Using Wearable Sensors to Assess Freezing of Gait in the Real World
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Equipment
2.4. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Task Instructions
- For the dual task portion of each task, give the participant a number greater than 100.
- Read the directions slowly and clearly, giving plenty of time for participants to comprehend what is being said.
- “You can have a seat while I explain this task. When I say ‘ready, set, go,’ walk out the door into the open box marked on the floor in the middle of the hallway. You will turn around inside the box, walk out of the box, and walk all the way around the outside of the box, and then return to the room. When you walk through the door, I will tell you which direction to turn.
- If I say to turn left, you will turn around inside the box toward your left like this [demonstrate]. You will then walk out of the box and make another left turn to walk around the outside of the box like this [demonstrate] before returning to the room.
- If I say to turn right, you will turn around inside the box toward your right like this [demonstrate]. You will then walk out of the box and make another right turn to walk around the outside of the box like this [demonstrate] before returning to the room.
Walk at a comfortable pace. Would you like me to demonstrate again? [Demonstrate if participant requests another demonstration.] Great, I will show you where to start. [Direct participant to assume starting position.]. Do you understand the instructions? [answer questions and ensure understanding before starting]. Great. When I want you to start, I will say “Ready, Set, Go.” Please wait for me to give the cue.” - “Please return to the starting position. [Direct participant.] I will tell you which direction to turn when you get to the door.”
- Repeat above.
- Repeat above.
- 5
- “I will tell you which direction to turn when you get to the door. This time, I want you to count backward while you walk. I will give you a number to start with. You will count backward by three. Please count out loud. If you make a mistake with counting, continue counting down by three as if nothing happened. When I want you to start, I will say ‘ready, set, [and then your number.]’ So, for example, I might say ‘ready, set, 243.’ When I do this, you will start counting backward by three from the number I give you and start walking, like this: “243, 240, 237, and so on” [Demonstrate walking while counting down]. Walk at a comfortable pace. Do you have any questions? [answer questions and ensure understanding before starting] Great, please wait for me to give the cue.”
- 6
- “Please return to the starting position. [Direct participant]. Start counting backward and walking when I give the cue.”
- 7
- Repeat above.
- 8
- Repeat above.
- “You can have a seat while I explain this task. When I say ‘ready, set, go,’ you will walk down the hallway. At some point while you’re walking, I will say “left” or “right.” [Begin walking away from participant.] When I say “left,” you will turn around toward your left like this [demonstrate turn] and continue walking in the opposite direction. [Begin walking away from participant.] When I say “right,” you will turn around toward your right like this [demonstrate] and continue walking in the opposite direction. Do not stop walking until I say the word “stop.” Walk at a comfortable pace. Would you like me to demonstrate again? [Demonstrate if participant requests another demonstration.] Great, I will show you where to start. [Direct participant to starting position.] Do you understand the instructions? [answer questions and ensure understanding before starting]. Great, please wait for me to give the cue.”
- “We will start from here this time. [Direct participant.] Great, please wait for me to give the cue.”
- Repeat above.
- Repeat above.
- 5
- “This time, I want you to count backward while you walk. I will give you a number to start with. You will count backward by three. Please count out loud. If you make a mistake with counting, continue counting down by three as if nothing happened. When I want you to start, I will say ‘ready, set, [and then your number.]’ So, for example, I might say ‘ready, set, 243.’ When I do this, you will start counting backward by three from the number I give you and start walking, like this: “243, 240, 237, and so on” [Demonstrate walking while counting down]. Walk at a comfortable pace. Do you have any questions? [answer questions and ensure understanding before starting.] Great, please wait for me to give the cue.
- 6
- “We will start from here this time. [Direct participant]. Start counting backward and walking when I give the cue.”
- 7
- Repeat above.
- 8
- Repeat above.
