Environmental Methamphetamine Exposures and Health Effects in 25 Case Studies
Abstract
1. Introduction
2. Materials and Methods
2.1. General
2.2. Identification of Opportunistic Case Studies
2.3. Characterisation of Exposure
2.3.1. Environmental Contamination Levels
2.3.2. Hair Analysis
2.4. Characterisation of Health Effects
2.4.1. Interview Data
- Participants—age, gender, hair colour, whether the hair was dyed, use of amphetamine-type stimulants, including attention-deficit/hyperactivity disorder (ADHD) drugs (particularly relevant for children);
- Housing situation—owning or renting, duration of time at the property, how much time is spent in the property, including whether the participant was the primary cleaner in the home, if they had undertaken renovations in the home, or whether children undertake a lot of floor play;
- Exposure situation—how the participant or family came to be living in the property and how they found out that the property was contaminated. Information about whether the property may have been contaminated from manufacture or use was also obtained;
- Health information—identification of pre-existing conditions, description of health issues that occurred while living in the property, with medical records or school attendance plus medical records provided to support the information provided, and information on whether the health effects persisted when out of the property. Where the health problems had resolved, questions relating to how long the health effects persisted after moving out of the home were also included. The collection of health information focused on health effects that occurred within the property that were different from or worse than health issues experienced prior to living in the property. As the health effects being documented were self-reported, it was considered important to document health effects specifically related to the time spent in the property. For some case studies, children had spent their whole lives living at the contaminated property. For these participants, the health information obtained from parents related to their overall health. In some cases, health effects related to the property could be identified more clearly as these did not persist whenever the participant was out of the property.
2.4.2. Behavioural Assessment
3. Results
3.1. Opportunistic Case Studies
3.2. Property Details
3.3. Data from Individual Participants
4. Discussion
4.1. Disclosure
4.2. Health Effects
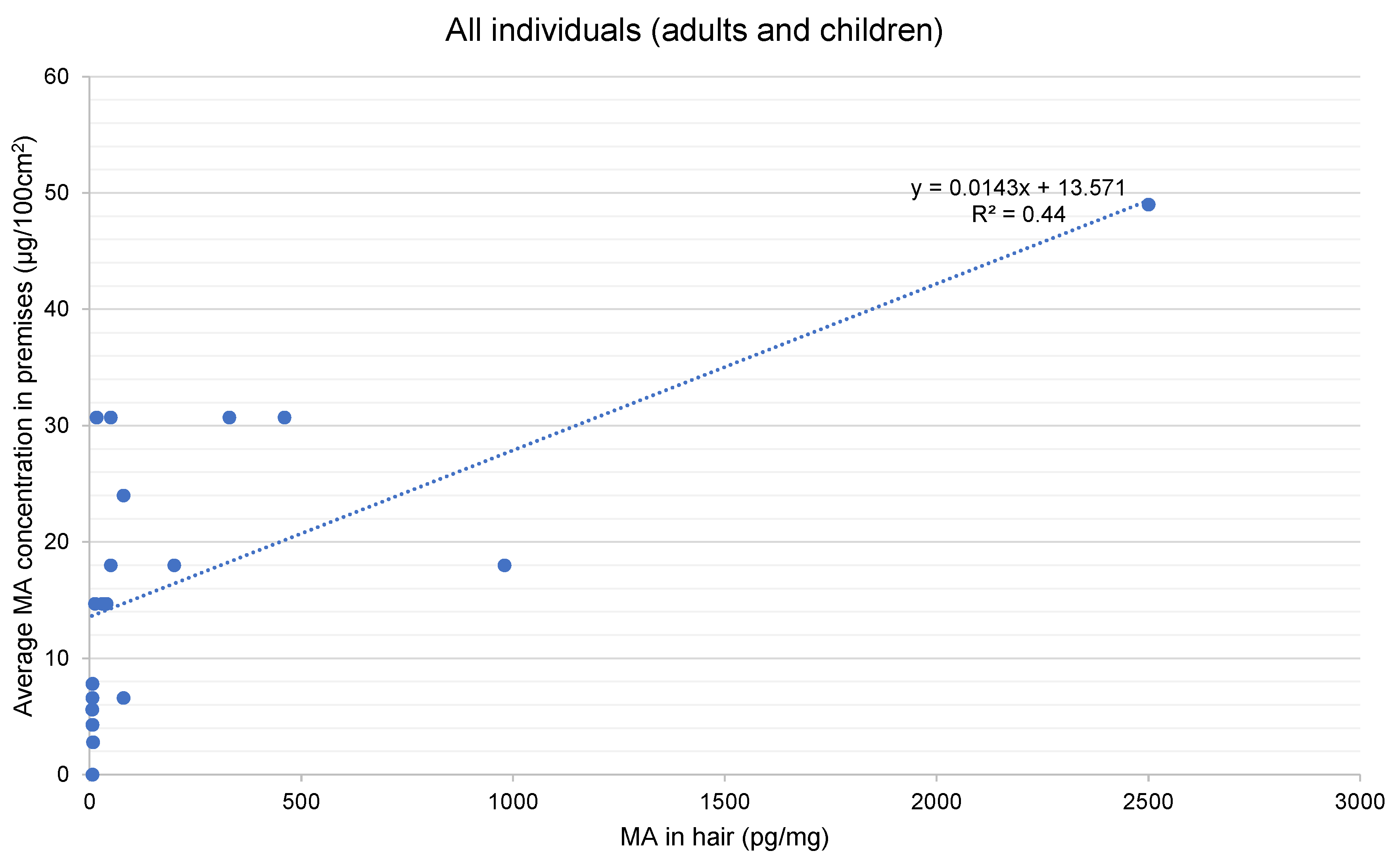
4.3. Hair Analysis
4.4. Use vs. Manufacture
4.5. Guidelines
4.6. Study Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Martyny, J.W.; Arbuckle, S.L.; McCammon, C.S.; Esswein, E.J.; Erb, N.; Van Dyke, M. Chemical concentrations and contamination associated with clandestine methamphetamine laboratories. J. Chem. Health Saf. 2007, 14, 40–52. [Google Scholar] [CrossRef]
- Martyny, J.W.; Arbuckle, S.L.; McCammon, C.S.; Erb, N. Methamphetamine Contamination on Environmental Surfaces Caused by Simulated Smoking of Methamphetamine; National Jewish Medical and Research Center: Denver, CO, USA, 2004. [Google Scholar]
- enHealth. enHealth Position Statement: Clandestine Drug Laboratories and Public Health Risks; enHealth: Canberra, Australia, 2017. [Google Scholar]
