Effect of Sextant Fixating Angle of Spiral Clavicle Plate on Biomechanical Stability—A Preliminary Finite Element Study
Abstract
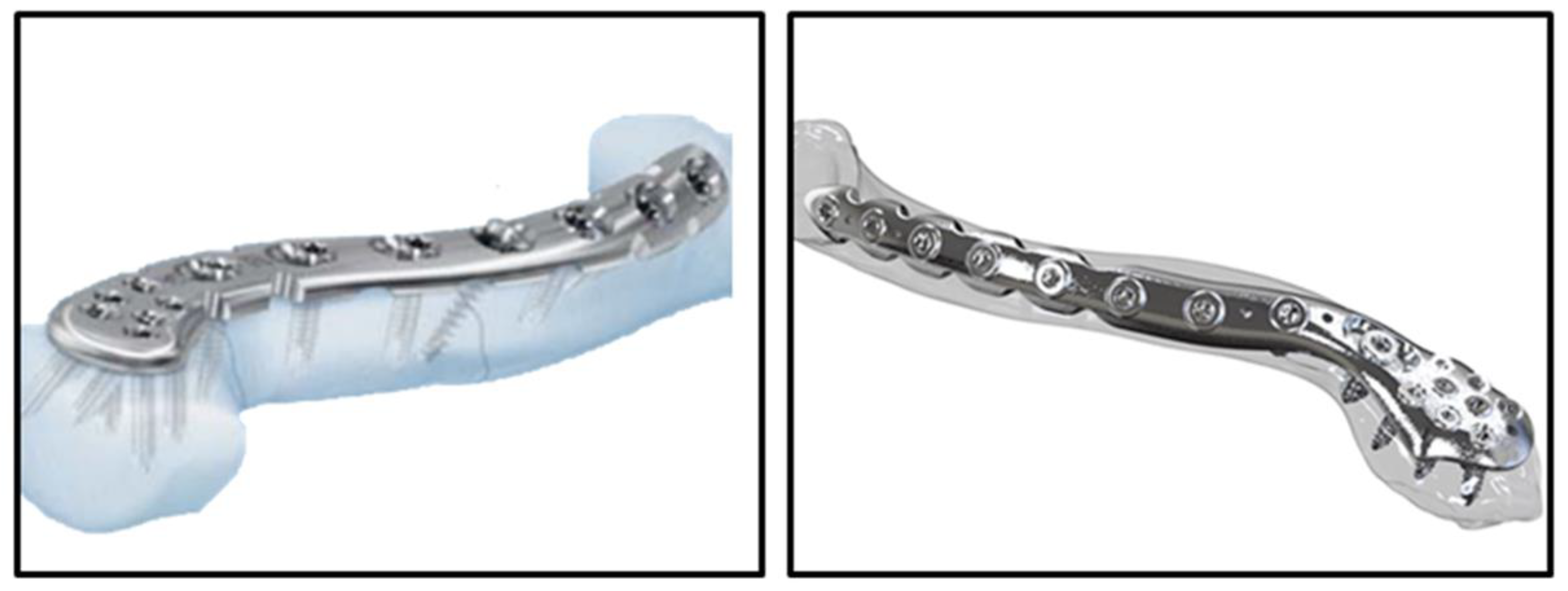
:1. Introduction
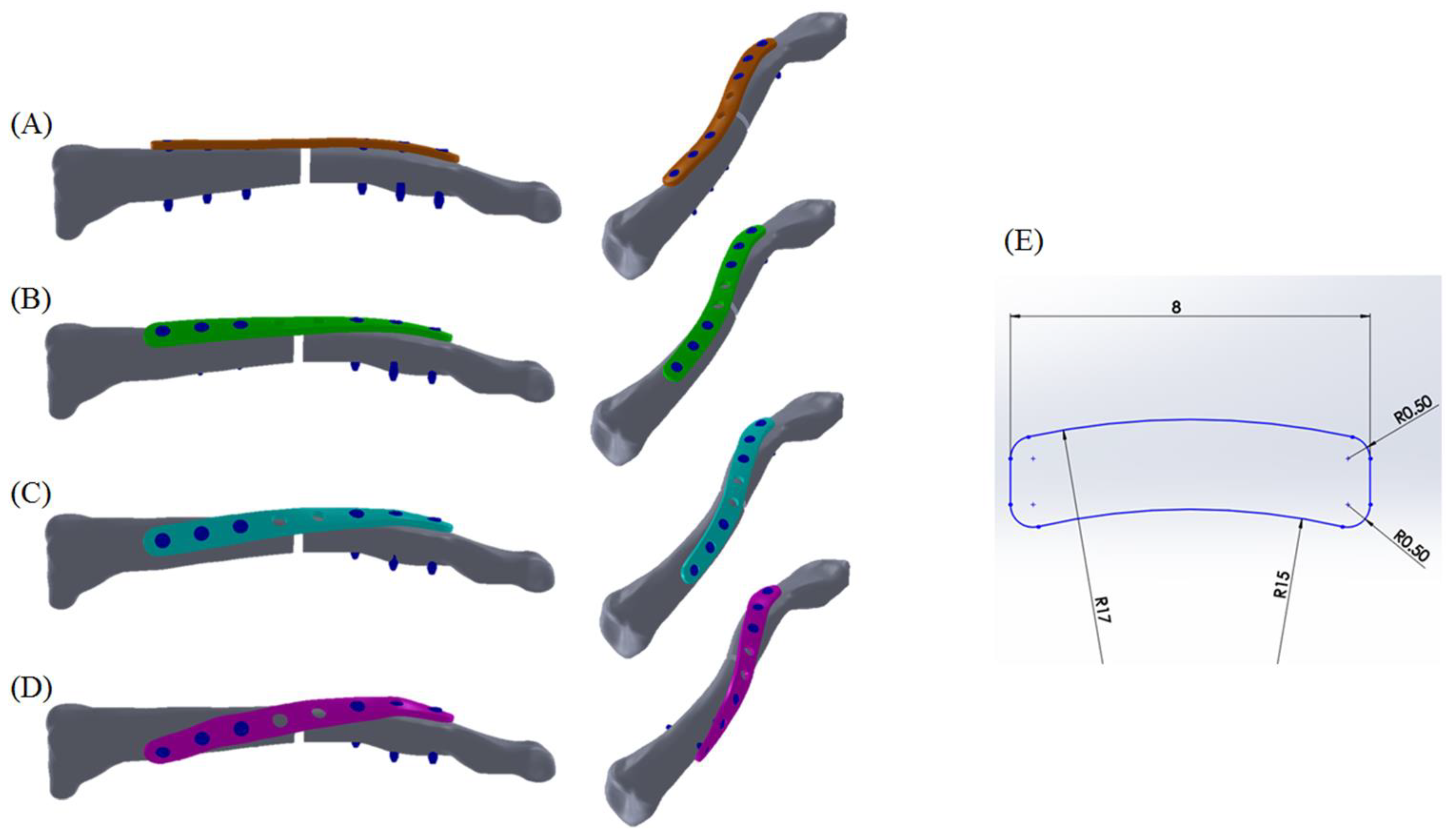
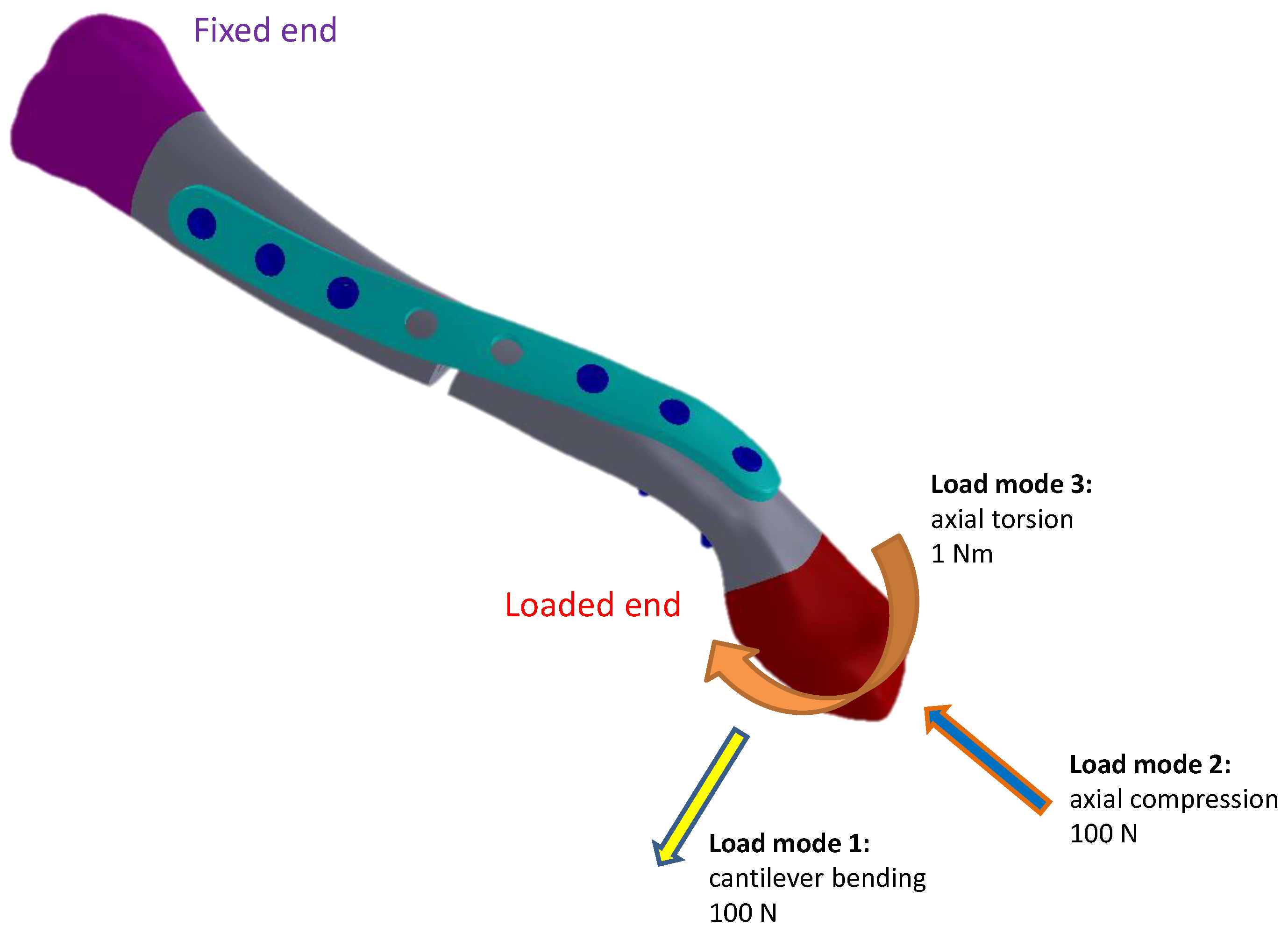
