Recent Advances in the Use of Polyhydroyalkanoates in Biomedicine
Abstract
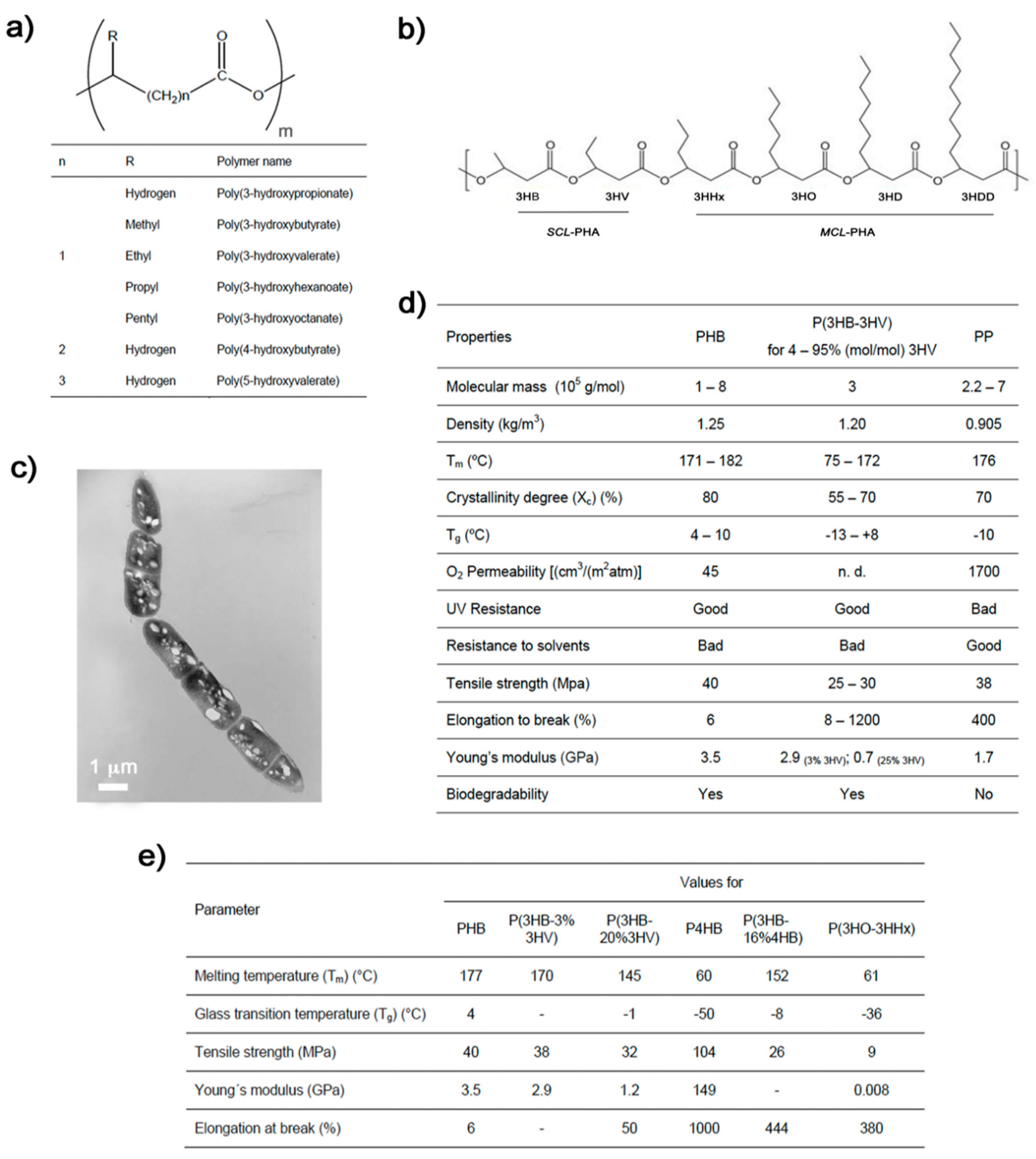
:1. Introduction
2. Tissue Engineering
2.1. Hard Tissue
2.1.1. Bone Tissue Engineering
2.1.2. Cartilage
2.2. Soft Tissue
2.2.1. Cardiac Tissue Engineering
2.2.2. Wound Healing
2.2.3. PHAs for Organ Tissues
3. Drug Delivery Systems
4. Conclusions
Funding
Conflicts of Interest
References
- Rodríguez-Contreras, A. Concepts and Recent Advances on Biopolymers for Biomedical Applications: Special Mention to the PHAs Family. Adv. Biotechnol. 2019, IV, 1–27. [Google Scholar]
- Mavelil-Sam, R.; Pothan, L.A.; Thomas, S. Polyssacharide and Protein BsedAerogels: An Introductory Outlook. In Biobased Aerogels: Polysaccharide and Protein-Based Materials; Thomas, S., Pothan, L.A., Mavelil-Sam, R., Eds.; Royal Society of Chemistry: London, UK, 2018. [Google Scholar]
- Won, J.-E.; El-Fiqi, A.; Jegal, S.-H.; Han, C.-M.; Lee, E.-J.; Knowles, J.C.; Kim, H.-W. Gelatin-apatite bone mimetic co-precipitates incorporated within biopolymer matrix to improve mechanical and biological properties useful for hard tissue repair. J. Biomater. Appl. 2013, 28, 1213–1225. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Augustine, R. Skin bioprinting: A novel approach for creating artificial skin from synthetic and natural building blocks. Prog. Biomater. 2018, 7, 77–92. [Google Scholar] [CrossRef] [PubMed]
- Park, H.-H.; Ko, S.-C.; Oh, G.-W.; Heo, S.-J.; Kang, D.-H.; Bae, S.-Y.; Jung, W.-K. Fabrication and characterization of phlorotannins/poly (vinyl alcohol) hydrogel for wound healing application. J. Biomater. Sci. Polym. Ed. 2018, 29, 972–983. [Google Scholar] [CrossRef] [PubMed]
- Caddeo, S.; Mattioli-Belmonte, M.; Cassino, C.; Barbani, N.; Dicarlo, M.; Gentile, P.; Baino, F.; Sartori, S.; Vitale-Brovarone, C.; Ciardelli, G. Newly-designed collagen/polyurethane bioartificial blend as coating on bioactive glass-ceramics for bone tissue engineering applications. Mater. Sci. Eng. C 2019, 96, 218–233. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.Y. Bacterial polyhydroxyalkanoates. Biotechnol. Bioeng. 1996, 49, 1–14. [Google Scholar] [CrossRef]
- Valappil, S.P.; Peiris, D.; Langley, G.J.; Herniman, J.M.; Boccaccini, A.R.; Bucke, C.; Roy, I. Polyhydroxyalkanoate (PHA) biosynthesis from structurally unrelated carbon sources by a newly characterized Bacillus spp. J. Biotechnol. 2007, 127, 475–487. [Google Scholar] [CrossRef] [PubMed]
- Chen, G. Plastics from Bacteria: Natural Functions and Applications, Microbiology Monographs; Chen, G.G.-Q., Ed.; Springer: Berlin/Heidelberg, Germany, 2010; Volume 14. [Google Scholar]