- Bitter, J.L. The persistence of illicit drug smoke residues and their recovery from common household surfaces. Drug Test. Anal. 2016, 9, 603–612. [Google Scholar] [CrossRef] [PubMed]
- Wright, J.; Edwards, J.; Walker, G.S. Exposures associated with clandestine methamphetamine drug laboratories in Australia. Rev. Environ. Health 2016, 31, 329–352. [Google Scholar] [CrossRef] [PubMed]
- Wright, J.; Walker, G.S.; Ross, K.E. Contamination of Homes with Methamphetamine: Is Wipe Sampling Adequate to Determine Risk? Int. J. Environ. Res. Public Health 2019, 16, 3568. [Google Scholar] [CrossRef] [PubMed]
- Wright, J. Exposure and Risk Associated with Clandestine Amphetamine-Type Stimulant Drug Laboratories. Ph.D. Thesis, Flinders University, Adelaide, Australia, 2016. [Google Scholar]
- Wright, J.; Kenneally, M.E.; Edwards, J.W.; Walker, G.S. Adverse Health Effects Associated with Living in a Former Methamphetamine Drug Laboratory-Victoria, Australia, 2015. MMWR. Morb. Mortal. Wkly. Rep. 2017, 65, 1470–1473. [Google Scholar] [CrossRef]
- Ferguson, T.J. Overview of Medical Toxicology and Potential for Exposures to Clandestine Drug Laboratories in California; University of California: Davis, CA, USA, 2003. [Google Scholar]
- Denehy, J. The meth epidemic: Its effect on children and communities. J. Sch. Nurs. 2006, 22, 63–65. [Google Scholar] [CrossRef]
- Mecham, N.; Melini, J. Unintentional victims: Development of a protocol for the care of children exposed to chemicals at methamphetamine laboratories. Pediatr. Emerg. Care 2002, 18, 327–332. [Google Scholar] [CrossRef]
- Thrasher, D.L.; Von Derau, K.; Burgess, J.L. Health effects from reported exposure to methamphetamine labs: A poison center-based study. J. Med. Toxicol. 2009, 5, 200–204. [Google Scholar] [CrossRef]
- Oregon Department of Human Services. Children in Methamphetamine “Labs” in Oregon; CD Summary, An Epdemiology Publication of the Oregon Department of Human Services; Oregon Department of Human Services: Portland, OR, USA, 2003; Volume 16, p. 2. [Google Scholar]
- Flannery, M.T.; Jones, J.; Farst, K.; Worley, K.B.; Worthington, T.; Rauls, S. The Use of Hair Analysis to Test Children for Exposure to Methamphetamine. MSU J. Med. Law 2006, 143, 143–254. [Google Scholar]
- Brinker, M.; Boote, M.; Donnell, S.; Hill, K.; Hick, R. C-62A Comparison of Externalizing Behaviors Between Children Prenatally Exposed to Methamphetamine and Children with Attention Deficit/Hyperactivity Disorder (ADHD). Arch. Clin. Neuropsychol. 2016, 31, 663. [Google Scholar] [CrossRef]
- Kwiatkowski, M.A.; Donald, K.A.; Stein, D.J.; Ipser, J.; Thomas, K.G.; Roos, A. Cognitive outcomes in prenatal methamphetamine exposed children aged six to seven years. Compr. Psychiatry 2018, 80, 24–33. [Google Scholar] [CrossRef]
- Smith, L.M.; Diaz, S.; Lagasse, L.L.; Wouldes, T.A.; Derauf, C.; Newman, E.; Arria, A.M.; Huestis, M.A.; Haning, W.; Strauss, A.; et al. Developmental and behavioral consequences of prenatal methamphetamine exposure: A review of the Infant Development, Environment, and Lifestyle (IDEAL) study. Neurotoxicol. Teratol. 2015, 51, 35–44. [Google Scholar] [CrossRef]
- Caldicott, D.; Pigou, P.E.; Beattie, R.; Edwards, J.W. Clandestine drug laboratories in Australia and the potential for harm. Aust. N. Z. J. Public Health 2005, 29, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Degenhardt, L.; Sara, G.; McKETIN, R.; Roxburgh, A.; Dobbins, T.A.; Farrell, M.; Burns, L.; Hall, W. Crystalline methamphetamine use and methamphetamine-related harms in Australia. Drug Alcohol Rev. 2016, 36, 160–170. [Google Scholar] [CrossRef]
