The Effect of Mechanical Circulatory Support on Blood Flow in the Ascending Aorta: A Combined Experimental and Computational Study
Abstract
1. Introduction
2. Methods and Materials
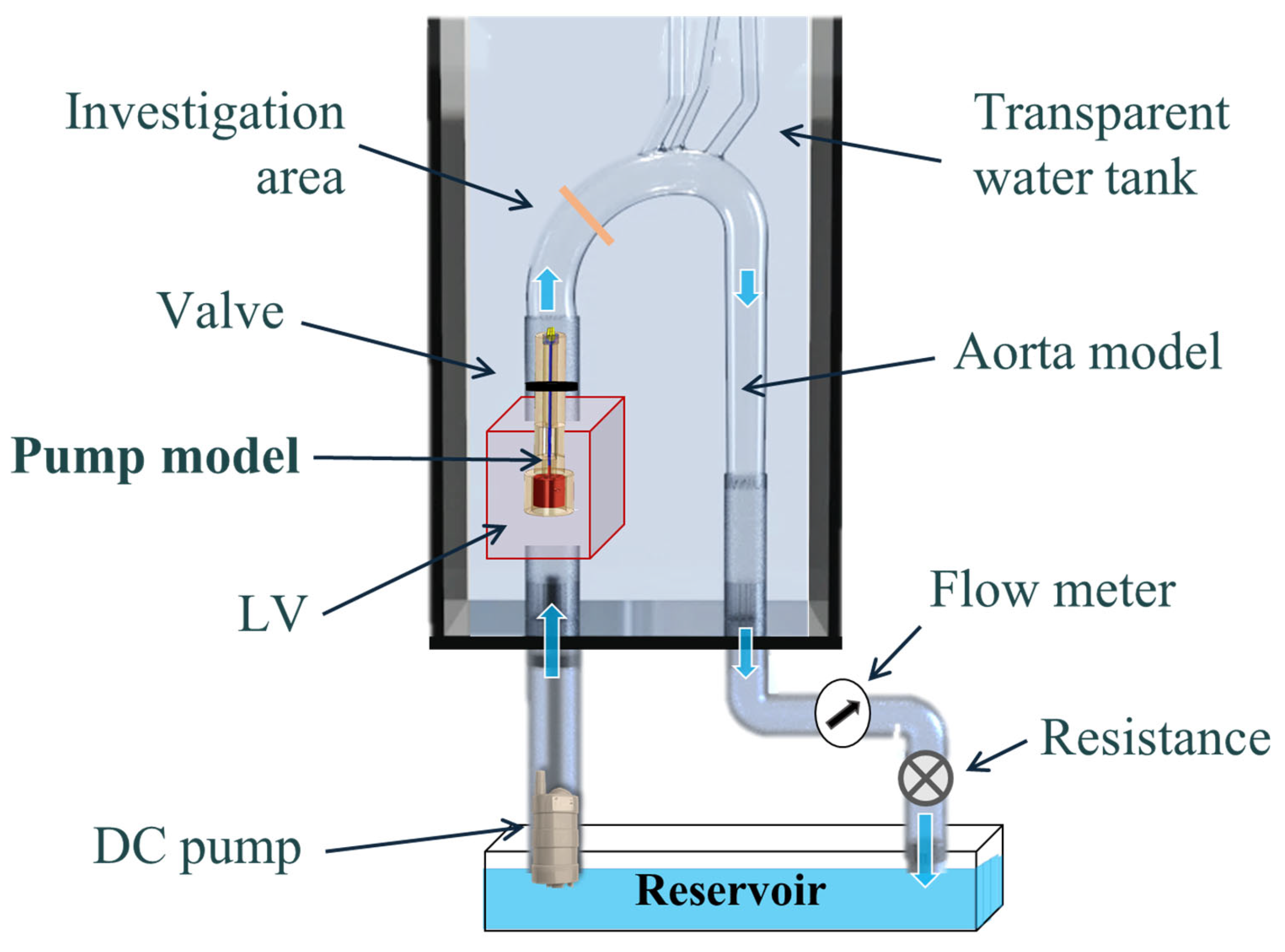
2.1. Experimental Setup
2.2. Cases Studied
2.3. Post-Processing
2.4. Numerical Model
3. Results
4. Discussion
- Swirling flow reduces the TKE of the pump’s jet inlet and improves the flow distribution near the aortic valve and the ascending aorta (and may reduce the risk of release of emboli from the aorta wall);
- Swirling flow increases the dominance of vortical flow near the valve and in the ascending aorta;
- In the case of the CW inlet case, the vortex was drawn toward the posterior wall of the aorta, while in the CCW inlet case, the vortex was drawn toward the anterior wall of the aorta;
- A high flow rate washed out the local turbulence near the pump inlet downstream toward the aortic arch, and thus, the local vortices formed near the outlet were more distributed in the ascending aorta;
- pLVAD with a CCW rotating impeller (such as in the Impella pump) induced non-physiological CCW helical flow in the descending aorta (which is the opposite of the natural helical flow);
- Clockwise swirl combined better with the natural helical flow.
