Cobalt Iron Oxide (CoFe2O4) Nanoparticles Induced Toxicity in Rabbits
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Chemicals and Preparation of Nanomaterials
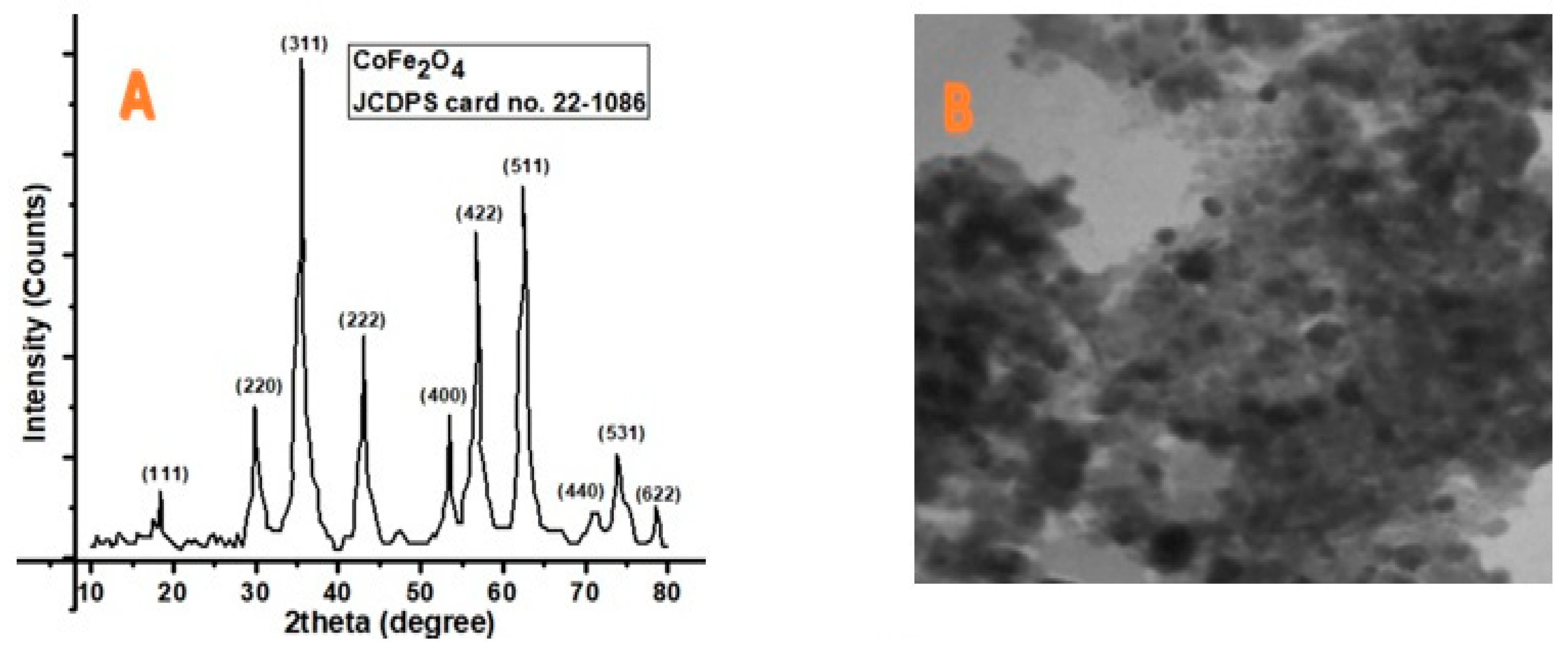
2.2. X-ray Diffraction (XRD) Analysis
2.3. Transmssion Electron Microscope (TEM) Analysis
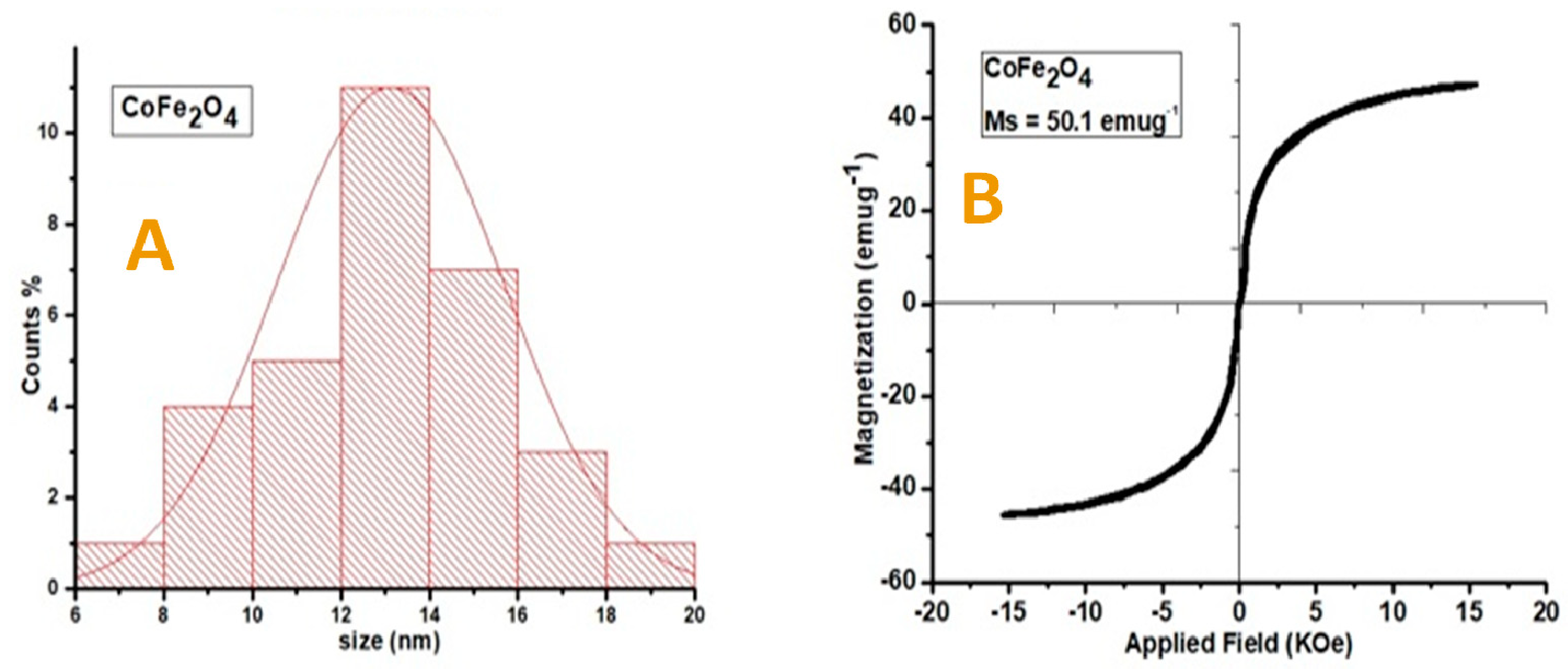
2.4. Vibrating Sample Magnetometer (VSM) Analysis
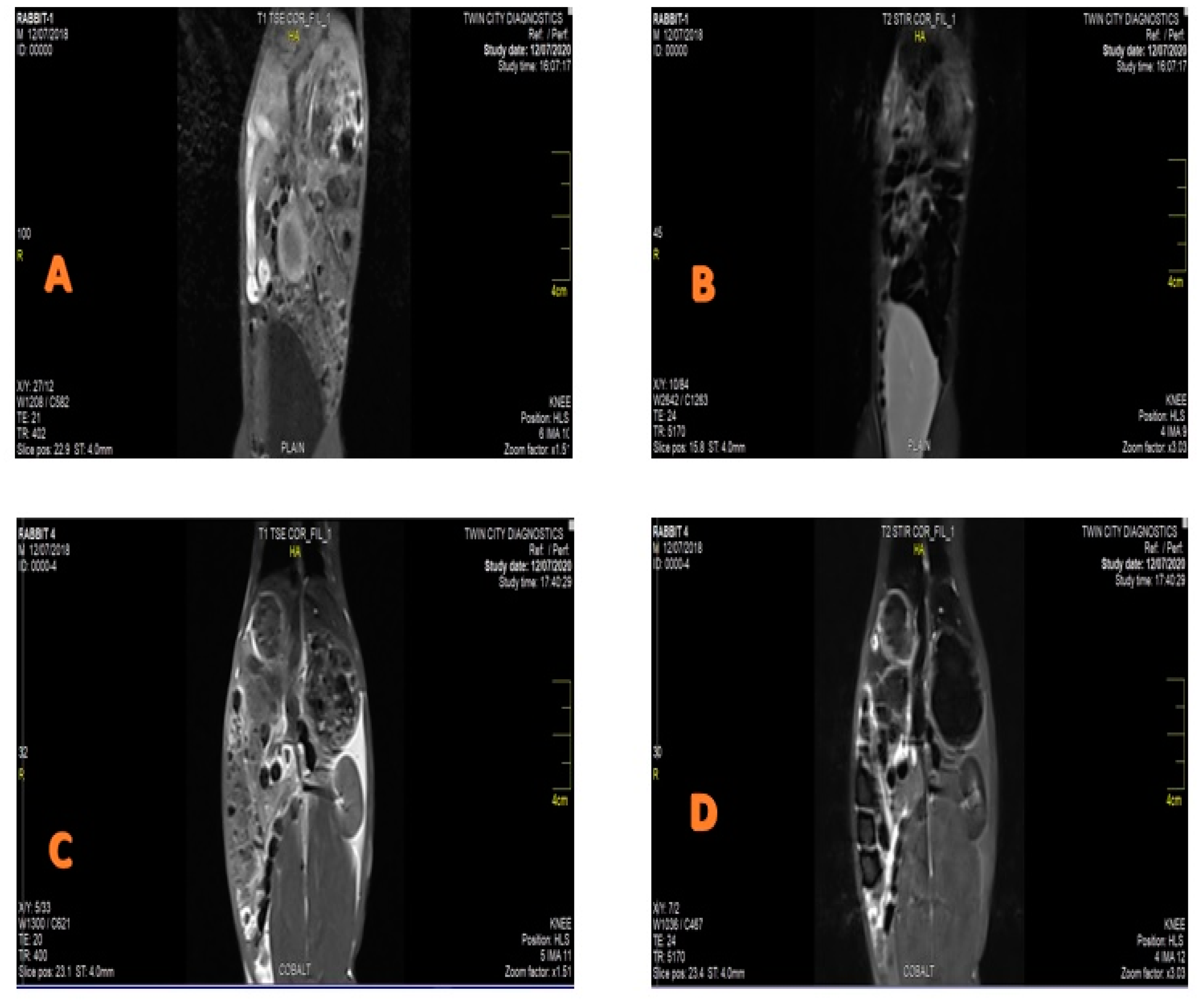
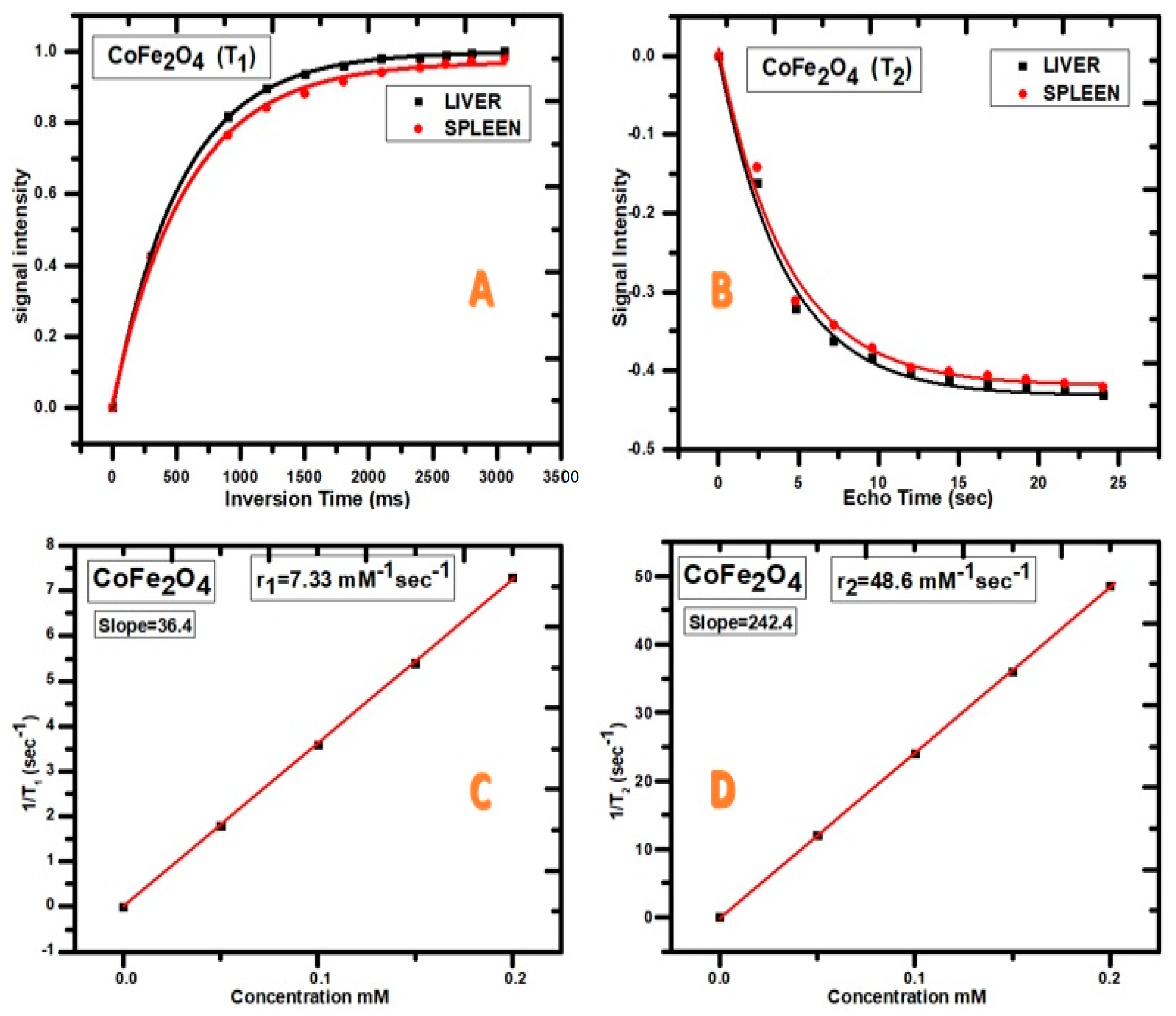
2.5. Magnetic Resonance Imaging (MRI) Contrast Agent (CA) and Relaxivity Analysis
2.6. Experimental Animals
2.7. Gross and Histopathology
2.8. Statistical Analysis
3. Results
3.1. XRD, Transmission Electron Microscope (TEM), and VSM Analysis
3.2. MRI Contrast Agent and Relaxivity
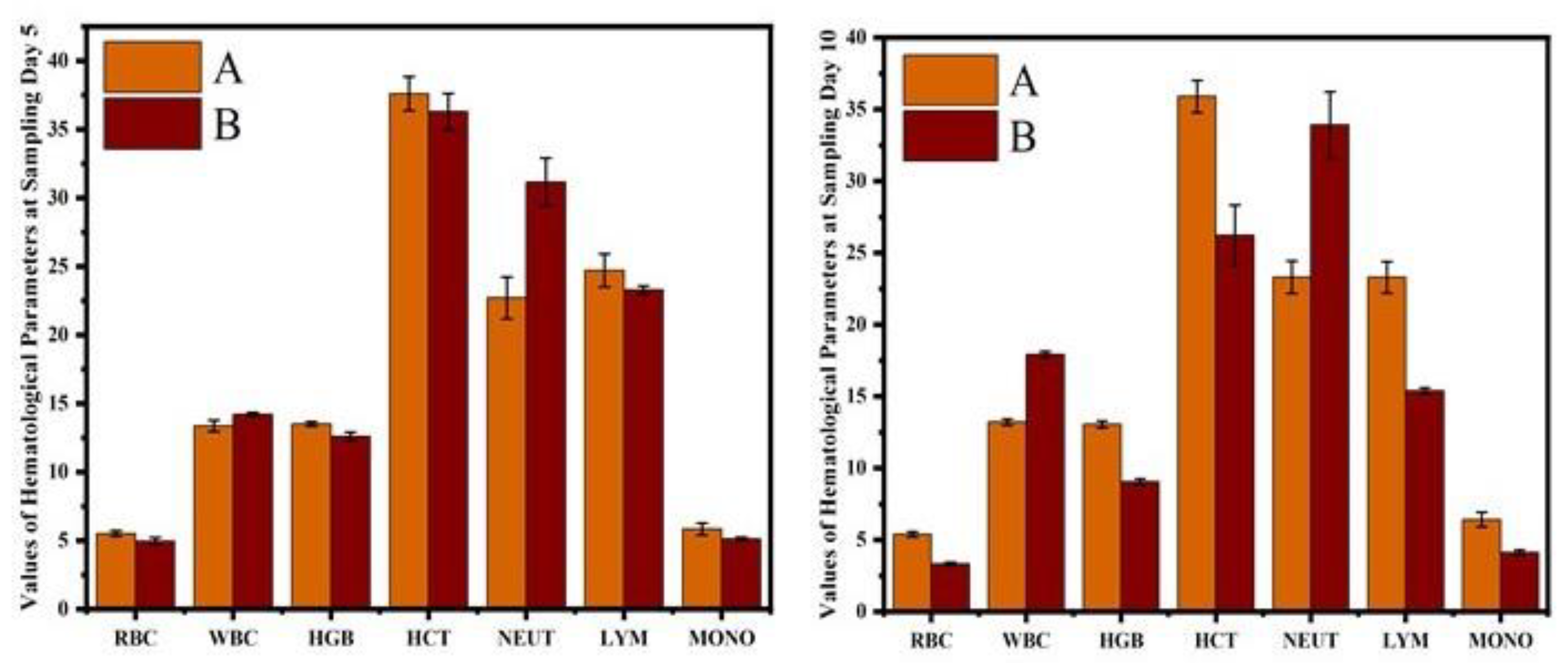
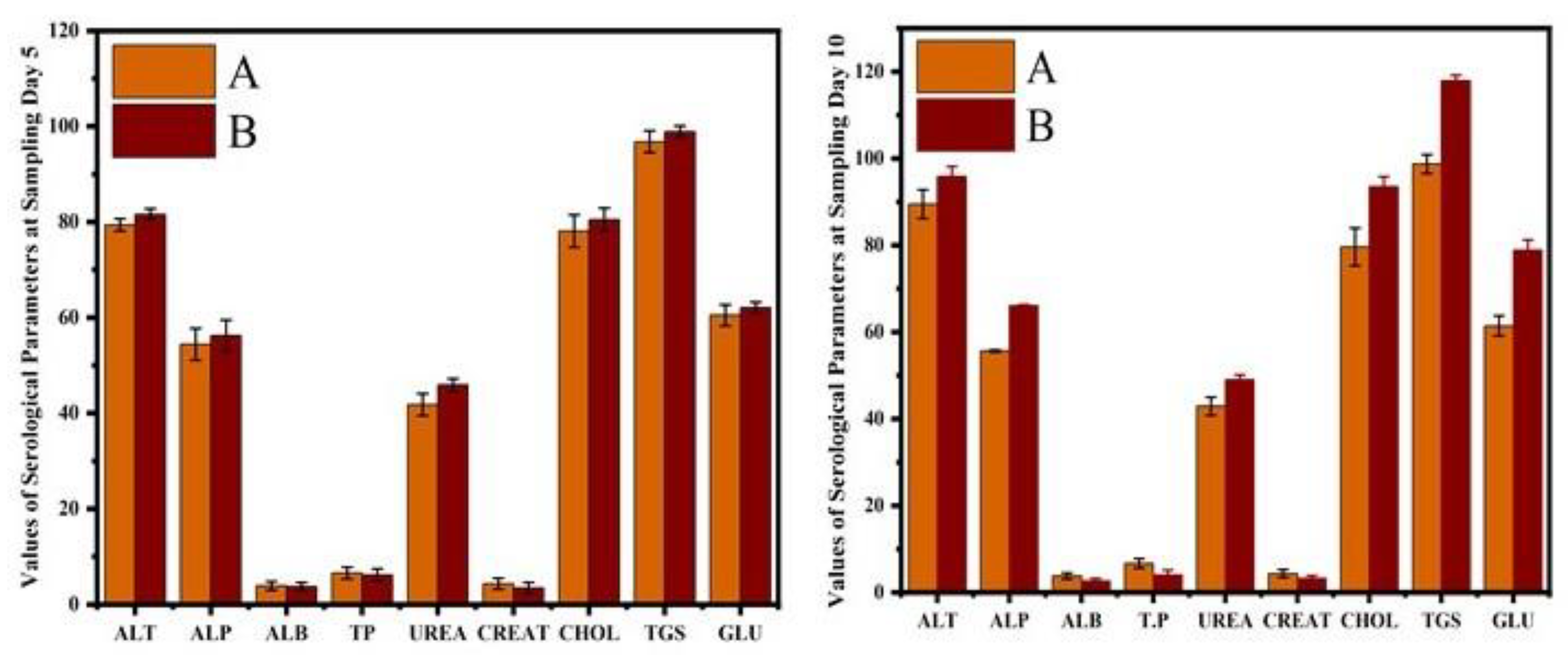
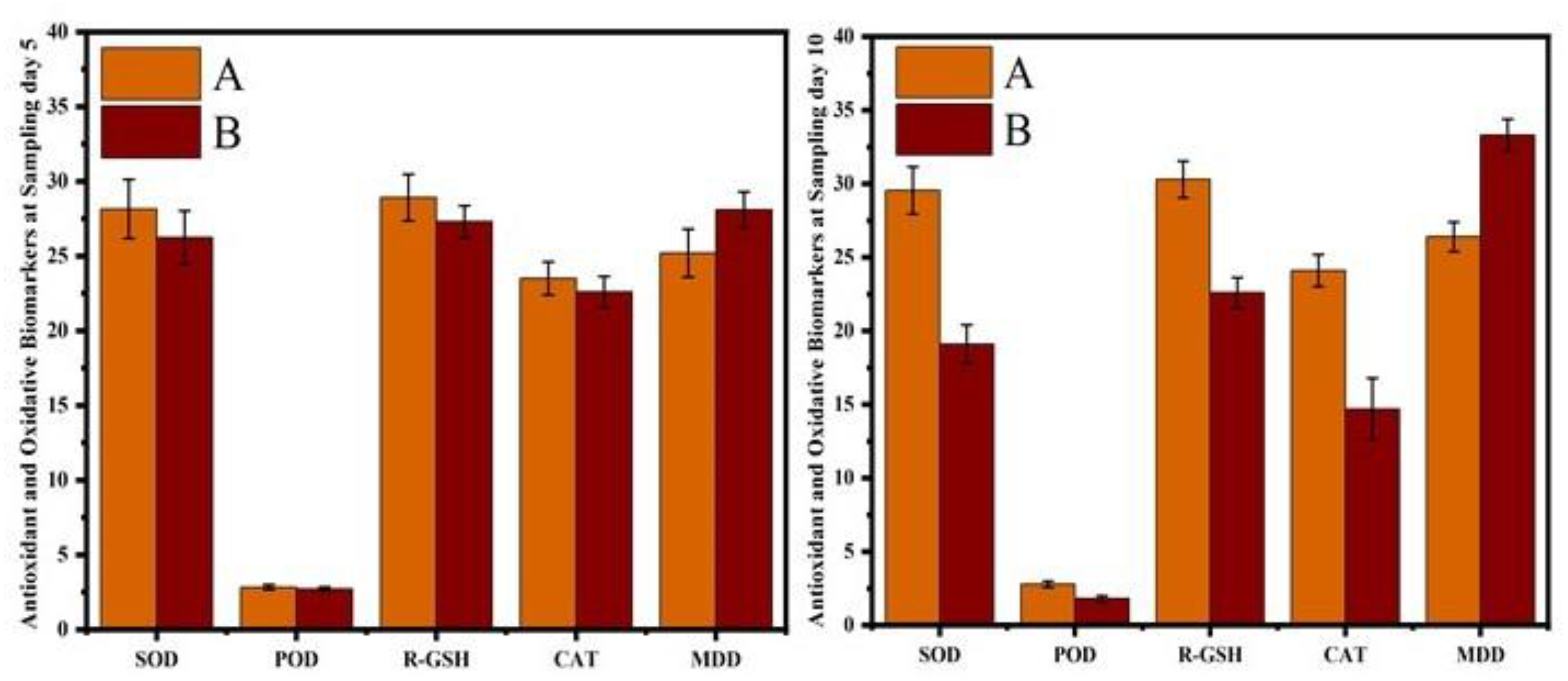
3.3. Hematological and Serum Analysis
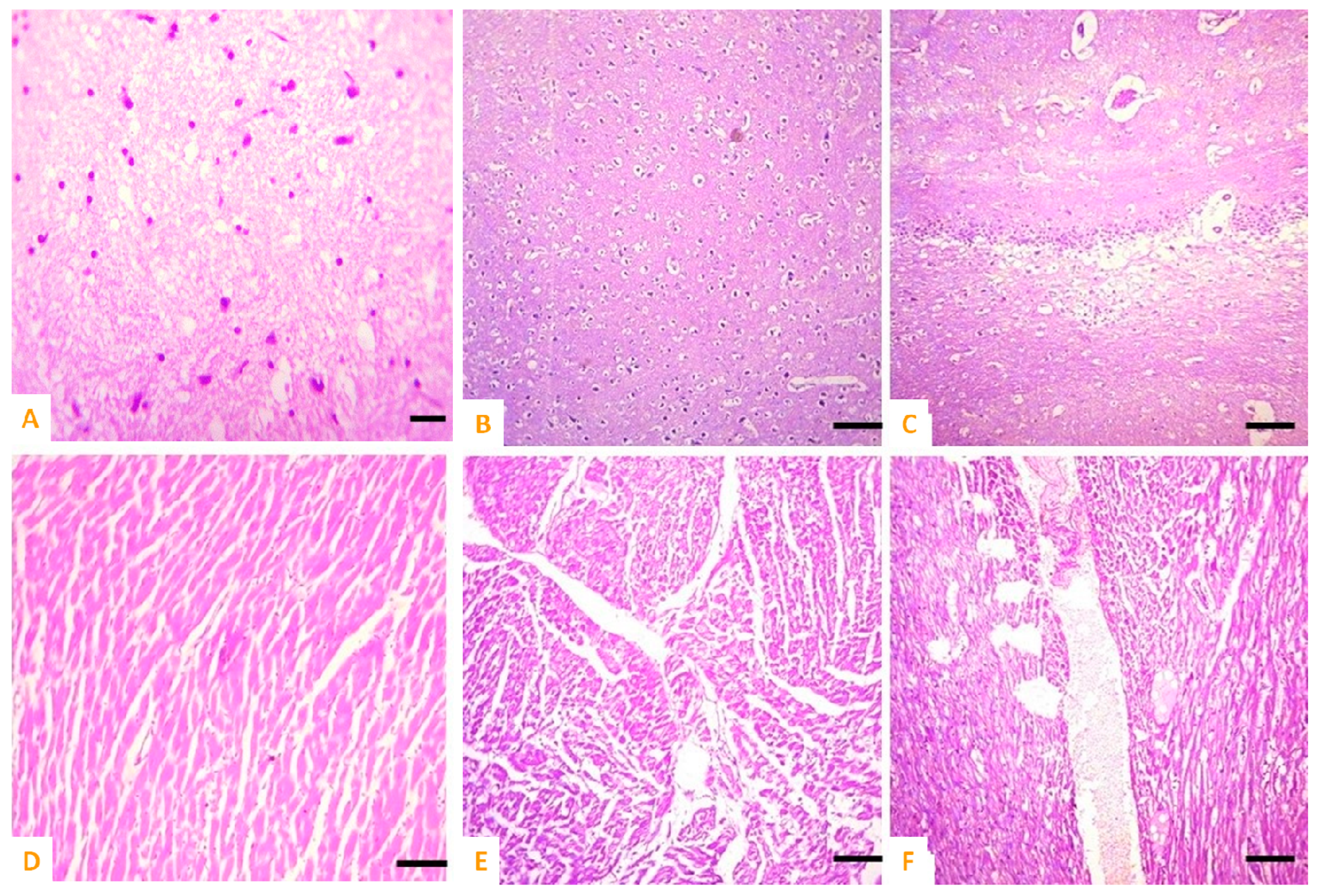
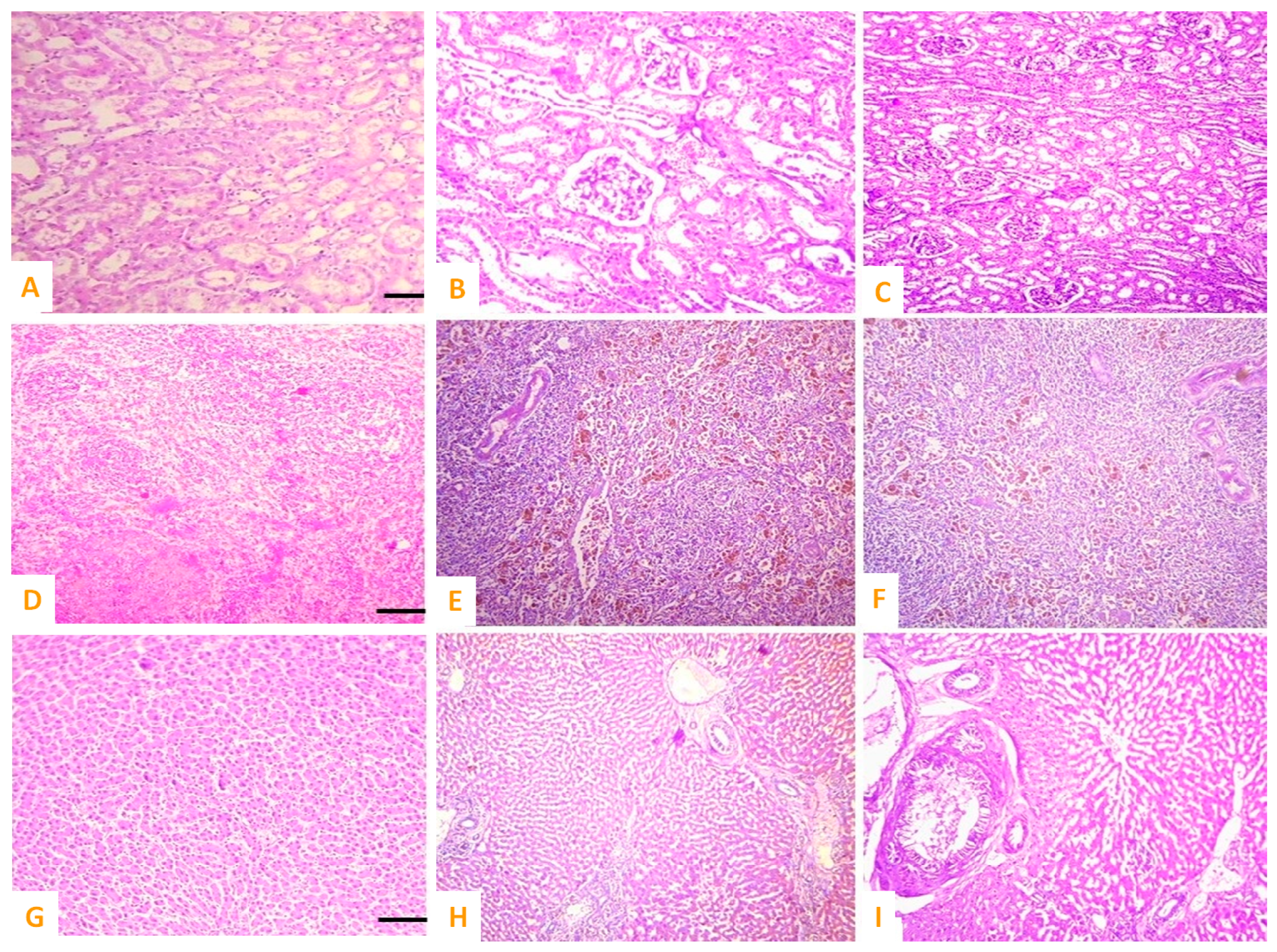
3.4. Microscopic Observations
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Budiyanto, E.; Salamon, S.; Wang, Y.; Wende, H.; Tüysüz, H. Phase segregation in cobalt iron oxide nanowires toward enhanced oxygen evolution reaction activity. J. Am. Chem. Soc. Au. 2022, 2, 697–710. [Google Scholar] [CrossRef] [PubMed]
- Wahab, A.; Imran, M.; Ikram, M.; Naz, M.; Aqeel, M.; Rafiq, A.; Majeed, H.; Ali, S. Dye degradation property of cobalt and manganese doped iron oxide nanoparticles. Appl. Nanosci. 2019, 9, 1823–1832. [Google Scholar] [CrossRef]
- Choppadandi, M.; Parmar, K.; Rao, K.S.; Rao, K.; Singh, A.; Kumar, H.; Guduru, A.T.; Shard, A.; Kapusetti, G. Self-regulated cobalt zinc ferrite system as a potential nanoplatform for the synergistic effect of hyperthermia-chemo agent for cancer therapy. Colloids Surf. B 2023, 222, 113077. [Google Scholar] [CrossRef] [PubMed]
- Kandeel, M.; Akhtar, T.; Zaheer, T.; Ahmad, S.; Ashraf, U.; Omar, M. Anti-parasitic Applications of Nanoparticles: A Review. Pak. Vet. J. 2022, 42, 2074–7764. [Google Scholar]
- Khan, I.; Zaneb, H.; Masood, S.; Ashraf, S.; Rehman, H.F.; Rehman, H.U.; Ahmad, S.; Taj, R.; Rahman, S.U. Supplemental Selenium Nanoparticles-loaded to Chitosan Improves Meat Quality, Pectoral Muscle Histology, Tibia Bone Morphometry and Tissue Mineral Retention in Broilers. Pak. Vet. J. 2022, 42, 236–240. [Google Scholar]
- Jalil, P.J.; Shnawa, B.H.; Hamad, S.M. Silver Nanoparticles: Green Synthesis, Characterization, Blood Compatibility and Protoscolicidal Efficacy against Echinococcus granulosus. Pak. Vet. J. 2021, 41. [Google Scholar]
- Zorai, A.; Souici, A.; Dragoe, D.; Rivière, E.; Ouhenia, S.; Belloni, J.; Mostafavi, M. Superparamagnetic cobalt ferrite nanoparticles synthesized by gamma irradiation. New J. Chem. 2023, 47, 2626–2634. [Google Scholar] [CrossRef]
- Kadam, R.; Shitole, R.; Kadam, S.; Desai, K.; Birajdar, A.; Barote, V.; Batoo, K.; Hussain, S.; Shirsath, S. A thorough Investigation of Rare-Earth Dy3+ Substituted Cobalt-Chromium Ferrite and Its Magnetoelectric Nanocomposite. Nanomaterials 2023, 13, 1165. [Google Scholar] [CrossRef]