- Reynolds, C.R.; Kamphaus, R.W. Behavior Assessment System for Children, 2nd ed.; American Guidance Service: Circle Pine, MN, USA, 2004. [Google Scholar]
- Altmann, R.A.; Reynolds, C.R.; Kamphaus, R.W.; Vannest, K.J. BASC-3, Encyclopedia of Clinical Neuropsychology; Kreutzer, J., DeLuca, J., Caplan, B., Eds.; Springer Science and Business Media LLC: Cham, Switzerland, 2017; pp. 1–7. [Google Scholar]
- NIOSH. Method 9111 Methamphetamine on Wipes by Liquid Chromatography-Mass Spectrometry-SIM. In NIOSH Manual of Analytical Methods (NMAM), 5th ed.; CDC, The National Institute for Occupational Safety and Health: Washington, DC, USA, 2011. [Google Scholar]
- Cooper, G.; Kronstrand, R.; Kintz, P. Society of Hair Testing guidelines for drug testing in hair. Forensic Sci. Int. 2012, 218, 20–24. [Google Scholar] [CrossRef] [PubMed]
- Van Dyke, M.; Erb, N.; Arbuckle, S.; Martyny, J. A 24-Hour Study to Investigate Persistent Chemical Exposures Associated with Clandestine Methamphetamine Laboratories. J. Occup. Environ. Hyg. 2008, 6, 82–89. [Google Scholar] [CrossRef]
- Salocks, C.B.; Hui, X.; Lamel, S.; Qiao, P.; Sanborn, J.R.; Maibach, H.I. Dermal exposure to methamphetamine hydrochloride contaminated residential surfaces. Food Chem. Toxicol. 2012, 50, 4436–4440. [Google Scholar] [CrossRef] [PubMed]
- Salocks, C.B.; Hui, X.; Lamel, S.; Hafeez, F.; Qiao, P.; Sanborn, J.R.; Maibach, H.I. Dermal exposure to methamphetamine hydrochloride contaminated residential surfaces II. Skin surface contact and dermal transfer relationship. Food Chem. Toxicol. 2014, 66, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Martyny, J.W.; Arbuckle, S.L.; McCammon, C.S.; Esswein, E.J.; Erb, N. Chemical Exposures Associated with Clandestine Methamphetamine Laboratories; National Jewish Medical and Research Center: Denver, CO, USA, 2004. [Google Scholar]
- Lawrence, D.J.; Johnson, S.; Hafekost, J.; Boterhoven de Haan, K.; Sawyer, M.; Ainley, J.; Zubrick, S.R. The Mental Health of Children and Adolescents, Report on the Second Australian Child and Adolescent Survey of Mental Health and Wellbeing; Department of Health: Canberra, Australia, 2015. [Google Scholar]
- Polanczyk, G.V.; Willcutt, E.G.; Salum, G.A.; Kieling, C.; Rohde, L.A. ADHD prevalence estimates across three decades: An updated systematic review and meta-regression analysis. Int. J. Epidemiol. 2014, 43, 434–442. [Google Scholar] [CrossRef]
- Rasmussen, L.; Pratt, N.L.; Roughead, E.E.; Moffat, A. Prevalence of Psychotropic Medicine Use in Australian Children with Autism Spectrum Disorder: A Drug Utilization Study Based on Children Enrolled in the Longitudinal Study of Australian Children. J. Autism Dev. Disord. 2018, 49, 227–235. [Google Scholar] [CrossRef]
- Pennar, A.L.; Shapiro, A.F.; Krysik, J. Drug endangered children: Examining children removed from methamphetamine laboratories. Child. Youth Serv. Rev. 2012, 34, 1777–1785. [Google Scholar] [CrossRef]
- Kintz, P.; Farrugia, A.; Ameline, A.; Eibel, A.; Raul, J.-S. High risk of misinterpreting hair analysis results for children tested for methadone. Forensic Sci. Int. 2017, 280, 176–180. [Google Scholar] [CrossRef]