- Examining the effect of CCW helical flow in the descending aorta on the flow to the branching arteries (e.g., coronaries, subclavian, carotid, and renal);
- Examining the effects of different rotational velocities on the flow;
- Examining the effects of a beating heart and the obtained combined flow (including the aortic valve’s dynamics);
- Examining the effects of the different flow features on each other.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Marcuschamer, I.A.; Abelow, A.; Kornowski, R. The evolving role of percutaneous ventricular assist devices in high-risk cardiac patients. Coron. Artery Dis. 2018, 29, 344–353. [Google Scholar] [CrossRef]
- Farmakis, D.; Parissis, J.; Karavidas, A.; Karvounis, C.; Triposkiadis, F.; Filippatos, G.; Lekakis, J.; Barbetseas, J.; Giannadaki, M.; Kakouros, S. In-hospital management of acute heart failure: Practical recommendations and future perspectives. Int. J. Cardiol. 2015, 201, 231–236. [Google Scholar] [CrossRef] [PubMed]
- Almajed, M.R.; Mahmood, S.; Obri, M.; Nona, P.; Gonzalez, P.E.; Chiang, M.; Wang, D.D.; Frisoli, T.; Lee, J.; Basir, M. Application of Impella mechanical circulatory support devices in transcatheter aortic valve replacement and balloon aortic valvuloplasty: A single center experience. Cardiovasc. Revascularization Med. 2023, 53, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Møller, J.E.; Kjaergaard, J.; Terkelsen, C.J.; Hassager, C. Impella to Treat Acute Myocardial Infarct-Related Cardiogenic Shock. J. Clin. Med. 2022, 11, 2427. [Google Scholar] [CrossRef]
- Raess, D.H.; Weber, D.M. Impella 2.5. J. Cardiovasc. Transl. Res. 2009, 2, 168–172. [Google Scholar] [CrossRef]
- Schmitz-Rode, T.; Graf, J.; Pfeffer, J.G.; Buss, F.; Brücker, C.; Günther, R.W. An expandable percutaneous catheter pump for left ventricular support: Proof of concept. J. Am. Coll. Cardiol. 2005, 45, 1856–1861. [Google Scholar] [CrossRef][Green Version]
- Ahmed, A.A.; Moharam, B.A.; Rashad, E.E. Improving energy efficiency and economics of motor-pump-system using electric variable-speed drives for automatic transition of working points. Comput. Electr. Eng. 2022, 97, 107607. [Google Scholar] [CrossRef]
- Arvand, A.; Hormes, M.; Reul, H. A validated computational fluid dynamics model to estimate hemolysis in a rotary blood pump. Artif. Organs 2005, 29, 531–540. [Google Scholar] [CrossRef] [PubMed]
- Goodman, D.; Stulak, J.; Rosenbaum, A.N. Left ventricular assist devices: A historical perspective at the intersection of medicine and engineering. Artif. Organs 2022, 46, 2343–2360. [Google Scholar] [CrossRef]
- Alushi, B.; Douedari, A.; Froehlig, G.; Knie, W.; Wurster, T.H.; Leistner, D.M.; Staehli, B.-E.; Mochmann, H.-C.; Pieske, B.; Landmesser, U. Impella versus IABP in acute myocardial infarction complicated by cardiogenic shock. Open Heart 2019, 6, e000987. [Google Scholar] [CrossRef]
- Amin, A.P.; Spertus, J.A.; Curtis, J.P.; Desai, N.; Masoudi, F.A.; Bach, R.G.; McNeely, C.; Al-Badarin, F.; House, J.A.; Kulkarni, H. The evolving landscape of Impella use in the United States among patients undergoing percutaneous coronary intervention with mechanical circulatory support. Circulation 2020, 141, 273–284. [Google Scholar] [CrossRef]