- Varvaro, G.; Omelyanchik, A.; Peddis, D. Ferroic Transition Metal Oxide Nano-heterostructures: From Fundamentals to Applications. In Tailored Functional Oxide Nanomaterials: From Design to Multi-Purpose Applications; Chiara, M., Davide, B., Eds.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2022; pp. 405–437. [Google Scholar]
- Dippong, T.; Levei, E.A.; Cadar, O. Investigation of structural, morphological and magnetic properties of MFe2O4 (M = Co, Ni, Zn, Cu, Mn) obtained by thermal decomposition. Int. J. Mol. Sci. 2022, 23, 8483. [Google Scholar] [CrossRef]
- Nahar, A.; Maria, K.H.; Liba, S.; Anwaruzzaman, M.; Khan, M.; Islam, A.; Choudhury, S.; Hoque, S. Surface-modified CoFe2O4 nanoparticles using Folate-Chitosan for cytotoxicity Studies, hyperthermia applications and Positive/Negative contrast of MRI. J. Magn. Magn. Mater. 2022, 554, 169282. [Google Scholar] [CrossRef]
- Hosseinzadeh, H.; Oveisi, H. Synthesis Factors Dependence of Magnetic Properties of CoFe2O4 and CoFe2-xGdxO4 Semicrystalline Nanoparticles with desired Morphology through Hydrothermal Procedure. Res. Sq. 2022; preprint. [Google Scholar]
- Salsabil, S.S.; Ardana, V.P.; Larastiyasa, R.R.P.B.; Pratiwi, I.W.; Widianti, R.A.; Pratama, A.M. Nanoparticles of Kirinyuh (Chromolaena odorata (L.) RM King & H. Rob.) Leaves Extract as a Candidate for Natural Remedies Lowering Hypercholesterol: In Silico and In vivo Study. Pak. Vet. J. 2022, 42, 397–403. [Google Scholar]
- Hou, K.; Zhang, Y.; Bao, M.; Xin, C.; Wei, Z.; Lin, G.; Wang, Z. A multifunctional magnetic red blood cell-mimetic micromotor for drug delivery and image-guided therapy. ACS Appl. Mater. Interfaces 2022, 14, 3825–3837. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Han, K.; Ma, S.; Qi, X.; Guo, L.; Li, X. Blood cells as supercarrier systems for advanced drug delivery. Med. Drug Discov. 2022, 13, 100119. [Google Scholar] [CrossRef]
- Wei, X.; Cai, L.; Chen, H.; Shang, L.; Zhao, Y.; Sun, W. Noninvasive multiplexed analysis of bladder cancer-derived urine exosomes via janus magnetic microspheres. Anal. Chem. 2022, 94, 18034–18041. [Google Scholar] [CrossRef]
- Kong, C.; Zhang, S.; Lei, Q.; Wu, S. State-of-the-art advances of nanomedicine for diagnosis and treatment of bladder cancer. Biosensors 2022, 12, 796. [Google Scholar] [CrossRef]
- Apu, E.H.; Nafiujjaman, M.; Sandeep, S.; Makela, A.V.; Khaleghi, A.; Vainio, S.; Contag, C.H.; Li, J.; Balasingham, I.; Kim, T. Biomedical applications of multifunctional magnetoelectric nanoparticles. Mater. Chem. Front. 2022, 6, 1368–1390. [Google Scholar]
- Khan, M.S.; Buzdar, S.A.; Hussain, R.; Afzal, G.; Jabeen, G.; Javid, M.A.; Iqbal, R.; Iqbal, Z.; Mudassir, K.B.; Saeed, S. Hematobiochemical, oxidative stress, and histopathological mediated toxicity induced by nickel ferrite (NiFe2O4) nanoparticles in rabbits. Oxid. Med. Cell. Longev. 2022, 2022, 5066167. [Google Scholar] [CrossRef]
- Chalise, D.; Cahill, D.G. Highly Sensitive and High-Throughput Magnetic Resonance Thermometry of Fluids Using Superparamagnetic Nanoparticles. Phys. Rev. Appl. 2023, 19, 014055. [Google Scholar] [CrossRef]