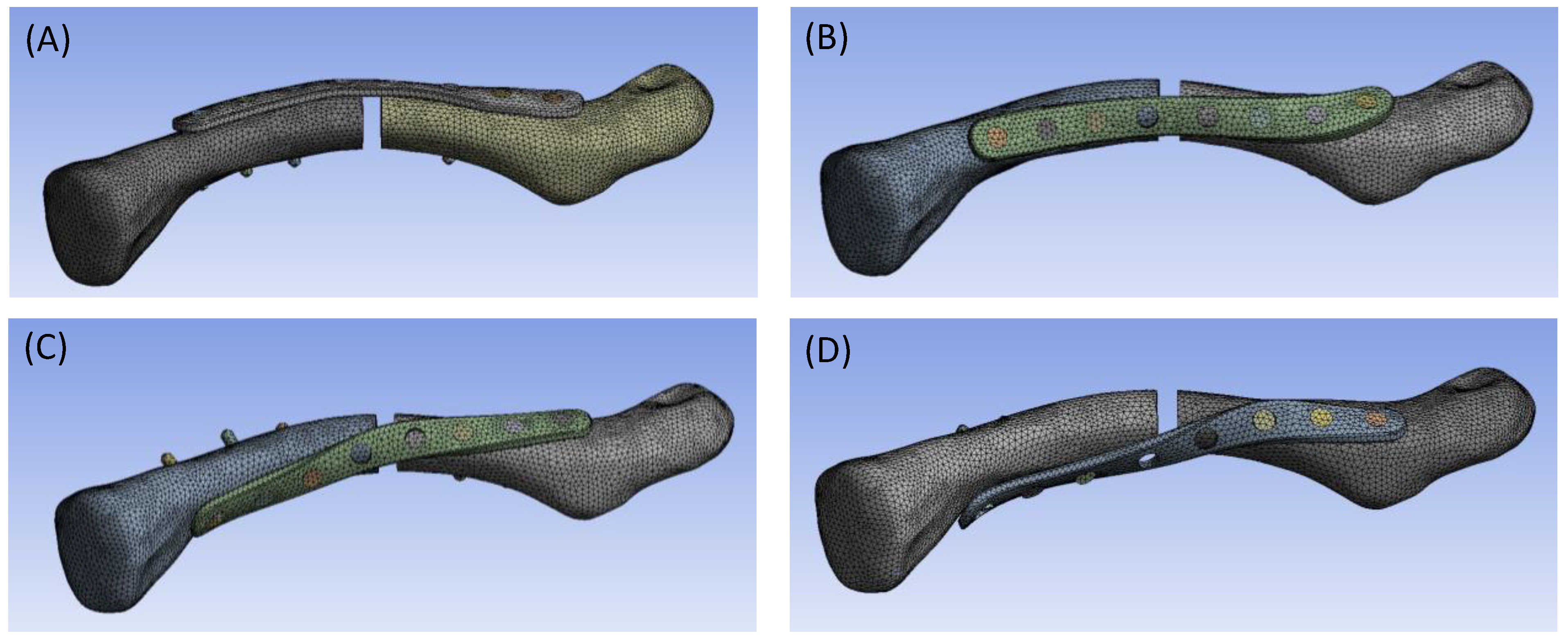
2. Materials and Methods
3. Results
3.1. Structural Stiffness
3.2. Stress on Clavicle Plates
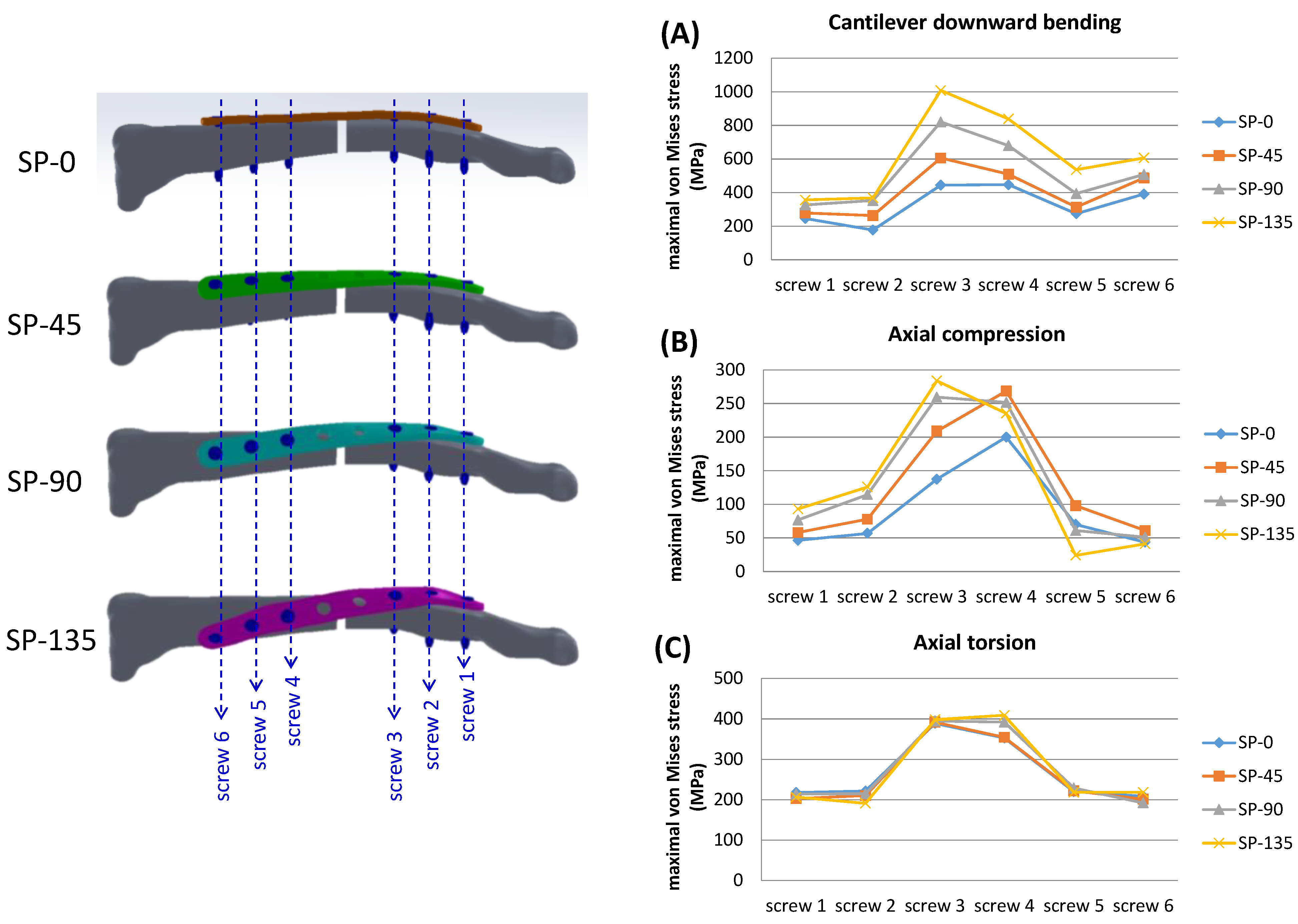
3.3. Stress on Locking Screws
4. Discussion
4.1. Structural Stiffness
4.2. Stress on Clavicle Plates
4.3. Stress on Locking Screws
4.4. Study Limitations
- -
- As a conceptual study in orthopedic biomechanics, the current study conducted finite element analyses using assumed homogeneous, isotropic, and linear elastic material properties. The quantified information obtained may provide guidance for predicting the biomechanical performance of various designs. However, to validate the results, practical biomechanical tests should be considered in future studies.