- Dhruva, S.S.; Ross, J.S.; Mortazavi, B.J.; Hurley, N.C.; Krumholz, H.M.; Curtis, J.P.; Berkowitz, A.; Masoudi, F.A.; Messenger, J.C.; Parzynski, C.S. Association of use of an intravascular microaxial left ventricular assist device vs intra-aortic balloon pump with in-hospital mortality and major bleeding among patients with acute myocardial infarction complicated by cardiogenic shock. JAMA 2020, 323, 734–745. [Google Scholar] [CrossRef] [PubMed]
- Vila, P.; de Vere, F.; Simon, A.; Walker, C. Severe Severe aortic valve regurgitation requiring mechanical aortic valve replacement following Impella device implantation. Perfusion 2021, 36, 311–314. [Google Scholar] [CrossRef]
- Butala, B.; Yu, R.; Schorr, R.; Gologorsky, E. Periprocedural dynamics of aortic regurgitation in patients supported with an Impella left ventricular assist device. J. Cardiothorac. Vasc. Anesth. 2020, 34, 659–662. [Google Scholar] [CrossRef] [PubMed]
- Sef, D.; Kabir, T.; Lees, N.J.; Stock, U. Valvular complications following the Impella device implantation. J. Card. Surg. 2021, 36, 1062–1066. [Google Scholar] [CrossRef]
- Morbiducci, U.; Ponzini, R.; Rizzo, G.; Cadioli, M.; Esposito, A.; Montevecchi, F.M.; Redaelli, A. Mechanistic insight into the physiological relevance of helical blood flow in the human aorta: An in vivo study. Biomech. Model. Mechanobiol. 2011, 10, 339–355. [Google Scholar] [CrossRef]
- Liu, X.; Sun, A.; Fan, Y.; Deng, X. Physiological significance of helical flow in the arterial system and its potential clinical applications. Ann. Biomed. Eng. 2015, 43, 3–15. [Google Scholar] [CrossRef] [PubMed]
- Markl, M.; Kilner, P.J.; Ebbers, T. Comprehensive 4D velocity mapping of the heart and great vessels by cardiovascular magnetic resonance. J. Cardiovasc. Magn. Reson. 2011, 13, 7. [Google Scholar] [CrossRef]
- Jarral, O.A.; Tan, M.K.; Salmasi, M.Y.; Pirola, S.; Pepper, J.R.; O’Regan, D.P.; Xu, X.Y.; Athanasiou, T. Phase-contrast magnetic resonance imaging and computational fluid dynamics assessment of thoracic aorta blood flow: A literature review. Eur. J. Cardio-Thorac. Surg. 2020, 57, 438–446. [Google Scholar] [CrossRef]
- Lee, C.-H.; Liu, K.-S.; Jhong, G.-H.; Liu, S.-J.; Hsu, M.-Y.; Wang, C.-J.; Hung, K.-C. Finite element analysis of helical flows in human aortic arch: A novel index. Biomicrofluidics 2014, 8, 024111. [Google Scholar] [CrossRef]
- Morbiducci, U.; Ponzini, R.; Rizzo, G.; Cadioli, M.; Esposito, A.; De Cobelli, F.; Del Maschio, A.; Montevecchi, F.M.; Redaelli, A. In vivo quantification of helical blood flow in human aorta by time-resolved three-dimensional cine phase contrast magnetic resonance imaging. Ann. Biomed. Eng. 2009, 37, 516–531. [Google Scholar] [CrossRef]
- Lu, X.; Kassab, G.S. Nitric oxide is significantly reduced in ex vivo porcine arteries during reverse flow because of increased superoxide production. J. Physiol. 2004, 561, 575–582. [Google Scholar] [CrossRef]
- Andersson, M.; Lantz, J.; Ebbers, T.; Karlsson, M. Multidirectional WSS disturbances in stenotic turbulent flows: A pre-and post-intervention study in an aortic coarctation. J. Biomech. 2017, 51, 8–16. [Google Scholar] [CrossRef]