- Barrera, G.; Allia, P.; Tiberto, P. Magnetization dynamics of superparamagnetic nanoparticles for magnetic particle spectroscopy and imaging. Phys. Rev. Appl. 2022, 18, 024077. [Google Scholar] [CrossRef]
- Rahman, M.R.; Bake, A.; Islam, S.M.K.N.; Wu, L.; Khakbaz, H.; FitzGerald, S.; Chalifour, A.; Livesey, K.L.; Knott, J.C.; Innis, P.C. Interplay between thermal and magnetic properties of polymer nanocomposites with superparamagnetic Fe3O4 nanoparticles. J. Magn. Magn. Mater. 2023, 579, 170859. [Google Scholar] [CrossRef]
- Gossuin, Y.; Vuong, Q.; Lascialfari, A. Comment on Structure-Correlated Magnetic Resonance Transverse Relaxivity Enhancement in Superparamagnetic Ensembles with Complex Anisotropy Landscape. Langmuir 2023, 39, 8935–8937. [Google Scholar] [CrossRef] [PubMed]
- Alzoubi, F.Y.; Abu Noqta, O.; Al Zoubi, T.; Al-Khateeb, H.M.; Alqadi, M.K.; Abuelsamen, A.; Makhadmeh, G.N. A Novel One-Pot Synthesis of PVP-Coated Iron Oxide Nanoparticles as Biocompatible Contrast Agents for Enhanced T2-Weighted MRI. J. Compos. Sci. 2023, 7, 131. [Google Scholar] [CrossRef]
- Majeed, S.; Rozi, N.A.B.M.; Danish, M.; Ibrahim, M.N.M.; Joel, E.L. In vitro apoptosis and molecular response of engineered green iron oxide nanoparticles with l-arginine in MDA-MB-231 breast cancer cells. J. Drug Deliv. Sci. Technol. 2023, 80, 104185. [Google Scholar] [CrossRef]
- Ou, A.; Wang, Y.; Zhang, J.; Huang, Y. Living Cells and Cell-Derived Vesicles: A Trojan Horse Technique for Brain Delivery. Pharmaceutics 2023, 15, 1257. [Google Scholar] [CrossRef]
- Hadrup, N.; Sørli, J.B.; Sharma, A.K. Pulmonary toxicity, genotoxicity, and carcinogenicity evaluation of molybdenum, lithium, and tungsten: A review. Toxicology 2022, 467, 153098. [Google Scholar] [CrossRef]
- Ansari, M.O.; Parveen, N.; Ahmad, M.F.; Wani, A.L.; Afrin, S.; Rahman, Y.; Jameel, S.; Khan, Y.A.; Siddique, H.R.; Tabish, M. Evaluation of DNA interaction, genotoxicity and oxidative stress induced by iron oxide nanoparticles both in vitroand in vivo: Attenuation by thymoquinone. Sci. Rep. 2019, 9, 6912. [Google Scholar] [CrossRef]
- El-Hamaky, A.M.; Hassan, A.A.; Wahba, A.K.; El, M.M. Influence of Copper and Zinc Nanoparticles on Genotyping Characterizations of Multi-Drug Resistance Genes for Some Calf Pathogens. Int. J. Vet. Sci. 2023, 12, 309–317. [Google Scholar]
- Ahamed, M.; Akhtar, M.J.; Khan, M.M.; Alhadlaq, H.A.; Alshamsan, A. Cobalt iron oxide nanoparticles induce cytotoxicity and regulate the apoptotic genes through ROS in human liver cells (HepG2). Colloids Surf. B 2016, 148, 665–673. [Google Scholar] [CrossRef]
- Ullah, A.; Al-Saeed, F.A.; Abduallah, A.M.; Ahmed, A.E.; Shahzad, A.; Amjad, N.; Ali, A.; Mostafa, M.S.; Hussain, R. Calcium Nanoparticles Induce Oxidative Stress in Erythrocytes, Neurotoxicity and Testicular Toxicity in Albino Rats. Pak. Vet. J. 2023, 43, 23–162. [Google Scholar]
- He, Y.; Li, J.; Chen, J.; Miao, X.; Li, G.; He, Q.; Xu, H.; Li, H.; Wei, Y. Cytotoxic effects of polystyrene nanoplastics with different surface functionalization on human HepG2 cells. Sci. Total Environ. 2020, 723, 138180. [Google Scholar] [CrossRef] [PubMed]
