome activation, and IL-1β secretion in macrophages to induce myofibroblast transformation. Arch. Toxicol. 2019, 93, 887–907. [Google Scholar] [CrossRef] [PubMed]
- Reynaud, D.; Pietras, E.; Barry-Holson, K. IL-6 Controls Leukemic Multipotent Progenitor Cell Fate and Contributes to Chronic Myelogenous Leukemia Development. Cancer Cell 2011, 20, 661–673. [Google Scholar] [CrossRef] [PubMed]
- Gañán-Gómez, I.; Wei, Y.; Starczynowski, D.T.; Colla, S.; Yang, H.; Cabrero-Calvo, M.; Bohannan, Z.S.; Verma, A.; Steidl, U.; Garcia-Manero, G. Deregulation of innate immune and inflammatory signaling in myelodysplastic syndromes. Leukemia 2015, 29, 1458–1469. [Google Scholar] [CrossRef]
- Schepers, K.; Pietras, E.M.; Reynaud, D.; Flach, J.; Binnewies, M.; Garg, T.; Wagers, A.J.; Hsiao, E.C.; Passegué, E. Myeloproliferative Neoplasia Remodels the Endosteal Bone Marrow Niche into a Self-Reinforcing Leukemic Niche. Cell Stem Cell 2013, 13, 285–299. [Google Scholar] [CrossRef]
- Welner, R.S.; Amabile, G.; Bararia, D.; Czibere, A.; Yang, H.; Zhang, H.; Pontes, L.L.D.F.; Ye, M.; Levantini, E.; Di Ruscio, A.; et al. Treatment of Chronic Myelogenous Leukemia by Blocking Cytokine Alterations Found in Normal Stem and Progenitor Cells. Cancer Cell 2015, 27, 671–681. [Google Scholar] [CrossRef]
- Rambaldi, A.; Torcia, M.; Dinarello, C.A.; Barbui, T.; Cozzolino, F. Modulation of cell proliferation and cytokine production in AML by recombinant interleukin-1 receptor antagonist. Leukemia 1993, 7, S10–S12. [Google Scholar]
- Stifter, G.; Heiss, S.; Gastl, G.; Tzankov, A.; Stauder, R. Over-expression of tumor necrosis factor-alpha in bone marrow biopsies from patients with myelodysplastic syndromes: Relationship to anemia and prognosis. Eur. J. Haematol. 2005, 75, 485–491. [Google Scholar] [CrossRef]
- Barreyro, L.; Will, B.; Bartholdy, B.; Zhou, L.; Todorova, T.I.; Stanley, R.F.; Ben-Neriah, S.; Montagna, C.; Parekh, S.; Pellagatti, A.; et al. Overexpression of IL-1 receptor accessory protein in stem and progenitor cells and outcome correlation in AML and MDS. Blood 2012, 120, 1290–1298. [Google Scholar] [CrossRef]
- Zhang, B.; Chu, S.; Agarwal, P. Inhibition of interleukin-1 signaling enhances elimination of tyrosine kinase inhibitor-treated CML stem cells. Blood 2016, 128, 2671–2682. [Google Scholar]
- de Mooij, C.E.M.; Netea, M.G.; van der Velden, W.J.F.M.; Blijlevens, N.M.A. Targeting the interleukin-1 pathway in patients with hematological disorders. Blood 2017, 129, 3155–3164. [Google Scholar] [CrossRef] [PubMed]
- Wen, T.; Yang, A.; Piao, L.; Hao, S.; Du, L.; Meng, J.; Liu, J.; Xu, H. Comparative study of in vitro effects of different nanoparticles at non-cytotoxic concentration on the adherens junction of human vascular endothelial cells. Int. J. Nanomedicine 2019, 14, 4475–4489. [Google Scholar] [CrossRef]
- Li, H.; Tan, X.Q.; Yan, L.; Zeng, B.; Meng, J.; Xu, H.Y.; Cao, J.M. Multi-walled carbon nanotubes act as a chemokine and recruit macrophages by activating the PLC/IP3/CRAC channel signaling pathway. Sci. Rep. 2017, 7, 226. [Google Scholar] [CrossRef]
