“BrainHeart”: Pilot Study on a Novel Application for Elderly Well-Being Based on Mindfulness Acceptance and Commitment Therapy
Abstract
1. Introduction
2. Materials and Methods
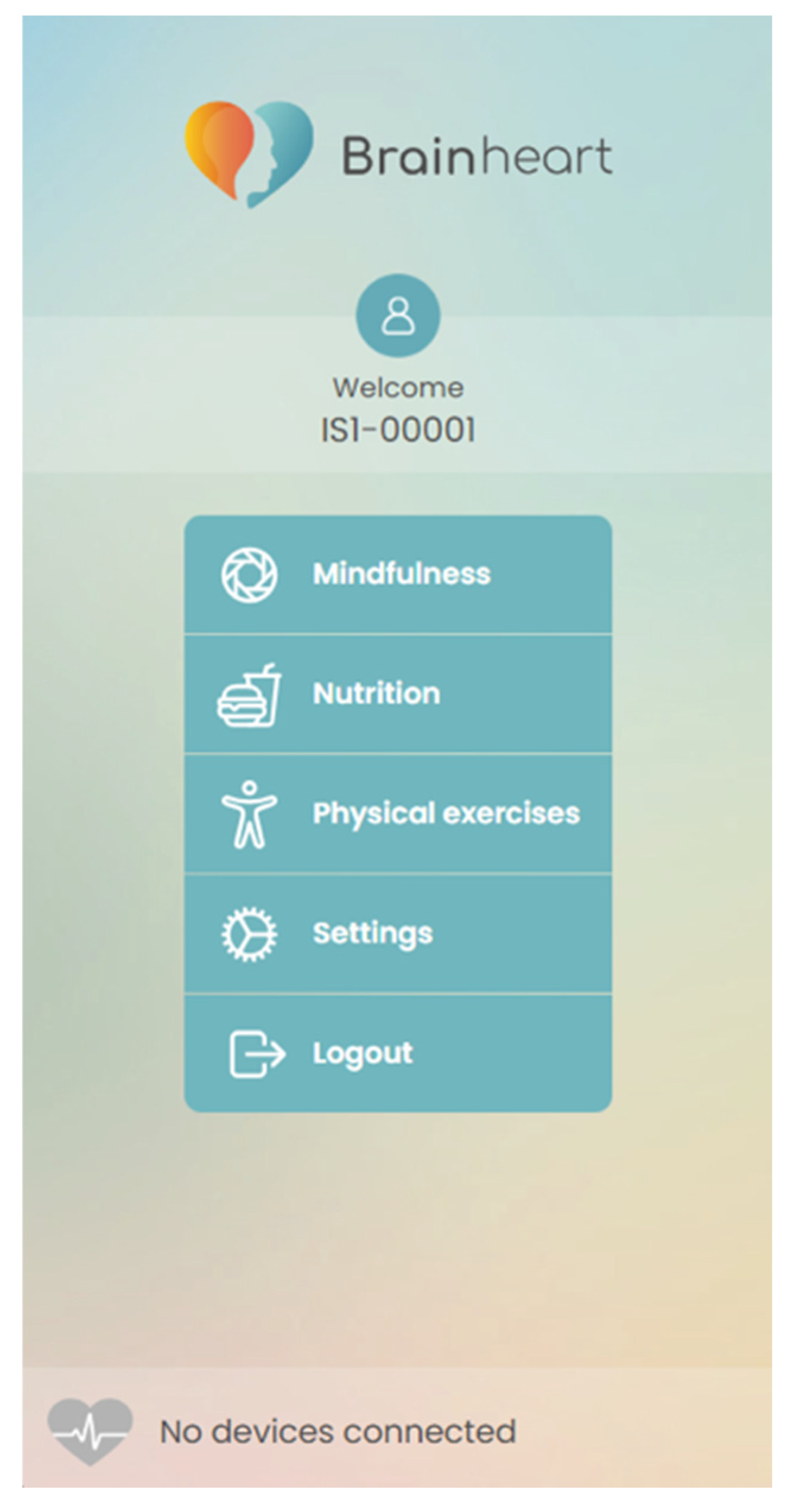
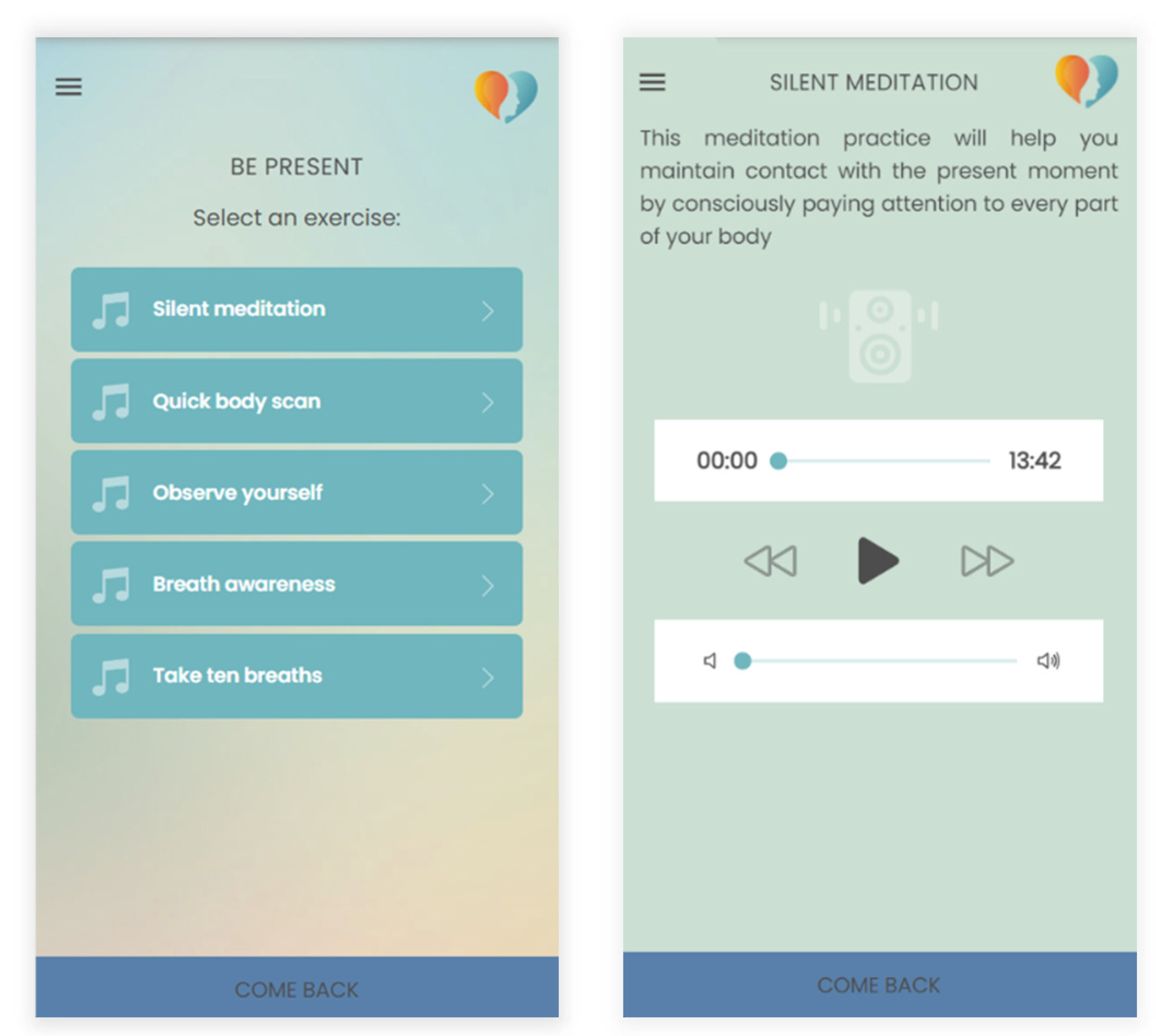
2.1. BrainHeart App Overview
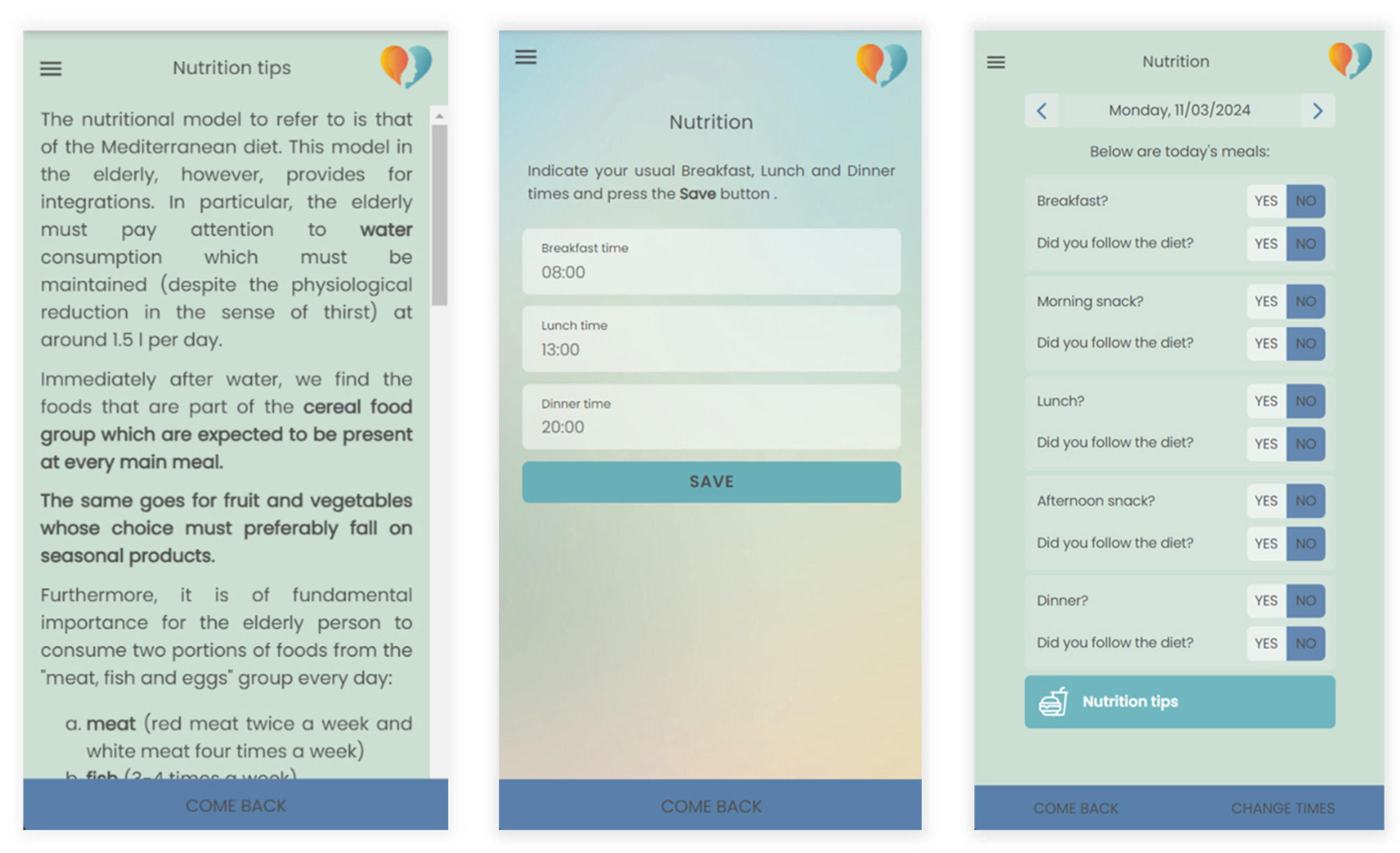
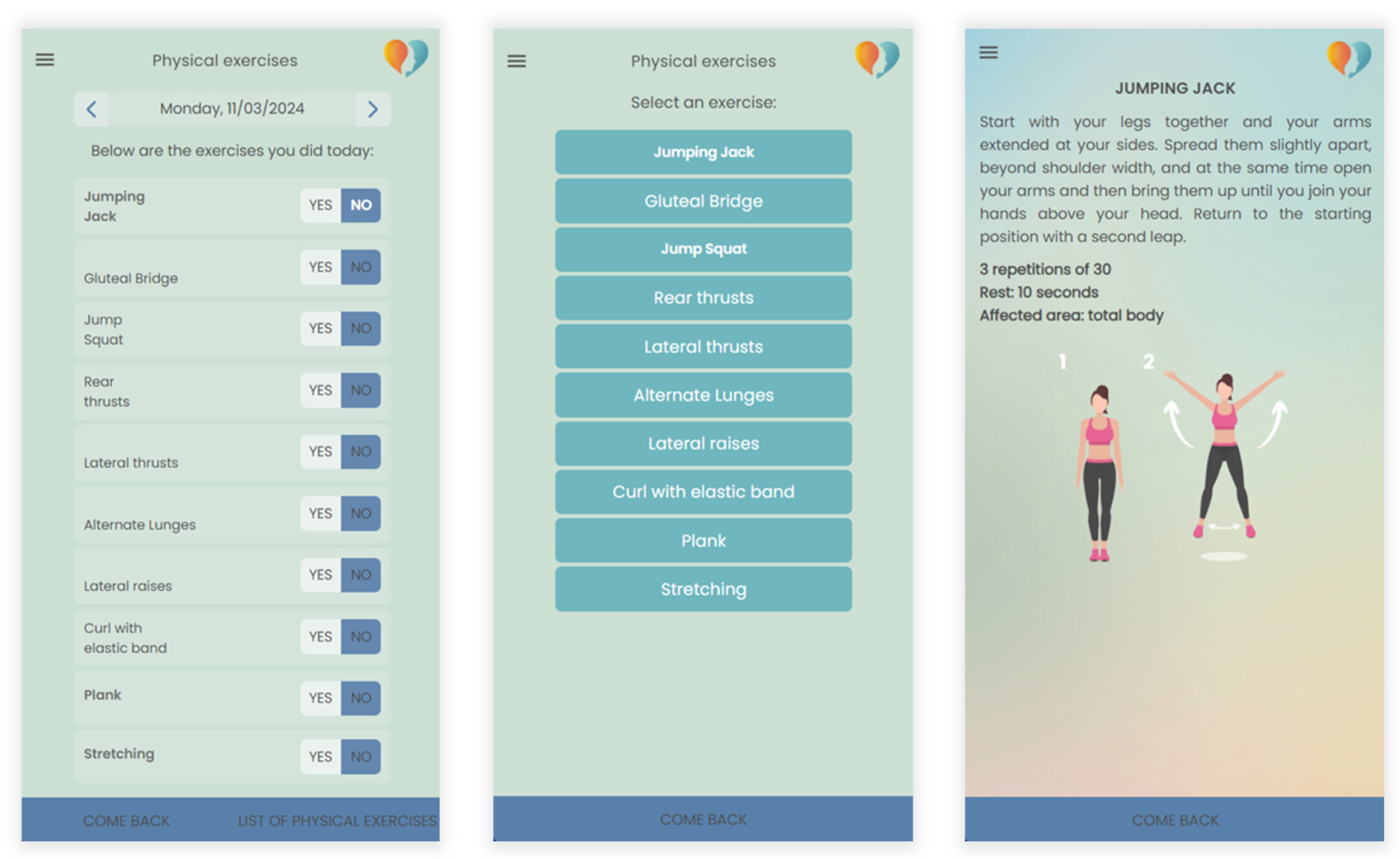
2.1.1. Nutrition and Physical Exercises Sections
2.1.2. Mindfulness Section
- Observing and letting go of thoughts, focusing on the present moment, with reflections on self-care and gratitude.
- Heightened awareness of bodily sensations.
- Emphasizes concentration on abdominal breathing and connecting with the present moment.
- Emphasizes the normality of the mind wandering, observing breath, and refocusing attention.
- Employing grounding techniques to connect with surroundings and manage thoughts and emotions.
- Focusing on posture, breath, letting go of distractions, and emphasizing self-care and gratitude.
- Focusing on breath and bodily sensations to deepen relaxation and awareness, encouraging gentle curiosity.
- Encouraging awareness of bodily sensations, thoughts, and emotions, and connecting with the present moment.
- Focusing on observing breath with curiosity, acknowledging distractions, and refocusing on breath.
- Using all the senses to imagine a vivid scene to deepen relaxation and awareness, acknowledging distractions like thoughts or feelings, noticing them without judgment, and refocusing on the scene.