- Chen, G.-Q. A microbial polyhydroxyalkanoates (PHA) based bio- and materials industry. Chem. Soc. Rev. 2009, 38, 2434–2446. [Google Scholar] [CrossRef]
- Koller, M. Production of Poly Hydroxyalkanoate (PHA) biopolyesters by extremophiles? MOJ Polym. Sci. 2017, 1, 69–85. [Google Scholar]
- Sudesh, K.; Abe, H.; Doi, Y. Synthesis, structure and properties of polyhydroxyalkanoates: Biological polyesters. Prog. Polym. Sci. 2000, 25, 1503–1555. [Google Scholar] [CrossRef]
- Yadav, P.; Yadav, H.; Shah, V.G.; Shah, G.; Dhaka, G. Biomedical Biopolymers, their Origin and Evolution in Biomedical Sciences: A Systematic Review. J. Clin. Diagn. Res. 2015, 9, ZE21–ZE25. [Google Scholar] [CrossRef] [PubMed]
- Koller, M. Polyhydroxyalkanoate Biosynthesis at the Edge of Water Activitiy-Haloarchaea as Biopolyester Factories. Bioengineering 2019, 6, 34. [Google Scholar] [CrossRef] [PubMed]
- Reddy, C.S.K.; Rashmi Ghai, R.; Kalia, V.C. Polyhydroxyalkanoates: An overview. Bioresour. Technol. 2003, 87, 137–146. [Google Scholar] [CrossRef]
- Koller, M. Chemical and Biochemical Engineering Approaches in Manufacturing Polyhydroxyalkanoate (PHA) Biopolyesters of Tailored Structure with Focus on the Diversity of Building Blocks. Chem. Biochem. Eng. Q. 2019, 32, 413–438. [Google Scholar] [CrossRef]
- Koller, M.; Salerno, A.; Dias, M.; Reiterer, A.; Braunegg, G. Modern Biotechnological Polymer Synthesis: A Review. Food Technol. Biotechnol. 2010, 48, 255–269. [Google Scholar]
- Constantinides, C.; Basnett, P.; Lukasiewicz, B.; Carnicer, R.; Swider, E.; Majid, Q.A.; Srinivas, M.; Carr, C.A.; Roy, I. In Vivo Tracking and 1H/19F Magnetic Resonance Imaging of Biodegradable Polyhydroxyalkanoate/Polycaprolactone Blend Scaffolds Seeded with Labeled Cardiac Stem Cells. ACS Appl. Mater. Interfaces 2018, 10, 25056–25068. [Google Scholar] [CrossRef]
- Fei, T.; Cazeneuve, S.; Wen, Z.; Wu, L.; Wang, T. Effective recovery of poly-β-hydroxybutyrate (PHB) biopolymer from Cupriavidus necator using a novel and environmentally friendly solvent system. Biotechnol. Prog. 2016, 32, 678–685. [Google Scholar] [CrossRef]
- Koller, M. Biodegradable and Biocompatible Polyhydroxy-alkanoates (PHA): Auspicious Microbial Macromolecules for Pharmaceutical and Therapeutic Applications. Molecules 2018, 23, 362. [Google Scholar] [CrossRef]
- Köse, G.T.; Kenar, H.; Hasırcı, N.; Hasırcı, V. Macroporous poly(3-hydroxybutyrate-co-3-hydroxyvalerate) matrices for bone tissue engineering. Biomaterials 2003, 24, 1949–1958. [Google Scholar] [CrossRef]
