Biomechanical Effects of Different Sitting Postures and Physiologic Movements on the Lumbar Spine: A Finite Element Study
Abstract
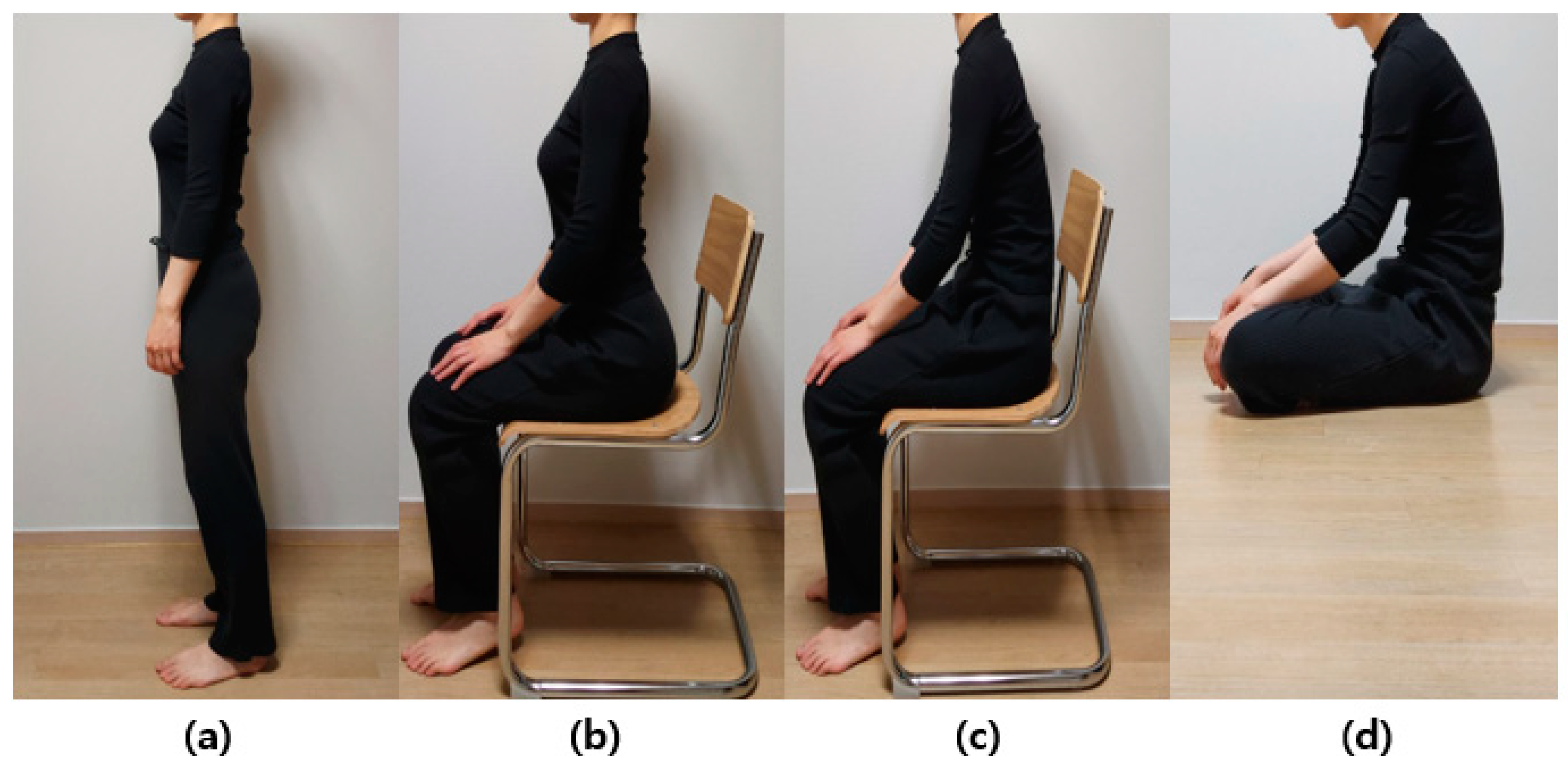
:1. Introduction
2. Materials and Methods
2.1. Development of the FEM
2.2. Mesh and Material Properties for the FEM
2.3. Loading and Boundary Conditions
3. Results
3.1. Flexion Mode
3.2. Lateral Bending Mode
3.3. Axial Rotation Mode
3.4. Von Mises Stress According to the Three Load Modes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Waxenbaum, J.A.; Reddy, V.; Williams, C.; Futterman, B. Anatomy, Back, Lumbar Vertebrae; StatPearls Publishing: St. Petersburg, FL, USA, 2017. [Google Scholar]
- Galbusera, F.; Wilke, H.-J. Biomechanics of the Spine: Basic Concepts, Spinal Disorders and Treatments; Academic Press: Cambridge, MA, USA, 2018. [Google Scholar]
- Iyer, S.; Sheha, E.; Fu, M.C.; Varghese, J.; Cunningham, M.E.; Albert, T.J.; Schwab, F.J.; Lafage, V.C.; Kim, H.J. Sagittal spinal alignment in adult spinal deformity: An overview of current concepts and a critical analysis review. JBJS Rev. 2018, 6, e2. [Google Scholar] [CrossRef]
- Hills, J.; Lenke, L.G.; Sardar, Z.M.; Le Huec, J.C.; Bourret, S.; Hasegawa, K.; Wong, H.K.; Hey, H.W.; Liu, G.; Riahi, H.; et al. The T4-L1-Hip Axis: Defining a Normal Sagittal Spinal Alignment. Spine 2022, 47, 1399–1406. [Google Scholar] [CrossRef] [PubMed]
- Williams, S.A.; Russo, G.A. Evolution of the hominoid vertebral column: The long and the short of it. Evol. Anthropol. Issues News Rev. 2015, 24, 15–32. [Google Scholar] [CrossRef] [PubMed]
- Sparrey, C.J.; Bailey, J.F.; Safaee, M.; Clark, A.J.; Lafage, V.; Schwab, F.; Smith, J.S.; Ames, C.P. Etiology of lumbar lordosis and its pathophysiology: A review of the evolution of lumbar lordosis, and the mechanics and biology of lumbar degeneration. Neurosurg. Focus 2014, 36, E1. [Google Scholar] [CrossRef]
- Tsagkaris, C.; Widmer, J.; Wanivenhaus, F.; Redaelli, A.; Lamartina, C.; Farshad, M. The sitting vs standing spine. N. Am. Spine Soc. J. 2022, 9, 100108. [Google Scholar] [CrossRef]
- Endo, K.; Suzuki, H.; Tanaka, H.; Kang, Y.; Yamamoto, K. Sagittal spinal alignment in patients with lumbar disc herniation. Eur. Spine J. 2010, 19, 435–438. [Google Scholar] [CrossRef]
- Shin, J.J.; Kim, B.; Kang, J.; Choi, J.; Moon, B.J.; Ryu, D.S.; Yoon, S.H.; Chin, D.K.; Lee, J.K.; Kim, K.N.; et al. Clinical, Radiographic, and Genetic Analyses in a Population-Based Cohort of Adult Spinal Deformity in the Older Population. Neurospine 2021, 18, 608–617. [Google Scholar] [CrossRef] [PubMed]