- Pragst, F.; Krumbiegel, F.; Thurmann, D.; Westendorf, L.; Methling, M.; Niebel, A.; Hartwig, S. Hair analysis of more than 140 families with drug consuming parents. Comparison between hair results from adults and their children. Forensic Sci. Int. 2019, 297, 161–170. [Google Scholar] [CrossRef] [PubMed]
- Witter, R.Z.; Martyny, J.W.; Mueller, K.; Gottschall, B.; Newman, L.S. Symptoms Experienced by Law Enforcement Personnel During Methamphetamine Lab Investigations. J. Occup. Environ. Hyg. 2007, 4, 895–902. [Google Scholar] [CrossRef] [PubMed]
- CDC. Public Health Consequences Among First Responders to Emergency Events Associated with Illicit Methamphetamine Laboratories—Selected States, 1996–1999. JAMA 2000, 284, 2715. [Google Scholar] [CrossRef][Green Version]
- Burgess, J.L.; Barnhart, S.; Checkoway, H. Investigating clandestine drug laboratories: Adverse medical effects in law enforcement personnel. Am. J. Ind. Med. 1996, 30, 488–494. [Google Scholar] [CrossRef]
- Alert, C.S. Clan Lab Safety Alert, Newsletter; Clandestine Laboratory Investigators Association (CLIA) and NES: Folsom, CA, USA, 2003–2015. [Google Scholar]
- Manning, T. Drug Labs and Endangered Children. PsycEXTRA Dataset 2013, 68. [Google Scholar] [CrossRef]
- Vearrier, D.; Greenberg, M.I.; Miller, S.N.; Okaneku, J.T.; Haggerty, D.A. Methamphetamine: History, Pathophysiology, Adverse Health Effects, Current Trends, and Hazards Associated with the Clandestine Manufacture of Methamphetamine. Disease 2012, 58, 38–89. [Google Scholar] [CrossRef]
- McFadden, D.; Kub, J.; Fitzgerald, S. Occupational Health Hazards to First Responders from Clandestine Methamphetamine Labs. J. Addict. Nurs. 2006, 17, 169–173. [Google Scholar] [CrossRef]
- Burgess, J.L.; Kovalchick, D.F.; Siegel, E.M.; Hysong, T.A.; McCurdy, S.A. Medical Surveillance of Clandestine Drug Laboratory Investigators. J. Occup. Environ. Med. 2002, 44, 184–189. [Google Scholar] [CrossRef]
- Rothenbaum, D.K. Exposed: An Officer’s Story, CSAlert; Newsletter of Clandestine Laboratory Investigators Association (CLIA) and NES: Folsom, CA, USA, 2010; Volume 7. [Google Scholar]
- Ross, G.H.; Sternquist, M.C. Methamphetamine exposure and chronic illness in police officers: Significant improvement with sauna-based detoxification therapy. Toxicol. Ind. Health 2012, 28, 758–768. [Google Scholar] [CrossRef] [PubMed]
- Watanabe-Galloway, S.; Ryan, S.; Hansen, K.; Hullsiek, B.; Muli, V.; Malone, A.C. Effects of Methamphetamine Abuse Beyond Individual Users. J. Psychoact. Drugs 2009, 41, 241–248. [Google Scholar] [CrossRef] [PubMed]
- Maxwell, J.C. Emerging research on methamphetamine. Curr. Opin. Psychiatry 2005, 18, 235–242. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cline, J.S. Illegal Methamphetamine Laboratories as a Public Health Hazard. Pop. Gov. Fall 2005, 24–36. [Google Scholar]
- Easter, M.G. Are You Living in a Former Meth Lab? In Health; Scientific American: New York, NY, USA, 29 April 2010. [Google Scholar]
- McGee, S.M.; McGee, D.N.; McGee, M.B. Spontaneous Intracerebral Hemorrhage Related to Methamphetamine Abuse: Autopsy findings and clinical correlation. Am. J. Forensic Med. Pathol. 2004, 25, 334–337. [Google Scholar] [CrossRef]
- Cruickshank, C.C.; Dyer, K.R. A review of the clinical pharmacology of methamphetamine. Addiction 2009, 104, 1085–1099. [Google Scholar] [CrossRef]