- Grigore, M.E.; Grigorescu, R.M.; Iancu, L.; Ion, R.-M.; Zaharia, C.; Andrei, E.R. Methods of synthesis, properties and biomedical applications of polyhydroxyalkanoates: A review. J. Biomater. Sci. Polym. Ed. 2019, 30, 695–712. [Google Scholar] [CrossRef]
- Berezina, N. Enhancing the 3-hydroxyvalerate component in bioplastic PHBV production by Cupriavidus necator. Biotechnol. J. 2012, 7, 304–309. [Google Scholar] [CrossRef] [PubMed]
- Rahayu, A.; Zaleha, Z.; Yahya, A.R.M.; Majid, M.I.A.; Amirul, A.A. Production of copolymer poly(3-hydroxybutyrate-co-4-hydroxybutyrate) through a one-step cultivation process. World J. Microbiol. Biotechnol. 2008, 24, 2403–2409. [Google Scholar] [CrossRef]
- Shijun, X.; Junsheng, M.; Jianqun, Z.; Ping, B. In vitro three-dimensional coculturing poly3-hydroxybutyrate-co-3-hydroxyhexanoate with mouse-induced pluripotent stem cells for myocardial patch application. J. Biomater. Appl. 2016, 30, 1273–1282. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.; Chen, J.-C.; Ma, Y.-M.; Chen, G.-Q. Engineering biosynthesis of polyhydroxyalkanoates (PHA) for diversity and cost reduction. Metab. Eng. 2019. [Google Scholar] [CrossRef] [PubMed]
- Brigham, C.J.; Riedel, S.L. The Potential of Polyhydroxyalkanoate Production from Food Wastes. Appl. Food Biotechnol. 2019, 6. [Google Scholar] [CrossRef]
- Rodriguez-Contreras, A.; Koller, M.; Miguel, M.-d.S.D.; Calafell, M.; Braunegg, G.; Marqués-Calvo, M.S. Novel Poly[(R)-3-hydroxybutyrate]-producing bacterium isolated from a Bolivian hypersaline lake. Food Technol. Biotechnol. 2013, 51, 123–130. [Google Scholar]
- Akaraonye, E.; Keshavarz, T.; Roy, I. Production of polyhydroxyalkanoates: The future green materials of choice. J. Chem. Technol. Biotechnol. 2010, 85, 732–743. [Google Scholar] [CrossRef]
- Waghmare, V.S.; Wadke, P.R.; Dyawanapelly, S.; Deshpande, A.; Jain, R.; Dandekar, P. Starch based nanofibrous scaffolds for wound healing applications. Bioact. Mater. 2018, 3, 255–266. [Google Scholar] [CrossRef] [PubMed]
- Findrik Balogová, A.; Hudák, R.; Tóth, T.; Schnitzer, M.; Feranc, J.; Bakoš, D.; Živčák, J. Determination of geometrical and viscoelastic properties of PLA/PHB samples made by additive manufacturing for urethral substitution. J. Biotechnol. 2018, 284, 123–130. [Google Scholar] [CrossRef] [PubMed]
- Lizarraga-Valderrama, L.R.; Taylor, C.S.; Claeyssens, F.; Haycock, J.W.; Knowles, J.C.; Roy, I. Unidirectional neuronal cell growth and differentiation on aligned polyhydroxyalkanoate blend microfibres with varying diameters. J. Tissue Eng. Regen. Med. 2019. [Google Scholar] [CrossRef] [PubMed]