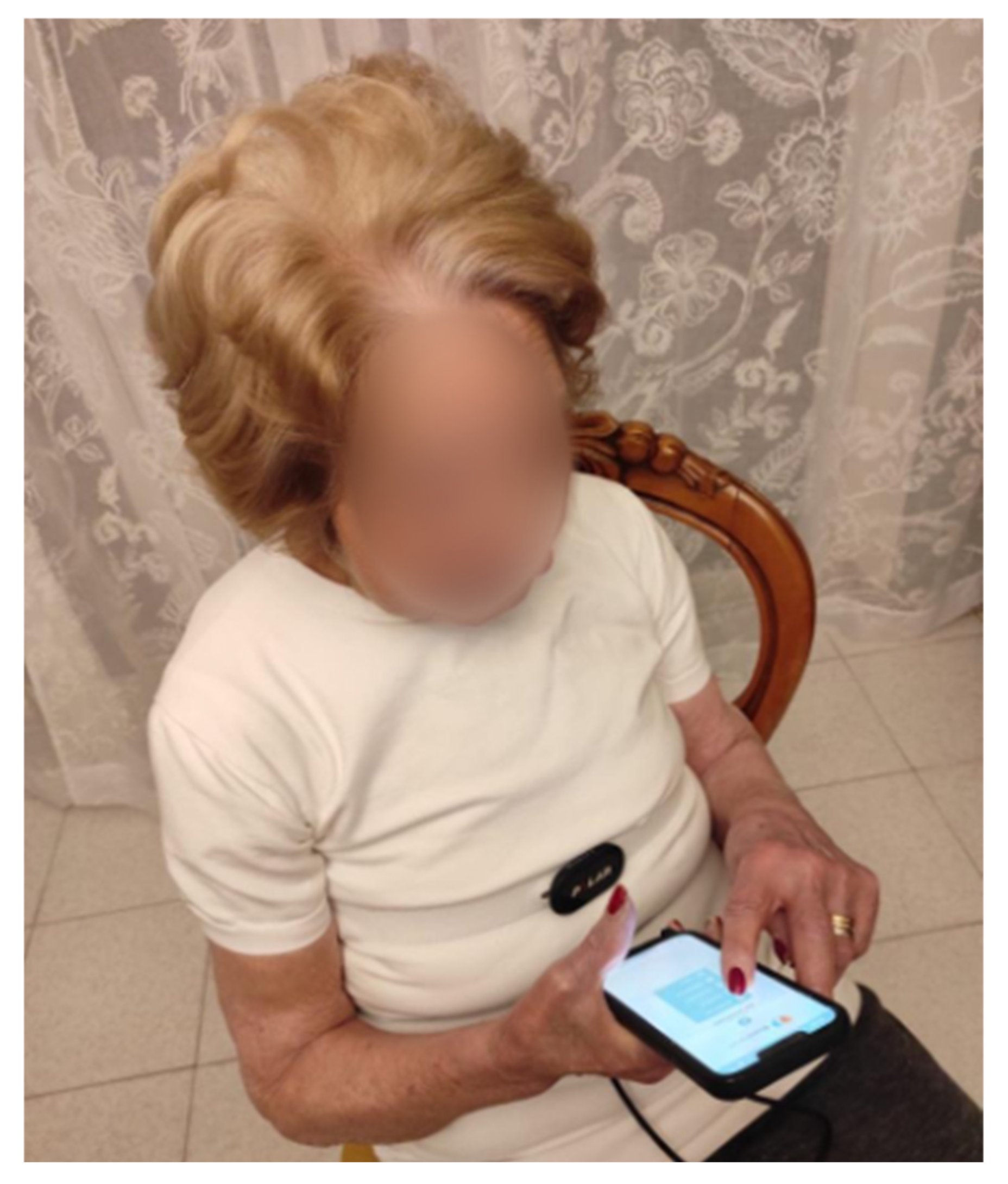
2.2. Usability Tests
2.3. Participants
2.4. Clinical Assessment
- Cognitive Defusion: Cognitive defusion involves creating distance from thoughts, reducing their impact. Instead of being fused with or dominated by thoughts, individuals learn techniques to observe thoughts without immediate attachment or identification. This allows for a more flexible and less reactive response to thoughts.
- Acceptance: Acceptance, in the ACT context, is about allowing thoughts and feelings to exist without struggling against them. Rather than trying to eliminate or control unwanted internal experiences, individuals practice accepting them as a natural part of the human experience. This process reduces the emotional struggle associated with difficult thoughts and emotions.
- Present Moment Awareness (Mindfulness): Mindfulness is the practice of being fully present in the current moment, paying attention to thoughts and feelings without judgment. It involves cultivating awareness and staying connected with the present rather than getting caught up in worries about the past or future.
- Self-as-Context: Self-as-context encourages individuals to recognize that they are not defined by their thoughts, feelings, or roles. Instead, they have a stable and consistent sense of self that remains unchanged by internal experiences. This process helps create a more resilient and less ego-identified sense of identity.
- Values Clarification: Values clarification involves exploring and clarifying the qualities and directions that a person values most in life. These values become a guide for decision-making and goal setting. Living in accordance with one’s values leads to a more meaningful and purposeful life.
- Committed Action: Once you have identified your values, committed action involves taking steps and making choices that align with those values. It is about moving in the direction of your values, even in the presence of difficulties or discomfort.
- The Mindfulness Awareness Attention Scale (MAAS) [41], made up of 15 items, enables the assessment of a fundamental aspect of dispositional mindfulness: the open and receptive awareness of the present moment.
- The Cognitive Fusion Questionnaire (CFQ-13) [42], a 13-item questionnaire used to evaluate cognitive defusion—the capacity to create distance from one’s thoughts and memories, facilitating the pursuit of personal goals and values independent of internal events.
- The Multidimensional Psychological Flexibility Inventory (MPFI) [40], consisting of 60 items, to examine both psychological inflexibility and flexibility.