- Herrmann, E.S.; Johnson, P.S.; Bruner, N.R.; Van Drey, R.; Johnson, M.W. Morning administration of oral methamphetamine dose-dependently disrupts nighttime sleep in recreational stimulant users. Drug Alcohol Depend. 2017, 178, 291–295. [Google Scholar] [CrossRef]
- Ostler, T.; Haight, W.; Black, J.; Choi, G.-Y.; Kingery, L.; Sheridan, K. Case Series: Mental health needs and perspectives of rural children reared by parents who abuse methamphetamine. J. Am. Acad. Child Adolesc. Psychiatry 2007, 46, 500–507. [Google Scholar] [CrossRef]
- Asanbe, C.B.; Hall, C.; Bolden, C.D. The Methamphetamine Home: Psychological Impact on Preschoolers in Rural Tennessee. J. Rural. Health 2008, 24, 229–235. [Google Scholar] [CrossRef]
- Haight, W.; Marshall, J.; Hans, S.; Black, J.; Sheridan, K. “They mess with me, I mess with them”: Understanding physical aggression in rural girls and boys from methamphetamine-involved families. Child. Youth Serv. Rev. 2010, 32, 1223–1234. [Google Scholar] [CrossRef]
- Haight, W.; Jacobsen, T.; Black, J.; Kingery, L.; Sheridan, K.; Mulder, C. “In these bleak days”: Parent methamphetamine abuse and child welfare in the rural Midwest. Child. Youth Serv. Rev. 2005, 27, 949–971. [Google Scholar] [CrossRef]
- Haight, W.; Black, J.; Sheridan, K. A mental health intervention for rural, foster children from methamphetamine-involved families: Experimental assessment with qualitative elaboration. Child. Youth Serv. Rev. 2010, 32, 1446–1457. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem; Colten, H.R., Altevogt, B.M., Eds.; Committee on Sleep Medicine and Research Board on Health Sciences Policy, The National Academies Press: Washington, DC, USA, 2006. [Google Scholar]
- McKetin, R.; Hickey, K.; Devlin, K.; Lawrence, K. The risk of psychotic symptoms associated with recreational methamphetamine use. Drug Alcohol Rev. 2010, 29, 358–363. [Google Scholar] [CrossRef]
- McKetin, R.; McLaren, J.; Lubman, D.I.; Hides, L. The prevalence of psychotic symptoms among methamphetamine users. Addiction 2006, 101, 1473–1478. [Google Scholar] [CrossRef] [PubMed]
- McKetin, R.; Lubman, D.I.; Baker, A.L.; Dawe, S.; Ali, R. Dose-Related Psychotic Symptoms in Chronic Methamphetamine Users: Evidence from a prospective longitudinal study. JAMA Psychiatry 2013, 70, 319–324. [Google Scholar] [CrossRef] [PubMed]
- Perez, A.Y.; Kirkpatrick, M.G.; Gunderson, E.W.; Marrone, G.; Silver, R.; Foltin, R.W.; Hart, C.L. Residual effects of intranasal methamphetamine on sleep, mood, and performance. Drug Alcohol Depend. 2008, 94, 258–262. [Google Scholar] [CrossRef][Green Version]
- Darke, S.; Kaye, S.; McKETIN, R.; Duflou, J. Major physical and psychological harms of methamphetamine use. Drug Alcohol Rev. 2008, 27, 253–262. [Google Scholar] [CrossRef]
- Dean, A.C.; Groman, S.M.; Morales, A.M.; London, E.D. An Evaluation of the Evidence that Methamphetamine Abuse Causes Cognitive Decline in Humans. Neuropsychopharmacol. Off. Publ. Am. Coll. Neuropsychopharmacol. 2012, 38, 259–274. [Google Scholar] [CrossRef]
- Proebstl, L.; Kamp, F.; Koller, G.; Soyka, M. Cognitive Deficits in Methamphetamine Users: How Strong is The Evidence? Pharmacopsychiatry 2018, 51, 243–250. [Google Scholar] [CrossRef]
- Buck, J.M.; Siegel, J.A. The effects of adolescent methamphetamine exposure. Front. Mol. Neurosci. 2015, 9, 151. [Google Scholar] [CrossRef]