- Butt, F.I.; Muhammad, N.; Hamid, A.; Moniruzzaman, M.; Sharif, F. Recent progress in the utilization of biosynthesized polyhydroxyalkanoates for biomedical applications—Review. Int. J. Biol. Macromol. 2018, 120, 1294–1305. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.K.; Srivastava, J.K.; Chandel, A.K.; Sharma, L.; Mallick, N.; Singh, S.P. Biomedical applications of microbially engineered polyhydroxyalkanoates: An insight into recent advances, bottlenecks, and solutions. Appl. Microbiol. Biotechnol. 2019, 103, 2007–2032. [Google Scholar] [CrossRef] [PubMed]
- Kai, G.; Martin, D.P. Chapter 7: Poly-4-hydroxybutyrate (P4HB) in Biomedical Applications and Tissue Engineering. In Biodegradable Polymers, Volume 2: New Biomaterials Advancement and Challenges; Chu, C.-C., Ed.; Nova Sience: Hauppauge, NY, USA, 2015; pp. 199–231. [Google Scholar]
- Degli Esposti, M.; Chiellini, F.; Bondioli, F.; Morselli, D.; Fabbri, P. Highly porous PHB-based bioactive scaffolds for bone tissue engineering by in situ synthesis of hydroxyapatite. Mater. Sci. Eng. C 2019, 100, 286–296. [Google Scholar] [CrossRef] [PubMed]
- Chernozem, R.V.; Surmeneva, M.A.; Shkarina, S.N.; Loza, K.; Epple, M.; Ulbricht, M.; Cecilia, A.; Krause, B.; Baumbach, T.; Abalymov, A.A.; et al. Piezoelectric 3-D Fibrous Poly(3-hydroxybutyrate)-Based Scaffolds Ultrasound-Mineralized with Calcium Carbonate for Bone Tissue Engineering: Inorganic Phase Formation, Osteoblast Cell Adhesion, and Proliferation. ACS Appl. Mater. Interfaces 2019, 11, 19522–19533. [Google Scholar] [CrossRef] [PubMed]
- Meischel, M.; Eichler, J.; Martinelli, E.; Karr, U.; Weigel, J.; Schmöller, G.; Tschegg, E.K.; Fischerauer, S.; Weinberg, A.M.; Stanzl-Tschegg, S.E. Adhesive strength of bone-implant interfaces and in-vivo degradation of PHB composites for load-bearing applications. J. Mech. Behav. Biomed. Mater. 2016, 53, 104–118. [Google Scholar] [CrossRef] [PubMed]
- Sadat-Shojai, M.; Khorasani, M.-T.; Jamshidi, A. A new strategy for fabrication of bone scaffolds using electrospun nano-HAp/PHB fibers and protein hydrogels. Chem. Eng. J. 2016, 289, 38–47. [Google Scholar] [CrossRef]
- Ding, Y.; Li, W.; Müller, T.; Schubert, D.W.; Boccaccini, A.R.; Yao, Q.; Roether, J.A. Electrospun Polyhydroxybutyrate/Poly(ε-caprolactone)/58S Sol–Gel Bioactive Glass Hybrid Scaffolds with Highly Improved Osteogenic Potential for Bone Tissue Engineering. ACS Appl. Mater. Interfaces 2016, 8, 17098–17108. [Google Scholar] [CrossRef]
- Ching, K.Y.; Andriotis, O.G.; Li, S.; Basnett, P.; Su, B.; Roy, I.; Tare, R.S.; Sengers, B.G.; Stolz, M. Nanofibrous poly(3-hydroxybutyrate)/poly(3-hydroxyoctanoate) scaffolds provide a functional microenvironment for cartilage repair. J. Biomater. Appl. 2016, 31, 77–91. [Google Scholar] [CrossRef] [Green Version]
