Nutraceuticals as Potential Targets for the Development of a Functional Beverage for Improving Sleep Quality
Abstract
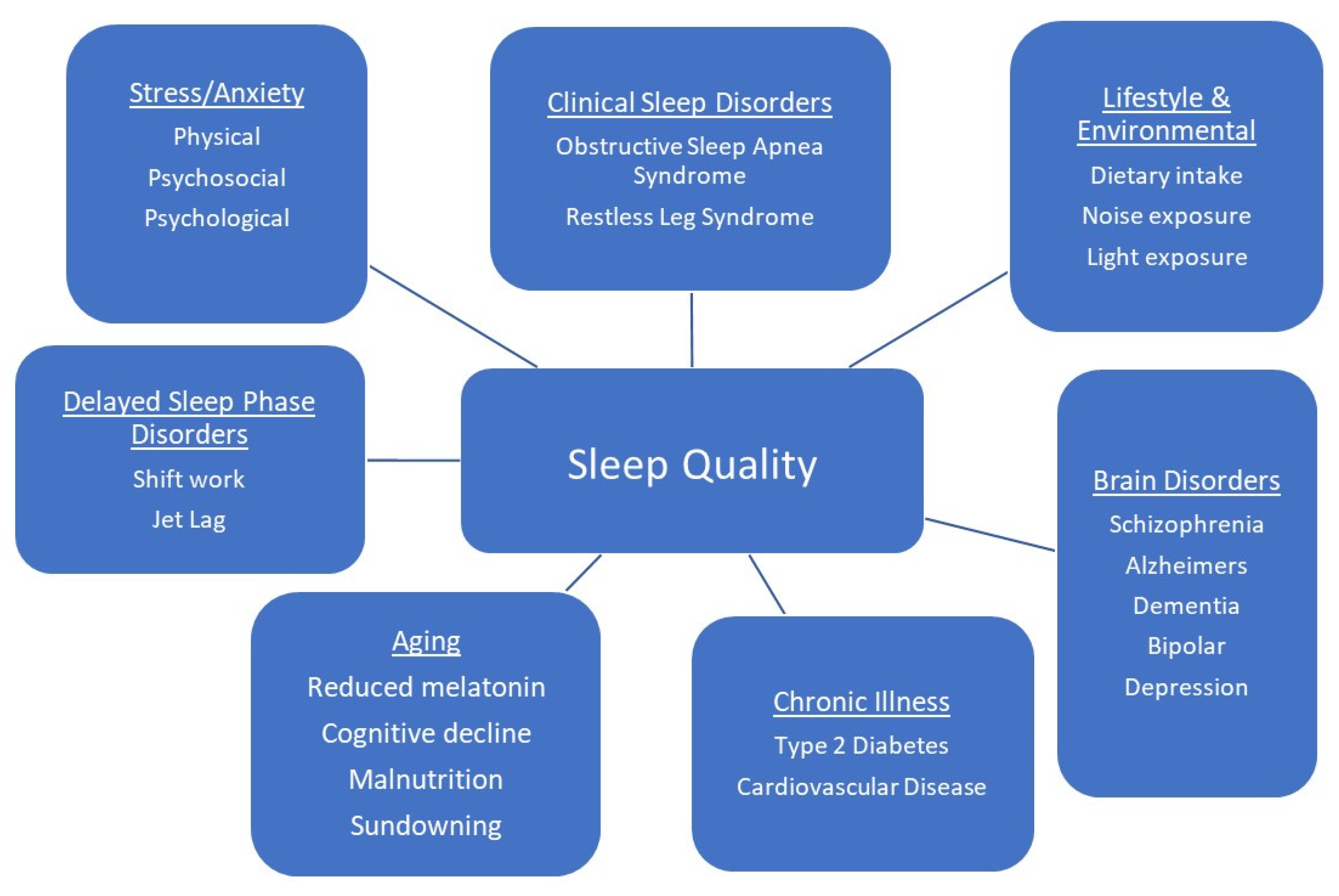
:1. Introduction
2. Active Compounds
2.1. L-Tryptophan
2.2. 5-Hydroxytryptophan
2.3. Melatonin
2.4. L-Theanine
2.5. L-Cysteine
2.6. Micronutrients
2.7. Nutraceutical Combinations
2.8. Traditional Sleep Promoting Beverages
3. Discussion
4. Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Özen, A.E.; Bibiloni, M.D.M.; Pons, A.; Tur, J.A. Fluid intake from beverages across age groups: A systematic review. J. Hum. Nutr. Diet. 2014, 28, 417–442. [Google Scholar] [CrossRef] [PubMed]
- Kaur, S.; Das, M. Functional foods: An overview. Food Sci. Biotechnol. 2011, 20, 861–875. [Google Scholar] [CrossRef]
- Siró, I.; Kápolna, E.; Kápolna, B.; Lugasi, A. Functional food. Product development, marketing and consumer acceptance—A review. Appetite 2008, 51, 456–467. [Google Scholar] [CrossRef] [PubMed]
- Corbo, M.R.; Bevilacqua, A.; Petruzzi, L.; Casanova, F.P.; Sinigaglia, M. Functional Beverages: The Emerging Side of Functional Foods. Compr. Rev. Food Sci. Food Saf. 2014, 13, 1192–1206. [Google Scholar] [CrossRef]
- Alkhatib, A.; Tsang, C.; Tiss, A.; Bahorun, T.; Arefanian, H.; Barake, R.; Khadir, A.; Tuomilehto, J. Functional Foods and Lifestyle Approaches for Diabetes Prevention and Management. Nutrients 2017, 9, 1310. [Google Scholar] [CrossRef] [Green Version]
- Roberfroid, M.B. Concepts and strategy of functional food science: The European perspective. Am. J. Clin. Nutr. 2000, 71, 1660S–1664S. [Google Scholar] [CrossRef] [Green Version]
- Cena, H.; Calder, P.C. Defining a Healthy Diet: Evidence for the Role of Contemporary Dietary Patterns in Health and Disease. Nutrients 2020, 12, 334. [Google Scholar] [CrossRef] [Green Version]
- Ventriglio, A.; Sancassiani, F.; Contu, M.P.; Latorre, M.; Di Slavatore, M.; Fornaro, M.; Bhugra, D. Mediterranean Diet and its Benefits on Health and Mental Health: A Literature Review. Clin. Pr. Epidemiology Ment. Heal. 2020, 16, 156–164. [Google Scholar] [CrossRef]
- Pan, S.-Y.; Litscher, G.; Gao, S.-H.; Zhou, S.-F.; Yu, Z.-L.; Chen, H.-Q.; Zhang, S.-F.; Tang, M.-K.; Sun, J.-N.; Ko, K.-M. Historical Perspective of Traditional Indigenous Medical Practices: The Current Renaissance and Conservation of Herbal Resources. Evid. Based Complement. Altern. Med. 2014, 2014, 1–20. [Google Scholar] [CrossRef]
- Zahiruddin, S.; Basist, P.; Parveen, A.; Parveen, R.; Khan, W.; Gaurav; Ahmad, S. Ashwagandha in brain disorders: A review of recent developments. J. Ethnopharmacol. 2020, 257, 112876. [Google Scholar] [CrossRef]
- Mishra, B.; John, E. A Systematic Review on Neuro-Psychopharmacological effects of Celastrus paniculatus (Malkangani) Oil. Res. J. Pharm. Technol. 2020, 13, 2452. [Google Scholar] [CrossRef]
- Purnima, B.M.; Kothiyal, P. A review article on phytochemistry and pharmacological profiles of Nardostachys jatamansi DC-medicinal herb. J. Pharmacogn. Phytochem. 2015, 3, 102–106. [Google Scholar]
- Dwivedi, S.; Chopra, D. Revisiting Terminalia arjuna—An Ancient Cardiovascular Drug. J. Tradit. Complement. Med. 2014, 4, 224–231. [Google Scholar] [CrossRef] [Green Version]
- Das, L.; Bhaumik, E.; Raychaudhuri, U.; Chakraborty, R. Role of nutraceuticals in human health. J. Food Sci. Technol. 2011, 49, 173–183. [Google Scholar] [CrossRef] [Green Version]
- Gil-Chávez, G.J.; Villa, J.A.; Ayala-Zavala, J.F.; Heredia, J.B.; Sepulveda, D.; Yahia, E.M.; González-Aguilar, G.A. Technologies for Extraction and Production of Bioactive Compounds to be Used as Nutraceuticals and Food Ingredients: An Overview. Compr. Rev. Food Sci. Food Saf. 2013, 12, 5–23. [Google Scholar] [CrossRef]
- Altemimi, A.; Watson, D.G.; Kinsel, M.; Lightfoot, D.A. Simultaneous extraction, optimization, and analysis of flavonoids and polyphenols from peach and pumpkin extracts using a TLC-densitometric method. Chem. Central J. 2015, 9, 1–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Altemimi, A.B.; Lakhssassi, N.; Baharlouei, A.; Watson, D.G.; Lightfoot, D.A. Phytochemicals: Extraction, Isolation, and Identification of Bioactive Compounds from Plant Extracts. Plants 2017, 6, 42. [Google Scholar] [CrossRef]
- Speer, H.; D’Cunha, N.M.; Davies, M.J.; McKune, A.J.; Naumovski, N. The Physiological Effects of Amino Acids Arginine and Citrulline: Is There a Basis for Development of a Beverage to Promote Endurance Performance? A Narrative Review of Orally Administered Supplements. Beverages 2020, 6, 11. [Google Scholar] [CrossRef] [Green Version]
- Sun-Waterhouse, D. The development of fruit-based functional foods targeting the health and wellness market: A review. Int. J. Food Sci. Technol. 2011, 46, 899–920. [Google Scholar] [CrossRef]
- Wootton-Beard, P.C.; Ryan, L. Improving public health?: The role of antioxidant-rich fruit and vegetable beverages. Food Res. Int. 2011, 44, 3135–3148. [Google Scholar] [CrossRef]
- Businesswire. Global Relaxation Drinks Market (2019 to 2027)—CAGR of 14.06% Expected During the Forecast Period—ResearchAndMarkets.com. 2020. Available online: https://www.businesswire.com/news/home/20200317005330/en/Global-Relaxation-Drinks-Market-2019-to-2027---CAGR-of-14.06-Expected-During-the-Forecast-Period---ResearchAndMarkets.com (accessed on 17 March 2021).