- Siegel, J.A.; Park, B.S.; Raber, J. Long-term effects of neonatal methamphetamine exposure on cognitive function in adolescent mice. Behav. Brain Res. 2011, 219, 159–164. [Google Scholar] [CrossRef] [PubMed]
- Bassindale, T. Quantitative analysis of methamphetamine in hair of children removed from clandestine laboratories—Evidence of passive exposure? Forensic Sci. Int. 2012, 219, 179–182. [Google Scholar] [CrossRef] [PubMed]
- Castaneto, M.S.; Barnes, A.J.; Scheidweiler, K.B.; Schaffer, M.; Rogers, K.K.; Stewart, D.; Huestis, M.A. Identifying Methamphetamine Exposure in Children. Ther. Drug Monit. 2013, 35, 823–830. [Google Scholar] [CrossRef] [PubMed]
- De La Torre, R.; Farré, M.; Navarro, M.; Pacifici, R.; Zuccaro, P.; Pichini, S. Clinical Pharmacokinetics of Amfetamine and Related Substances: Monitoring in conventional and non-conventional matrices. Clin. Pharmacokinet. 2004, 43, 157–185. [Google Scholar] [CrossRef]
- Han, E.; Yang, H.; Seol, I.; Park, Y.; Lee, B.; Song, J.M. Segmental hair analysis and estimation of methamphetamine use pattern. Int. J. Leg. Med. 2012, 127, 405–411. [Google Scholar] [CrossRef]
- Nakahara, Y. Detection and diagnostic interpretation of amphetamines in hair. Forensic Sci. Int. 1995, 70, 135–153. [Google Scholar] [CrossRef]
- Tsanaclis, L.; Wicks, J.F. Differentiation between drug use and environmental contamination when testing for drugs in hair. Forensic Sci. Int. 2008, 176, 19–22. [Google Scholar] [CrossRef]
- Tsanaclis, L.; Wicks, J.F. Patterns in drug use in the United Kingdom as revealed through analysis of hair in a large population sample. Forensic Sci. Int. 2007, 170, 121–128. [Google Scholar] [CrossRef]
- Han, E.; Paulus, M.P.; Wittmann, M.; Chung, H.-S.; Song, J.M. Hair analysis and self-report of methamphetamine use by methamphetamine dependent individuals. J. Chromatogr. B 2011, 879, 541–547. [Google Scholar] [CrossRef]
- AG & ACC. Clandestine Drug Laboratory Remediation Guidelines; Attorney-General’s Department and Australian Crime Commission, Commonwealth of Australia: Canberra, Australia, 2011. [Google Scholar]
- Wright, J. Derivation of Risk-Based Investigation Levels, Clandestine Drug Laboratory, Site Investigation Guidelines; Environmental Risk Sciences: Sydney, Australia, 2009. [Google Scholar]
- Wright, J. Australian Voluntary Code of Practice, Assessment, Remediation and Validation: Former Clandestine Drug Laboratories and Other Methamphetamine Contaminated Properties; Environmental Health Australia (EHA) and ALGA: Australia, 2019. [Google Scholar]




| Case Study | General Location | Type of Property | Ownership | Occupants | Duration of Time in Property | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| R | U | H | A | O | T | PH | Adults | Children | ||
| CS01 | y | y | y | 2 | 3 | 1.5 years | ||||
| CS02 | y | y | y | 1 | 2 | 2 years | ||||
| CS03 | y | y | y | 1 | 8 months | |||||
| CS04 | y | y | y | 2 | 2 | 5 weeks | ||||
| CS05 | y | y | y | y | 2 | 1 | 3 years | |||
| CS06 | y | y | y | y | 1 | 7 years | ||||
| CS07 | y | y | y | 1 | 1 | 2 years | ||||
| CS08 | y | y | y | 2 | 3 | 4 months | ||||
| CS09 | y | y | y | 2 | 5 months | |||||
| CS10 | y | y | y | y | 1 | 3 years | ||||
| CS11 | y | y | y | 1 | 7 months | |||||
| CS12 | y | y | y | 2 | 3 | 4.5 months | ||||
| CS13 | y | y | y | y | 1 | Regular short visits | ||||