- Yang, M.; Nie, X.; Meng, J.; Liu, J.; Sun, Z.; Xu, H. Carbon Nanotubes Activate Limulus Amebocyte Lysate Coagulation by Interface Adsorption. ACS Appl. Mater. Interfaces 2017, 9, 8450–8454. [Google Scholar] [CrossRef]
- Tashakori-Miyanroudi, M.; Janzadeh, A.; Seifalian, A.; Aboutaleb, N.; Azizi, Y.; Ramezani, F. Will carbon nanotube/nanofiber bring new hope for the treatment of heart damage? A systematic review. Nanomedicine 2022, 17, 2189–2205. [Google Scholar] [CrossRef] [PubMed]
- Mohajer, F.; Ziarani, G.M.; Badiei, A.; Iravani, S.; Varma, R.S. MXene-Carbon Nanotube Composites: Properties and Applications. Nanomaterials 2023, 13, 345. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; Liu, H.; Ye, Y.; Lei, Y.; Islam, R.; Tan, S.; Tong, R.; Miao, Y.B.; Cai, L. Smart nanoparticles for cancer therapy. Signal Transduct. Target. Ther. 2023, 8, 418. [Google Scholar] [CrossRef]
- Meng, J.; Li, X.; Wang, C.; Guo, H.; Liu, J.; Xu, H. Carbon nanotubes activate macrophages into a M1/M2 mixed status: Recruiting naïve macrophages and supporting angiogenesis. ACS Appl. Mater. Interfaces 2015, 7, 3180–3188. [Google Scholar] [CrossRef]
- Tan, X.-Q.; Cheng, X.-L.; Zhang, L.; Wu, B.-W.; Liu, Q.-H.; Meng, J.; Xu, H.-Y.; Cao, J.-M. Multi-walled carbon nanotubes impair Kv4.2/4.3 channel activities, delay membrane repolarization and induce bradyarrhythmias in the rat. PLoS ONE 2017, 9, e101545. [Google Scholar] [CrossRef]
- Meng, J.; Cheng, X.; Kong, H.; Yang, M.; Xu, H. Preparation and biocompatibility evaluation of polyurethane filled with multiwalled carbon nanotubes. J. Nanosci. Nanotechnol. 2013, 13, 1467–1471. [Google Scholar] [CrossRef]
- Jie, M.; Cheng, X.L.; Jian, L. Effects of long and short carboxylated or aminated multiwalled carbon nanotubes on blood coagulation. PLoS ONE 2017, 7, e38995. [Google Scholar]
- Yang, M.; Meng, J.; Cheng, X.; Lei, J.; Guo, H.; Zhang, W.; Kong, H.; Xu, H. Multiwalled carbon nanotubes interact with macrophages and influence tumor progression and metastasis. Theranostics 2012, 2, 258–270. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Meng, J.; Mao, X.B. Carbon nanotubes induce secondary structure changes of bovine albumin in aqueous phase. J. Nanosci. Nanotechnol. 2010, 10, 7550–7553. [Google Scholar] [CrossRef] [PubMed]
- Meng, J.; Yang, M.; Jia, F.; Xu, Z.; Kong, H.; Xu, H. Immune responses of BALB/c mice to subcutaneously injected multi-walled carbon nanotubes. Nanotoxicology 2011, 5, 583–591. [Google Scholar] [CrossRef]
- Meng, J.; Han, Z.; Kong, H. Electrospun aligned nanofibrous composite of MWCNT/polyurethane to enhance vascular endothelium cells proliferation and function. J. Biomed. Mater. Res. 2010, 95, 312–320. [Google Scholar] [CrossRef]
- Xu, H.; Bai, J.; Meng, J.; Hao, W.; Xu, H.; Cao, J. Multi-walled carbon nanotubes suppress potassium channel activities in PC12 cells. Nanotechnology 2009, 20, 285102. [Google Scholar] [CrossRef]
- Han, Z.; Kong, H.; Meng, J.; Wang, C.; Xie, S.; Xu, H. Electrospun aligned nanofibrous scaffold of carbon nanotubes-polyurethane composite for endothelial cells. J. Nanosci. Nanotechnol. 2009, 9, 1400–1402. [Google Scholar] [CrossRef]