- Jahangirian, H.; Kalantari, K.; Izadiyan, Z.; Rafiee-Moghaddam, R.; Shameli, K.; Webster, T.J. A review of small molecules and drug delivery applications using gold and iron nanoparticles. Int. J. Nanomed. 2019, 2019, 1633–1657. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Li, Q.; Wang, C.; Hao, Y.; Yang, N.; Chen, M.; Ji, J.; Feng, L.; Liu, Z. Rational Design of Biomaterials to Potentiate Cancer Thermal Therapy. Chem. Rev. 2023, 123, 7326–7378. [Google Scholar] [CrossRef] [PubMed]
- Alarifi, S.; Ali, D.; Alkahtani, S.; Alhader, M. Iron oxide nanoparticles induce oxidative stress, DNA damage, and caspase activation in the human breast cancer cell line. Biol. Trace Elem. Res. 2014, 159, 416–424. [Google Scholar] [CrossRef]
- Srivastava, V.; Gusain, D.; Sharma, Y.C. Critical review on the toxicity of some widely used engineered nanoparticles. Ind. Eng. Chem. Res. 2015, 54, 6209–6233. [Google Scholar] [CrossRef]
- Ahamed, M.; A Alhadlaq, H.; Alam, J.; Khan, M.; Ali, D.; Alarafi, S. Iron oxide nanoparticle-induced oxidative stress and genotoxicity in human skin epithelial and lung epithelial cell lines. Curr. Pharm. Des. 2013, 19, 6681–6690. [Google Scholar] [CrossRef]
- Mortezaee, K.; Najafi, M.; Samadian, H.; Barabadi, H.; Azarnezhad, A.; Ahmadi, A. Redox interactions and genotoxicity of metal-based nanoparticles: A comprehensive review. Chem. Biol. Interact. 2019, 312, 108814. [Google Scholar] [CrossRef]
- Aziz, S.; Abdullah, S.; Anwar, H.; Latif, F.; Mustfa, W. Effect of Engineered Nickel Oxide Nanoparticles on Antioxidant Enzymes in Freshwater Fish, Labeo rohita. Pak. Vet. J. 2021, 41, 424–428. [Google Scholar] [CrossRef]
- Aziz, S.; Abdullah, S.; Anwar, H.; Latif, F. DNA Damage and Oxidative Stress in Economically Important Fish, Bighead Carp (Hypophthalmichthys nobilis) Exposed to Engineered Copper Oxide Nanoparticles. Pak. Vet. J. 2022, 42, 1–8. [Google Scholar]
- Samy, A.; Hassan, H.; Elsherif, H. Effect of nano zinc oxide and traditional zinc (oxide and sulphate) sources on performance, bone characteristics and physiological parameters of broiler chicks. Int. J. Vet. Sci. 2022, 11, 486–492. [Google Scholar]
- Arshad, J.M.; Raza, W.; Amin, N.; Nadeem, K.; Arshad, M.I.; Khan, M.A. Synthesis and characterization of cobalt ferrites as MRI contrast agent. Mater. Today Proc. 2021, 47, S50–S54. [Google Scholar] [CrossRef]
- Venkatesan, K.; Rajan Babu, D.; Kavya Bai, M.P.; Supriya, R.; Vidya, R.; Madeswaran, S.; Anandan, P.; Arivanandhan, M.; Hayakawa, Y. Structural and magnetic properties of cobalt-doped iron oxide nanoparticles prepared by solution combustion method for biomedical applications. Int. J. Nanomed. 2015, 10, 189–198. [Google Scholar]
- Ansari, S.M.; Sinha, B.B.; Pai, K.R.; Bhat, S.K.; Ma, Y.-R.; Sen, D.; Kolekar, Y.D.; Ramana, C. Controlled surface/interface structure and spin enabled superior properties and biocompatibility of cobalt ferrite nanoparticles. Appl. Surf. Sci. 2018, 459, 788–801. [Google Scholar] [CrossRef]