- Otluoglu, G.D.; Konya, D.; Toktas, Z.O. The Influence of Mechanic Factors in Disc Degeneration Disease as a Determinant for Surgical Indication. Neurospine 2020, 17, 215–220. [Google Scholar] [CrossRef]
- Araújo, A.; Peixinho, N.; Pinho, A.; Claro, J.C.P. On the experimental intradiscal pressure measurement techniques: A review. New Trends Mech. Mach. Sci. 2015, 243–250. [Google Scholar] [CrossRef]
- Nachemson, A. The load on lumbar disks in different positions of the body. Clin. Orthop. Relat. Res. (1976–2007) 1966, 45, 107–122. [Google Scholar] [CrossRef]
- Goto, K.; Tajima, N.; Chosa, E.; Totoribe, K.; Kuroki, H.; Arizumi, Y.; Arai, T. Mechanical analysis of the lumbar vertebrae in a three-dimensional finite element method model in which intradiscal pressure in the nucleus pulposus was used to establish the model. J. Orthop. Sci. 2002, 7, 243–246. [Google Scholar] [CrossRef] [PubMed]
- Li, J.-Q.; Kwong, W.-H.; Chan, Y.-L.; Kawabata, M. Comparison of in vivo intradiscal pressure between sitting and standing in human lumbar spine: A systematic review and meta-analysis. Life 2022, 12, 457. [Google Scholar] [CrossRef] [PubMed]
- Nachemson, A.; Morris, J.M. In Vivo Measurements of Intradiscal Pressure. Discometry, a Method for the Determination of Pressure in the Lower Lumbar Discs. J. Bone Joint Surg. Am. 1964, 46, 1077–1092. [Google Scholar] [CrossRef] [PubMed]
- Wilke, H.J.; Neef, P.; Caimi, M.; Hoogland, T.; Claes, L.E. New in vivo measurements of pressures in the intervertebral disc in daily life. Spine 1999, 24, 755–762. [Google Scholar] [CrossRef]
- Matthews, C.E.; Chen, K.Y.; Freedson, P.S.; Buchowski, M.S.; Beech, B.M.; Pate, R.R.; Troiano, R.P. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am. J. Epidemiol. 2008, 167, 875–881. [Google Scholar] [CrossRef]
- Hong, J.-H.; Han, M.-S.; Lee, S.-K.; Lee, J.-K.; Moon, B.J. Is the agricultural work a risk factor for Koreans elderly spinal sagittal imbalance? J. Korean Neurosurg. Soc. 2020, 63, 623–630. [Google Scholar] [CrossRef]
- Lee, S.-H.; Kim, K.-T.; Suk, K.-S.; Lee, J.-H.; Seo, E.-M.; Huh, D.-S. Sagittal decompensation after corrective osteotomy for lumbar degenerative kyphosis: Classification and risk factors. Spine 2011, 36, E538–E544. [Google Scholar] [CrossRef]