- -
- In the current study, common functional features found in commercial bone plates, such as decompression concaves, combi-holes, or reconstruction notches, were not considered. Instead, an identical cross-sectional pattern was assigned to all conceptual clavicle plate models to simplify and eliminate potential misjudgment of stress-based results due to complicated geometric designs.
- -
- While screw and plate stress performance may be associated with important aspects of clavicle bone remodeling, the current study focused on the effect of plate geometry on structural performance. Previous biomechanical studies have emphasized the stress-shielding effect after clavicle plate fixation in the treatment of clavicle fractures. Cortical bone atrophy underneath the strong metallic plate may occur [42]. For the newly formed bony structure at the previous fracture site, the bone quality is not as strong as that of the surrounding bone, which is a major cause of re-fracture after clavicle plate removal [17]. Zhang et al.’s finite element study represented end-to-end stress transmission (from the proximal screw hole to the sternal end of the clavicle) through the plate in the reconstructed clavicle model from a midshaft fracture, reflecting an obvious stress-shielding effect after spiral clavicle plate implantation [32]. However, due to simplified finite element definitions and the omission of detailed parameters such as screw thread characteristics, bony trabecular structure, bone density reconstruction from the radiographs, and comprehensive element behavior, the current study may not provide sufficient information on the impact of implant design on bone remodeling and possible stress-shielding performance under appropriate physiological loading conditions.
- -
- The parameters of the clavicle plate design, including plate thickness, width, length, curvature radius, spiral sextant angle, and screw diameters in the current study, are intended solely for conceptual purposes.
- -
- The loading conditions referenced in previous publications [29,30,32] have been applied in the current study. Biomechanical behavior and the influence of implant design can be evaluated for quantitative comparison. However, physiological clavicular activities involve much greater complexity, requiring detailed definitions of soft tissue attachments and consideration of multiple load exertions. The current bony model lacks the scapular part, which is essential for defining appropriate soft tissue origin/insertion boundaries and muscle forces. Nevertheless, the simplified loading conditions introduced in previous studies provide a straightforward viewpoint for biomechanical evaluation.
- -
- The bony model was reconstructed from only one subject. For a more objective evaluation, future studies should consider expanding the research to include different clavicle geometries, bone qualities, and other individual differences.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Court-Brown, C.; Caesar, B. Epidemiology of adult fractures. Injury 2006, 37, 691–697. [Google Scholar] [CrossRef]
- Lenza, M.; Belloti, J.C.; Andriolo, R.B.; Gomes Dos Santos, J.B.; Faloppa, F. Conservative interventions for treating middle third clavicle fractures in adolescents and adults. Cochrane Database Syst. Rev. 2009, 2, CD007121. [Google Scholar]
- Nordqvist, A.; Petersson, C. The incidence of fractures of the clavicle. Clin. Orthop. 1994, 300, 127–132. [Google Scholar] [CrossRef]
- Robinson, C.M. Fractures of the clavicle in the adult. Epidemiology and classification. J. Bone Jt. Surg. Br. 1998, 80-B, 476–484. [Google Scholar] [CrossRef]