- Assefa, S.Z.; Diaz-Abad, M.; Wickwire, E.M.; Scharf, S.M. The Functions of Sleep. AIMS Neurosci. 2015, 2, 155–171. [Google Scholar] [CrossRef]
- Donlea, J.M. Roles for sleep in memory: Insights from the fly. Curr. Opin. Neurobiol. 2019, 54, 120–126. [Google Scholar] [CrossRef]
- Holst, S.C.; Landolt, H.-P. Sleep-Wake Neurochemistry. Sleep Med. Clin. 2018, 13, 137–146. [Google Scholar] [CrossRef] [Green Version]
- Mechan, A.O.; Fowler, A.; Seifert, N.; Rieger, H.; Wöhrle, T.; Etheve, S.; Wyss, A.; Schüler, G.; Colletto, B.; Kilpert, C.; et al. Monoamine reuptake inhibition and mood-enhancing potential of a specified oregano extract. Br. J. Nutr. 2010, 105, 1150–1163. [Google Scholar] [CrossRef] [Green Version]
- Chaput, J.-P.; Dutil, C.; Sampasa-Kanyinga, H. Sleeping hours: What is the ideal number and how does age impact this? Nat. Sci. Sleep 2018, 10, 421–430. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lyon, L. Is an epidemic of sleeplessness increasing the incidence of Alzheimer’s disease? Brain 2019, 142, e30. [Google Scholar] [CrossRef]
- Longordo, F.; Kopp, C.; Lüthi, A. Consequences of sleep deprivation on neurotransmitter receptor expression and function. Eur. J. Neurosci. 2009, 29, 1810–1819. [Google Scholar] [CrossRef]
- Guarnieri, B.M.; Sorbi, S. Sleep and Cognitive Decline: A Strong Bidirectional Relationship. It Is Time for Specific Recommendations on Routine Assessment and the Management of Sleep Disorders in Patients with Mild Cognitive Impairment and Dementia. Eur. Neurol. 2015, 74, 43–48. [Google Scholar] [CrossRef]
- Xi, B.; He, D.; Zhang, M.; Xue, J.; Zhou, D. Short sleep duration predicts risk of metabolic syndrome: A systematic review and meta-analysis. Sleep Med. Rev. 2014, 18, 293–297. [Google Scholar] [CrossRef]
- Firth, J.; Solmi, M.; Wootton, R.E.; Vancampfort, D.; Schuch, F.B.; Hoare, E.; Gilbody, S.; Torous, J.; Teasdale, S.B.; Jackson, S.E.; et al. A meta-review of “lifestyle psychiatry”: The role of exercise, smoking, diet and sleep in the prevention and treatment of mental disorders. World Psychiatry 2020, 19, 360–380. [Google Scholar] [CrossRef]
- Cappuccio, F.P.; D’Elia, L.; Strazzullo, P.; Miller, M.A. Quantity and Quality of Sleep and Incidence of Type 2 Diabetes: A systematic review and meta-analysis. Diabetes Care 2009, 33, 414–420. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cappuccio, F.P.; Cooper, D.; D’Elia, L.; Strazzullo, P.; Miller, M.A. Sleep duration predicts cardiovascular outcomes: A systematic review and meta-analysis of prospective studies. Eur. Hear. J. 2011, 32, 1484–1492. [Google Scholar] [CrossRef] [Green Version]
- Ibarra-Coronado, E.G.; Pantaleón-Martínez, A.M.; Velazquéz-Moctezuma, J.; Prospéro-García, O.; Méndez-Díaz, M.; Pérez-Tapia, M.; Pavón, L.; Morales-Montor, J. The Bidirectional Relationship between Sleep and Immunity against Infections. J. Immunol. Res. 2015, 2015, 1–14. [Google Scholar] [CrossRef] [Green Version]
- St-Onge, M.-P.; Mikic, A.; Pietrolungo, C.E. Effects of Diet on Sleep Quality. Adv. Nutr. 2016, 7, 938–949. [Google Scholar] [CrossRef]
- Ikonte, C.J.; Mun, J.G.; Reider, C.A.; Grant, R.W.; Mitmesser, S.H. Mun Micronutrient Inadequacy in Short Sleep: Analysis of the NHANES 2005. Nutrients 2019, 11, 2335. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Campanini, M.M.Z.; Guallar-Castillón, P.; Rodríguez-Artalejo, F.; Lopez-Garcia, E. Mediterranean Diet and Changes in Sleep Duration and Indicators of Sleep Quality in Older Adults. Sleep 2016, 40. [Google Scholar] [CrossRef]
- Zuraikat, F.M.; Makarem, N.; St-Onge, M.-P.; Xi, H.; Akkapeddi, A.; Aggarwal, B. A Mediterranean Dietary Pattern Predicts Better Sleep Quality in US Women from the American Heart Association Go Red for Women Strategically Focused Research Network. Nutrients 2020, 12, 2830. [Google Scholar] [CrossRef]
- Peuhkuri, K.; Sihvola, N.; Korpela, R. Diet promotes sleep duration and quality. Nutr. Res. 2012, 32, 309–319. [Google Scholar] [CrossRef]
- Markus, C.R.; Jonkman, L.M.; Lammers, J.H.C.M.; Deutz, N.E.P.; Messer, M.H.; Rigtering, N. Evening intake of α-lactalbumin increases plasma tryptophan availability and improves morning alertness and brain measures of attention. Am. J. Clin. Nutr. 2005, 81, 1026–1033. [Google Scholar] [CrossRef]
- Ong, J.N.; Hackett, D.A.; Chow, C.-M. Sleep quality and duration following evening intake of alpha-lactalbumin: A pilot study. Biol. Rhythm. Res. 2017, 48, 507–517. [Google Scholar] [CrossRef]
- Cubero, J.; Narciso, D.; Terrón, P.; Rial, R.; Esteban, S.; Rivero, M.; Parvez, H.; Rodríguez, A.B.; Barriga, C. Chrononutrition applied to formula milks to consolidate infants’ sleep/wake cycle. Neuro Endocrinol. Lett. 2007, 28, 360–366. [Google Scholar] [PubMed]
- Bravo, R.; Matito, S.; Cubero, J.; Paredes, S.D.; Franco, L.; Rivero, M.; Rodríguez, A.B.; Barriga, C. Tryptophan-enriched cereal intake improves nocturnal sleep, melatonin, serotonin, and total antioxidant capacity levels and mood in elderly humans. AGE 2012, 35, 1277–1285. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bruni, O.; Ferri, R.; Miano, S.; Verrillo, E. L-5-Hydroxytryptophan treatment of sleep terrors in children. Eur. J. Nucl. Med. Mol. Imaging 2004, 163, 402–407. [Google Scholar] [CrossRef]
- Scheer, F.A.; Morris, C.J.; Garcia, J.I.; Smales, C.; Kelly, E.E.; Marks, J.; Malhotra, A.; Shea, S.A. Repeated Melatonin Supplementation Improves Sleep in Hypertensive Patients Treated with Beta-Blockers: A Randomized Controlled Trial. Sleep 2012, 35, 1395–1402. [Google Scholar] [CrossRef]
- Grima, N.A.; Rajaratnam, S.M.W.; Mansfield, D.; Sletten, T.L.; Spitz, G.; Ponsford, J.L. Efficacy of melatonin for sleep disturbance following traumatic brain injury: A randomised controlled trial. BMC Med. 2018, 16, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Xu, H.; Zhang, C.; Qian, Y.; Zou, J.; Li, X.; Liu, Y.; Zhu, H.; Meng, L.; Liu, S.; Zhang, W.; et al. Efficacy of melatonin for sleep disturbance in middle-aged primary insomnia: A double-blind, randomised clinical trial. Sleep Med. 2020, 76, 113–119. [Google Scholar] [CrossRef]
- Sadasivam, K.; Patial, K.; Vijayan, V.K.; Ravi, K. Anti-oxidant treatment in obstructive sleep apnoea syndrome. Indian J. chest Dis. Allied Sci. 2011, 53, 153–162. [Google Scholar]
- Rao, T.P.; Ozeki, M.; Juneja, L.R. In Search of a Safe Natural Sleep Aid. J. Am. Coll. Nutr. 2015, 34, 436–447. [Google Scholar] [CrossRef]
- Lyon, M.R.; Kapoor, M.P.; Juneja, L.R. The effects of L-theanine (Suntheanine®) on objective sleep quality in boys with attention deficit hyperactivity disorder (ADHD): A randomized, double-blind, placebo-controlled clinical trial. Altern. Med. Rev. J. Clin. Ther. 2011, 16, 348. [Google Scholar]
- Sarris, J.; Byrne, G.J.; Cribb, L.; Oliver, G.; Murphy, J.; Macdonald, P.; Nazareth, S.; Karamacoska, D.; Galea, S.; Short, A.; et al. L-theanine in the adjunctive treatment of generalized anxiety disorder: A double-blind, randomised, placebo-controlled trial. J. Psychiatr. Res. 2019, 110, 31–37. [Google Scholar] [CrossRef] [Green Version]
- Hidese, S.; Ogawa, S.; Ota, M.; Ishida, I.; Yasukawa, Z.; Ozeki, M.; Kunugi, H. Effects of L-Theanine Administration on Stress-Related Symptoms and Cognitive Functions in Healthy Adults: A Randomized Controlled Trial. Nutrients 2019, 11, 2362. [Google Scholar] [CrossRef] [Green Version]
- Mayer, G.; Kröger, M.; Meier-Ewert, K. Effects of Vitamin B12 on Performance and Circadian Rhythm in Normal Subjects. Neuropsychopharmacology 1996, 15, 456–464. [Google Scholar] [CrossRef] [Green Version]