- Lee, C.-S.; Kim, Y.-T.; Kim, E. Clinical study of lumbar degenerative kyphosis. J. Korean Soc. Spine Surg. 1997, 4, 27–35. [Google Scholar]
- Jain, P.; Khan, M.R. Comparison of novel stabilisation device with various stabilisation approaches: A finite element based biomechanical analysis. Int. J. Artif. Organs 2022, 45, 514–522. [Google Scholar] [CrossRef]
- Jain, P.; Rana, M.; Biswas, J.K.; Khan, M.R. Biomechanics of spinal implants—A review. Biomed. Phys. Eng. Express 2020, 6, 042002. [Google Scholar] [CrossRef]
- Wolf, A.; Shoham, M.; Michael, S.; Moshe, R. Morphometric study of the human lumbar spine for operation–workspace specifications. Spine 2001, 26, 2472–2477. [Google Scholar] [CrossRef] [PubMed]
- Bae, J.S.; Jang, J.-S.; Lee, S.-H.; Kim, J.U. A comparison study on the change in lumbar lordosis when standing, sitting on a chair, and sitting on the floor in normal individuals. J. Korean Neurosurg. Soc. 2012, 51, 20–23. [Google Scholar] [CrossRef] [PubMed]
- Song, S.-Y.; Kang, S.W.; Cho, S.H.; Heo, S.-J.; Cho, M.G.; Park, Y.-J.; Oh, S.H.; Jung, G.-H.; Kim, D.-H. Effects of Location and Volume of Intraosseous Cement on Adjacent Level of Osteoporotic Spine Undergoing Kyphoplasty: Finite Element Analysis. World Neurosurg. 2022, 162, e73–e85. [Google Scholar] [CrossRef]
- Cho, I.Y.; Park, S.Y.; Park, J.H.; Kim, T.K.; Jung, T.W.; Lee, H.M. The effect of standing and different sitting positions on lumbar lordosis: Radiographic study of 30 healthy volunteers. Asian Spine J. 2015, 9, 762. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.; Park, C.-H.; Jung, H.; Lee, S.; Min, Y.-S.; Kim, C.-H.; Cho, M.; Jung, G.-H.; Kim, D.-H.; Kim, K.-T. Analysis of the physiological load on lumbar vertebrae in patients with osteoporosis: A finite-element study. Sci. Rep. 2022, 12, 11001. [Google Scholar] [CrossRef]
- Cho, A.-R.; Cho, S.-B.; Jae-Ho, L.; Kim, K.-H. Effect of augmentation material stiffness on adjacent vertebrae after osteoporotic vertebroplasty using finite element analysis with different loading methods. Pain Physician 2015, 18, E1101. [Google Scholar] [CrossRef]
- Jeon, T.-S.; Kim, S.-B.; Park, W.-K. Lordoplasty: An alternative technique for the treatment of osteoporotic compression fracture. Clin. Orthop. Surg. 2011, 3, 161–166. [Google Scholar] [CrossRef]
- Andersson, G.; Ortengren, R.; Nachemson, A. Quantitative studies of the load on the back in different working-postures. Scand. J. Rehabil. Med. 1978, 6, 173–181. [Google Scholar]