- Toloue, E.B.; Karbasi, S.; Salehi, H.; Rafienia, M. Evaluation of Mechanical Properties and Cell Viability of Poly (3-Hydroxybutyrate)-Chitosan/Al(2)O(3) Nanocomposite Scaffold for Cartilage Tissue Engineering. J. Med. Signals Sens. 2019, 9, 111–116. [Google Scholar] [CrossRef]
- Bagdadi, A.V.; Safari, M.; Dubey, P.; Basnett, P.; Sofokleous, P.; Humphrey, E.; Locke, I.; Edirisinghe, M.; Terracciano, C.; Boccaccini, A.R.; et al. Poly(3-hydroxyoctanoate), a promising new material for cardiac tissue engineering. J. Tissue Eng. Regen. Med. 2018, 12, e495–e512. [Google Scholar] [CrossRef]
- Ma, Y.-X.; Mu, J.-S.; Zhang, J.-Q.; Bo, P. Myocardial Patch Formation by Three-Dimensional 3-Hydroxybutyrate-co-4-Hydroxybutyrate Cultured with Mouse Embryonic Stem Cells. J. Biomater. Tissue Eng. 2016, 6, 629–634. [Google Scholar] [CrossRef]
- Xue, Y.; Sant, V.; Phillippi, J.; Sant, S. Biodegradable and biomimetic elastomeric scaffolds for tissue-engineered heart valves. Acta Biomater. 2017, 48, 2–19. [Google Scholar] [CrossRef]
- Chen, Q.; Liang, S.; Thouas, G.A. Elastomeric biomaterials for tissue engineering. Prog. Polym. Sci. 2013, 38, 584–671. [Google Scholar] [CrossRef]
- Shishatskaya, E.I.; Nikolaeva, E.D.; Vinogradova, O.N.; Volova, T.G. Experimental wound dressings of degradable PHA for skin defect repair. J. Mater. Sci. Mater. Med. 2016, 27, 165. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sezer, A.D.; Cevher, E. Biopolymers as Wound Healing Materials: Challenges and New Strategies. In Biomaterials Applications for Nanomedicine; Rosario, P., Ed.; IntechOpen Limited: London, UK, 2011; pp. 383–414. [Google Scholar]
- Marcano, A.; Bou Haidar, N.; Marais, S.; Valleton, J.-M.; Duncan, A.C. Designing Biodegradable PHA-Based 3D Scaffolds with Antibiofilm Properties for Wound Dressings: Optimization of the Microstructure/Nanostructure. ACS Biomater. Sci. Eng. 2017, 3, 3654–3661. [Google Scholar] [CrossRef]
- Li, P.; Zhang, J.; Liu, J.; Ma, H.; Liu, J.; Lie, P.; Wang, Y.; Liu, G.; Zeng, H.; Li, Z.; et al. Promoting the recovery of injured liver with poly (3-hydroxybutyrate-co-3-hydroxyvalerate-co-3-hydroxyhexanoate) scaffolds loaded with umbilical cord-derived mesenchymal stem cells. Tissue Eng Part A 2015, 21, 603–615. [Google Scholar] [CrossRef] [PubMed]
- Su, Z.; Li, P.; Wu, B.; Ma, H.; Wang, Y.; Liu, G.; Zeng, H.; Li, Z.; Wei, X. PHBVHHx scaffolds loaded with umbilical cord-derived mesenchymal stem cells or hepatocyte-like cells differentiated from these cells for liver tissue engineering. Mater. Sci. Eng. C 2014, 45, 374–382. [Google Scholar] [CrossRef]