- “You can have a seat while I explain this task. When I say ‘right,’ I want you to make a complete turn to the right, like this [demonstrate]. When I say ‘left,’ I want you to make a complete turn to the left, like this [demonstrate]. In other words, each time I say ‘right’ or ‘left’ you will make a complete turn in that direction. Turn at a comfortable pace. If you start to feel dizzy, let me know, and we can pause the test. Would you like me to demonstrate again? [Demonstrate if participant requests another demonstration.] Great, I will show you where to start. [Direct participant to starting position.] Do you understand the instructions? [answer questions and ensure understanding before starting]. Great, please wait for me to give the cue.” [Cue: “Ready, set, right/left.”]
- “Right/left”
- “Right/left”
- “Right/left” [After participant completes turn: “Ok you can stop and take a step back now.”]
- 5
- “This time, I want you to count backward while you turn. I will give you a number to start with. You will count backward by three. Please count out loud. If you make a mistake with counting, continue counting down by three as if nothing happened. When I want you to start counting, I will say ‘ready, set, [and then your number.]’ So, for example, I might say ‘ready, set, 243.’ When I do this, you will start counting backward by three from the number I give you, like this: “243, 240, 237, and so on”. While you are counting backward, I will say either ‘right’ or ‘left’ several times and you will make a complete turn in whichever direction I say. Turn at a comfortable pace. Do you have any questions? [answer questions and ensure understanding before starting.] Great, please wait for me to give your number. [Cue: “Ready, set, number.”] [After participant successfully subtracts by three twice, state “right/left.”]
- 6
- “Right/left”
- 7
- “Right/left”
- 8
- “Right/left” [After participant completes turn: “Ok you can stop and take a seat now.”]
Appendix B. Gait Up Physilog Home Instructions
- -
- The rest of the day after you leave the lab (Day 0: _________)
- -
- The first day after your lab testing day (Day 1: _________)
- -
- The second day after your lab testing day (Day 2: _________)
- -
- The third day after your lab testing day (Day 3: _________)
- TAKE THE SENSORS OFF.
- -
- Take the hip sensor pouch off your belt or pants. Leave the shoe sensor pouches on the shoes. Take the sensors out of the pouches to charge them.
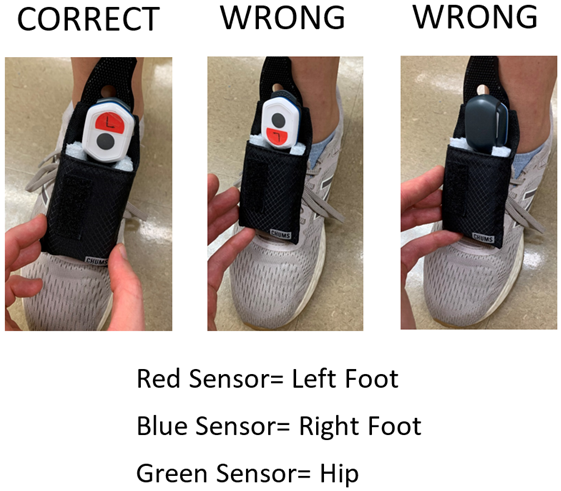
- TURN THE SENSORS OFF
- -
- Press the button on one sensor (any sensor) and hold it pressed until the light changes from green to orange (about 1 s). If you hold the button down too long (over 5 s) this will cause the sensors to reset, and any data you’ve collected will be lost.
- -
- Confirm the light is steadily off. If the light is flashing, repeat the above step or call Pietro or David (numbers above)
- -
- Repeat the above steps for the remaining 2 sensors
- CHARGE THE SENSORS
- -
- Plug a cable into each sensor and connect to a wall outlet
- -
- The sensors will flash purple for a few hours. They will change to steady green to indicate they have completed charging.
- CONFIRM THE SENSORS ARE FULLY CHARGED.
- -
- If they are fully charged, the light on each sensor will be a steady green, and you can unplug the sensors.
- -
- If the lights are not steady green, let them keep charging and call Pietro or David (numbers above).
- TURN THE SENSORS ON
- -
- Press the button on one sensor (any sensor) and hold it pressed until the green light turns off (about 1 s)
- -
- Confirm that the light is flashing green (about every second; each flash is very fast and faint; this is normal).
- -
- After a few seconds, the 3 sensors’ lights should be flashing green all at the same time.