- Luboshitzky, R.; Ophir, U.; Nave, R.; Epstein, R.; Shen-Orr, Z.; Herer, P. The effect of pyridoxine administration on melatonin secretion in normal men. Neuro Endocrinol. Lett. 2002, 23, 213–217. [Google Scholar]
- Ebben, M.; Lequerica, A.; Spielman, A. Effects of Pyridoxine on Dreaming: A Preliminary Study. Percept. Mot. Skills 2002, 94, 135–140. [Google Scholar] [CrossRef]
- Aspy, D.J.; Madden, N.A.; Delfabbro, P. Effects of Vitamin B6 (Pyridoxine) and a B Complex Preparation on Dreaming and Sleep. Percept. Mot. Ski. 2018, 125, 451–462. [Google Scholar] [CrossRef]
- Ghaderi, A.; Banafshe, H.R.; Motmaen, M.; Rasouli-Azad, M.; Bahmani, F.; Asemi, Z. Clinical trial of the effects of vitamin D supplementation on psychological symptoms and metabolic profiles in maintenance methadone treatment patients. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2017, 79, 84–89. [Google Scholar] [CrossRef] [PubMed]
- Mason, C.; Tapsoba, J.D.D.; Duggan, C.; Wang, C.-Y.; Korde, L.; McTiernan, A. Repletion of vitamin D associated with deterioration of sleep quality among postmenopausal women. Prev. Med. 2016, 93, 166–170. [Google Scholar] [CrossRef] [Green Version]
- Dadashpour, S.; Hajmiri, M.S.; Roshani, D. Effect of intravenous vitamin C supplementation on the quality of sleep, itching and restless leg syndrome in patients undergoing hemodialysis; A double-blind randomized clinical trial. J. Nephropharmacol. 2018, 7, 131–136. [Google Scholar] [CrossRef]
- Yeom, C.H.; Jung, G.C.; Song, K.J. Changes of Terminal Cancer Patients’ Health-related Quality of Life after High Dose Vitamin C Administration. J. Korean Med. Sci. 2007, 22, 7–11. [Google Scholar] [CrossRef] [Green Version]
- Murck, H.; Held, K.; Antonijevic, I.; Künzel, H.; Golly, I.; Steiger, A. Oral Mg2+-supplementation reverses age related sleep-endocrine changes in humans. Eur. Neuropsychopharmacol. 2000, 10, 373. [Google Scholar] [CrossRef]
- Abbasi, B.; Kimiagar, M.; Sadeghniiat, K.; Shirazi, M.M.; Hedayati, M.; Rashidkhani, B. The effect of magnesium supplementation on primary insomnia in elderly: A double-blind placebo-controlled clinical trial. J. Res. Med. Sci. 2012, 17, 1161–1169. [Google Scholar]
- Hornyak, M.; Haas, P.; Veit, J.; Gann, H.; Riemann, D. Magnesium Treatment of Primary Alcohol-Dependent Patients During Subacute Withdrawal: An Open Pilot Study with Polysomnography. Alcohol. Clin. Exp. Res. 2004, 28, 1702–1709. [Google Scholar] [CrossRef] [Green Version]
- Saito, H.; Cherasse, Y.; Suzuki, R.; Mitarai, M.; Ueda, F.; Urade, Y. Zinc-rich oysters as well as zinc-yeast- and astaxanthin-enriched food improved sleep efficiency and sleep onset in a randomized controlled trial of healthy individuals. Mol. Nutr. Food Res. 2017, 61, 1600882. [Google Scholar] [CrossRef] [PubMed]
- Baradari, A.G.; Alipour, A.; Mahdavi, A.; Sharifi, H.; Nouraei, S.M.; Zeydi, A.E. The Effect of Zinc Supplementation on Sleep Quality of ICU Nurses: A Double Blinded Randomized Controlled Trial. Work Health Saf. 2018, 66, 191–200. [Google Scholar] [CrossRef] [PubMed]
- Friedman, M. Analysis, Nutrition, and Health Benefits of Tryptophan. Int. J. Tryptophan Res. 2018, 11. [Google Scholar] [CrossRef] [Green Version]
- Marx, W.; Lane, M.; Hockey, M.; Aslam, H.; Berk, M.; Walder, K.; Borsini, A.; Firth, J.; Pariante, C.M.; Berding, K.; et al. Diet and depression: Exploring the biological mechanisms of action. Mol. Psychiatry 2021, 26, 134–150. [Google Scholar] [CrossRef] [PubMed]
- van der Leek, A.P.; Yanishevsky, Y.; Kozyrskyj, A.L. The Kynurenine Pathway as a Novel Link between Allergy and the Gut Microbiome. Front. Immunol. 2017, 8, 1374. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nayak, B.N.P.; Singh, R.B.M.; Buttar, H.S.P. Role of Tryptophan in Health and Disease: Systematic Review of the Anti-Oxidant, Anti-Inflammation, and Nutritional Aspects of Tryptophan and Its Metabolites. World Heart J. 2019, 11, 161–178. [Google Scholar]
- Doherty, R.; Madigan, S.; Warrington, G.; Ellis, J. Sleep and Nutrition Interactions: Implications for Athletes. Nutrients 2019, 11, 822. [Google Scholar] [CrossRef] [Green Version]
- Sandyk, R. L-Tryptophan in Neuropsychiatry Disorders: A Review. Int. J. Neurosci. 1992, 67, 127–144. [Google Scholar] [CrossRef]
- Silber, B.; Schmitt, J. Effects of tryptophan loading on human cognition, mood, and sleep. Neurosci. Biobehav. Rev. 2010, 34, 387–407. [Google Scholar] [CrossRef]
- Favennec, M.; Hennart, B.; Caiazzo, R.; Leloire, A.; Yengo, L.; Verbanck, M.; Arredouani, A.; Marre, M.; Pigeyre, M.; Bessede, A.; et al. The kynurenine pathway is activated in human obesity and shifted toward kynurenine monooxygenase activation. Obesity 2015, 23, 2066–2074. [Google Scholar] [CrossRef]
- Braidy, N.; Berg, J.; Clement, J.; Khorshidi, F.; Poljak, A.; Jayasena, T.; Grant, R.; Sachdev, P. Role of Nicotinamide Adenine Dinucleotide and Related Precursors as Therapeutic Targets for Age-Related Degenerative Diseases: Rationale, Biochemistry, Pharmacokinetics, and Outcomes. Antioxid. Redox Signal. 2019, 30, 251–294. [Google Scholar] [CrossRef]
- Lovelace, M.; Varney, B.; Sundaram, G.; Franco, N.F.; Ng, M.L.; Pai, S.; Lim, E.; Guillemin, G.J.; Brew, B.J. Current Evidence for a Role of the Kynurenine Pathway of Tryptophan Metabolism in Multiple Sclerosis. Front. Immunol. 2016, 7, 246. [Google Scholar] [CrossRef] [Green Version]
- Wang, Q.; Liu, D.; Song, P.; Zou, M.H. Tryptophan-kynurenine pathway is dysregulated in inflammation, and immune activation. Front. Biosci. 2015, 20, 1116–1143. [Google Scholar]
- Badawy, A.A.-B. Kynurenine Pathway of Tryptophan Metabolism: Regulatory and Functional Aspects. Int. J. Tryptophan Res. 2017, 10, 1178646917691938. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Le Floc’H, N.; Otten, W.; Merlot, E. Tryptophan metabolism, from nutrition to potential therapeutic applications. Amino Acids 2011, 41, 1195–1205. [Google Scholar] [CrossRef] [PubMed]
- Schwarcz, R.; Stone, T. The kynurenine pathway and the brain: Challenges, controversies and promises. Neuropharmacology 2017, 112, 237–247. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Castro-Portuguez, R.; Sutphin, G.L. Kynurenine pathway, NAD+ synthesis, and mitochondrial function: Targeting tryptophan metabolism to promote longevity and healthspan. Exp. Gerontol. 2020, 132, 110841. [Google Scholar] [CrossRef]
- Höglund, E.; Øverli, Ø.; Winberg, S. Tryptophan Metabolic Pathways and Brain Serotonergic Activity: A Comparative Review. Front. Endocrinol. 2019, 10, 158. [Google Scholar] [CrossRef]
- Chen, Y.; Guillemin, G.J. Kynurenine Pathway Metabolites in Humans: Disease and Healthy States. Int. J. Tryptophan Res. 2009, 2, 1–19. [Google Scholar] [CrossRef] [Green Version]
- Stone, T.W.; Darlington, L.G. The kynurenine pathway as a therapeutic target in cognitive and neurodegenerative disorders. Br. J. Pharmacol. 2013, 169, 1211–1227. [Google Scholar] [CrossRef]
- Adams, S.; Braidy, N.; Bessesde, A.; Brew, B.; Grant, R.; Teo, C.; Guillemin, G.J. The Kynurenine Pathway in Brain Tumor Pathogenesis. Cancer Res. 2012, 72, 5649–5657. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sutanto, C.N.; Loh, W.W.; Kim, J.E. The impact of tryptophan supplementation on sleep quality: A systematic review, meta-analysis, and meta-regression. Nutr. Rev. 2021. [Google Scholar] [CrossRef]
- Richard, D.M.; Dawes, M.A.; Mathias, C.W.; Acheson, A.; Hill-Kapturczak, N.; Dougherty, D.M. L-Tryptophan: Basic Metabolic Functions, Behavioral Research and Therapeutic Indications. Int. J. Tryptophan Res. 2009, 2, 45–60. [Google Scholar] [CrossRef] [Green Version]