- Ha, H.; Ziegler, M.; Welander, M.; Bjarnegård, N.; Carlhäll, C.-J.; Lindenberger, M.; Länne, T.; Ebbers, T.; Dyverfeldt, P. Age-related vascular changes affect turbulence in aortic blood flow. Front. Physiol. 2018, 9, 36. [Google Scholar] [CrossRef]
- Sameshima, N.; Yamashita, A.; Sato, S.; Matsuda, S.; Matsuura, Y.; Asada, Y. The values of wall shear stress, turbulence kinetic energy and blood pressure gradient are associated with atherosclerotic plaque erosion in rabbits. J. Atheroscler. Thromb. 2014, 21, 831–838. [Google Scholar] [CrossRef]
- Ozturk, M.; Papavassiliou, D.V.; O’Rear, E.A. An approach for assessing turbulent flow damage to blood in medical devices. J. Biomech. Eng. 2017, 139, 011008. [Google Scholar] [CrossRef] [PubMed]
- Kameneva, M.V.; Burgreen, G.W.; Kono, K.; Repko, B.; Antaki, J.F.; Umezu, M. Effects Of Turbulent Stresses On Mechanical Hemolysis: Experimental And Computational Analysis. ASAIO J. 2004, 50, 418. [Google Scholar] [CrossRef] [PubMed]
- Salman, H.E.; Ramazanli, B.; Yavuz, M.M.; Yalcin, H.C. Biomechanical investigation of disturbed hemodynamics-induced tissue degeneration in abdominal aortic aneurysms using computational and experimental techniques. Front. Bioeng. Biotechnol. 2019, 7, 111. [Google Scholar] [CrossRef] [PubMed]
- Gülan, U.; Lüthi, B.; Holzner, M.; Liberzon, A.; Tsinober, A.; Kinzelbach, W. Experimental study of aortic flow in the ascending aorta via particle tracking velocimetry. Exp. Fluids 2012, 53, 1469–1485. [Google Scholar] [CrossRef]
- Zhang, Q.; Gao, B.; Chang, Y. Helical flow component of left ventricular assist devices (LVADs) outflow improves aortic hemodynamic states. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2018, 24, 869. [Google Scholar] [CrossRef] [PubMed]
- Zhang, P.H.; Tkatch, C.; Vainchtein, D.; Kresh, J.Y. Aortic hemodynamics of spiral-flow-generated mechanical assistance. Ann. Thorac. Surg. 2020, 109, 1449–1457. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Wang, J.; Peng, J.; Huo, M.; Yang, Z.; Giridharan, G.A.; Luan, Y.; Qin, K. Effects of a Short-Term Left Ventricular Assist Device on Hemodynamics in a Heart Failure Patient-Specific Aorta Model: A CFD Study. Front. Physiol. 2021, 12, 733464. [Google Scholar] [CrossRef]
- Zhang, Q.; Gao, B.; Chang, Y. Effect of different rotational directions of BJUT-II VAD on aortic swirling flow characteristics: A primary computational fluid dynamics study. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2016, 22, 2576. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Büsen, M.; Arenz, C.; Neidlin, M.; Liao, S.; Schmitz-Rode, T.; Steinseifer, U.; Sonntag, S.J. Development of an In Vitro PIV setup for preliminary investigation of the effects of aortic compliance on flow patterns and hemodynamics. Cardiovasc. Eng. Technol. 2017, 8, 368–377. [Google Scholar] [CrossRef]
- Catapano, F.; Pambianchi, G.; Cundari, G.; Rebelo, J.; Cilia, F.; Carbone, I.; Catalano, C.; Francone, M.; Galea, N. 4D flow imaging of the thoracic aorta: Is there an added clinical value? Cardiovascular Diagnosis and Therapy. Cardiovasc. Diagn. Ther. 2020, 10, 1068. [Google Scholar] [CrossRef] [PubMed]