- -
- If the 3 lights are not flashing green at the same time, turn each sensor off and repeat the above steps, or call Pietro Mazzoni (number above)
- WEAR THE SENSORS
- -
- Fasten the hip sensor pouch on your belt, near your left hip
- -
- Place each sensor in its pouch.
- ○
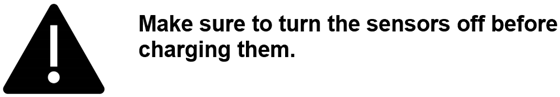
- Be sure to put the left foot sensor on the participant’s left foot and the right foot sensor on the participant’s right foot.
- ○
- Be sure to put each sensor in its pouch with the sticker facing away from the participant’s body. Do not put the sensors in the pouch upside down. See images below.
- -
- At the end of day 3: turn the sensors off and charge them. Let them stay plugged in and charging until a research team member is ready to pick them up.
- -
- Take the pouches off your shoes and pants or belt. If you cannot get the pouches off the shoes, a research team member will be happy to do it for you when we pick the sensors up.
- -
- Place the 3 sensors, the pouches, and the charging cables in the box provided.
- -
- Wait for a phone call from Pietro or David who will provide instructions on how to return the sensors
Appendix C. Actigraph Link Home Instructions
- -
- The rest of the day after you leave the lab (Day 0: _________)
- -
- The first day after your lab testing day (Day 1: _________)
- -
- The second day after your lab testing day (Day 2: _________)
- -
- The third day after your lab testing day (Day 3: _________)


- The left foot sensor goes on the participant’s left foot.
- The right foot sensor goes on the participant’s right foot.
- The hip sensor goes on the participant’s left hip (clipped to belt).
- TAKE THE SENSORS OFF.
- -
- Take the hip sensor pouch off your belt or pants. Leave the shoe sensor pouches on the shoes. Take the sensors out of the pouches to charge them.
- CHARGE THE SENSORS
- -
- Plug each of the three charging docks in to a wall outlet
- -
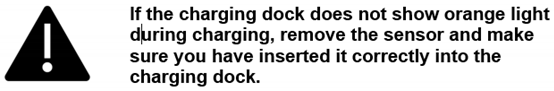
- Place each sensor on a charging dock as shown below.
- -
- Charging dock should light up orange. This will change to green when they are fully charged.

- CONFIRM THE SENSORS ARE FULLY CHARGED.
- -
- If they are fully charged, the light on each charging dock will be a steady green, and you can unplug the sensors.
- -
- If the lights are not steady green, let them keep charging and call Pietro or David (numbers above).
- WEAR THE SENSORS
- -
- Fasten the hip sensor pouch on your belt, near your left hip
- -
- Place each sensor in its pouch.
- ○
- Be sure to put the left foot sensor on the participant’s left foot and the right foot sensor on the participant’s right foot.
- ○
- Be sure to put each sensor in its pouch with the front side (screen side) facing away from the participant’s body. Do not put the sensors in the pouch upside down. See images below.
- -
- At the end of day 3: place the sensors on the chargers. Let them stay plugged in and charging until a research team member is ready to pick them up.
- -
- A research team member will assist you with taking the pouches off the shoes unless otherwise instructed.
- -
- Place the 3 sensors, the pouches, the charging docks, and charging cables in the box provided.
- -
- Wait for a phone call from Pietro or David who will provide instructions on how to return the sensors.