- Sergi, D.; Naumovski, N.N.; Heilbronn, L.H.K.; Abeywardena, M.; O’Callaghan, N.; Lionetti, L.; Luscombe-Marsh, N.L.-M. Mitochondrial (Dys)function and Insulin Resistance: From Pathophysiological Molecular Mechanisms to the Impact of Diet. Front. Physiol. 2019, 10, 532. [Google Scholar] [CrossRef] [PubMed]
- Afaghi, A.; O’Connor, H.; Chow, C.M. High-glycemic-index carbohydrate meals shorten sleep onset. Am. J. Clin. Nutr. 2007, 85, 426–430. [Google Scholar] [CrossRef]
- Fernstrom, J.D. A Perspective on the Safety of Supplemental Tryptophan Based on Its Metabolic Fates. J. Nutr. 2016, 146, 2601S–2608S. [Google Scholar] [CrossRef] [Green Version]
- Turner, E.H.; Loftis, J.; Blackwell, A.D. Serotonin a la carte: Supplementation with the serotonin precursor 5-hydroxytryptophan. Pharmacol. Ther. 2006, 109, 325–338. [Google Scholar] [CrossRef] [Green Version]
- Gendle, M.H.; Golding, A.C. Oral administration of 5-hydroxytryptophan (5-HTP) impairs decision making under ambiguity but not under risk: Evidence from the Iowa Gambling Task. Hum. Psychopharmacol. Clin. Exp. 2010, 25, 491–499. [Google Scholar] [CrossRef]
- Maffei, M.E. 5-Hydroxytryptophan (5-HTP): Natural Occurrence, Analysis, Biosynthesis, Biotechnology, Physiology and Toxicology. Int. J. Mol. Sci. 2020, 22, 181. [Google Scholar] [CrossRef]
- Esposito, D.; Belli, A.; Ferri, R.; Bruni, O. Sleeping without Prescription: Management of Sleep Disorders in Children with Autism with Non-Pharmacological Interventions and Over-the-Counter Treatments. Brain Sci. 2020, 10, 441. [Google Scholar] [CrossRef] [PubMed]
- Jacobsen, J.P.; Krystal, A.D.; Krishnan, K.R.R.; Caron, M.G. Adjunctive 5-Hydroxytryptophan Slow-Release for Treatment-Resistant Depression: Clinical and Preclinical Rationale. Trends Pharmacol. Sci. 2016, 37, 933–944. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lewandowska, K.; Małkiewicz, M.A.; Siemiński, M.; Cubała, W.J.; Winklewski, P.J.; Mędrzycka-Dąbrowska, W.A. The role of melatonin and melatonin receptor agonist in the prevention of sleep disturbances and delirium in intensive care unit–A clinical review. Sleep Med. 2020, 69, 127–134. [Google Scholar] [CrossRef]
- Xie, Z.; Chen, F.; Li, W.A.; Geng, X.; Li, C.; Meng, X.; Feng, Y.; Liu, W.; Yu, F. A review of sleep disorders and melatonin. Neurol. Res. 2017, 39, 559–565. [Google Scholar] [CrossRef]
- McGrane, I.R.; Leung, J.G.; Louis, E.K.S.; Boeve, B.F. Melatonin therapy for REM sleep behavior disorder: A critical review of evidence. Sleep Med. 2015, 16, 19–26. [Google Scholar] [CrossRef] [Green Version]
- Williams, J.; Kellett, J.; Roach, P.D.; McKune, A.; Mellor, D.; Thomas, J.; Naumovski, N. l-Theanine as a Functional Food Additive: Its Role in Disease Prevention and Health Promotion. Beverages 2016, 2, 13. [Google Scholar] [CrossRef] [Green Version]
- Naumovski, N.; Foscolou, A.; D’Cunha, N.M.; Tyrovolas, S.; Chrysohoou, C.; Sidossis, L.S.; Rallidis, L.; Matalas, A.-L.; Polychronopoulos, E.; Pitsavos, C.; et al. The Association between Green and Black Tea Consumption on Successful Aging: A Combined Analysis of the ATTICA and MEDiterranean ISlands (MEDIS) Epidemiological Studies. Molecules 2019, 24, 1862. [Google Scholar] [CrossRef] [Green Version]
- Türközü, D.; Şanlier, N. L-theanine, unique amino acid of tea, and its metabolism, health effects, and safety. Crit. Rev. Food Sci. Nutr. 2017, 57, 1681–1687. [Google Scholar] [CrossRef]
- Deb, S.; Dutta, A.; Phukan, B.C.; Manivasagam, T.; Thenmozhi, A.J.; Bhattacharya, P.; Paul, R.; Borah, A. Neuroprotective attributes of L-theanine, a bioactive amino acid of tea, and its potential role in Parkinson’s disease therapeutics. Neurochem. Int. 2019, 129, 104478. [Google Scholar] [CrossRef]
- Kakuda, T. Neuroprotective effects of theanine and its preventive effects on cognitive dysfunction. Pharmacol. Res. 2011, 64, 162–168. [Google Scholar] [CrossRef]
- Kobayashi, K.; Nagato, Y.; Aoi, N.; Juneja, L.R.; Kim, M.; Yamamoto, T.; Sugimoto, S. Effects of L-Theanine on the Release of.ALPHA.-Brain Waves in Human Volunteers. J. Agric. Chem. Soc. Jpn. 1998, 72, 153–157. [Google Scholar] [CrossRef] [Green Version]
- Song, C.H.; Jung, J.H.; Oh, J.S.; Kim, K.S. Effects of theanine on the release of brain alpha wave in adult males. Korean J. Nutr. 2003, 36, 918–923. [Google Scholar]
- Rogers, P.J.; Smith, J.E.; Heatherley, S.V.; Pleydell-Pearce, C.W. Time for tea: Mood, blood pressure and cognitive performance effects of caffeine and theanine administered alone and together. Psychopharmacology 2007, 195, 569–577. [Google Scholar] [CrossRef] [PubMed]
- Yoto, A.; Motoki, M.; Murao, S.; Yokogoshi, H. Effects of L-theanine or caffeine intake on changes in blood pressure under physical and psychological stresses. J. Physiol. Anthr. 2012, 31, 28. [Google Scholar] [CrossRef] [Green Version]
- Yin, J.; Ren, W.; Yang, G.; Duan, J.; Huang, X.; Fang, R.; Li, C.; Li, T.; Yin, Y.; Hou, Y.; et al. L-Cysteine metabolism and its nutritional implications. Mol. Nutr. Food Res. 2016, 60, 134–146. [Google Scholar] [CrossRef]
- Armstrong, J.S.; Steinauer, K.K.; Hornung, B.; Irish, J.M.; Lecane, P.; Birrell, G.W.; Peehl, D.M.; Knox, S.J. Role of glutathione depletion and reactive oxygen species generation in apoptotic signaling in a human B lymphoma cell line. Cell Death Differ. 2002, 9, 252–263. [Google Scholar] [CrossRef] [Green Version]
- Lushchak, V.I. Glutathione Homeostasis and Functions: Potential Targets for Medical Interventions. J. Amino Acids 2012, 2012, 1–26. [Google Scholar] [CrossRef] [Green Version]
- Pizzino, G.; Irrera, N.; Cucinotta, M.; Pallio, G.; Mannino, F.; Arcoraci, V.; Squadrito, F.; Altavilla, D.; Bitto, A. Oxidative Stress: Harms and Benefits for Human Health. Oxidative Med. Cell. Longev. 2017. [Google Scholar] [CrossRef]
- Trivedi, M.S.; Holger, D.; Bui, A.T.; Craddock, T.; Tartar, J.L. Short-term sleep deprivation leads to decreased systemic redox metabolites and altered epigenetic status. PLoS ONE 2017, 12, e0181978. [Google Scholar] [CrossRef]
- Slattery, J.; Kumar, N.; Delhey, L.; Berk, M.; Dean, O.; Spielholz, C.; Frye, R. Clinical trials of N-acetylcysteine in psychiatry and neurology: A systematic review. Neurosci. Biobehav. Rev. 2015, 55, 294–321. [Google Scholar]
- Mokhtari, V.; Afsharian, P.; Shahhoseini, M.; Kalantar, S.M.; Moini, A. A Review on Various Uses of N-Acetyl Cysteine. Cell. J. 2016, 19, 11–17. [Google Scholar]
- Shahripour, R.B.; Harrigan, M.R.; Alexandrov, A.V. N-acetylcysteine (NAC) in neurological disorders: Mechanisms of action and therapeutic opportunities. Brain Behav. 2014, 4, 108–122. [Google Scholar] [CrossRef]
- Dean, O.; Giorlando, F.; Berk, M. N-acetylcysteine in psychiatry: Current therapeutic evidence and potential mechanisms of action. J. Psychiatry Neurosci. 2011, 36, 78–86. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lavie, L. Oxidative stress in obstructive sleep apnea and intermittent hypoxia—Revisited—The bad ugly and good: Implications to the heart and brain. Sleep Med. Rev. 2015, 20, 27–45. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, D.O. B Vitamins and the Brain: Mechanisms, Dose and Efficacy—A Review. Nutrients 2016, 8, 68. [Google Scholar] [CrossRef] [Green Version]
- Peuhkuri, K.; Sihvola, N.; Korpela, R. Dietary factors and fluctuating levels of melatonin. Food Nutr. Res. 2012, 56, 17252. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hashimoto, S.; Kohsaka, M.; Morita, N.; Fukuda, N.; Honma, S.; Honma, K.-I. Vitamin B12 enhances the phase-response of circadian melatonin rhythm to a single bright light exposure in humans. Neurosci. Lett. 1996, 220, 129–132. [Google Scholar] [CrossRef]