- Tashjian, R.; Kolz, C.; Suter, T.; Henninger, H. Biomechanics of Polyhydroxyalkanoate Mesh-Augmented Single-Row Rotator Cuff Repairs. Am. J. Orthop. 2016, 45, E527–E533. [Google Scholar]
- Yutaka, T.; Buenaventurada, C. Degradation of Microbial Polyesters. Biotechnol. Lett. 2004, 26, 1181–1189. [Google Scholar]
- Rodríguez-Contreras, A.; Calafell-Monfort, M.; Marqués-Calvo, M.S. Enzymatic degradation of poly(3-hydroxybutyrate) by a commercial lipase. Polym. Degrad. Stab. 2012, 97, 2473–2476. [Google Scholar] [CrossRef]
- Rodríguez-Contreras, A.; Calafell-Monfort, M.; Marqués-Calvo, M.S. Enzymatic degradation of poly(3-hydroxybutyrate-co-4-hydroxybutyrate) by commercial lipases. Polym. Degrad. Stab. 2012, 97, 597–604. [Google Scholar] [CrossRef]
- Misra, S.K.; Valappil, S.P.; Roy, I.; Boccaccini, A.R. Polyhydroxyalkanoate (PHA)/Inorganic Phase Composites for Tissue Engineering Applications. Biomacromolecules 2006, 7, 2249–2258. [Google Scholar] [CrossRef]
- Gil-Castell, O.; Badia, J.D.; Bou, J.; Ribes-Greus, A. Performance of Polyester-Based Electrospun Scaffolds under In Vitro Hydrolytic Conditions: From Short-Term to Long-Term Applications. Nanomaterials 2019, 9, 786. [Google Scholar] [CrossRef]
- Errico, C.; Bartoli, C.; Chiellini, F.; Chiellini, E. Poly(hydroxyalkanoates)-Based Polymeric Nanoparticles for Drug Delivery. J. Biomed. Biotechnol. 2009, 2009, 10. [Google Scholar] [CrossRef]
- Li, Z.; Loh, X.J. Recent advances of using polyhydroxyalkanoate-based nanovehicles as therapeutic delivery carriers. Nanomed. Nanobiotechnology 2017, 9, e1429. [Google Scholar] [CrossRef]
- Masood, F. Polymeric nanoparticles for targeted drug delivery system for cancer therapy. Mater. Sci. Eng. C 2016, 60, 569–578. [Google Scholar] [CrossRef]
- Michalak, M.; Kurcok, P.; Hakkarainen, M. Polyhydroxyalkanoate-based drug delivery systems. Polym. Int. 2017, 66, 617–622. [Google Scholar] [CrossRef]
- Pramual, S.; Assavanig, A.; Bergkvist, M.; Batt, C.A.; Sunintaboon, P.; Lirdprapamongkol, K.; Svasti, J.; Niamsiri, N. Development and characterization of bio-derived polyhydroxyalkanoate nanoparticles as a delivery system for hydrophobic photodynamic therapy agents. J. Mater. Sci. Mater. Med. 2016, 27, 40. [Google Scholar] [CrossRef]
- Masood, F.; Chen, P.; Yasin, T.; Hameed, A. Novel Delivery System for Anticancer Drug Based on Short-Chain- Length Polyhydroxyalkanoate Nanoparticles. U.S. Patent US2015/0118293A1, 30 April 2015. [Google Scholar]
- Murueva, A.V.; Shershneva, A.M.; Abanina, K.V.; Prudnikova, S.V.; Shishatskaya, E.I. Development and characterization of ceftriaxone-loaded P3HB-based microparticles for drug delivery. Dry. Technol. 2019, 37, 1131–1142. [Google Scholar] [CrossRef]