- Sharifi Dehsari, H.; Ksenofontov, V.; Möller, A.; Jakob, G.; Asadi, K. Determining magnetite/maghemite composition and core–shell nanostructure from magnetization curve for iron oxide nanoparticles. J. Phys. Chem. C 2018, 122, 28292–28301. [Google Scholar] [CrossRef]
- Balguri, S.P.; Adelli, G.R.; Majumdar, S. Topical ophthalmic lipid nanoparticle formulations (SLN, NLC) of indomethacin for delivery to the posterior segment ocular tissues. Eur. J. Pharm. 2016, 109, 224–235. [Google Scholar] [CrossRef]
- Sharma, A.; Tandon, A.; Tovey, J.C.; Gupta, R.; Robertson, J.D.; Fortune, J.A.; Klibanov, A.M.; Cowden, J.W.; Rieger, F.G.; Mohan, R.R. Polyethylenimine-conjugated gold nanoparticles: Gene transfer potential and low toxicity in the cornea. Nanomedicine NBM 2011, 7, 505–513. [Google Scholar] [CrossRef]
- Hussain, R.; Ali, F.; Rafique, A.; Ghaffar, A.; Jabeen, G.; Rafay, M.; Liaqat, S.; Khan, I.; Malik, R.; Khan, M.K. Exposure to Sub-Acute Concentrations of Glyphosate Induce Clinico-Hematological, Serum Biochemical and Genotoxic Damage in Adult Cockerels. Pak. Vet. J. 2019, 39. [Google Scholar]
- Ghaffar, A.; Hussain, R.; Noreen, S.; Abbas, G.; Chodhary, I.R.; Khan, A.; Ahmed, Z.; Khan, M.K.; Akram, K.; Ulhaq, M. Dose and time-related pathological and genotoxic studies on thiamethoxam in fresh water fish (Labeo rohita) in Pakistan. Pak. Vet. J. 2020, 40, 151–156. [Google Scholar] [CrossRef]
- Hussain, R.; Ghaffar, A.; Ali, H.M.; Abbas, R.Z.; Khan, J.A.; Khan, I.A.; Ahmad, I.; Iqbal, Z. Analysis of different toxic impacts of Fipronil on growth, hemato-biochemistry, protoplasm and reproduction in adult cockerels. Toxin Rev. 2018, 37, 294–303. [Google Scholar] [CrossRef]
- Khanna, L.; Verma, N.; Tripathi, S. Burgeoning tool of biomedical applications-Superparamagnetic nanoparticles. J. Alloys Compd. 2018, 752, 332–353. [Google Scholar] [CrossRef]
- Layne, K.A.; Dargan, P.I.; Archer, J.R.; Wood, D.M. Gadolinium deposition and the potential for toxicological sequelae—A literature review of issues surrounding gadolinium—based contrast agents. Br. J. Clin. Pharmacol. 2018, 84, 2522–2534. [Google Scholar] [CrossRef]
- Mohammed, L.; Gomaa, H.G.; Ragab, D.; Zhu, J. Magnetic nanoparticles for environmental and biomedical applications: A review. Particuology 2017, 30, 1–14. [Google Scholar] [CrossRef]
- Bohara, R.A.; Thorat, N.D.; Yadav, H.M.; Pawar, S.H. One-step synthesis of uniform and biocompatible amine functionalized cobalt ferrite nanoparticles: A potential carrier for biomedical applications. N. J. Chem. 2014, 38, 2979–2986. [Google Scholar] [CrossRef]
- Lima-Tenório, M.K.; Tenório-Neto, E.T.; Hechenleitner, A.A.W.; Fessi, H.; Pineda, E.A.G. CoFe2O4 and ZnFe2O4 nanoparticles: An overview about structure, properties, synthesis and biomedical applications. J. Colloid Sci. Biotechnol. 2016, 5, 45–54. [Google Scholar] [CrossRef]
- Amiri, S.; Shokrollahi, H. The role of cobalt ferrite magnetic nanoparticles in medical science. Mater. Sci. Eng. C 2013, 33, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Laurent, S.; Saei, A.A.; Behzadi, S.; Panahifar, A.; Mahmoudi, M. Superparamagnetic iron oxide nanoparticles for delivery of therapeutic agents: Opportunities and challenges. Drug Deliv. 2014, 11, 1449–1470. [Google Scholar] [CrossRef] [PubMed]