- Viljoen, M.; Swanepoel, A.; Bipath, P. Antidepressants may lead to a decrease in niacin and NAD in patients with poor dietary intake. Med. Hypotheses 2015, 84, 178–182. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van Hunsel, F.; van de Koppel, S.; van Puijenbroek, E.; Kant, A. Vitamin B6 in Health Supplements and Neuropathy: Case Series Assessment of Spontaneously Reported Cases: An International Journal of Medical Toxicology and Drug Experience. Drug Saf. 2018, 41, 859–869. [Google Scholar] [CrossRef]
- McCarty, D.E.; Chesson, A.L.; Jain, S.K.; Marino, A.A. The link between vitamin D metabolism and sleep medicine. Sleep Med. Rev. 2014, 18, 311–319. [Google Scholar] [CrossRef]
- Wilson, L.R.; Tripkovic, L.; Hart, K.H.; Lanham-New, S.A. Vitamin D deficiency as a public health issue: Using vitamin D2or vitamin D3in future fortification strategies. Proc. Nutr. Soc. 2017, 76, 392–399. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Massa, J.; Stone, K.L.; Wei, E.K.; Harrison, S.L.; Barrett-Connor, E.; Lane, N.E.; Paudel, M.; Redline, S.; Ancoli-Israel, S.; Orwoll, E.; et al. Vitamin D and Actigraphic Sleep Outcomes in Older Community-Dwelling Men: The MrOS Sleep Study. Sleep 2015, 38, 251–257. [Google Scholar] [CrossRef] [Green Version]
- Jung, Y.S.; Chae, C.H.; Kim, Y.O.; Son, J.S.; Kim, C.W.; Park, H.O.; Lee, J.H.; Shin, Y.H.; Kwak, H.S. The relationship between serum vitamin D levels and sleep quality in fixed day indoor field workers in the electronics manufacturing industry in Korea. Ann. Occup. Environ. Med. 2017, 29, 25. [Google Scholar] [CrossRef] [PubMed]
- Han, B.; Zhu, F.-X.; Shi, C.; Wu, H.-L.; Gu, X.-H. Association between Serum Vitamin D Levels and Sleep Disturbance in Hemodialysis Patients. Nutrients 2017, 9, 139. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patrick, R.P.; Ames, B.N. Vitamin D hormone regulates serotonin synthesis. Part 1: Relevance for autism. FASEB J. 2014, 28, 2398–2413. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Majid, M.S.; Ahmad, H.S.; Bizhan, H.; Hosein, H.Z.M.; Mohammad, A. The effect of vitamin D supplement on the score and quality of sleep in 20–50 year-old people with sleep disorders compared with control group. Nutr. Neurosci. 2018, 21, 511–519. [Google Scholar] [CrossRef] [PubMed]
- Pilz, S.; März, W.; Cashman, K.D.; Kiely, M.E.; Whiting, S.J.; Holick, M.F.; Grant, W.B.; Pludowski, P.; Hiligsmann, M.; Trummer, C.; et al. Rationale and Plan for Vitamin D Food Fortification: A Review and Guidance Paper. Front. Endocrinol. 2018, 9, 373. [Google Scholar] [CrossRef]
- Padayatty, S.J.; Katz, A.; Wang, Y.; Eck, P.; Kwon, O.; Lee, J.-H.; Chen, S.; Corpe, C.; Dutta, A.; Dutta, S.K.; et al. Vitamin C as an Antioxidant: Evaluation of Its Role in Disease Prevention. J. Am. Coll. Nutr. 2003, 22, 18–35. [Google Scholar] [CrossRef]
- Otocka-Kmiecik, A.; Krol, A. The Role of Vitamin C in Two Distinct Physiological States: Physical Activity and Sleep. Nutrients 2020, 12, 3908. [Google Scholar] [CrossRef]
- Vollbracht, C.; Kraft, K. Feasibility of Vitamin C in the Treatment of Post Viral Fatigue with Focus on Long COVID, Based on a Systematic Review of IV Vitamin C on Fatigue. Nutrients 2021, 13, 1154. [Google Scholar] [CrossRef]
- Pacier, C.; Martirosyan, D.M. Vitamin C: Optimal dosages, supplementation and use in disease prevention. Funct. Foods Heal. Dis. 2015, 5, 89–107. [Google Scholar] [CrossRef]
- Wilson, M.K.; Baguley, B.C.; Wall, C.; Jameson, M.B.; Findlay, M.P. Review of high-dose intravenous vitamin C as an anticancer agent. Asia Pacific J. Clin. Oncol. 2014, 10, 22–37. [Google Scholar] [CrossRef] [PubMed]
- Fawcett, W.J.; Haxby, E.J.; Male, D.A. Magnesium: Physiology and pharmacology. Br. J. Anaesth. 1999, 83, 302–320. [Google Scholar] [CrossRef]
- Holz, J.; Piosczyk, H.; Feige, B.; Spiegelhalder, K.; Baglioni, C.; Riemann, D.; Nissen, C. EEG sigma and slow-wave activity during NREM sleep correlate with overnight declarative and procedural memory consolidation. J. Sleep Res. 2012, 21, 612–619. [Google Scholar] [CrossRef]
- Gröber, U.; Schmidt, J.; Kisters, K. Magnesium in Prevention and Therapy. Nutrients 2015, 7, 8199–8226. [Google Scholar] [CrossRef] [Green Version]
- Cherasse, Y.; Urade, Y. Dietary Zinc Acts as a Sleep Modulator. Int. J. Mol. Sci. 2017, 18, 2334. [Google Scholar] [CrossRef] [Green Version]
- Derwand, R.; Scholz, M. Does zinc supplementation enhance the clinical efficacy of chloroquine/hydroxychloroquine to win today’s battle against COVID-19? Med. Hypotheses 2020, 142, 109815. [Google Scholar] [CrossRef]
- Rondanelli, M.; Opizzi, A.; Monteferrario, F.; Antoniello, N.; Manni, R.; Klersy, C. The Effect of Melatonin, Magnesium, and Zinc on Primary Insomnia in Long-Term Care Facility Residents in Italy: A Double-Blind, Placebo-Controlled Clinical Trial. J. Am. Geriatr. Soc. 2011, 59, 82–90. [Google Scholar] [CrossRef]
- Djokic, G.; Vojvodic, P.; Korcok, D.; Agic, A.; Rankovic, A.; Djordjevic, V.; Vojvodic, A.; Vlaskovic-Jovicevic, T.; Peric-Hajzler, Z.; Vojvodic, J.; et al. The Effects of Magnesium—Melatonin—Vit B Complex Supplementation in Treatment of Insomnia. Open Access Maced. J. Med Sci. 2019, 7, 3101–3105. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hulsken, S.; Martin, A.; Mohajeri, M.H.; Homberg, J.R. Food-derived serotonergic modulators: Effects on mood and cognition. Nutr. Res. Rev. 2013, 26, 223–234. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mohajeri, M.H.; Wittwer, J.; Vargas, K.; Hogan, E.; Holmes, A.; Rogers, P.J.; Goralczyk, R.; Gibson, E.L. Chronic treatment with a tryptophan-rich protein hydrolysate improves emotional processing, mental energy levels and reaction time in middle-aged women. Br. J. Nutr. 2015, 113, 350–365. [Google Scholar] [CrossRef] [Green Version]
- Scholz-Ahrens, K.E.; Ahrens, F.; Barth, C.A. Nutritional and health attributes of milk and milk imitations. Eur. J. Nutr. 2019, 59, 19–34. [Google Scholar] [CrossRef]
- Komada, Y.; Okajima, I.; Kuwata, T. The Effects of Milk and Dairy Products on Sleep: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 9440. [Google Scholar] [CrossRef]
- Březinová, V.; Oswald, I. Sleep after a Bedtime Beverage. BMJ 1972, 2, 431–433. [Google Scholar] [CrossRef] [Green Version]
- Adam, K. Dietary Habits and Sleep After Bedtime Food Drinks. Sleep 1980, 3, 47–58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Valtonen, M.; Niskanen, L.; Kangas, A.-P.; Koskinen, T. Effect of melatonin-rich night-time milk on sleep and activity in elderly institutionalized subjects. Nord. J. Psychiatry 2005, 59, 217–221. [Google Scholar] [CrossRef] [PubMed]
- Fakhr-Movahedi, A.; Mirmohammadkhani, M.; Ramezani, H. Effect of milk-honey mixture on the sleep quality of coronary patients: A clinical trial study. Clin. Nutr. ESPEN 2018, 28, 132–135. [Google Scholar] [CrossRef]
- Schramm, D.D.; Karim, M.; Schrader, H.R.; Holt, R.R.; Cardetti, A.M.; Keen, C.L. Honey with High Levels of Antioxidants Can Provide Protection to Healthy Human Subjects. J. Agric. Food Chem. 2003, 51, 1732–1735. [Google Scholar] [CrossRef]
- Paul, A.A.; Kumar, S.; Kumar, V.; Sharma, R. Milk Analog: Plant based alternatives to conventional milk, production, potential and health concerns. Crit. Rev. Food Sci. Nutr. 2020, 60, 3005–3023. [Google Scholar] [CrossRef]
- McKay, D.L.; Blumberg, J.B. A Review of the bioactivity and potential health benefits of chamomile tea (Matricaria recutita L.). Phytother. Res. 2006, 20, 519–530. [Google Scholar] [CrossRef]
- Hieu, T.H.; Dibas, M.; Dila, K.A.S.; Sherif, N.A.; Hashmi, M.U.; Mahmoud, M.; Trang, N.T.T.; Abdullah, L.; Nghia, T.L.B.; Hirayama, K.; et al. Therapeutic efficacy and safety of chamomile for state anxiety, generalized anxiety disorder, insomnia, and sleep quality: A systematic review and meta-analysis of randomized trials and quasi-randomized trials. Phytother. Res. 2019, 33, 1604–1615. [Google Scholar] [CrossRef]