References
- Giladi, N.; Nieuwboer, A. Understanding and treating freezing of gait in parkinsonism, proposed working definition, and setting the stage. Mov. Disord. 2008, 23, S423–S425. [Google Scholar] [CrossRef] [PubMed]
- Nutt, J.G.; Bloem, B.R.; Giladi, N.; Hallett, M.; Horak, F.B.; Nieuwboer, A. Freezing of gait: Moving forward on a mysterious clinical phenomenon. Lancet Neurol. 2011, 10, 734–744. [Google Scholar] [CrossRef] [PubMed]
- Giladi, N.; McMahon, D.; Przedborski, S.; Flaster, E.; Guillory, S.; Kostic, V.; Fahn, S. Motor blocks in Parkinson’s disease. Neurology 1992, 42, 333. [Google Scholar] [CrossRef]
- Schaafsma, J.D.; Balash, Y.; Gurevich, T.; Bartels, A.L.; Hausdorff, J.M.; Giladi, N. Characterization of freezing of gait subtypes and the response of each to levodopa in Parkinson’s disease. Eur. J. Neurol. 2003, 10, 391–398. [Google Scholar] [CrossRef] [Green Version]
- Snijders, A.H.; Nijkrake, M.J.; Bakker, M.; Munneke, M.; Wind, C.; Bloem, B.R. Clinimetrics of freezing of gait. Mov. Disord. 2008, 23 (Suppl. S2), S468–S474. [Google Scholar] [CrossRef]
- Mancini, M.; Bloem, B.R.; Horak, F.B.; Lewis, S.J.; Nieuwboer, A.; Nonnekes, J. Clinical and methodological challenges for assessing freezing of gait: Future perspectives. Mov. Disord. 2019, 34, 783–790. [Google Scholar] [CrossRef]
- Hallett, M. The intrinsic and extrinsic aspects of freezing of gait. Mov. Disord. 2008, 23, S439–S443. [Google Scholar] [CrossRef] [Green Version]
- Redgrave, P.; Rodriguez, M.; Smith, Y.; Rodriguez-Oroz, M.C.; Lehericy, S.; Bergman, H.; Agid, Y.; DeLong, M.R.; Obeso, J.A. Goal-directed and habitual control in the basal ganglia: Implications for Parkinson’s disease. Nat. Rev. Neurosci. 2010, 11, 760–772. [Google Scholar] [CrossRef] [Green Version]
- Martens, K.E.; Ellard, C.G.; Almeida, Q.J. Does Anxiety Cause Freezing of Gait in Parkinson’s Disease? PLoS ONE 2014, 9, e106561. [Google Scholar] [CrossRef] [Green Version]
- Martens, K.A.E.; Lukasik, E.L.; Georgiades, M.J.; Gilat, M.; Hall, J.; Walton, C.; Lewis, S. Predicting the onset of freezing of gait: A longitudinal study. Mov. Disord. 2018, 33, 128–135. [Google Scholar] [CrossRef]
- Nieuwboer, A.; Rochester, L.; Herman, T.; Vandenberghe, W.; Emil, G.E.; Thomaes, T.; Giladi, N. Reliability of the new freezing of gait questionnaire: Agreement between patients with Parkinson’s disease and their carers. Gait Posture 2009, 30, 459–463. [Google Scholar] [CrossRef]
- Bloem, B.R.; Marinus, J.; Almeida, Q.; Dibble, L.; Nieuwboer, A.; Post, B.; Růžička, E.; Goetz, C.; Stebbins, G.; Martinez-Martin, P.; et al. Measurement instruments to assess posture, gait, and balance in Parkinson’s disease: Critique and recommendations. Mov. Disord. 2016, 31, 1342–1355. [Google Scholar] [CrossRef] [PubMed]
- Shine, J.; Moore, S.; Bolitho, S.; Morris, T.; Dilda, V.; Naismith, S.; Lewis, S. Assessing the utility of Freezing of Gait Questionnaires in Parkinson’s Disease. Park. Relat. Disord. 2012, 18, 25–29. [Google Scholar] [CrossRef]