- Kandasamy, G.; Maity, D. Recent advances in superparamagnetic iron oxide nanoparticles (SPIONs) for in vitro and in vivo cancer nanotheranostics. Int. J. Pharm. 2015, 496, 191–218. [Google Scholar] [CrossRef] [PubMed]
- Thangamani, K.; Andal, N.M.; Kumar, E.R.; Saravanabhavan, M. Utilization of magnetic nano cobalt ferrite doped Capra aegagrus hircus dung activated carbon composite for the adsorption of anionic dyes. J. Environ. Chem. Eng. 2017, 5, 2820–2829. [Google Scholar] [CrossRef]
- Deepak, F.L.; Bañobre-López, M.; Carbó-Argibay, E.; Cerqueira, M.F.; Piñeiro-Redondo, Y.; Rivas, J.; Thompson, C.M.; Kamali, S.; Rodríguez-Abreu, C.; Kovnir, K. A systematic study of the structural and magnetic properties of Mn-, Co-, and Ni-doped colloidal magnetite nanoparticles. J. Phys. Chem. C 2015, 119, 11947–11957. [Google Scholar] [CrossRef]
- Abu-Abdeen, M.; Saber, O.; Mousa, E. Preparation and physical characterization of cobalt iron oxide magnetic nanoparticles loaded polyvinyl alcohol. J. Thermoplast. Compos. Mater 2023, 36, 201–217. [Google Scholar] [CrossRef]
- Ghayour, H.; Abdellahi, M.; Ozada, N.; Jabbrzare, S.; Khandan, A. Hyperthermia application of zinc doped nickel ferrite nanoparticles. J. Phys. Chem. Solids 2017, 111, 464–472. [Google Scholar] [CrossRef]
- Kour, S.; Jasrotia, R.; Kumari, N.; Singh, V.P.; Singh, P.; Kumar, R. A current review on synthesis and magnetic properties of pure and doped manganese ferrites. AIP Conf. Proc. 2022, 2357, 050007. [Google Scholar]
- Strijkers, G.; Mulder, W.; Van Heeswijk, R.; Frederik, P.; Bomans, P.; Magusin, P.; Nicolay, K. Relaxivity of liposomal paramagnetic MRI contrast agents. MAGMA 2005, 18, 186–192. [Google Scholar] [CrossRef]
- Cho, S.-J.; Jarrett, B.R.; Louie, A.Y.; Kauzlarich, S.M. Gold-coated iron nanoparticles: A novel magnetic resonance agent for T1 and T2 weighted imaging. Nanotechnology 2006, 17, 640. [Google Scholar] [CrossRef]
- Iqbal, M.Z.; Ma, X.; Chen, T.; Ren, W.; Xiang, L.; Wu, A. Silica-coated super-paramagnetic iron oxide nanoparticles (SPIONPs): A new type contrast agent of T 1 magnetic resonance imaging (MRI). J. Mater. Chem. B 2015, 3, 5172–5181. [Google Scholar] [CrossRef]
- Pillarisetti, S.; Uthaman, S.; Huh, K.M.; Koh, Y.S.; Lee, S.; Park, I.-K. Multimodal composite iron oxide nanoparticles for biomedical applications. Tissue Eng. Regen. Med. 2019, 16, 451–465. [Google Scholar] [CrossRef] [PubMed]
- Dunbar, L.; Sowden, R.J.; Trotter, K.D.; Taylor, M.K.; Smith, D.; Kennedy, A.R.; Spickett, C.M. Copper complexes as a source of redox active MRI contrast agents. BioMetals 2015, 28, 903–912. [Google Scholar] [CrossRef]
- Ding, N. Development and Evaluation of Cancer-Targeted Pre-Operative and Intra-Operative Dual-Imaging Probes Based on Metal Nanoparticles. Ph.D. Thesis, Kyoto University, Kyoto, Japan, 2019. [Google Scholar]