- Chang, S.; Chen, C. Effects of an intervention with drinking chamomile tea on sleep quality and depression in sleep disturbed postnatal women: A randomized controlled trial. J. Adv. Nurs. 2015, 72, 306–315. [Google Scholar] [CrossRef] [PubMed]
- Singh, O.; Khanam, Z.; Misra, N.; Srivastava, M.K. Chamomile (Matricaria chamomilla L.): An overview. Pharmacogn. Rev. 2011, 5, 82–95. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salehi, B.; Venditti, A.; Sharifi-Rad, M.; Kręgiel, D.; Sharifi-Rad, J.; Durazzo, A.; Lucarini, M.; Santini, A.; Souto, E.B.; Novellino, E.; et al. The Therapeutic Potential of Apigenin. Int. J. Mol. Sci. 2019, 20, 1305. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Campbell, E.L.; Chebib, M.; Johnston, G.A. The dietary flavonoids apigenin and (−)-epigallocatechin gallate enhance the positive modulation by diazepam of the activation by GABA of recombinant GABAA receptors. Biochem. Pharmacol. 2004, 68, 1631–1638. [Google Scholar] [CrossRef] [PubMed]
- Adib-Hajbaghery, M.; Mousavi, S.N. The effects of chamomile extract on sleep quality among elderly people: A clinical trial. Complement. Ther. Med. 2017, 35, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Zick, S.M.; Wright, B.D.; Sen, A.; Arnedt, J.T. Preliminary examination of the efficacy and safety of a standardized chamomile extract for chronic primary insomnia: A randomized placebo-controlled pilot study. BMC Complement. Altern. Med. 2011, 11, 78. [Google Scholar] [CrossRef] [Green Version]
- Durg, S.; Dhadde, S.B.; Vandal, R.; Shivakumar, B.S.; Charan, C.S. Withania somnifera (Ashwagandha) in neurobehavioural disorders induced by brain oxidative stress in rodents: A systematic review and meta-analysis. J. Pharm. Pharmacol. 2015, 67, 879–899. [Google Scholar] [CrossRef]
- Nile, S.H.; Nile, A.; Gansukh, E.; Baskar, V.; Kai, G. Subcritical water extraction of withanosides and withanolides from ashwagandha (Withania somnifera L) and their biological activities. Food Chem. Toxicol. 2019, 132, 110659. [Google Scholar] [CrossRef]
- Langade, D.; Kanchi, S.; Salve, J.; Debnath, K.; Ambegaokar, D. Efficacy and Safety of Ashwagandha (Withania somnifera) Root Extract in Insomnia and Anxiety: A Double-blind, Randomized, Placebo-controlled Study. Cureus 2019, 11, e5797. [Google Scholar] [CrossRef] [Green Version]
- Langade, D.; Thakare, V.; Kanchi, S.; Kelgane, S. Clinical evaluation of the pharmacological impact of ashwagandha root extract on sleep in healthy volunteers and insomnia patients: A double-blind, randomized, parallel-group, placebo-controlled study. J. Ethnopharmacol. 2021, 264, 113276. [Google Scholar] [CrossRef] [PubMed]
- Marder, M.; Viola, H.; Wasowski, C.; Fernández, S.; Medina, J.H.; Paladini, A.C. 6-Methylapigenin and hesperidin: New valeriana flavonoids with activity on the CNS. Pharmacol. Biochem. Behav. 2003, 75, 537–545. [Google Scholar] [CrossRef]
- Yuan, C.-S.; Mehendale, S.; Xiao, Y.; Aung, H.H.; Xie, J.-T.; Ang-Lee, M.K. The Gamma-Aminobutyric Acidergic Effects of Valerian and Valerenic Acid on Rat Brainstem Neuronal Activity. Anesthesia Analg. 2004, 98, 353–358. [Google Scholar] [CrossRef]
- Fernández, S.; Wasowski, C.; Paladini, A.C.; Marder, M. Sedative and sleep-enhancing properties of linarin, a flavonoid-isolated from Valeriana officinalis. Pharmacol. Biochem. Behav. 2004, 77, 399–404. [Google Scholar] [CrossRef]
- Taibi, D.M.; Vitiello, M.V.; Barsness, S.; Elmer, G.W.; Anderson, G.D.; Landis, C.A. A randomized clinical trial of valerian fails to improve self-reported, polysomnographic, and actigraphic sleep in older women with insomnia. Sleep Med. 2009, 10, 319–328. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ziegler, G.; Ploch, M.; Miettinen-Baumann, A.; Collet, W. Efficacy and tolerability of valerian extract LI 156 compared with oxazepam in the treatment of non-organic insomnia--a randomized, double-blind, comparative clinical study. Eur. J. Med. Res. 2002, 7, 480–486. [Google Scholar]
- Taavoni, S.; Ekbatanin, N.N.; Haghani, H. Can valerian improve menopausal sleep quality? J. Neurol. Sci. 2013, 333, e629. [Google Scholar] [CrossRef]
- Diaper, A.; Hindmarch, I. A double-blind, placebo-controlled investigation of the effects of two doses of a valerian preparation on the sleep, cognitive and psychomotor function of sleep-disturbed older adults. Phytother. Res. 2004, 18, 831–836. [Google Scholar] [CrossRef] [PubMed]
- Shinjyo, N.; Waddell, G.; Green, J. Valerian Root in Treating Sleep Problems and Associated Disorders—A Systematic Review and Meta-Analysis. J. Evid. Based Integr. Med. 2020, 25. [Google Scholar] [CrossRef]
- Williams, J.L.; Everett, J.M.; D’Cunha, N.M.; Sergi, D.; Georgousopoulou, E.N.; Keegan, R.J.; McKune, A.J.; Mellor, D.D.; Anstice, N.; Naumovski, N. The Effects of Green Tea Amino Acid L-Theanine Consumption on the Ability to Manage Stress and Anxiety Levels: A Systematic Review. Plant. Foods Hum. Nutr. 2020, 75, 12–23. [Google Scholar] [CrossRef]
- Unno, K.; Yamada, H.; Iguchi, K.; Ishida, H.; Iwao, Y.; Morita, A.; Nakamura, Y. Anti-stress Effect of Green Tea with Lowered Caffeine on Humans: A Pilot Study. Biol. Pharm. Bull. 2017, 40, 902–909. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Unno, K.; Noda, S.; Kawasaki, Y.; Yamada, H.; Morita, A.; Iguchi, K.; Nakamura, Y. Ingestion of green tea with lowered caffeine improves sleep quality of the elderly via suppression of stress. J. Clin. Biochem. Nutr. 2017, 61, 210–216. [Google Scholar] [CrossRef] [Green Version]
- Unno, K.; Noda, S.; Kawasaki, Y.; Yamada, H.; Morita, A.; Iguchi, K.; Nakamura, Y. Reduced Stress and Improved Sleep Quality Caused by Green Tea Are Associated with a Reduced Caffeine Content. Nutrients 2017, 9, 777. [Google Scholar] [CrossRef] [PubMed]
- Hu, J.; Webster, D.; Cao, J.; Shao, A. The safety of green tea and green tea extract consumption in adults—Results of a systematic review. Regul. Toxicol. Pharmacol. 2018, 95, 412–433. [Google Scholar] [CrossRef]
- Liguori, I.; Russo, G.; Curcio, F.; Bulli, G.; Aran, L.; DELLA Morte, D.; Gargiulo, G.; Testa, G.; Cacciatore, F.; Bonaduce, D.; et al. Oxidative stress, aging, and diseases. Clin. Interv. Aging 2018, ume 13, 757–772. [Google Scholar] [CrossRef] [Green Version]
- Granato, D.; Nunes, D.S.; Barba, F.J. An integrated strategy between food chemistry, biology, nutrition, pharmacology, and statistics in the development of functional foods: A proposal. Trends Food Sci. Technol. 2017, 62, 13–22. [Google Scholar] [CrossRef]
- Santana-Gálvez, J.; Cisneros-Zevallos, L.; Jacobo-Velázquez, D.A. A practical guide for designing effective nutraceutical combinations in the form of foods, beverages, and dietary supplements against chronic degenerative diseases. Trends Food Sci. Technol. 2019, 88, 179–193. [Google Scholar] [CrossRef]
- DeMuro, R.L.; Nafziger, A.N.; Blask, D.E.; Menhinick, A.M.; Bertino, J.S., Jr. The Absolute Bioavailability of Oral Melatonin. J. Clin. Pharmacol. 2000, 40, 781–784. [Google Scholar] [CrossRef]
- Scheid, L.; Ellinger, S.; Alteheld, B.; Herholz, H.; Ellinger, J.; Henn, T.; Helfrich, H.-P.; Stehle, P. Kinetics of L-Theanine Uptake and Metabolism in Healthy Participants Are Comparable after Ingestion of L-Theanine via Capsules and Green Tea. J. Nutr. 2012, 142, 2091–2096. [Google Scholar] [CrossRef] [Green Version]
- Ye, Q.; Georges, N.; Selomulya, C. Microencapsulation of active ingredients in functional foods: From research stage to commercial food products. Trends Food Sci. Technol. 2018, 78, 167–179. [Google Scholar] [CrossRef]