2.5. Protocol
2.6. Statistical Analysis
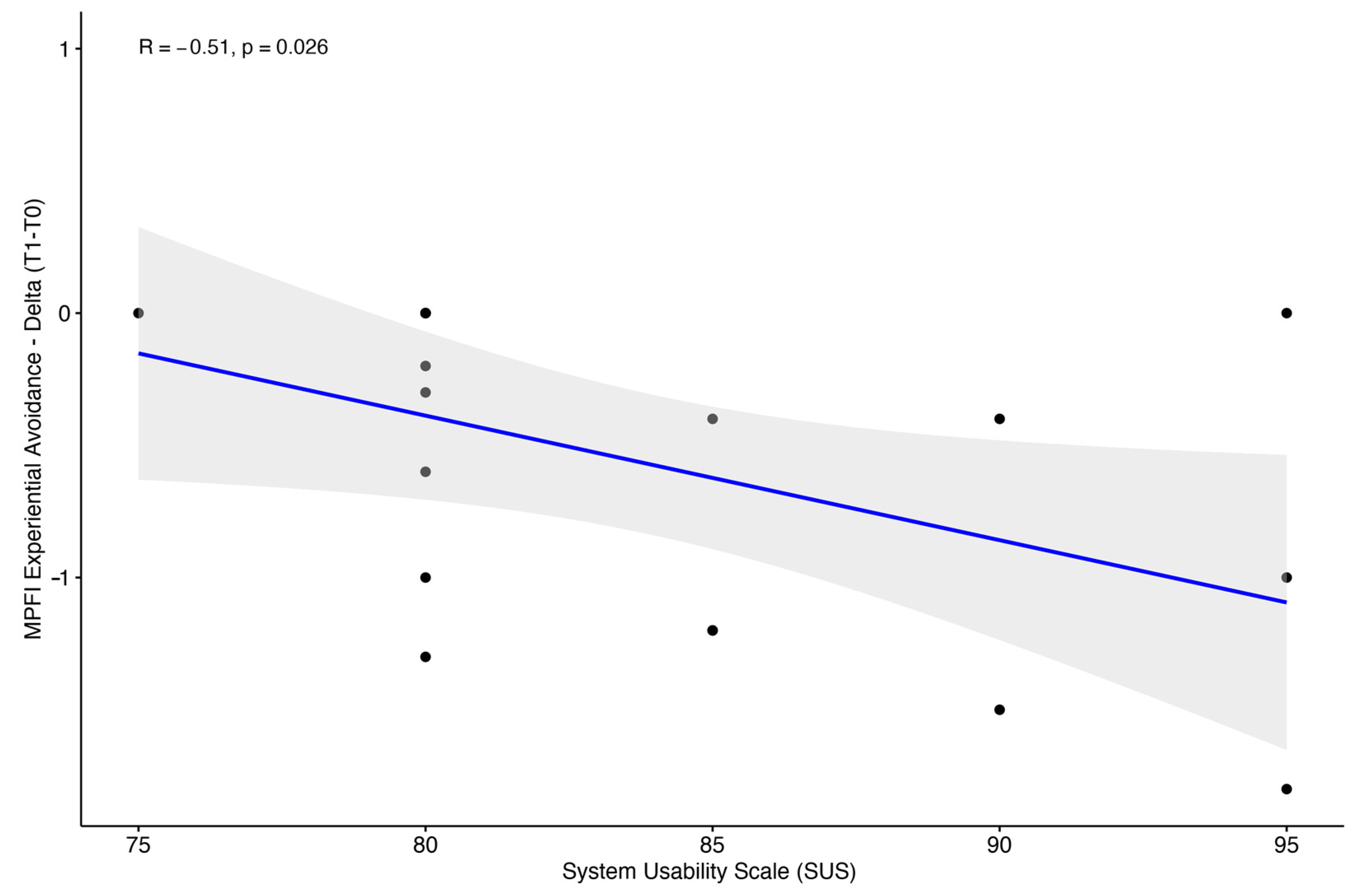
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ageing and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 27 March 2024).
- Tan, M.P. Healthcare for older people in lower and middle income countries. Age Ageing 2022, 51, afac016. [Google Scholar] [CrossRef]
- de Mendonça Lima, C.A.; Ivbijaro, G. Mental health and wellbeing of older people: Opportunities and challenges. Ment. Health Fam. Med. 2013, 10, 125–127. [Google Scholar] [PubMed]
- Sporinova, B.; Manns, B.; Tonelli, M.; Hemmelgarn, B.; MacMaster, F.; Mitchell, N.; Au, F.; Ma, Z.; Weaver, R.; Quinn, A. Association of Mental Health Disorders with Health Care Utilization and Costs Among Adults with Chronic Disease. JAMA Netw. Open 2019, 2, e199910. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Gao, Q.; Huo, L.; Yang, J. Impaired Activity of Daily Living Status of the Older Adults and Its Influencing Factors: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 15607. [Google Scholar] [CrossRef] [PubMed]
- Majnarić, L.T.; Bosnić, Z.; Guljaš, S.; Vučić, D.; Kurevija, T.; Volarić, M.; Martinović, I.; Wittlinger, T. Low Psychological Resilience in Older Individuals: An Association with Increased Inflammation, Oxidative Stress and the Presence of Chronic Medical Conditions. Int. J. Mol. Sci. 2021, 22, 8970. [Google Scholar] [CrossRef] [PubMed]
- Petkus, A.J.; Wetherell, J.L. Acceptance and Commitment Therapy with Older Adults: Rationale and Considerations. Cogn. Behav. Pract. 2013, 20, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Mental Health of Older Adults. Available online: https://www.who.int/news-room/fact-sheets/detail/mental-health-of-older-adults (accessed on 27 March 2024).
- Todhunter-Brown, A.; Baer, G.; Campbell, P.; Choo, P.L.; Forster, A.; Morris, J.; Pomeroy, V.M.; Langhorne, P. Physical rehabilitation approaches for the recovery of function and mobility following stroke. Cochrane Database Syst. Rev. 2014, 2014, CD001920. [Google Scholar]
- National Research Council (US) Panel on a Research Agenda and New Data for an Aging World. The Health of Aging Populations. In Preparing for an Aging World: The Case for Cross-National Research; National Academies Press: Washington, DC, USA, 2001. Available online: https://www.ncbi.nlm.nih.gov/books/NBK98373/ (accessed on 27 March 2024).