- Hulzinga, F.; Nieuwboer, A.; Dijkstra, B.W.; Mancini, M.; Strouwen, C.; Bloem, B.R.; Ginis, P. The New Freezing of Gait Questionnaire: Unsuitable as an Outcome in Clinical Trials? Mov. Disord. Clin. Pr. 2020, 7, 199–205. [Google Scholar] [CrossRef] [PubMed]
- Prateek, G.V.; Skog, I.; McNeely, M.E.; Duncan, R.P.; Earhart, G.M.; Nehorai, A. Modeling, Detecting, and Tracking Freezing of Gait in Parkinson Disease Using Inertial Sensors. IEEE Trans. Biomed. Eng. 2018, 65, 2152–2161. [Google Scholar] [CrossRef]
- Prateek, G.V.; Mazzoni, P.; Earhart, G.M.; Nehorai, A. Gait Cycle Validation and Segmentation Using Inertial Sensors. IEEE Trans. Biomed. Eng. 2019, 67, 2132–2144. [Google Scholar] [CrossRef]
- Gundannavar Vijay, P. A Modular Approach for Modeling, Detecting, and Tracking Freezing of Gait in Parkinson Disease Using Inertial Sensors. Ph.D. Thesis, Washington University in St. Louis—McKelvey School of Engineering, St. Louis, MO, USA, August 2019. [Google Scholar] [CrossRef]
- Mancini, M.; Shah, V.V.; Stuart, S.; Curtze, C.; Horak, F.B.; Safarpour, D.; Nutt, J.G. Measuring freezing of gait during daily-life: An open-source, wearable sensors approach. J. Neuroeng. Rehabilitation 2021, 18, 1. [Google Scholar] [CrossRef]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-Mental State”. A Practical Method for Grading the Cognitive State of Patients for the Clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Goetz, C.G.; Tilley, B.C.; Shaftman, S.R.; Stebbins, G.T.; Fahn, S.; Martinez-Martin, P.; Poewe, W.; Sampaio, C.; Stern, M.B.; Dodel, R.; et al. Movement Disorder Society-sponsored revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS): Scale presentation and clinimetric testing results. Mov. Disord. 2008, 23, 2129–2170. [Google Scholar] [CrossRef]
- Ziegler, K.; Schroeteler, F.; Ceballos-Baumann, A.O.; Fietzek, U.M. A new rating instrument to assess festination and freezing gait in Parkinsonian patients. Mov. Disord. 2010, 25, 1012–1018. [Google Scholar] [CrossRef] [PubMed]
- Van Rossum, G.; Drake, F.L. Python 3 Reference Manual; CreateSpace: Scotts Valley, CA, USA, 2009. [Google Scholar]
- The Pandas Development Team. Pandas-Dev/Pandas: Pandas. Zenodo, May 2022. Available online: https://doi.org/10.5281/zenodo.3509134 (accessed on 2 September 2021).
- Harris, C.R.; Millman, K.J.; van der Walt, S.J.; Gommers, R.; Virtanen, P.; Cournapeau, D.; Wieser, E.; Taylor, J.; Berg, S.; Smith, N.J.; et al. Array programming with NumPy. Nature 2020, 585, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Virtanen, P.; Gommers, R.; Oliphant, T.E.; Haberland, M.; Reddy, T.; Cournapeau, D.; Burovski, E.; Peterson, P.; Weckesser, W.; Bright, J.; et al. SciPy 1.0 Contributors. SciPy 1.0 Fundamental Algorithms for Scientific Computing in Python. Nat. Methods 2020, 17, 261–272. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lundh, F. An Introduction to Tkinter. 1999. Available online: https://docs.python.org/pl/3.8/library/tkinter.html (accessed on 16 September 2021).