- Li, N.; Xia, T.; Nel, A.E. The role of oxidative stress in ambient particulate matter-induced lung diseases and its implications in the toxicity of engineered nanoparticles. Free Radical Biol. Med. 2008, 44, 1689–1699. [Google Scholar] [CrossRef]
- Ilinskaya, A.; Dobrovolskaia, M. Immunosuppressive and anti-inflammatory properties of engineered nanomaterials. Br. J. Pharmacol. 2014, 171, 3988–4000. [Google Scholar] [CrossRef]
- Serra, M.; Papakonstantinou, S.; Adamcova, M.; O’Brien, P.J. Veterinary and toxicological applications for the detection of cardiac injury using cardiac troponin. Vet. J. 2010, 185, 50–57. [Google Scholar] [CrossRef]
- Sayadi, M.H.; Mansouri, B.; Shahri, E.; Tyler, C.R.; Shekari, H.; Kharkan, J. Exposure effects of iron oxide nanoparticles and iron salts in blackfish (Capoeta fusca): Acute toxicity, bioaccumulation, depuration, and tissue histopathology. Chemosphere 2020, 247, 125900. [Google Scholar] [CrossRef] [PubMed]
- Malhotra, N.; Lee, J.-S.; Liman, R.A.D.; Ruallo, J.M.S.; Villaflores, O.B.; Ger, T.-R.; Hsiao, C.-D. Potential toxicity of iron oxide magnetic nanoparticles: A review. Molecules 2020, 25, 3159. [Google Scholar] [CrossRef] [PubMed]
- Lin, K.-I. NF-kappa B and the Regulation of Sindbis Virus-Induced Apoptosis; The Johns Hopkins University: Baltimore, MD, USA, 1998. [Google Scholar]
- Steinmetz-Späh, J. Studies on Anti-Inflammatory and Vasoactive Effects of MPGES-1 Inhibition; Karolinska Institutet: Stockholm, Sweden, 2023. [Google Scholar]
- Willhite, C.C.; Karyakina, N.A.; Yokel, R.A.; Yenugadhati, N.; Wisniewski, T.M.; Arnold, I.M.; Momoli, F.; Krewski, D. Systematic review of potential health risks posed by pharmaceutical, occupational and consumer exposures to metallic and nanoscale aluminum, aluminum oxides, aluminum hydroxide and its soluble salts. Crit. Rev. Toxicol. 2014, 44, 1–80. [Google Scholar] [CrossRef] [PubMed]
- Corot, C.; Robert, P.; Idée, J.-M.; Port, M. Recent advances in iron oxide nanocrystal technology for medical imaging. Adv. Drug Deliv. Rev. 2006, 58, 1471–1504. [Google Scholar] [CrossRef]
- Elshenawy, O.H.; El-Kadi, A.O. Modulation of aryl hydrocarbon receptor-regulated enzymes by trimethylarsine oxide in C57BL/6 mice: In vivo and in vitro studies. Toxicol. Lett. 2015, 238, 17–31. [Google Scholar] [CrossRef]
- Feng, S.; Cao, Z.; Wang, X. Role of aryl hydrocarbon receptor in cancer. Biochim. Biophys. Acta (BBA) Cancer Treat. Rev. 2013, 1836, 197–210. [Google Scholar] [CrossRef]
- Hernández-Aquino, E.; Muriel, P. Beneficial effects of naringenin in liver diseases: Molecular mechanisms. World J. Gastroenterol. 2018, 24, 1679. [Google Scholar] [CrossRef]
- Monteiro, A.; Afolabi, A.; Bilgili, E. Continuous production of drug nanoparticle suspensions via wet stirred media milling: A fresh look at the Rehbinder effect. Drug Dev. Ind. Pharm. 2013, 39, 266–283. [Google Scholar] [CrossRef]
- Ghalamizade Elyaderani, S.M.; Jafari, A. Investigation of interactions between silica nanoparticle, alkaline, and polymer in micromodel flooding for enhanced oil recovery. Energy Sources A Recovery Util. Environ. Eff. 2020, 42, 1–18. [Google Scholar] [CrossRef]