- Hofmann, S.G.; Asnaani, A.; Vonk, I.J.J.; Sawyer, A.T.; Fang, A. The Efficacy of Cognitive Behavioral Therapy: A Review of Meta-analyses. Cogn. Ther. Res. 2012, 36, 427–440. [Google Scholar] [CrossRef] [PubMed]
- Bond, F.; Hayes, S.; Barnes-Homes, D. Psychological Flexibility, ACT, and Organizational Behavior. J. Organ. Behav. Manag. 2006, 26, 25–54. [Google Scholar] [CrossRef]
- Doorley, J.D.; Goodman, F.R.; Kelso, K.C.; Kashdan, T.B. Psychological flexibility: What we know, what we do not know, and what we think we know. Soc. Pers. Psychol. Compass 2020, 14, 1–11. [Google Scholar] [CrossRef]
- Hayes, S.C.; Strosahl, K.D.; Wilson, K.G. (Eds.) Acceptance and Commitment Therapy: The Process and Practice of Mindful Change; Guilford Press: New York, NY, USA, 2011. [Google Scholar]
- Forman, E.M.; Herbert, J.D.; Moitra, E.; Yeomans, P.D.; Geller, P.A. A randomized controlled effectiveness trial of acceptance and commitment therapy and cognitive therapy for anxiety and depression. Behav. Modif. 2007, 31, 772–799. [Google Scholar] [CrossRef] [PubMed]
- Jentsch, V.L.; Wolf, O.T. The impact of emotion regulation on cardiovascular, neuroendocrine and psychological stress responses. Biol. Psychol. 2020, 154, 107893. [Google Scholar] [CrossRef] [PubMed]
- Rashidi, A.; Whitehead, L.; Newson, L.; Astin, F.; Gill, P.; Lane, D.A.; Lip, G.Y.H.; Neubeck, L.; Ski, C.F.; Thompson, D.R.; et al. The Role of Acceptance and Commitment Therapy in Cardiovascular and Diabetes Healthcare: A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 8126. [Google Scholar] [CrossRef] [PubMed]
- Kildal, E.; Stadskleiv, K.; Boysen, E.S.; Øderud, T.; Dahl, I.L.; Seeberg, T.M.; Guldal, S.; Strisland, F.; Morland, C.; Hassel, B. Increased heart rate functions as a signal of acute distress in non-communicating persons with intellectual disability. Sci. Rep. 2021, 11, 6479. [Google Scholar] [CrossRef] [PubMed]
- Berntson, G.G.; Bigger, J.T., Jr.; Eckberg, D.L.; Grossman, P.; Kaufmann, P.G.; Malik, M.; Nagaraja, H.N.; Porges, S.W.; Saul, J.P.; Stone, P.H.; et al. Heart rate variability: Origins, methods, and interpretive caveats. Psychophysiology 1997, 34, 623–648. [Google Scholar] [CrossRef] [PubMed]
- Bortolla, R.; Galli, M.; Spada, G.E.; Maffei, C. Mindfulness Effects on Mind Wandering and Autonomic Balance. Appl. Psychophysiol. Biofeedback 2022, 47, 53–64. [Google Scholar] [CrossRef]
- Meuldijk, D.; Wuthrich, V.M.; Rapee, R.M.; Draper, B.; Brodaty, H.; Cuijpers, P.; Cutler, H.; Hobbs, M.; Johnco, C.; Jones, M.; et al. Translating evidence-based psychological interventions for older adults with depression and anxiety into public and private mental health settings using a stepped care framework: Study protocol. Contemp. Clin. Trials 2021, 104, 106360. [Google Scholar] [CrossRef] [PubMed]
- Xiang, X.; Wu, S.; Zuverink, A.; Tomasino, K.N.; An, R.; Himle, J.A. Internet-Delivered Cognitive Behavioral Therapies for Late-Life Depressive Symptoms: A Systematic Review and Meta-analysis. Aging Ment. Health 2020, 24, 1196–1206. [Google Scholar] [CrossRef]
- Choi, N.G.; Gonzalez, J.M. Barriers and Contributors to Minority Older Adults’ Access to Mental Health Treatment: Perceptions of Geriatric Mental Health Clinicians. J. Gerontol. Soc. Work. 2005, 44, 115–135. [Google Scholar] [CrossRef]
- Weinberger, M.I.; Mateo, C.; Sirey, J.A. Perceived barriers to mental health care and goal setting among depressed, community-dwelling older adults. Patient Prefer. Adherence 2009, 3, 145–149. [Google Scholar] [CrossRef]
- Meuldijk, D.; Carlier, I.; van Vliet, I.M.; van Veen, T.; Wolterbeek, R.; van Hemert, A.; Zitman, F. The clinical effectiveness of concise cognitive behavioral therapy with or without pharmacotherapy for depressive and anxiety disorders; a pragmatic randomized controlled equivalence trial in clinical practice. Contemp. Clin. Trials 2016, 47, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Bouwmans, C.; Krol, M.; Severens, H.; Koopmanschap, M.; Brouwer, W.; Hakkaart-van Roijen, L. The iMTA Productivity Cost Questionnaire: A Standardized Instrument for Measuring and Valuing Health-Related Productivity Losses. Value Health 2015, 18, 753–758. [Google Scholar] [CrossRef] [PubMed]
- Sunderland, M.; Anderson, T.M.; Sachdev, P.S.; Titov, N.; Andrews, G. Lifetime and current prevalence of common DSM-IV mental disorders, their demographic correlates, and association with service utilisation and disability in older Australian adults. Aust. N. Z. J. Psychiatry 2015, 49, 145–155. [Google Scholar] [CrossRef]
- Paterniti, S.; Dufouil, C.; Alpérovitch, A. Long-term benzodiazepine use and cognitive decline in the elderly: The Epidemiology of Vascular Aging Study. J. Clin. Psychopharmacol. 2002, 22, 285–293. [Google Scholar] [CrossRef]
- Norton, A.R.; Abbott, M.J.; Norberg, M.M.; Hunt, C. A systematic review of mindfulness and acceptance-based treatments for social anxiety disorder. J. Clin. Psychol. 2015, 71, 283–301. [Google Scholar] [CrossRef] [PubMed]
- de Beurs, E.; Beekman, A.T.F.; van Balkom, A.J.L.M.; Deeg, D.J.H.; van Dyck, R.; van Tilburg, W. Consequences of anxiety in older persons: Its effect on disability, well-being and use of health services. Psychol. Med. 1999, 29, 583–593. [Google Scholar] [CrossRef] [PubMed]
- Hood, M.; Wilson, R.; Corsica, J.; Bradley, L.; Chirinos, D.; Vivo, A. What do we know about mobile applications for diabetes self-management? A review of reviews. J. Behav. Med. 2016, 39, 981–994. [Google Scholar] [CrossRef]
- Iribarren, S.J.; Akande, T.O.; Kamp, K.J.; Barry, D.; Kader, Y.G.; Suelzer, E. Effectiveness of Mobile Apps to Promote Health and Manage Disease: Systematic Review and Meta-analysis of Randomized Controlled Trials. JMIR mHealth uHealth 2021, 9, e21563. [Google Scholar] [CrossRef]
- Koh, J.; Tng, G.Y.Q.; Hartanto, A. Potential and Pitfalls of Mobile Mental Health Apps in Traditional Treatment: An Umbrella Review. J. Pers. Med. 2022, 12, 1376. [Google Scholar] [CrossRef]
- ISO 9241-11:2018; Ergonomics of Human-System Interaction. Part 11: Usability: Definitions and Concepts. ISO: Geneva, Switzerland, 2018. Available online: https://www.iso.org/standard/63500.html (accessed on 13 March 2024).