- van der Meijden, O.A.; Gaskill, T.R.; Millett, P.J. Treatment of clavicle fractures: Current concepts review. J. Shoulder Elb. Surg. 2012, 21, 423–429. [Google Scholar] [CrossRef]
- Lazarides, S.; Zafiropoulos, G. Conservative treatment of fractures at the middle third of the clavicle: The relevance of shortening and clinical outcome. J. Shoulder Elb. Surg. 2006, 15, 191–194. [Google Scholar] [CrossRef] [PubMed]
- Postacchini, F.; Gumina, S.; De Santis, P.; Albo, F. Epidemiology of clavicle fractures. J. Shoulder Elb. Surg. 2002, 11, 452–456. [Google Scholar] [CrossRef]
- Hill, J.M.; McGuire, M.H.; Crosby, L.A. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J. Bone Jt. Surg. Br. 1997, 79, 537–539. [Google Scholar] [CrossRef]
- Altamimi, S.A.; McKee, M.D. Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. Surgical technique. J. Bone Jt. Surg. Am. 2008, 90 Pt 1 (Suppl. 2), 1–8. [Google Scholar] [CrossRef]
- Althausen, P.L.; Shannon, S.; Lu, M.; O’Mara, T.J.; Bray, T.J. Clinical and financial comparison of operative and nonoperative treatment of displaced clavicle fractures. J. Shoulder Elb. Surg. 2013, 22, 608–611. [Google Scholar] [CrossRef]
- Xu, J.; Xu, L.; Xu, W.; Gu, Y.; Xu, J. Operative versus nonoperative treatment in the management of midshaft clavicular fractures: A meta-analysis of randomized controlled trials. J. Shoulder Elb. Surg. 2014, 23, 173–181. [Google Scholar] [CrossRef]
- Song, H.S.; Kim, H. Current concepts in the treatment of midshaft clavicle fractures in adults. Clin. Shoulder Elb. 2021, 24, 189–198. [Google Scholar] [CrossRef]
- Wang, S.H.; Lin, H.J.; Shen, H.C.; Pan, R.Y.; Yang, J.J. Biomechanical comparison between solid and cannulated intramedullary devices for midshaft clavicle fixation. BMC Musculoskelet Disord. 2019, 20, 178. [Google Scholar] [CrossRef]
- Axelrod, D.E.; Ekhtiari, S.; Bozzo, A.; Bhandari, M.; Johal, H. What Is the Best Evidence for Management of Displaced Midshaft Clavicle Fractures? A Systematic Review and Network Meta-analysis of 22 Randomized Controlled Trials. Clin. Orthop. Relat. Res. 2020, 478, 392–402. [Google Scholar] [CrossRef]
- Pathak, S.K.; Gautam, R.K.; Godara, A.; Singh, M.; Kumar, N.; Sharma, A.; Vyas, A.; Khan, S.; Kumar, B.; Mateen, M.O. Plate Osteo-synthesis or Figure-of-Eight Brace: Which One Is Better in Midshaft Clavicle Fractures? Cureus 2021, 13, e14339. [Google Scholar] [PubMed]
- Yadav, S.; Phalak, M.O.; Shevate, I.; Salunkhe, R.; Khandge, A.; Deshmukh, A.; Patel, S.; Patil, G.L. Comparative Study of Postop-erative Outcomes of Clavicle Midshaft Fracture Treated by Nailing vs. Plating. Cureus 2022, 14, e22862. [Google Scholar] [PubMed]
- Fernandes, M.G.; Alves, J.L. Fonseca EMM. Diaphyseal femoral fracture: 3D biomodel and intramedullary nail created by additive manufacturing. Int. J. Mater. Eng. Innov. 2016, 7, 130–142. [Google Scholar] [CrossRef]
- Yang, K.H. Helical plate fixation for treatment of comminuted fractures of the proximal and middle one-third of the humerus. Injury 2005, 36, 75–80. [Google Scholar] [CrossRef] [PubMed]
- Gardner, M.J.; Griffith, M.H.; Lorich, D.G. Helical plating of the proximal humerus. Injury 2005, 36, 1197–1200. [Google Scholar] [CrossRef]
- Krishna, K.R.; Sridhar, I.; Ghista, D.N. Analysis of the helical plate for bone fracture fixation. Injury 2008, 39, 1421–1436. [Google Scholar] [CrossRef]
- Beirer, M.; Siebenlist, S.; Crönlein, M.; Postl, L.; Huber-Wagner, S.; Biberthaler, P.; Kirchhoff, C. Clinical and radiological outcome following treatment of displaced lateral clavicle fractures using a locking compression plate with lateral extension: A prospective study. BMC Musculoskelet. Disord. 2014, 15, 380. [Google Scholar] [CrossRef] [PubMed]