| CS14 | y | y | y | 1 | 10 days per fortnight over 2 years | |||||
| CS15 | y | y | y | y | 1 | 1 | 3 years | |||
| CS16 | y | y | y | 1 | 8 months | |||||
| CS17 | y | y | y | 1 | 5 months | |||||
| CS18 | y | y | y | 2 | 2 | 8 months | ||||
| CS19 | y | y | y | 2 | 2 | 8 years | ||||
| CS20 | y | y | y | 2 | 2 years—few days at a time | |||||
| CS21 | y | y | y | 1 | 4 weeks | |||||
| CS22 | y | y | y | 2 | 2 | 10 years | ||||
| CS23 | y | y | y | 2 | 2 | 6 years | ||||
| CS24 | y | y | y | 1 | 3 | 6 weeks | ||||
| CS25 | y | y | y | y | 1 | 13 months | ||||
| N = | 3:22 | 20:5 | 7 | 18 | 6 | 34:29 | ||||
| Case Study | Activity Likely to Have Resulted in Contamination | Contamination Status of Methamphetamine, Based on Wipe Sample Results (µg/100 cm2) | |||
|---|---|---|---|---|---|
| Manufacture | Use | Minimum | Maximum | Average * | |
| CS01 | y (police seized) | 11 | 107 | 30.7 | |
| CS02 | y | <0.02 | 42 | 2.2 | |
| CS03 | y | 0.01 | >10 | NA | |
| CS04 | y, suspected | 7.3 | 8.3 | 7.8 | |
| CS05 | y | <0.03 | 20.7 | 2.8 | |
| CS06 | y | <0.03 | 1.32 | 0.31 | |
| CS07 | y | 0.02 | 4.4 | 0.96 | |
| CS08 | y | 0.1 | 5.7 | 2.2 | |
| CS09 | potential | potential | 0.12 | 53 | 3.1 |
| CS10 | y, suspected | 0.69 | >100 | 25 | |
| CS11 | potential | potential | 0.19 | 42.9 | 7.8 |
| CS12 | potential | potential | 3.5 | 7.8 | 5.6 |
| CS13 | y | <0.02 | 20 | 2 | |
| CS14 | y | NA | NA | NA | |
| CS15 | y | <0.02 | 0.13 | 0.06 | |
| CS16 | y | 4.1 | 107 | 49 | |
| CS17 | potential | y | 5.34 | 45.09 | 24 |
| CS18 | y | 0.32 | 9.9 | 4.3 | |
| CS19 | y | <0.02 | 245 | 18.8 | |
| CS20 | y | 0.05 | 31 | 2.3 | |
| CS21 | y | <0.02 | 2 | 0.34 | |
| CS22 | potential | potential | 0.38 | 250 | 18 |
| CS23 | y | 0.18 | 125 | 14.7 | |
| CS24 | potential | potential | 0.03 | 25 | 6.6 |
| CS25 | potential | potential | <0.02 | 3.5 | 1.2 |
| Manufactured—Yes | 7 | ||||
| Manufactured—Suspected | 2 | ||||
| Manufactured—Potential | 7 | ||||
| Manufactured—No | 10 | ||||
| Use—Yes | 11 | ||||
| Use—Potential | 6 | ||||
| Use—No | 8 | ||||
| Manufactured (Potential) + Use | 1 | ||||
| Manufactured (Potential) + Use (Potential) | 6 | ||||
| Health Effect Reported | Number of Participants Reporting Health Effect as Number (% All Participants) | Resolution of Health Effects Once Out of the Property | |
|---|---|---|---|
| Children and Adolescents [n = 29] | Adults, 21 Years and Older [n = 34] | ||
| Skin (rashes, irritation) | 16 (55%) | 19 (56%) | Yes—within days to weeks |
| Eyes (sore, watering) | 16 (55%) | 20 (59%) | Yes—within hours to days |
| Respiratory—total | 18 (62%) | 18 (53%) | |
| - Persistent cough | 16 (55%) | 16 (47%) | Yes—within days to weeks |
| - Asthma or asthma-like symptoms | 10 (34%) | 10 (29%) | Yes—within days to weeks |
| Immune (chronic or constant infections—respiratory or sinus) | 7 (24%) | 11 (32%) | Yes—within weeks |
| Headache | 2 (7%) | 16 (47%) | Yes—within days to weeks |
| Sleep—total | 21 (72%) | 23 (68%) | |
| - Difficulty sleeping | 18 (62%) | 21 (62%) | Yes—within days to weeks |
| - Unusual dreams | 12 (41%) | 10 (29%) | Yes—within days to weeks |
| Behavioural and cognitive—total | 23 (79%) | 22 (65%) | Most resolved within a month to a year. For 3 participants, depression continued for a longer time, likely due to prolonged issues in dealing with the contaminated property. In addition, for some parents there is ongoing anxiety about their children’s health in the long term. |