- Tuena, C.; Pedroli, E.; Trimarchi, P.D.; Gallucci, A.; Chiappini, M.; Goulene, K.; Gaggioli, A.; Riva, G.; Lattanzio, F.; Giunco, F.; et al. Usability Issues of Clinical and Research Applications of Virtual Reality in Older People: A Systematic Review. Front. Hum. Neurosci. 2020, 14, 93. [Google Scholar] [CrossRef]
- Lewis, J.R.; Sauro, J. The Factor Structure of the System Usability Scale. In Human Centered Design; Kurosu, M., Ed.; Springer: Berlin/Heidelberg, Germany, 2009; pp. 94–103. [Google Scholar]
- Bangor, A.; Kortum, P.; Miller, J. Determining What Individual SUS Scores Mean: Adding an Adjective Rating Scale. J. Usability Stud. 2009, 4, 114–123. [Google Scholar]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Tombaugh, T.N.; McIntyre, N.J. The mini-mental state examination: A comprehensive review. J. Am. Geriatr. Soc. 1992, 40, 922–935. [Google Scholar] [CrossRef]
- Rolffs, J.L.; Rogge, R.D.; Wilson, K.G. Disentangling Components of Flexibility via the Hexaflex Model: Development and Validation of the Multidimensional Psychological Flexibility Inventory (MPFI). Assessment 2018, 25, 458–482. [Google Scholar] [CrossRef] [PubMed]
- Brown, K.W.; Ryan, R.M. Mindful Attention Awareness Scale (MAAS); [Database Record]; APA PsycTests: Washington, DC, USA, 2003. [Google Scholar] [CrossRef]
- Gillanders, D.T.; Bolderston, H.; Bond, F.W.; Dempster, M.; Flaxman, P.E.; Campbell, L.; Kerr, S.; Tansey, L.; Noel, P.; Ferenbach, C.; et al. Cognitive Fusion Questionnaire (CFQ); [Database Record]; APA PsycTests: Washington, DC, USA, 2014. [Google Scholar] [CrossRef]
- Nielsen, J. Designing Web Usability: The Practice of Simplicity; New Riders Publishing: Indianapolis, IN, USA, 1999; Available online: https://www.nngroup.com/books/designing-web-usability/ (accessed on 22 July 2024).
- Petkus, A.J.; Gum, A.; Wetherell, J.L. Thought suppression is associated with psychological distress in homebound older adults. Depress. Anxiety 2012, 29, 219–225. [Google Scholar] [CrossRef] [PubMed]
- Loucks, E.B.; Schuman-Olivier, Z.; Britton, W.B.; Fresco, D.M.; Desbordes, G.; Brewer, J.A.; Fulwiler, C. Mindfulness and Cardiovascular Disease Risk: State of the Evidence, Plausible Mechanisms, and Theoretical Framework. Curr. Cardiol. Rep. 2015, 17, 112. [Google Scholar] [CrossRef] [PubMed]
- Vailati Riboni, F.; Sadowski, I.; Comazzi, B.; Pagnini, F. Mindful Age and Technology: A Qualitative Analysis of a Tablet/Smartphone App Intervention Designed for Older Adults. Integr. Psychol. Behav. Sci. 2022, 56, 739–754. [Google Scholar] [CrossRef]
- Mahlo, L.; Windsor, T.D. Feasibility, Acceptability, and Preliminary Efficacy of an App-Based Mindfulness-Meditation Program Among Older Adults. Gerontologist 2021, 61, 775–786. [Google Scholar] [CrossRef]