- Eden, L.; Doht, S.; Frey, S.P.; Ziegler, D.; Stoyhe, J.; Fehske, K.; Blunk, T.; Meffert, R.H. Biomechanical comparison of the Locking Compression superior anterior clavicle plate with seven and ten hole reconstruction plates in midshaft clavicle fracture stabilisation. Int. Orthop. 2012, 36, 2537–2543. [Google Scholar] [CrossRef] [PubMed]
- Marie, C. Strength analysis of clavicle fracture fixation devices and fixation techniques using finite element analysis with musculoskeletal force input. Med. Biol. Eng. Comput. 2015, 53, 759–769. [Google Scholar] [CrossRef]
- Partal, G.; Meyers, K.N.; Sama, N.; Pagenkopf, E.; Lewis, P.B.; Goldman, A.; Wright, T.M.; Helfet, D.L. Superior versus anteroinferior plating of the clavicle revisited: A mechanical study. J. Orthop. Trauma. 2010, 24, 420–425. [Google Scholar] [CrossRef]
- Formaini, N.; Taylor, B.C.; Backes, J.; Bramwell, T.J. Superior versus anteroinferior plating of clavicle fractures. Orthopedics 2013, 36, e898–e904. [Google Scholar] [CrossRef]
- Favre, P.; Kloen, P.; Helfet, D.L.; Werner, C.M. Superior versus anteroinferior plating of the clavicle: A finite element study. J. Orthop. Trauma. 2011, 25, 661–665. [Google Scholar] [CrossRef]
- Firas, N.R.; Ramawan, E. A biomechanical comparison of midshaft clavicle plate fixation between two screws and three screws on each side of the fractures. Qanun Med. Med. J. Fac. Med. Muhammadiyah Surabaya 2022, 6, 33–40. [Google Scholar] [CrossRef]
- Zaidenberg, E.E.; Voor, M.; Pereira, E.; Rossi, L.A.; Zaidenberg, C.R. Bicortical versus unicortical fixation of plated clavicular fractures: A biomechanical study. Shoulder Elb. 2021, 13, 426–432. [Google Scholar] [CrossRef]
- Wu, D.K.; Chen, W.C.; Lin, K.J.; Tsai, C.L.; Lin, K.P.; Wei, H.W. Advantage of multi-directional stability of spiral clavicle plate in treatment of middle one-third clavicle fracture: A finite element study. J. Med. Biol. Eng. 2021, 41, 405–411. [Google Scholar] [CrossRef]
- Huang, T.L.; Chen, W.C.; Lin, K.J.; Tsai, C.L.; Lin, K.P.; Wei, H.W. Conceptual finite element study for comparison among superior, anterior, and spiral clavicle plate fixations for midshaft clavicle fracture. Med. Eng. Phys. 2016, 38, 1070–1075. [Google Scholar] [CrossRef]
- Duprey, S.; Bruyere, K.; Verriest, J.P. Clavicle fracture prediction: Simulation of shoulder lateral impacts with geometrically personalized finite elements models. J. Trauma. 2010, 68, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Cheng, X.; Yin, B.; Wang, J.; Li, S.; Liu, G.; Hu, Z.; Wu, W.; Zhang, Y. Finite element analysis of spiral plate and Herbert screw fixation for treatment of midshaft clavicle fractures. Medicine 2019, 98, e16898. [Google Scholar] [CrossRef]
- Lima, G.V.; La Banca, V.; Murachovsky, J.; Nascimento, L.G.P.; Almeida, L.H.O.; Ikemoto, R.Y. Assessment of the measurement methods in midshaft clavicle fracture. BMC Musculoskelet. Disord. 2022, 23, 992. [Google Scholar] [CrossRef] [PubMed]
- Ramponi, D.R.; Jo Cerepani, M. Clavicle Fractures. Adv. Emerg. Nurs. J. 2021, 43, 123–127. [Google Scholar] [CrossRef] [PubMed]
- Iannotti, M.R.; Crosby, L.A.; Stafford, P.; Grayson, G.; Goulet, R. Effects of plate location and selection on the stability of midshaft clavicle osteotomies: A biomechanical study. J. Shoulder Elb. Surg. 2002, 11, 457–462. [Google Scholar] [CrossRef]