- Chen, J.; Liao, S.; Xiao, Z.; Pan, Q.; Wang, X.; Shen, K.; Wang, S.; Yang, L.; Guo, F.; Liu, H.-F.; et al. The development and improvement of immunodeficient mice and humanized immune system mouse models. Front. Immunol. 2022, 13, 1007579. [Google Scholar] [CrossRef]
- Meng, J.; Yang, M.; Song, L.; Kong, H.; Wang, C.; Wang, R.; Xie, S.; Xu, H. Concentration control of carbon nanotubes in aqueous solution and its influence on the growth behavior of fibroblasts. Colloids Surf. B Biointerfaces 2009, 71, 148–153. [Google Scholar] [CrossRef]
- Meng, J.; Kong, H.; Han, Z. Enhancement of nanofibrous scaffold of multiwalled carbon nanotubes/polyurethane composite to the fibroblasts growth and biosynthesis. J. Biomed. Mater. Res. 2009, 88, 105–116. [Google Scholar] [CrossRef]
- Liu, Z.; Robinson, J.T.; Sun, X.; Dai, H. PEGylated nanographene oxide for delivery of water-insoluble cancer drugs. J. Am. Chem. Soc. 2008, 130, 10876–10877. [Google Scholar] [CrossRef] [PubMed]
- Wolff, L.; Koller, R.; Hu, X.; Anver, M.R. A Moloney murine leukemia virus-based retrovirus with 4070A long terminal repeat sequences induces a high incidence of myeloid as well as lymphoid neoplasms. J. Virol 2003, 77, 4965–4971. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Zhang, Z.; Pan, Z.; Liu, Y. Advanced bioactive nanomaterials for biomedical applications. Exploration 2021, 1, 20210089. [Google Scholar] [CrossRef] [PubMed]
- Dai, H.; Fan, Q.; Wang, C. Recent applications of immunomodulatory biomaterials for disease immunotherapy. Exploration 2022, 2, 20210157. [Google Scholar] [CrossRef]
- Yin, B.; Delwel, R.; Valk, P.J. A retroviral mutagenesis screen reveals strong cooperation between Bcl11a overexpression and loss of the Nf1 tumor suppressor gene. Blood 2009, 113, 1075–1085. [Google Scholar] [CrossRef][Green Version]
- Xing, L.H.; Fan, Z.; Xiaolian, S. The genotype-dependent influence of functionalized multiwalled carbon nanotubes on fetal development. Biomaterials 2014, 35, 856–865. [Google Scholar]
- Luanpitpong, S.; Wang, L.Y.; Castranova, V.; Rojanasakul, Y. Induction of stem-like cells with malignant properties by chronic exposure of human lung epithelial cells to single-walled carbon nanotubes. Part. Fibre Toxicol. 2014, 11, 22. [Google Scholar] [CrossRef]
- Atsuya, T.; Akihiko, H.; Tetsuji, N. Induction of mesothelioma in p53+/− mouse by intraperitoneal application of multi-wall carbon nanotube. J. Toxicol. Sci. 2008, 33, 105–116. [Google Scholar]
- Al Ustwani, O.; Ford, L.A.; Sait, S.J.; Block, A.M.W.; Barcos, M.; Vigil, C.E.; Griffiths, E.A.; Thompson, J.E.; Wang, E.S.; Ambrus, J., Jr.; et al. Myelodysplastic syndromes and autoimmune diseases-Case series and review of literature. Leuk. Res. 2013, 37, 894–899. [Google Scholar] [CrossRef]
- Basiorka, A.A.; McGraw, K.L.; Eksioglu, E.A.; Chen, X.; Johnson, J.; Zhang, L.; Zhang, Q.; Irvine, B.A.; Cluzeau, T.; Sallman, D.A.; et al. The NLRP3 inflammasome functions as a driver of the myelodysplastic syndrome phenotype. Blood 2016, 128, 2960–2975. [Google Scholar] [CrossRef]