- Lord, M.J.; Small, J.M.; Dinsay, J.M.; Watkins, R.G. Lumbar lordosis. Effects of sitting and standing. Spine 1997, 22, 2571–2574. [Google Scholar] [CrossRef]
- Cao, K.D.; Grimm, M.J.; Yang, K.-H. Load sharing within a human lumbar vertebral body using the finite element method. Spine 2001, 26, e253–e260. [Google Scholar] [CrossRef]
- Lu, Y.; Rosenau, E.; Paetzold, H.; Klein, A.; Püschel, K.; Morlock, M.M.; Huber, G. Strain changes on the cortical shell of vertebral bodies due to spine ageing: A parametric study using a finite element model evaluated by strain measurements. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2013, 227, 1265–1274. [Google Scholar] [CrossRef] [PubMed]
- Christiansen, B.A.; Kopperdahl, D.L.; Kiel, D.P.; Keaveny, T.M.; Bouxsein, M.L. Mechanical contributions of the cortical and trabecular compartments contribute to differences in age-related changes in vertebral body strength in men and women assessed by QCT-based finite element analysis. J. Bone Miner. Res. 2011, 26, 974–983. [Google Scholar] [CrossRef] [PubMed]
- Palepu, V.; Rayaprolu, S.D.; Nagaraja, S. Differences in trabecular bone, cortical shell, and endplate microstructure across the lumbar spine. Int. J. Spine Surg. 2019, 13, 361–370. [Google Scholar] [CrossRef]
- Watanabe, S.; Kobara, K.; Ishida, H.; Eguchi, A. Influence of trunk muscle co-contraction on spinal curvature during sitting cross-legged. Electromyogr. Clin. Neurophysiol. 2010, 50, 187–192. [Google Scholar] [PubMed]
- Moon, M.-S.; Lee, H.; Kim, S.-T.; Kim, S.-J.; Kim, M.-S.; Kim, D.-S. Spinopelvic orientation on radiographs in various body postures: Upright standing, chair sitting, Japanese style kneel sitting, and Korean style cross-legged sitting. Clin. Orthop. Surg. 2018, 10, 322–327. [Google Scholar] [CrossRef]
- Wang, W.; Pei, B.; Wu, S.; Lu, D.; He, P.; Ma, C.; Wu, X. Biomechanical responses of human lumbar spine and pelvis according to the Roussouly classification. PLoS ONE 2022, 17, e0266954. [Google Scholar] [CrossRef] [PubMed]
- Takemitsu, Y.; Harada, Y.; Iwahara, T.; Miyamoto, M.; Miyatake, Y. Lumbar degenerative kyphosis. Clinical, radiological and epidemiological studies. Spine 1988, 13, 1317–1326. [Google Scholar] [CrossRef]
- Jang, J.-S.; Lee, S.-H.; Min, J.-H.; Han, K.-M. Lumbar degenerative kyphosis: Radiologic analysis and classifications. Spine 2007, 32, 2694–2699. [Google Scholar] [CrossRef]