- Dhakal, S.P.; He, J. Microencapsulation of vitamins in food applications to prevent losses in processing and storage: A review. Food Res. Int. 2020, 137, 109326. [Google Scholar] [CrossRef]
- Greene, S.C.; Noonan, P.K.; Sanabria, C.; Peacock, W.F. Effervescent N-Acetylcysteine Tablets versus Oral Solution N-Acetylcysteine in Fasting Healthy Adults: An Open-Label, Randomized, Single-Dose, Crossover, Relative Bioavailability Study. Curr. Ther. Res. 2016, 83, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Compound | Reference/Country | Participants | Intervention/Duration | Study Design | Outcome Measures | Effects on Sleep |
|---|---|---|---|---|---|---|
| Markus et al. (2005) [40] Netherlands | Adults without sleep complaints (n = 14) Age (22 ± 3 years) Adults with mild sleep complaint (n = 14) Age (22 ± 2 years) | 20 g L-TRP-enriched A-LAC protein (4.8 g L-TRP/100 g amino acids w/w) 1 night | Double-blind Placebo-controlled | Subjective Sleep Quality Measures: Stanford Sleepiness Scale | Improved morning alertness (p = 0.013) and increased attention (p = 0.002) in both groups. Improved performance in participants with sleep complaints only (p = 0.05). | |
| L-Tryptophan | Ong et al. (2017) [41] Australia | Healthy males without sleep complaint (n = 10) Age (26.9 ± 5.3 years) | 20 g L-TRP-enriched A-LAC protein (4.8 g L-TRP/100 g amino acids w/w) of A-LAC protein 2 nights | Double-blind Placebo-controlled Randomized Crossover | Objective Sleep Quality Measures (Actigraphy): Total sleep time Sleep onset latency Sleep efficiency (%) Wake time after sleep onset Subjective Sleep Measures (Sleep Log): Bedtime Time taken to fall asleep Frequency of awakenings Time taken to return to sleep Waking time Rising time Total sleep time | Increased objective and subjective total sleep time by 12.8% (p = 0.037) and 10.8% (p = 0.013), respectively; increased objective sleep efficiency by 7.0% (p = 0.028). |
| Cubero et al. (2007) [42] Spain | Pre-weaning infants (n = 30) Age (4–20 weeks) | Diet A: Standard formula Diet B: Standard formula during the day and night formula (3.4 g L-TRP/100 g protein) Diet C: Day formula during the day (1.5 g L-TRP/100 g protein) + night formula (3.4 g L-TRP/100 g protein) in the evening 1 week per formula | Double-blind Randomized | Objective Sleep Quality Measures (Actigraphy): Time of nocturnal sleep Minutes of immobility Sleep latency Nocturnal awakenings Sleep efficiency (%) Sleep Diary: Sleep over 24 h Number of bottle feeds Observations or incidences that would influence the infants rest | Diet C improved objective total sleep time (p < 0.05) and subjective (parent) sleep improvement; Diet B and Diet C reduced objective sleep onset latency; Diet B improved objective sleep efficiency. (All p’s < 0.05) | |
| Bravo et al. (2013) [43] Spain | Older adults with sleep difficulties (n = 35) Age (55–75 years) | L-TRP (60 mg) enriched cereal for breakfast and dinner 1 week | Blind assay | Objective Sleep Quality Measures (Actigraphy): Time in bed Assumed sleep Actual sleep time Sleep onset latency Sleep efficiency (%) Number of awakenings Immobile time Total activity Fragmentation index (indicator of quality of rest) | Improvements in objective sleep measures including increase in actual sleep time (p < 0.01); increase in sleep efficiency (p < 0.001); increase in immobile time (p < 0.01); reduction in sleep latency (p < 0.01); wake bouts (p < 0.05); total activity (p < 0.01); fragmentation index (p < 0.001). | |
| 5-HTP | Bruni et al. (2004) [44] Italy | Children with sleep terrors (n = 45) Age (3.2–10.6 years) | 2 mg/kg (Daily) 20 days | Randomized, controlled | Frequency of sleep terrors | After 1-month: Sleep terrors reduced > 50% from baseline in 93.5% of children treated with 5-HTP (p < 0.00001). After 6 months: 51.6% were sleep-terror free (p < 0.001). |
| Melatonin | Scheer et al. (2012) [45] USA | Hypertensive adults on beta blockers (n = 16) Age (45–64 years) | 2.5 mg (nightly, 1 h before bedtime) 3 weeks | Randomized, Double-blind Placebo-controlled Parallel-group design | Objective Sleep Quality Measures (Polysomnography): Sleep stages Total sleep time Time in bed Sleep efficiency (%) Objective Sleep Quality Measures (Actigraphy): Sleep onset latency Total sleep time Sleep efficiency (%) | Increased total sleep time by 32 min (p = 0.046); increased sleep efficiency by 7.6% (p = 0.046). Decreased sleep onset latency to stage 2 NREM sleep by 14 min (p = 0.001) and increased the duration of stage 2 NREM sleep by 42 min (p = 0.037). |
| Grima et al. (2018) [46] Australia | Adults with sleep disturbance post onset of traumatic brain injury (n = 33) Age (37 ± 11 years) | 2 mg (nightly 2 h before bedtime) 4 weeks | Randomized, Double-blind Placebo-controlled Two-period Two-treatment Crossover study | Objective Sleep Quality Measures (Actigraphy) Sleep onset latency Total sleep time Sleep duration Sleep efficiency (%) Sleep Diary: Sleep onset/offset Sleep duration Subjective Sleep Quality Measures: PSQI ESS FSS | Improved subjective sleep quality (p < 0.0001) and objective sleep efficiency (p < 0.04). | |
| Xu et al. (2020) [47] China | Adults with primary insomnia (n = 97) Age (45–60 years) | 3 mg (nightly 1 h before bedtime) 4 weeks | Randomized, Double-blind Placebo-controlled Parallel study | Objective Sleep Quality Measures (Polysomnography): Sleep stages Total sleep time Sleep onset latency Wake after sleep onset Sleep efficiency (%) Subjective Sleep Quality Measures: PSQI ESS ISI | Decreased objective sleep measures including early morning wake (p = 0.001) and decreased percentage of Stage 2 NREM sleep (p = 0.031). | |
| L-Cysteine | Sadasivam et al. (2011) [48] India | Adults with obstructive sleep apnea (n = 20) Age (53.1 ± 2.3 years) | 600 mg (Mucinac, Cipla), three times per day 30 days | Randomized, Placebo-controlled | Objective Sleep Quality Measures (Polysomnography): Sleep stages Total sleep time Sleep onset latency Wake after sleep onset Sleep efficiency (%) Sleep apnea Snoring Subjective Sleep Quality Measures: ESS | Improvements in objective slow wave sleep as sleep percent time (p < 0.001) and sleep efficiency. (p < 0.05). Reduction in subjective Epworth Sleepiness Score (p < 0.001). |
| Rao et al. (2019) [49] Japan | Healthy adult males (n = 22) Age (27.5 ± 0.9 years) | 4 × 50 mg (nightly, 1 h before bedtime) 6 days | Randomized, Double-blind Placebo-controlled Crossover trial | Objective Sleep Quality Measures (Actigraphy): Time in bed Wake after sleep onset Sleep onset latency Sleep length Sleep efficiency (%) Subjective Sleep Quality Measures: Obstructive Sleep Apnea Inventory questionnaire | Improvements in objective sleep measures including an increase in objective sleep efficiency (p < 0.047) and reduction in intermittent wakening (p < 0.044). Improvements in subjective sleep measures including feeling of recovery from exhaustion or fatigue scores (p < 0.042) and improvement in refreshed upon awakening scores (p < 0.014). | |
| L-Theanine | Lyon et al. (2011) [50] Canada | Boys with ADHD (n = 98) Age (8–12 years) | 2 × 100 mg (twice per day, morning and evening) 6 weeks | Randomized, Double-blind Placebo-controlled Parallel trial | Objective Sleep Quality Measures (Actigraphy): Wake after sleep onset Sleep onset latency Sleep length Nocturnal activity Sleep efficiency (%) Subjective Sleep Quality Measures: Pediatric Sleep Questionnaire | Improved objective measures including sleep efficiency (p < 0.05), and reduced nocturnal activity (p < 0.05). |