- Rodríguez-Contreras, A.; Canal, C.; Calafell-Monfort, M.; Ginebra, M.-P.; Julio-Moran, G.; Marqués-Calvo, M.-S. Methods for the preparation of doxycycline-loaded phb micro- and nano-spheres. Eur. Polym. J. 2013, 49, 3501–3511. [Google Scholar] [CrossRef]
- Rodríguez-Contreras, A.; Marqués-Calvo, M.S.; Gil, F.J.; Manero, J.M. Modification of titanium surfaces by adding antibiotic-loaded PHB spheres and PEG for biomedical applications. J. Mater. Sci. Mater. Med. 2016, 27, 124. [Google Scholar] [CrossRef]
- Lee, Y.-F.; Sridewi, N.; Ramanathan, S.; Sudesh, K. The Influence of Electrospinning Parameters and Drug Loading on Polyhydroxyalkanoate (PHA) Nanofibers for Drug Delivery. Int. J. Biotechnol. Wellness Ind. 2015, 4, 103–113. [Google Scholar]
- Rodríguez-Contreras, A.; Rupérez, E.; Marqués-Calvo, M.S.; Manero, J.M. Chapter 7—PHAs as matrices for drug delivery. In Materials for Biomedical Engineering; Holban, A.-M., Grumezescu, A.M., Eds.; Elsevier: Amsterdam, The Netherlands, 2019; pp. 183–213. [Google Scholar]
- Rodríguez-Contreras, A.; García, Y.; Manero, J.M.; Rupérez, E. Antibacterial PHAs coating for titanium implants. Eur. Polym. J. 2017, 90, 66–78. [Google Scholar] [CrossRef] [Green Version]
- Rodríguez-Contreras, A.; Guillem-Marti, J.; Lopez, O.; Manero, J.M.; Ruperez, E. Antimicrobial PHAs coatings for solid and porous Tantalum implants. Colloids Surf. B Biointerfaces 2019, 182, 110317. [Google Scholar] [CrossRef]
- Timin, A.S.; Muslimov, A.R.; Zyuzin, M.V.; Peltek, O.O.; Karpov, T.E.; Sergeev, I.S.; Dotsenko, A.I.; Goncharenko, A.A.; Yolshin, N.D.; Sinelnik, A.; et al. Multifunctional Scaffolds with Improved Antimicrobial Properties and Osteogenicity Based on Piezoelectric Electrospun Fibers Decorated with Bioactive Composite Microcapsules. ACS Appl. Mater. Interfaces 2018, 10, 34849–34868. [Google Scholar] [CrossRef]


© 2019 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodriguez-Contreras, A. Recent Advances in the Use of Polyhydroyalkanoates in Biomedicine. Bioengineering 2019, 6, 82. https://doi.org/10.3390/bioengineering6030082
Rodriguez-Contreras A. Recent Advances in the Use of Polyhydroyalkanoates in Biomedicine. Bioengineering. 2019; 6(3):82. https://doi.org/10.3390/bioengineering6030082
Chicago/Turabian StyleRodriguez-Contreras, Alejandra. 2019. "Recent Advances in the Use of Polyhydroyalkanoates in Biomedicine" Bioengineering 6, no. 3: 82. https://doi.org/10.3390/bioengineering6030082
APA StyleRodriguez-Contreras, A. (2019). Recent Advances in the Use of Polyhydroyalkanoates in Biomedicine. Bioengineering, 6(3), 82. https://doi.org/10.3390/bioengineering6030082