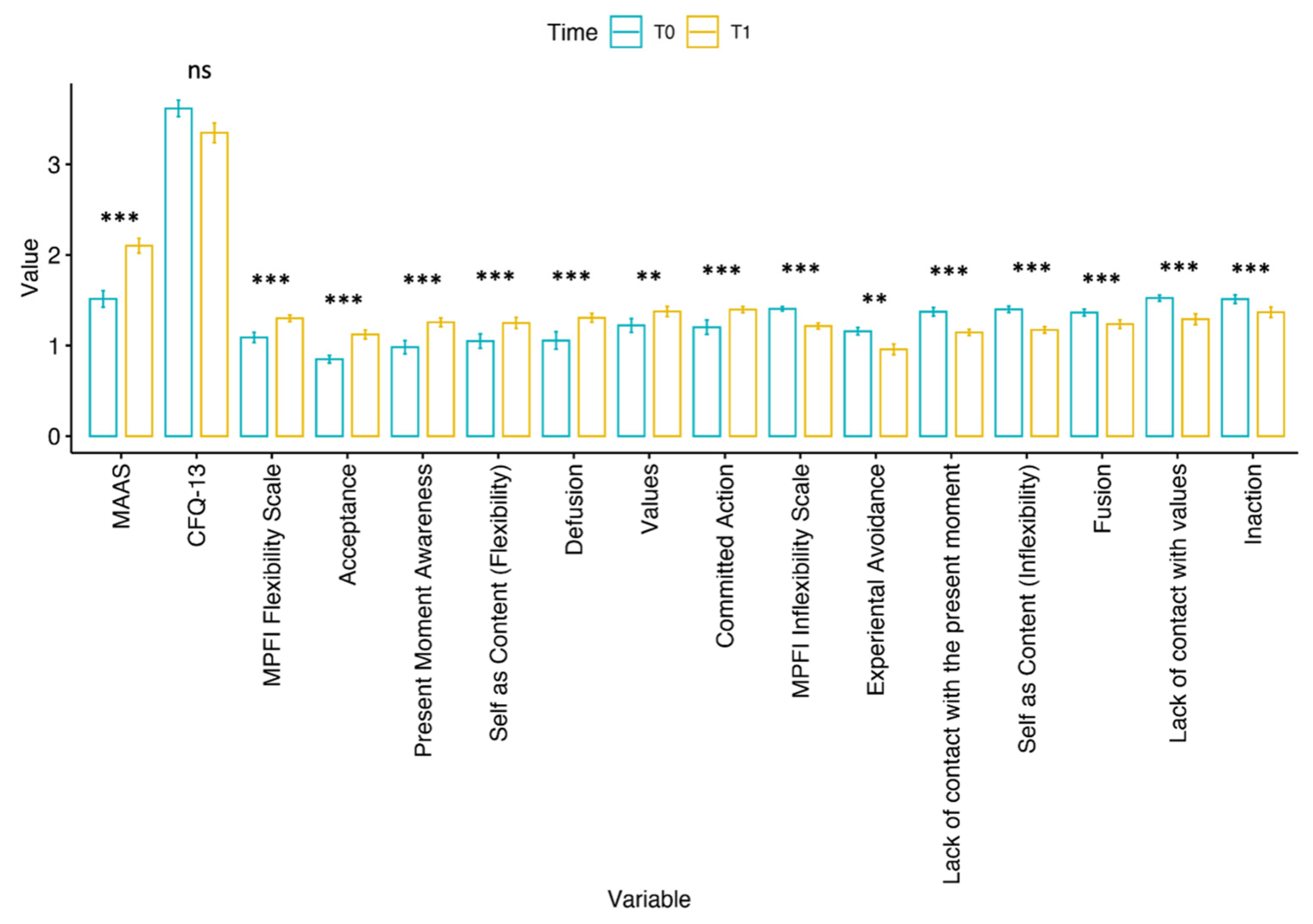
| Variable | Statistics | p-Value | Mean Difference |
|---|---|---|---|
| MAAS | 0.0 | <0.001 | −3.500 |
| CFQ-13 | 99.0 | 0.297 | 5.000 |
| MPFI Flexibility Scale | 0.0 | <0.001 | −0.700 |
| Acceptance | 0.0 | <0.001 | −0.900 |
| Present Moment Awareness | 0.0 | <0.001 | −1.050 |
| Self as Content (Flexibility) | 0.0 | 0.001 | −0.800 |
| Defusion | 0.0 | 0.001 | −0.950 |
| Values | 0.0 | 0.004 | −0.950 |
| Committed Action | 0.0 | 0.001 | −0.500 |
| MPFI Inflexibility Scale | 210.0 | <0.001 | 0.675 |
| Experiential Avoidance | 78.0 | 0.003 | 0.900 |
| Lack of contact with the present moment | 136.0 | <0.001 | 1.000 |
| Self as Content (Inflexibility) | 153.0 | <0.001 | 0.950 |
| Fusion | 131.5 | 0.001 | 0.500 |
| Lack of contact with values | 171.0 | <0.001 | 0.900 |
| Inaction | 152.0 | <0.001 | 0.650 |
| Time Point | Mean | Median | SD | Range | Minimum | Maximum |
|---|---|---|---|---|---|---|
| T0 | 81.5 | 80.4 | 9.60 | 34.1 | 66.6 | 100.7 |
| T1 | 75.3 | 75.5 | 10.95 | 47.9 | 46.0 | 94.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bruschetta, R.; Latella, D.; Formica, C.; Campisi, S.; Failla, C.; Marino, F.; Iacono Isidoro, S.; Giambò, F.M.; Bonanno, L.; Cerasa, A.; et al. “BrainHeart”: Pilot Study on a Novel Application for Elderly Well-Being Based on Mindfulness Acceptance and Commitment Therapy. Bioengineering 2024, 11, 787. https://doi.org/10.3390/bioengineering11080787
Bruschetta R, Latella D, Formica C, Campisi S, Failla C, Marino F, Iacono Isidoro S, Giambò FM, Bonanno L, Cerasa A, et al. “BrainHeart”: Pilot Study on a Novel Application for Elderly Well-Being Based on Mindfulness Acceptance and Commitment Therapy. Bioengineering. 2024; 11(8):787. https://doi.org/10.3390/bioengineering11080787
Chicago/Turabian StyleBruschetta, Roberta, Desiree Latella, Caterina Formica, Simona Campisi, Chiara Failla, Flavia Marino, Serena Iacono Isidoro, Fabio Mauro Giambò, Lilla Bonanno, Antonio Cerasa, and et al. 2024. "“BrainHeart”: Pilot Study on a Novel Application for Elderly Well-Being Based on Mindfulness Acceptance and Commitment Therapy" Bioengineering 11, no. 8: 787. https://doi.org/10.3390/bioengineering11080787
APA StyleBruschetta, R., Latella, D., Formica, C., Campisi, S., Failla, C., Marino, F., Iacono Isidoro, S., Giambò, F. M., Bonanno, L., Cerasa, A., Quartarone, A., Marino, S., Pioggia, G., Calabrò, R. S., & Tartarisco, G. (2024). “BrainHeart”: Pilot Study on a Novel Application for Elderly Well-Being Based on Mindfulness Acceptance and Commitment Therapy. Bioengineering, 11(8), 787. https://doi.org/10.3390/bioengineering11080787