- Mardare, M.; Oprea, M.; Popa, I.; Zazgyva, A.; Niculescu, M.; Poenaru, D.V. Sagittal balance parameters correlate with spinal conformational type and MRI changes in lumbar degenerative disc disease: Results of a retrospective study. Eur. J. Orthop. Surg. Traumatol. 2016, 26, 735–743. [Google Scholar] [CrossRef]
- Yang, X.; Kong, Q.; Song, Y.; Liu, L.; Zeng, J.; Xing, R. The characteristics of spinopelvic sagittal alignment in patients with lumbar disc degenerative diseases. Eur. Spine J. 2014, 23, 569–575. [Google Scholar] [CrossRef]
- Miura, T.; Hongo, M.; Kasukawa, Y.; Kijima, H.; Kudo, D.; Saito, K.; Kimura, R.; Iwami, T.; Miyakoshi, N. Relationship between intervertebral disc compression force and sagittal spinopelvic lower limb alignment in elderly women in standing position with patient-specific whole body musculoskeletal model. Int. J. Environ. Res. Public Health 2022, 19, 16452. [Google Scholar] [CrossRef] [PubMed]
- Pourabbas Tahvildari, B.; Masroori, Z.; Erfani, M.A.; Solooki, S.; Vosoughi, A.R. The impact of spino-pelvic parameters on pathogenesis of lumbar disc herniation. Musculoskelet. Surg. 2022, 106, 195–199. [Google Scholar] [CrossRef] [PubMed]
- Williams, M.M.; Hawley, J.A.; Mckenzie, R.A.; van Wijmen, P.M. A comparison of the effects of two sitting postures on back and referred pain. Spine 1991, 16, 1185–1191. [Google Scholar] [CrossRef] [PubMed]
- Aota, Y.; Iizuka, H.; Ishige, Y.; Mochida, T.; Yoshihisa, T.; Uesugi, M.; Saito, T. Effectiveness of a lumbar support continuous passive motion device in the prevention of low back pain during prolonged sitting. Spine 2007, 32, E674–E677. [Google Scholar] [CrossRef] [PubMed]
- Moriguchi, C.S.; Sato, T.O.; Coury, H. An Instrumented Workstation to Evaluate Weight-Bearing Distribution in the Sitting Posture. Saf. Health Work 2019, 10, 314–320. [Google Scholar] [CrossRef]
- Izzo, R.; Guarnieri, G.; Guglielmi, G.; Muto, M. Biomechanics of the spine. Part I: Spinal stability. Eur. J. Radiol. 2013, 82, 118–126. [Google Scholar] [CrossRef]
- Mosabbir, A. Mechanisms behind the development of chronic low back pain and its neurodegenerative features. Life 2022, 13, 84. [Google Scholar] [CrossRef]
- Kang, S.; Chang, M.C.; Kim, H.; Kim, J.; Jang, Y.; Park, D.; Hwang, J.-m. The effects of paraspinal muscle volume on physiological load on the lumbar vertebral column: A finite-element study. Spine 2021, 46, E1015–E1021. [Google Scholar] [CrossRef]