| - Fatigue or tiredness | 8 (28%) | 13 (38%) | |
| - Increased aggression or irritability | 16 (55%) | 5 (15%) | |
| - Moodiness, depression, anxiety | 5 (17%) | 13 (38%) | |
| - Vagueness or not thinking clearly | 5 (17%) | 10 (29%) | |
| - Memory issues | 0 | 6 (18%) | |
| Exacerbation of pre-existing conditions | 2 (7%) | 7 (21%) | Yes—within months |
| Sample Code * | Age (Years) | Hair Analysis Results (pg/mg) | Average Level of MA Contamination in Property ** (µg/100 cm2) | Likely Source of Contamination | |||
|---|---|---|---|---|---|---|---|
| Hair Matrix | Hair Wash | ||||||
| MA | AMP | MA | AMP | ||||
| CS01F40 | 40 | 17 | <5 | 8 | <5 | 30.7 | M |
| CS01M38 | 38 | 5 | <5 | <5 | <5 | 30.7 | M |
| CS01F11 | 11 | 50 | <5 | <5 | <5 | 30.7 | M |
| CS01M8 | 8 | 330 | 16 | <5 | <5 | 30.7 | M |
| CS01M7 | 7 | 460 | 20 | <5 | <5 | 30.7 | M |
| CS04F2 | 2 | <5 | <5 | <5 | <5 | 7.8 | M |
| CS05F13 | 13 | 8 | <5 | <5 | <5 | 2.8 | U |
| CS08M11 | 11 | <5 | <5 | <5 | <5 | 2.2 | U |
| CS08M8 | 8 | <5 | <5 | <5 | <5 | 2.2 | U |
| CS08F6 | 6 | <5 | <5 | <5 | <5 | 2.2 | U |
| CS09F30 | 30 | <5 | <5 | <5 | <5 | 3.1 | M and/or U |
| CS10F44 | 44 | <5 | <5 | <5 | <5 | 25 | M |
| CS11F61 | 61 | 7 | <5 | <5 | <5 | 7.8 | M and/or U |
| CS12M10 | 10 | <5 | <5 | <5 | <5 | 5.6 | M and/or U |
| CS12M6 | 6 | <5 | <5 | <5 | <5 | 5.6 | M and/or U |
| CS12M3 | 3 | 6 | <5 | <5 | <5 | 5.6 | M and/or U |
| CS14M2 | 2 | 7 | <5 | <5 | <5 | NA | U |
| CS16F47 | 47 | >2500 | 590 | 710 | 100 | 49 | M |
| CS17M56 | 56 | 80 | 7 | <5 | <5 | 24 | M and/or U |
| CS18F47 | 47 | <5 | <5 | <5 | <5 | 4.3 | M |
| CS18M13 | 13 | 7 | <5 | <5 | <5 | 4.3 | M |
| CS19F44 | 44 | <5 | <5 | <5 | <5 | 18.8 | M |
| CS19M51 | 51 | <5 | <5 | <5 | <5 | 18.8 | M |
| CS19M7 | 7 | <5 | <5 | <5 | <5 | 18.8 | M |
| CS19F4 | 4 | <5 | <5 | <5 | <5 | 18.8 | M |
| CS22F39 | 39 | 50 | <5 | 11 | <5 | 18 | M and/or U |
| CS22F4 | 4 | 200 | 15 | 40 | <5 | 18 | M and/or U |
| CS22M2 | 2 | 980 | 50 | 280 | 17 | 18 | M and/or U |
| CS23F41 | 41 | <5 | <5 | <5 | <5 | 14.7 | U |
| CS23F42 | 42 | 30 | <5 | <5 | <5 | 14.7 | U |
| CS23F7 | 7 | 13 | <5 | <5 | <5 | 14.7 | U |
| CS23F3 | 3 | 40 | <5 | <5 | <5 | 14.7 | U |
| CS24F8 | 8 | <5 | <5 | <5 | <5 | 6.6 | M and/or U |
| CS24M6 | 6 | 7 | <5 | <5 | <5 | 6.6 | M and/or U |
| CS24M0 | 0.66 | 80 | <5 | 16 | <5 | 6.6 | M and/or U |
| CS25M63 | 63 | <5 | <5 | <5 | <5 | 1.2 | M and/or U |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wright, J.; Kenneally, M.; Ross, K.; Walker, S. Environmental Methamphetamine Exposures and Health Effects in 25 Case Studies. Toxics 2020, 8, 61. https://doi.org/10.3390/toxics8030061
Wright J, Kenneally M, Ross K, Walker S. Environmental Methamphetamine Exposures and Health Effects in 25 Case Studies. Toxics. 2020; 8(3):61. https://doi.org/10.3390/toxics8030061
Chicago/Turabian StyleWright, Jackie, Michaela Kenneally, Kirstin Ross, and Stewart Walker. 2020. "Environmental Methamphetamine Exposures and Health Effects in 25 Case Studies" Toxics 8, no. 3: 61. https://doi.org/10.3390/toxics8030061
APA StyleWright, J., Kenneally, M., Ross, K., & Walker, S. (2020). Environmental Methamphetamine Exposures and Health Effects in 25 Case Studies. Toxics, 8(3), 61. https://doi.org/10.3390/toxics8030061