- Sashida, G.; Harada, H.; Matsui, H. Ezh2 loss promotes development of myelodysplastic syndrome but attenuates its predisposition to leukaemic transformation. Nat. Commun. 2014, 5, 4177. [Google Scholar] [CrossRef] [PubMed]
- Sallman, D.A.; List, A. The central role of inflammatory signaling in the pathogenesis of myelodysplastic syndromes. Blood 2019, 133, 1039–1048. [Google Scholar] [CrossRef] [PubMed]
- Zambetti, N.A.; Ping, Z.; Chen, S.; Kenswil, K.J.G.; Mylona, M.A.; Sanders, M.A.; Hoogenboezem, R.M.; Bindels, E.M.J.; Adisty, M.N.; Van Strien, P.M.H.; et al. Mesenchymal Inflammation Drives Genotoxic Stress in Hematopoietic Stem Cells and Predicts Disease Evolution in Human Pre-leukemia. Cell Stem Cell 2016, 19, 613–627. [Google Scholar] [CrossRef]
- Dong, L.; Yu, W.M.; Zheng, H. Leukaemogenic effects of Ptpn11 activating mutations in the stem cell microenvironment. Nature 2016, 539, 304–308. [Google Scholar] [CrossRef] [PubMed]
- Jacquelin, S.; Straube, J.; Cooper, L. Jak2V617F and Dnmt3a loss cooperate to induce myelofibrosis through activated enhancer-driven inflammation. Blood 2018, 132, 2707–2721. [Google Scholar] [CrossRef]
- Ewald, P.W.; Swain, E.H.A. The scope of viral causation of human cancers: Interpreting virus density from an evolutionary perspective. Philos. Trans. R. Soc. Lond. Ser. B Biol. Sci. 2019, 374, 20180304. [Google Scholar] [CrossRef]




| Organ | |
|---|---|
| Immune System | Spleen |
| Lymph Nodes | |
| Respiratory System | Lung |
| Urinary System | Kidney |
| Digestive System | Liver |
| Treatment | Myeloid | T | B | Mixed |
|---|---|---|---|---|
| MuLV (N = 15) | 5 | 5 | 1 | 4 |
| MuLV + MWCNTs (N = 15) | 4 | 6 | 0 | 5 |
| Group of Mouse | WBC (×103/μL) | Hemoglobin (g/L) | RBC (×106/μL) | Platelet (×109/μL) |
|---|---|---|---|---|
| Control | 4.78 (0.46) | 13.93 (0.25) | 9.40 (1.01) | 895.70 (36.92) |
| MuLV | 6.18 (1.07) | 13.48 (1.06) | 8.24 (0.67) | 841.43 (164.8) |
| MuLV + MWCNT | 7.68 (2.02) | 13.10 (0.78) | 8.48 (0.64) | 923.24 (176.68) |
| MuLV + MWCNT-PEG | 6.73 (1.22) | 12.36 (0.78) | 8.43 (1.08) | 915.03 (177.92) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Q.; Han, J.; Wei, M.; Miao, H.; Zhang, M.; Wu, B.; Chen, Y.; Zheng, Y.; Gale, R.P.; Yin, B. Multi-Walled Carbon Nanotubes Accelerate Leukaemia Development in a Mouse Model. Toxics 2024, 12, 646. https://doi.org/10.3390/toxics12090646
Wang Q, Han J, Wei M, Miao H, Zhang M, Wu B, Chen Y, Zheng Y, Gale RP, Yin B. Multi-Walled Carbon Nanotubes Accelerate Leukaemia Development in a Mouse Model. Toxics. 2024; 12(9):646. https://doi.org/10.3390/toxics12090646
Chicago/Turabian StyleWang, Qingqing, Jingdan Han, Mujia Wei, Huikai Miao, Min Zhang, Biao Wu, Yao Chen, Yanwen Zheng, Robert Peter Gale, and Bin Yin. 2024. "Multi-Walled Carbon Nanotubes Accelerate Leukaemia Development in a Mouse Model" Toxics 12, no. 9: 646. https://doi.org/10.3390/toxics12090646
APA StyleWang, Q., Han, J., Wei, M., Miao, H., Zhang, M., Wu, B., Chen, Y., Zheng, Y., Gale, R. P., & Yin, B. (2024). Multi-Walled Carbon Nanotubes Accelerate Leukaemia Development in a Mouse Model. Toxics, 12(9), 646. https://doi.org/10.3390/toxics12090646