- Hunter, J.D. Matplotlib: A 2D graphics environment. Comput. Sci. Eng. 2007, 9, 90–95. [Google Scholar] [CrossRef]
- Waskom, M.L. seaborn: Statistical data visualization. J. Open Source Softw. 2021, 6, 3021. [Google Scholar] [CrossRef]
- Cicceri, G.; De Vita, F.; Bruneo, D.; Merlino, G.; Puliafito, A. A deep learning approach for pressure ulcer prevention using wearable computing. Human-centric Comput. Inf. Sci. 2020, 10, 5. [Google Scholar] [CrossRef]
- Babli, M.; Rincón-Arango, J.; Onaindia De La Rivaherrera, E.; Carrascosa Casamayor, C.; Julian, V. Deliberative Context-Aware Ambient Intelligence System for Assisted Living Homes. Hum. Cent. Comput. Inf. Sci. 2021, 11, 1–18. [Google Scholar] [CrossRef]
- Wang, J.; Yang, Y.; Wang, T.; Sherratt, R.S.; Zhang, J. Big Data Service Architecture: A Survey. J. Internet Technol. 2020, 21, 393–405. [Google Scholar]
- Lee, S.; Park, D. Adaptive ECG Signal Compression Method Based on Look-Ahead Linear Approximation for Ultra Long-Term Operating of Healthcare IoT Devices. Hum. Cent. Comput. Inf. Sci. 2021, 11, 30. [Google Scholar] [CrossRef]
- Jingyu, Z.; Siqi, Z.; Wang, T.; Chao, H.C.; Wang, J. Blockchain-based Systems and Applications: A Survey. J. Internet Technol. 2020, 21, 1–14. [Google Scholar]
- Pu, B.; Li, K.; Li, S.; Zhu, N. Automatic Fetal Ultrasound Standard Plane Recognition Based on Deep Learning and IIoT. IEEE Trans. Ind. Informatics 2021, 17, 7771–7780. [Google Scholar] [CrossRef]
- Denk, D.; Herman, T.; Zoetewei, D.; Ginis, P.; Brozgol, M.; Thumm, P.C.; Decaluwe, E.; Ganz, N.; Palmerini, L.; Giladi, N.; et al. Daily-Living Freezing of Gait as Quantified Using Wearables in People With Parkinson Disease: Comparison With Self-Report and Provocation Tests. Phys. Ther. 2022, 102, pzac129. [Google Scholar] [CrossRef] [PubMed]


| Participant Demographics, n = 19 | |
|---|---|
| Age in years (mean ± SD) | 71.95 ± 7.21 |
| Sex (males, females) | M = 13, F = 6 |
| MDS-UPDRS-III Score (mean ± SD) | 41.89 ± 13.45 |
| Hoehn and Yahr Stages (Stage 2, 3, 4) | n = 8, n = 9, n = 2 |
| Levodopa Equivalent Daily Dose (mean ± SD) | 955.2 ± 602.5 |
| New Freezing of Gait Questionnaire Score | 18.63 ± 4.98 |
| Sensor-Based FOG Detection Accuracy, n = 19 | |
|---|---|
| Vacuum Task | 95.37% ± 5.03% |
| Dish Task | 93.43% ± 10.48% |
| Sitting Task | 98.60% ± 5.49% |
| Community Task | 95.95% ± 5.29% |
| In-Person Lab Visit (Clinic FOG Tasks + Simulated IADL Tasks) | 90.38% ± 8.57% |
| Percent of Active Time Spent Freezing (%ATSF), n = 19 | |
|---|---|
| Sensors: In-Person Visit (Clinic FOG Tasks + Simulated IADL Tasks) | 6.36 ± 7.31 |
| Sensors: Simulated IADL Tasks | 1.84 ± 3.25 |
| Sensors: Home | 1.94 ± 3.06 |
| Video Review: In-Person Visit (Clinic FOG Tasks + Simulated IADL Tasks) | 11.22 ± 11.08 |
| Video Review: Simulated IADL Tasks | 1.90 ± 2.68 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
May, D.S.; Tueth, L.E.; Earhart, G.M.; Mazzoni, P. Using Wearable Sensors to Assess Freezing of Gait in the Real World. Bioengineering 2023, 10, 289. https://doi.org/10.3390/bioengineering10030289
May DS, Tueth LE, Earhart GM, Mazzoni P. Using Wearable Sensors to Assess Freezing of Gait in the Real World. Bioengineering. 2023; 10(3):289. https://doi.org/10.3390/bioengineering10030289
Chicago/Turabian StyleMay, David S., Lauren E. Tueth, Gammon M. Earhart, and Pietro Mazzoni. 2023. "Using Wearable Sensors to Assess Freezing of Gait in the Real World" Bioengineering 10, no. 3: 289. https://doi.org/10.3390/bioengineering10030289
APA StyleMay, D. S., Tueth, L. E., Earhart, G. M., & Mazzoni, P. (2023). Using Wearable Sensors to Assess Freezing of Gait in the Real World. Bioengineering, 10(3), 289. https://doi.org/10.3390/bioengineering10030289