- Ziegler, C.G.; Aman, Z.S.; Storaci, H.W.; Finch, H.; Dornan, G.J.; Kennedy, M.I.; Provencher, M.T.; Hackett, T.R. Low-Profile Dual Small Plate Fixation Is Biomechanically Similar to Larger Superior or Anteroinferior Single Plate Fixation of Midshaft Clavicle Fractures. Am. J. Sports Med. 2019, 47, 2678–2685. [Google Scholar] [CrossRef]
- Zhang, F.; Chen, F.; Qi, Y.; Qian, Z.; Ni, S.; Zhong, Z.; Zhang, X.; Li, D.; Yu, B. Finite element analysis of dual small plate fixation and single plate fixation for treatment of midshaft clavicle fractures. J. Orthop. Surg. Res. 2020, 15, 148. [Google Scholar] [CrossRef] [PubMed]
- Ariga, A.; Shimura, H.; Fujita, K.; Nimura, A. Anteroinferior plating is an independent factor for decreasing symptomatic implant removal rates after plate fixation for midshaft clavicle fractures. OTA Int. 2023, 6, e253. [Google Scholar] [CrossRef]
- Pengrung, N.; Lakdee, N.; Puncreobutr, C.; Lohwongwatana, B.; Sangasoongsong, P. Finite element analysis comparison be-tween superior clavicle locking plate with and without screw holes above fracture zone in midshaft clavicular fracture. BMC Musculoskelet. Disord. 2019, 20, 465. [Google Scholar] [CrossRef]
- Han, Z.; Luo, Q.; Deng, G.; Bi, C.; Yin, G.; Lin, H.; Wu, J.; Wu, X. Canceling Notch Improves the Mechanical Safety of Clavicle Locking Plate: A 3D Finite Element Study. Orthop. Surg. 2023, 15, 2152–2156. [Google Scholar] [CrossRef]
- Bellapianta, J.; Dow, K.; Pallotta, N.A.; Hospodar, P.P.; Uhl, R.L.; Ledet, E.H. Threaded screw head inserts improve locking plate biomechanical properties. J. Orthop. Trauma. 2011, 25, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Woo, S.L.; Akeson, W.H.; Coutts, R.D.; Rutherford, L.; Doty, D.; Jemmott, G.F.; Amiel, D. A comparison of cortical bone atrophy secondary to fixation with plates with large differences in bending stiffness. J. Bone Jt. Surg. Am. 1976, 58, 190–195. [Google Scholar] [CrossRef]


| Interface | Contact | Target | Behavior | Frictional Coefficient |
|---|---|---|---|---|
| Plate/screw | plate | screw | bond | - |
| Plate/bone | bone | plate | contact | Frictionless |
| Screw/bone | bone | screw | bond | - |
| Bone/bone | Proximal fragment | Distal fragment | contact | 0.2 |
| Materials | Young’s Modulus (MPa) | Poisson’s Ratio |
|---|---|---|
| Cortical bone | 11,000 | 0.3 |
| Cancellous bone | 500 | 0.1 |
| Titanium alloy | 110,000 | 0.3 |
| Downward Bending | Axial Compression | Axial Torsion | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Max. | Min. | Avg. | Max. | Min. | Avg. | Max. | Min. | Avg. | |
| SP-0 | 447.6 | 177.1 | 330.1 | 199.9 | 43.7 | 92.4 | 389.3 | 208.5 | 268.4 |
| SP-45 | 606.0 | 262.8 | 409.5 | 268.5 | 58.1 | 128.7 | 392.2 | 201.2 | 263.9 |
| SP-90 | 820.5 | 326.5 | 513.7 | 259.4 | 51.1 | 135.7 | 394.7 | 192.1 | 272.8 |
| SP-135 | 1008.2 | 356.6 | 619.1 | 283.7 | 24.1 | 133.9 | 408.5 | 191.0 | 273.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hu, M.-H.; Su, P.-F.; Lin, K.-J.; Chen, W.-C.; Wang, S.-P. Effect of Sextant Fixating Angle of Spiral Clavicle Plate on Biomechanical Stability—A Preliminary Finite Element Study. Bioengineering 2024, 11, 713. https://doi.org/10.3390/bioengineering11070713
Hu M-H, Su P-F, Lin K-J, Chen W-C, Wang S-P. Effect of Sextant Fixating Angle of Spiral Clavicle Plate on Biomechanical Stability—A Preliminary Finite Element Study. Bioengineering. 2024; 11(7):713. https://doi.org/10.3390/bioengineering11070713
Chicago/Turabian StyleHu, Ming-Hsien, Po-Feng Su, Kun-Jhih Lin, Wen-Chuan Chen, and Shun-Ping Wang. 2024. "Effect of Sextant Fixating Angle of Spiral Clavicle Plate on Biomechanical Stability—A Preliminary Finite Element Study" Bioengineering 11, no. 7: 713. https://doi.org/10.3390/bioengineering11070713