| Sarris et al. (2019) [51] Australia | Adults with GAD (n = 46) Age (40.7 ± 15 years in TG; 32.2 ± 9.29 years in PG) | 225 mg (twice daily); increased to 450 mg (twice daily) if anxiety score did not reduce by ≥35% after 4 weeks 8 weeks | Randomized, Double-blind Placebo-controlled Multi-center pilot study | Subjective Sleep Quality Measures: ISI | Improved subjective sleep satisfaction (p < 0.015); improvements in ISI scores for “difficulty in falling asleep” (p < 0.049); “Problems waking up too early” (p < 0.017); and “interference with daily functioning” (p = 0.030) in control. | |
| Hidese et al. (2019) [52] Japan | Healthy Adults (n = 30) Age (48.3 ± 11.9 years) | 200 mg tablet daily before sleep 4 weeks | Randomized, Double-blind Placebo-controlled Crossover trial | Subjective Sleep Quality Measures: PSQI | Improved subjective sleep quality (p < 0.013), reduced sleep onset latency, sleep disturbance and use of sleep medication (All p’s < 0.05). | |
| Vitamin B12 | Mayer et al. (1996) [53] | Healthy Adults (n = 20) Age (CB12 = 36.6 ± 5.2 years. MB12 = 36.2 ± 5.2 years) | 3 mg (cyano-(CB12) or methylcobalamin (MB12)) 14 days | Randomized Single-blind Between subject’s design | Objective Sleep Quality Measures (Actigraphy): Wake after sleep onset Sleep onset latency Sleep length Nocturnal activity Sleep efficiency (%) Subjective Sleep Quality Measures: Morning and Evening VAS | Reduction in objective sleep time (p = 0.036) in MB12 group improvements in sleep quality and daytime alertness (All p’s < 0.05). |
| Luboshitzky et al. (2002) [54] Israel | Healthy Adult Males (n = 12) Age (22–26 years) | 100 mg (5.00 PM) Once | Randomized Placebo-controlled Parallel trial | Objective Sleep Quality Measures (EEG): Sleep stages (%) Total recording time Sleep latency Actual sleep time Sleep efficiency (%) REM latency | No effect. | |
| Vitamin B6 | Ebben et al. (2002) [55] USA | Healthy Adults (n = 12) Age (18–28 years) | 100 mg 250 mg Placebo (All nightly before bed) 5 days per treatment | Placebo-controlled Double-blind Crossover trial | Subjective Sleep Quality Measures: Sleep questionnaire Dream Salience Scale | Increase in dream salient scores in 250 mg B6 treatment compared to placebo (p = 0.05). |
| Aspy et al. (2018) [56] Australia | Healthy Adults (n = 100) Age (mean = 27.5) | 120 mg (pyridoxine hydrochloride) Vitamin B Complex (120 mg pyridoxine hydrochloride + other B vitamins) Placebo (All nightly before bed) 5 days | Randomized Double-blind Placebo-controlled trial | Subjective Sleep Quality Measures: Sleep log | Increased the amount of dream content recalled (p = 0.032) and decrease in sleep quality (p = 0.014) in B complex group. | |
| Vitamin D | Ghaderi et al. (2017) [57] Iran | Adults undergoing Methadone Treatment. (n = 68) Age (25–70 years) | 50,000 IU (once per fortnight) 12 weeks | Randomized Double-blind Placebo-controlled trial | Subjective Sleep Quality Measures: PSQI | Improvement in subjective sleep score (p = 0.02). |
| Mason et al. (2016) [58] USA | Overweight menopausal females with low VitD (n = 218) Age (50–75 years) | 2000 IU vitamin D3 (daily) 12 months | Randomized Double-blind Placebo-controlled trial | Subjective Sleep Quality Measures: PSQI | Increase in PSQI score (p = 0.01) and increase in need to take sleep medication (p < 0.01). | |
| Vitamin C | Dadashpour et al. (2018) [59] Iran | Adults on hemodialysis with sleep disorder (n = 90) Age (18–70 years) | 500 mg /5 cc intravenously–3 times per week 8 weeks | Randomized Double-blind Trial | Subjective Sleep Quality Measures: PSQI VAS | Reductions in subjective sleep quality, sleep latency, daytime dysfunction (All p’s = 0.001). |
| Yeom et al. (2007) [60] Korea | Adults with Stage IV cancer (n = 39) Age (53.5 ± 10.5 years) | 10 g vitamin C intravenously twice with 3-day interval, then 4 g oral supplement daily 1 week | Prospective study | Subjective Sleep Quality Measures: European Organization for Research and Treatment of Cancer Core Quality-of-Life questionnaire (EORTC QLQ-C30)-Korean Version | Lower subjective scores for sleep disturbance and fatigue (p < 0.005). | |
| Murck et al. (2000) [61] Germany | Older adults without sleep disturbances (n = 12) Age (60–80 years) | 10 mmol for 3 days, then 20 mmol for 3 days, then 30 mmol daily for 14 days | Randomized Placebo-controlled Crossover design | Objective Sleep Quality Measures (EEG): Sleep stages (%) Total recording time Sleep latency Actual sleep time Sleep efficiency (%) REM latency | Increase in slow wave sleep (p < 0.05), delta and sigma waves (p < 0.05 for both). | |
| Magnesium | Abbasi et al. (2012) [62] Iran | Older adults (n = 43) Age (65 ± 4.6 years) | 414 mg magnesium oxide (250 mg Mg) Twice per day 8 weeks | Double-blind Placebo-controlled trial | Subjective Sleep Quality Measures: ISI Sleep Log | Increase in subjective sleep time (p = 0.002) and subjective sleep efficiency (p = 0.03); decrease in subjective sleep onset latency (p = 0.04), and insomnia severity index (p = 0.006). |
| Hornyak et al. (2004) [63] Germany | Alcohol dependent adults in subacute withdrawal with sleep disturbance (n = 11) | 30 mmol Magnesium L-aspartate hydrochloride (10 mmol morning and 20 mmol evening) daily 4 weeks | Open Pilot Study | Objective Sleep Quality Measures (Polysomnography): Sleep stages Total sleep time Sleep onset latency Wake after sleep onset Sleep efficiency (%) Periodic leg movements in sleep (PLMS) Subjective Sleep Quality Measures: PSQI | Decrease in objective sleep latency (p = 0.03), improvement in subjective sleep quality (p = 0.05). | |
| Zinc | Saito et al. (2017) [64] Japan | Healthy Adults (n = 94) Age (20–84 years) | Group A: Placebo Group B: 15 mg Group C: 15 mg + Astx Group D: Placebo + 16 mg + Astx 12 weeks | Randomized Double-blind Placebo-controlled Parallel group trial | Objective Sleep Quality Measures (Actigraphy): Wake after sleep onset Sleep onset latency Sleep length Frequency Nocturnal activity Sleep efficiency (%) Subjective Sleep Quality Measures: PSQI | Improvements in objective sleep efficiency in group B (p = 0.025); objective sleep onset latency in Group B and D (p < 0.032) and (p = 0.004), respectively. |
| Gholipour et al. (2018) [65] Iran | ICU nurses (n = 54) Age (31.2 ± 5.42 years) | 1 × 220 mg (every 72 h) 1 month | Multi-center Randomized Two parallel group Placebo-controlled trial | Subjective Sleep Quality Measures: PSQI | Improvements in subjective total sleep quality (p < 0.002); sleep onset latency (p < 0.003), sleep duration (p < 0.02) and total sleep quality score (p < 0.008). |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bulman, A.; D’Cunha, N.M.; Marx, W.; McKune, A.J.; Jani, R.; Naumovski, N. Nutraceuticals as Potential Targets for the Development of a Functional Beverage for Improving Sleep Quality. Beverages 2021, 7, 33. https://doi.org/10.3390/beverages7020033
Bulman A, D’Cunha NM, Marx W, McKune AJ, Jani R, Naumovski N. Nutraceuticals as Potential Targets for the Development of a Functional Beverage for Improving Sleep Quality. Beverages. 2021; 7(2):33. https://doi.org/10.3390/beverages7020033
Chicago/Turabian StyleBulman, Amanda, Nathan M. D’Cunha, Wolfgang Marx, Andrew J. McKune, Rati Jani, and Nenad Naumovski. 2021. "Nutraceuticals as Potential Targets for the Development of a Functional Beverage for Improving Sleep Quality" Beverages 7, no. 2: 33. https://doi.org/10.3390/beverages7020033
APA StyleBulman, A., D’Cunha, N. M., Marx, W., McKune, A. J., Jani, R., & Naumovski, N. (2021). Nutraceuticals as Potential Targets for the Development of a Functional Beverage for Improving Sleep Quality. Beverages, 7(2), 33. https://doi.org/10.3390/beverages7020033