- Wang, K.; Deng, Z.; Chen, X.; Shao, J.; Qiu, L.; Jiang, C.; Niu, W. The role of multifidus in the biomechanics of lumbar spine: A musculoskeletal modeling study. Bioengineering 2023, 10, 67. [Google Scholar] [CrossRef]
- Waongenngarm, P.; Rajaratnam, B.S.; Janwantanakul, P. Perceived body discomfort and trunk muscle activity in three prolonged sitting postures. J. Phys. Ther. Sci. 2015, 27, 2183–2187. [Google Scholar] [CrossRef]
- Wong, A.Y.; Chan, T.P.; Chau, A.W.; Cheung, H.T.; Kwan, K.C.; Lam, A.K.; Wong, P.Y.; De Carvalho, D. Do different sitting postures affect spinal biomechanics of asymptomatic individuals? Gait Posture 2019, 67, 230–235. [Google Scholar] [CrossRef] [PubMed]






| Component | Number of Nodes | Number of Elements | Elastic Modulus (MPa) | Poisson Ratio | Reference |
|---|---|---|---|---|---|
| Cortical bone | 210,671 | 117,993 | 12,000 | 0.3 | [28] |
| Cancellous bone | 36,063 | 20,061 | 200 | 0.25 | [28] |
| Posterior element | 70,248 | 38,010 | 3500 | 0.25 | [28] |
| End plate | 44,100 | 21,009 | 1000 | 0.3 | [28] |
| Nucleus pulposus | 22,147 | 11,709 | 1 | 0.49 | [28] |
| Annulus fiber | 36,352 | 18,434 | 4.2 | 0.45 | [28] |
| Facet joint | 2222 | 990 | 11 | 0.4 | [29] |
| Average (MPa) | |||||
|---|---|---|---|---|---|
| Flexion | |||||
| Standing | Erect Sitting | Slumped Sitting | Sitting on the Floor | ||
| Cortical Bone | L1 | 4.34 | 3.25 | 6.40 | 7.17 |
| L2 | 4.40 | 5.02 | 15.90 | 9.89 | |
| L3 | 2.38 | 2.62 | 11.09 | 4.69 | |
| L4 | 2.56 | 2.58 | 9.77 | 4.76 | |
| L5 | 1.82 | 3.71 | 7.11 | 3.82 | |
| Annulus fiber | L2-L1 | 0.33 | 0.27 | 0.50 | 0.54 |
| L3-L2 | 0.22 | 0.29 | 0.42 | 0.56 | |
| L4-L3 | 0.18 | 0.25 | 0.28 | 0.49 | |
| L5-L4 | 0.31 | 0.45 | 0.15 | 0.67 | |
| S-L5 | 0.16 | 0.19 | 0.07 | 0.25 | |
| Nucleus pulposus | L2-L1 | 0.08 | 0.06 | 0.15 | 0.13 |
| L3-L2 | 0.05 | 0.06 | 0.09 | 0.15 | |
| L4-L3 | 0.05 | 0.06 | 0.07 | 0.10 | |
| L5-L4 | 0.07 | 0.09 | 0.03 | 0.18 | |
| S-L5 | 0.03 | 0.03 | 0.01 | 0.05 | |
| Average (MPa) | |||||
|---|---|---|---|---|---|
| Lateral Bending | |||||
| Standing | Erect Sitting | Slumped Sitting | Sitting on the Floor | ||
| Cortical Bone | L1 | 4.38 | 3.33 | 6.22 | 7.18 |
| L2 | 3.12 | 3.55 | 12.87 | 8.34 | |
| L3 | 1.71 | 1.89 | 8.58 | 3.88 | |
| L4 | 1.73 | 1.80 | 7.46 | 3.68 | |
| L5 | 1.92 | 3.18 | 5.82 | 3.06 | |
| Annulus fiber | L2-L1 | 0.33 | 0.29 | 0.51 | 0.54 |
| L3-L2 | 0.20 | 0.27 | 0.40 | 0.50 | |