- Beck-Broichsitter, M.; Dalla-Bona, A.C.; Kissel, T.; Seeger, W.; Schmehl, T. Polymer nanoparticle-based controlled pulmonary drug delivery. Drug Deliv. Syst. 2014, 1141, 133–145. [Google Scholar]
- Hassanen, E.I.; Khalaf, A.A.; Tohamy, A.F.; Mohammed, E.R.; Farroh, K.Y. Toxicopathological and immunological studies on different concentrations of chitosan-coated silver nanoparticles in rats. Int. J. Nanomed. 2019, 14, 4723–4739. [Google Scholar] [CrossRef] [PubMed]
- Ghonimi, W.A.; Alferah, M.A.; Dahran, N.; El-Shetry, E.S. Hepatic and renal toxicity following the injection of copper oxide nanoparticles (CuO NPs) in mature male Westar rats: Histochemical and caspase 3 immunohistochemical reactivities. Environ. Sci. Pollut. Res. 2022, 29, 81923–81937. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Latif, H.M.; Shukry, M.; El Euony, O.I.; Mohamed Soliman, M.; Noreldin, A.E.; Ghetas, H.A.; Dawood, M.A.; Khallaf, M.A. Hazardous effects of SiO2 nanoparticles on liver and kidney functions, histopathology characteristics, and transcriptomic responses in Nile Tilapia (Oreochromis niloticus) Juveniles. Biology 2021, 10, 183. [Google Scholar] [CrossRef]
- Zhou, Y.; Peng, Z.; Seven, E.S.; Leblanc, R.M. Crossing the blood-brain barrier with nanoparticles. J. Control Release 2018, 270, 290–303. [Google Scholar] [CrossRef]
- Mishra, A.; Kumar, R.; Mishra, J.; Dutta, K.; Ahlawat, P.; Kumar, A.; Dhanasekaran, S.; Gupta, A.K.; Sinha, S.; Bishi, D.K. Strategies facilitating the permeation of nanoparticles through blood-brain barrier: An insight towards the development of brain-targeted drug delivery system. J. Drug Deliv. Sci. Technol. 2023, 86, 104694. [Google Scholar] [CrossRef]
- Ijaz, M.U.; Aziz, S.; Faheem, M.; Abbas, K.; Nasir, S.; Naz, H.; Ali, A.; Imran, M. Orientin Attenuates Cisplatin-Induced Renal Toxicity by Reducing Oxidative Stress and Inflammation. Pak. Vet. J. 2021, 41, 2074–7764. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khan, M.S.; Buzdar, S.A.; Hussain, R.; Alouffi, A.; Aleem, M.T.; Farhab, M.; Javid, M.A.; Akhtar, R.W.; Khan, I.; Almutairi, M.M. Cobalt Iron Oxide (CoFe2O4) Nanoparticles Induced Toxicity in Rabbits. Vet. Sci. 2023, 10, 514. https://doi.org/10.3390/vetsci10080514
Khan MS, Buzdar SA, Hussain R, Alouffi A, Aleem MT, Farhab M, Javid MA, Akhtar RW, Khan I, Almutairi MM. Cobalt Iron Oxide (CoFe2O4) Nanoparticles Induced Toxicity in Rabbits. Veterinary Sciences. 2023; 10(8):514. https://doi.org/10.3390/vetsci10080514
Chicago/Turabian StyleKhan, Muhammad Shahid, Saeed Ahmad Buzdar, Riaz Hussain, Abdulaziz Alouffi, Muhammad Tahir Aleem, Muhammad Farhab, Muhammad Arshad Javid, Rana Waseem Akhtar, Iahtasham Khan, and Mashal M. Almutairi. 2023. "Cobalt Iron Oxide (CoFe2O4) Nanoparticles Induced Toxicity in Rabbits" Veterinary Sciences 10, no. 8: 514. https://doi.org/10.3390/vetsci10080514
APA StyleKhan, M. S., Buzdar, S. A., Hussain, R., Alouffi, A., Aleem, M. T., Farhab, M., Javid, M. A., Akhtar, R. W., Khan, I., & Almutairi, M. M. (2023). Cobalt Iron Oxide (CoFe2O4) Nanoparticles Induced Toxicity in Rabbits. Veterinary Sciences, 10(8), 514. https://doi.org/10.3390/vetsci10080514