- Gülan, U.; Lüthi, B.; Holzner, M.; Liberzon, A.; Tsinober, A.; Kinzelbach, W. An in vitro investigation of the influence of stenosis severity on the flow in the ascending aorta. Med. Eng. Phys. 2014, 36, 1147–1155. [Google Scholar] [CrossRef] [PubMed]
- Ramaekers, M.J.; Adriaans, B.P.; Juffermans, J.F.; Van Assen, H.C.; Bekkers, S.C.; Scholte, A.J.; Kenjeres, S.; Lamb, H.J.; Hildberger, J.E.; Westenberg, J.J. Characterization of ascending aortic flow in patients with degenerative aneurysms: A 4D flow magnetic resonance study. Investig. Radiol. 2021, 56, 494–500. [Google Scholar] [CrossRef] [PubMed]
- Sieren, M.M.; Schultz, V.; Fujita, B.; Wegner, F.; Huellebrand, M.; Scharfschwerdt, M.; Sievers, H.-H.; Barkhausen, J.; Frydrychowicz, A.; Oechtering, T.H. 4D flow CMR analysis comparing patients with anatomically shaped aortic sinus prostheses, tube prostheses and healthy subjects introducing the wall shear stress gradient: A case control study. J. Cardiovasc. Magn. Reson. 2020, 22, 1–14. [Google Scholar] [CrossRef]
- Triep, M.; Brücker, C.; Schröder, W.; Siess, T. Computational fluid dynamics and digital particle image velocimetry study of the flow through an optimized micro-axial blood pump. Artif. Organs 2006, 30, 384–391. [Google Scholar] [CrossRef]
- Zein, R.; Patel, C.; Mercado-Alamo, A.; Schreiber, T.; Kaki, A. A review of the Impella Devices. Interv. Cardiol. Rev. Res. Resour. 2022, 17, e05. [Google Scholar] [CrossRef]
- Fraser, K.H.; Taskin, M.E.; Griffith, B.P.; Wu, Z.J. The use of computational fluid dynamics in the development of ventricular assist devices. Med. Eng. Phys. 2011, 33, 263–280. [Google Scholar] [CrossRef] [PubMed]
- Kannojiya, V.; Das, A.K.; Das, P.K. Comparative assessment of different versions of axial and centrifugal LVADs: A review. Artif. Organs 2021, 45, 665–681. [Google Scholar] [CrossRef]
- Sahni, A.; McIntyre, E.E.; Pal, J.D.; Mukherjee, D. Quantitative assessment of aortic hemodynamics for varying left ventricular assist device outflow graft angles and flow pulsation. Ann. Biomed. Eng. 2023, 51, 1226–1243. [Google Scholar] [CrossRef]
- Steinlauf, S.; Shenberger, S.H.; Halak, M.; Liberzon, A.; Avrahami, I. Aortic arch aneurysm repair–Unsteady hemodynamics and perfusion at different heart rates. J. Biomech. 2021, 121, 110351. [Google Scholar] [CrossRef]
- Jakanani, G.; Adair, W. Frequency of variations in aortic arch anatomy depicted on multidetector CT. Clin. Radiol. 2010, 65, 481–487. [Google Scholar] [CrossRef] [PubMed]
- Paruchuri, V.; Salhab, K.F.; Kuzmik, G.; Gubernikoff, G.; Fang, H.; Rizzo, J.A.; Ziganshin, B.A.; Elefteriades, J.A. Aortic size distribution in the general population: Explaining the size paradox in aortic dissection. Cardiology 2015, 131, 265–272. [Google Scholar] [CrossRef]
- Thielicke, W.; Stamhuis, E. PIVlab–towards user-friendly, affordable and accurate digital particle image velocimetry in MATLAB. J. Open Res. Softw. 2014, 2, 30. [Google Scholar] [CrossRef]
- Thielicke, W.; Sonntag, R. Particle Image Velocimetry for MATLAB: Accuracy and enhanced algorithms in PIVlab. J. Open Res. Softw. 2021, 9, 12. [Google Scholar] [CrossRef]
- Moisy, F. PIVMat 4.20, MATLAB Central File Exchange. Available online: https://www.mathworks.com/matlabcentral/fileexchange/10902-pivmat-4-20 (accessed on 29 December 2022).