| L4-L3 | 0.20 | 0.22 | 0.29 | 0.42 | |
| L5-L4 | 0.26 | 0.31 | 0.26 | 0.52 | |
| S-L5 | 0.12 | 0.13 | 0.06 | 0.20 | |
| Nucleus pulposus | L2-L1 | 0.08 | 0.06 | 0.15 | 0.13 |
| L3-L2 | 0.04 | 0.06 | 0.10 | 0.13 | |
| L4-L3 | 0.04 | 0.05 | 0.08 | 0.09 | |
| L5-L4 | 0.06 | 0.07 | 0.05 | 0.14 | |
| S-L5 | 0.02 | 0.06 | 0.01 | 0.04 | |
| Average (MPa) | |||||
|---|---|---|---|---|---|
| Axial Rotation | |||||
| Standing | Erect Sitting | Slumped Sitting | Sitting on the Floor | ||
| Cortical Bone | L1 | 4.39 | 3.40 | 6.25 | 7.23 |
| L2 | 2.99 | 3.15 | 12.76 | 8.31 | |
| L3 | 1.45 | 1.60 | 8.51 | 3.81 | |
| L4 | 1.35 | 1.48 | 7.35 | 3.62 | |
| L5 | 1.48 | 2.83 | 5.71 | 3.03 | |
| Annulus fiber | L2-L1 | 0.33 | 0.26 | 0.49 | 0.54 |
| L3-L2 | 0.19 | 0.20 | 0.38 | 0.49 | |
| L4-L3 | 0.13 | 0.15 | 0.22 | 0.39 | |
| L5-L4 | 0.15 | 0.24 | 0.10 | 0.49 | |
| S-L5 | 0.12 | 0.13 | 0.06 | 0.20 | |
| Nucleus pulposus | L2-L1 | 0.08 | 0.06 | 0.15 | 0.13 |
| L3-L2 | 0.04 | 0.05 | 0.09 | 0.13 | |
| L4-L3 | 0.03 | 0.04 | 0.06 | 0.08 | |
| L5-L4 | 0.03 | 0.05 | 0.02 | 0.13 | |
| S-L5 | 0.02 | 0.02 | 0.01 | 0.04 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cho, M.; Han, J.-S.; Kang, S.; Ahn, C.-H.; Kim, D.-H.; Kim, C.-H.; Kim, K.-T.; Kim, A.-R.; Hwang, J.-M. Biomechanical Effects of Different Sitting Postures and Physiologic Movements on the Lumbar Spine: A Finite Element Study. Bioengineering 2023, 10, 1051. https://doi.org/10.3390/bioengineering10091051
Cho M, Han J-S, Kang S, Ahn C-H, Kim D-H, Kim C-H, Kim K-T, Kim A-R, Hwang J-M. Biomechanical Effects of Different Sitting Postures and Physiologic Movements on the Lumbar Spine: A Finite Element Study. Bioengineering. 2023; 10(9):1051. https://doi.org/10.3390/bioengineering10091051
Chicago/Turabian StyleCho, Mingoo, Jun-Sang Han, Sungwook Kang, Chang-Hwan Ahn, Dong-Hee Kim, Chul-Hyun Kim, Kyoung-Tae Kim, Ae-Ryoung Kim, and Jong-Moon Hwang. 2023. "Biomechanical Effects of Different Sitting Postures and Physiologic Movements on the Lumbar Spine: A Finite Element Study" Bioengineering 10, no. 9: 1051. https://doi.org/10.3390/bioengineering10091051
APA StyleCho, M., Han, J.-S., Kang, S., Ahn, C.-H., Kim, D.-H., Kim, C.-H., Kim, K.-T., Kim, A.-R., & Hwang, J.-M. (2023). Biomechanical Effects of Different Sitting Postures and Physiologic Movements on the Lumbar Spine: A Finite Element Study. Bioengineering, 10(9), 1051. https://doi.org/10.3390/bioengineering10091051