- Nardi, A.; Avrahami, I. Approaches for treatment of aortic arch aneurysm, a numerical study. J. Biomech. 2017, 50, 158–165. [Google Scholar] [CrossRef]
- Avrahami, I.; Dilmoney, B.; Azuri, A.; Brand, M.; Cohen, O.; Shani, L.; Nir, R.R.; Bolotin, G. Investigation of risks for cerebral embolism associated with the hemodynamics of cardiopulmonary bypass cannula: A numerical model. Artif. Organs 2013, 37, 857–865. [Google Scholar] [CrossRef]
- Simpson, B.; Tansley, G. Guidelines for Choosing an Appropriate Turbulence Model when Simulating Blood Flows in Cardiovascular Devices; Griffith University: Brisbane, QLD, Australia, 2015. [Google Scholar]
- Blauth, C.I.; Cosgrove, D.M.; Webb, B.W.; Ratliff, N.B.; Boylan, M.; Piedmonte, M.R.; Lytle, B.W.; Loop, F.D. Atheroembolism from the ascending aorta: An emerging problem in cardiac surgery. J. Thorac. Cardiovasc. Surg. 1992, 103, 1104–1112. [Google Scholar] [CrossRef] [PubMed]
- Damluji, A.A.; van Diepen, S.; Katz, J.N.; Menon, V.; Tamis-Holland, J.E.; Bakitas, M.; Cohen, M.G.; Balsam, L.B.; Chikwe, J. Mechanical complications of acute myocardial infarction: A scientific statement from the American Heart Association. Circulation 2021, 144, e16–e35. [Google Scholar] [CrossRef] [PubMed]














| Experiment | Numerical Boundary Conditions | |||
|---|---|---|---|---|
| Flow Rate | Rotational Speed * | Jet Inlet | CW Inlet | CCW Inlet |
| 1 L/min | 9000 RPM | u = 0.21 m/s ω = 0 rad/s | u = 0.21 m/s ω = 900 rad/s CW | u = 0.21 m/s ω = 900 rad/s CCW |
| 1.5 L/min | 12,000 RPM | u = 0.32 m/s ω = 0 rad/s | u = 0.32 m/s ω = 1270 rad/s CW | u = 0.32 m/s ω = 1270 rad/s CCW |
| 2 L/min | 15,500 RPM | u = 0.42 m/s ω = 0 rad/s | u = 0.42 m/s ω = 1630 rad/s CW | u = 0.42 m/s ω = 1630 rad/s CCW |
| 2.5 L/min | 19,000 RPM | u = 0.53 m/s ω = 0 rad/s | u = 0.53 m/s ω = 2000 rad/s CW | u = 0.53 m/s ω = 2000 rad/s CCW |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hazan Shenberger, S.; Avrahami, I. The Effect of Mechanical Circulatory Support on Blood Flow in the Ascending Aorta: A Combined Experimental and Computational Study. Bioengineering 2024, 11, 238. https://doi.org/10.3390/bioengineering11030238
Hazan Shenberger S, Avrahami I. The Effect of Mechanical Circulatory Support on Blood Flow in the Ascending Aorta: A Combined Experimental and Computational Study. Bioengineering. 2024; 11(3):238. https://doi.org/10.3390/bioengineering11030238
Chicago/Turabian StyleHazan Shenberger, Sapir, and Idit Avrahami. 2024. "The Effect of Mechanical Circulatory Support on Blood Flow in the Ascending Aorta: A Combined Experimental and Computational Study" Bioengineering 11, no. 3: 238. https://doi.org/10.3390/bioengineering11030238
APA StyleHazan Shenberger, S., & Avrahami, I. (2024). The Effect of Mechanical Circulatory Support on Blood Flow in the Ascending Aorta: A Combined Experimental and Computational Study. Bioengineering, 11(3), 238. https://doi.org/10.3390/bioengineering11030238






