Assisting the Learning of Clinical Reasoning by Veterinary Medical Learners with a Case Example
Abstract
Simple Summary
Abstract
1. Introduction
2. Background to Learning Clinical Reasoning by Veterinary Medical Learners
| Stage | Activity/ Element | Example of Veterinary Medical Learner’s Synthesis of Information |
|---|---|---|
| 1. Consider client ± patient situation | NA | Mrs Jane Do is an experienced dairy farmer and has presented Margery, a 5-year-old Holstein cow with recurrent mastitis in both rear quarters. Margery is otherwise ‘healthy’. Mrs. Do is very concerned about Margery as she is used as a ‘donor cow’ for embryo transfer. |
| 2. Collect data | Presenting problem | Recurrent mastitis in both rear quarters. |
| Health interview | Margery is a homegrown cow that had a previous bout of mastitis about 3 weeks ago in both rear quarters. As Mrs Do has an on-farm milk culturing system, she tried to isolate the causative pathogen/s, but the culture result was negative. She had no other recorded health problems throughout Margery’s life. Mrs. Do has purchased 10 cows from a producer who was selling their business, just over 3 months ago. The sale was due to the old shed and high herd-level somatic cell cows that were not controllable. Mrs. Do has purchased only cows that had high genetic merit, but no other history was available for these cows. The current milking herd consists of approximately 600 milking and 200 dry cows, in addition to 300 pregnant heifers and 2 bulls. Cows are milked twice daily through a rotary milking shed with 60 units. The milking machine is thoroughly washed after every milking cycle. Herd testing is carried out every month. The number of cows with increased individual cow somatic cell counts in the last two herd tests seems high. In the last two months, the bulk tank milk somatic cell counts and number of cows with clinical mastitis have started to increase in a progressive fashion, in comparison to historical data. Most cows with mastitis had signs in two or more quarters. By plating on selective media, the applicable on-farm culturing system allows for the identification of common mastitis pathogens from the groups of coliforms, staphylococci, and streptococci. No growth has been detected using the on-farm culture system. Additionally, there were three replacement neonatal calves with fever, head tilt, severe obtundancy, and poor response to antimicrobial treatment. These calves were euthanized on animal welfare grounds. | |
| Various examination steps | Environment and husbandry—no abnormalities detected (NAD). Margery’s clinical examination findings—Bright and alert. Except for the changes in the milk composition from both rear quarters, no other abnormal findings. Milk composition from both rear quarters—watery with small flecks in the first approximately 10 strips becoming milk-like with small flecks thereafter. No signs of increased heat, pain, or swelling of the affected quarters. | |
| Ancillary examination techniques/tests | California Mastitis Test (CMT) results—Both rear quarters: thick gel (+++). Front left quarter: light gel formation (+). Front right quarter: no gel (−). Double, aseptically collected milk samples were submitted for common bacterial pathogens culture from all quarters (individual sampling per quarter). Culture results—no growth after 72 h. Resubmission and request to culture for Mycoplasma spp. resulted in both rear quarters having heavy Mycoplasma spp. growth. The front left quarter also resulted in a light Mycoplasma spp. growth. | |
| 3. Analyze the data and 4. Identify problem/s ± Issue/s | Review data/Problem representation | Mrs Jane Do is an experienced dairy farmer and has presented Margery, a 5-year-old valuable Holstein cow, with recurrent mastitis in both rear quarters that have not grown common mastitis pathogens using the on-farm mastitis culturing system. Margery’s mastitis is of a mild character. No other abnormalities were detected in her, but the herd-level incidence of clinical mastitis and somatic cell counts progressively increased over the last two months. |
| Review context | Mrs Do mentioned that Margery is used as a ‘donor cow’, meaning she is quite valuable and genetically superior. The client is concerned about Margery’s animal welfare and progressively rising somatic cell counts coupled with an increasing number of clinical cases at the herd level. Valuable cow for the client. | |
| Problem identification | Altered secretion from both rear quarters resulted in positive CMT. Culture identified Mycoplasma spp. as a causative pathogen. Increasing incidence of clinical mastitis. Increasing bulk tank somatic cell counts. Calves with suspected otitis, non-responsive to antimicrobial treatment. | |
| Recall knowledge | Exemplars/Illness scripts/Prototypes/Semantic qualifiers Mastitis is an inflammation of the mammary gland/s that is most commonly caused by bacterial pathogens. Based on the main characteristics of the causative pathogen, mastitis can be environmental or contagious. Based on the presentation, mastitis can be mild, moderate, severe, or subclinical (Figure 1). Diagnosis of clinical mastitis is based on the presence of clinical signs. Diagnosis of subclinical mastitis is based on the use of various tests detecting the pathogen or changes in the milk composition. Etiologic diagnosis requires identification of the causative pathogen. | |
| Interpretation | Recurrent mastitis in both rear quarters with no growth on traditional culture but positive on Mycoplasma spp. | |
| Discrimination | ‘Margery does not present with generalized malaise.’ | |
| Relating | ‘Although Margery has mild mastitis, her overall demeanor does not seem to be affected.’ | |
| Inferring | ‘Margery’s mastitis is likely associated with the increased incidence of clinical mastitis on the enterprise, and to the progressively raising bulk tank somatic cell count. Based on the presented data, it seems that we are dealing with a contagious mastitis.’ | |
| Matching | Mastitis in multiple quarters, often of a recurrent nature, that may be associated with otitis media and respiratory disease in other herd members is common with Mycoplasma spp. as a causative pathogen. | |
| Predicting | Even without treatment, Margery’s mastitis is likely to apparently self-cure in a few days, but the real cure is much lower. | |
| 5. Establish mutually agreed goals | NA | ‘Margery’s wellbeing is marginally affected. The most likely diagnosis is Mycoplasma mastitis which is difficult or impossible to treat. As this form of mastitis is contagious, we agreed that the best course of action is to minimize the spread to uninfected cows by introducing milking segregation. However, if Margery’s mastitis does not self-cure in 3–5 days, we may consider drying her off or culling her. Are we all in agreement?’ |
| 6. Take action | NA | In this encounter, due to the contagious nature of the causative pathogen, the best course of action is milking segregation of all cows and milking them in the following order: (1) cows with low somatic cell count and no signs of clinical mastitis; (2) cows with high somatic cell count but no signs of clinical mastitis; and (3) cows with signs of clinical mastitis (milk discarded). Cows suspected of having subclinical and clinical mastitis will be regularly sampled and tested by culture or PCR for the pathogen. Additionally, all 10 points of the National Mastitis Council should be followed in detail [5]. To prevent the spread to calves, milk fed to calves must be pasteurized. Alternatively, calves can be fed with milk replacers. |
| 7. Evaluate the outcome | NA | Margery’s mastitis apparently disappeared in two days. As her condition is non-treatable and self-cure rates for Mycoplasma mastitis are lower than for most forms of mastitis, the client may consider culling. Yet, her genetic superiority may prevent culling. If Margery does not self-cure, she may need to be used only as a ‘donor’ cow before culling and milking is not advisable. Additionally, Mycoplasma mastitis is of a contagious nature and does not respond well to dry cow treatment. This makes all cows infected with Mycoplasma spp. being a continuous source of infection for uninfected cows. |
| 8. Reflection and new learning | NA | Mrs Do mentioned that Margery is used as a ‘donor cow’, meaning she is quite valuable and genetically superior. Culling as an option is unlikely to be easily acceptable by the client. The risk to other cows should be considered and explained to the client. The client should be aware that the eradication of the pathogen from the enterprise is not easy, and may take a few years of meticulous work, coupled with cooperative labor working with cattle. |
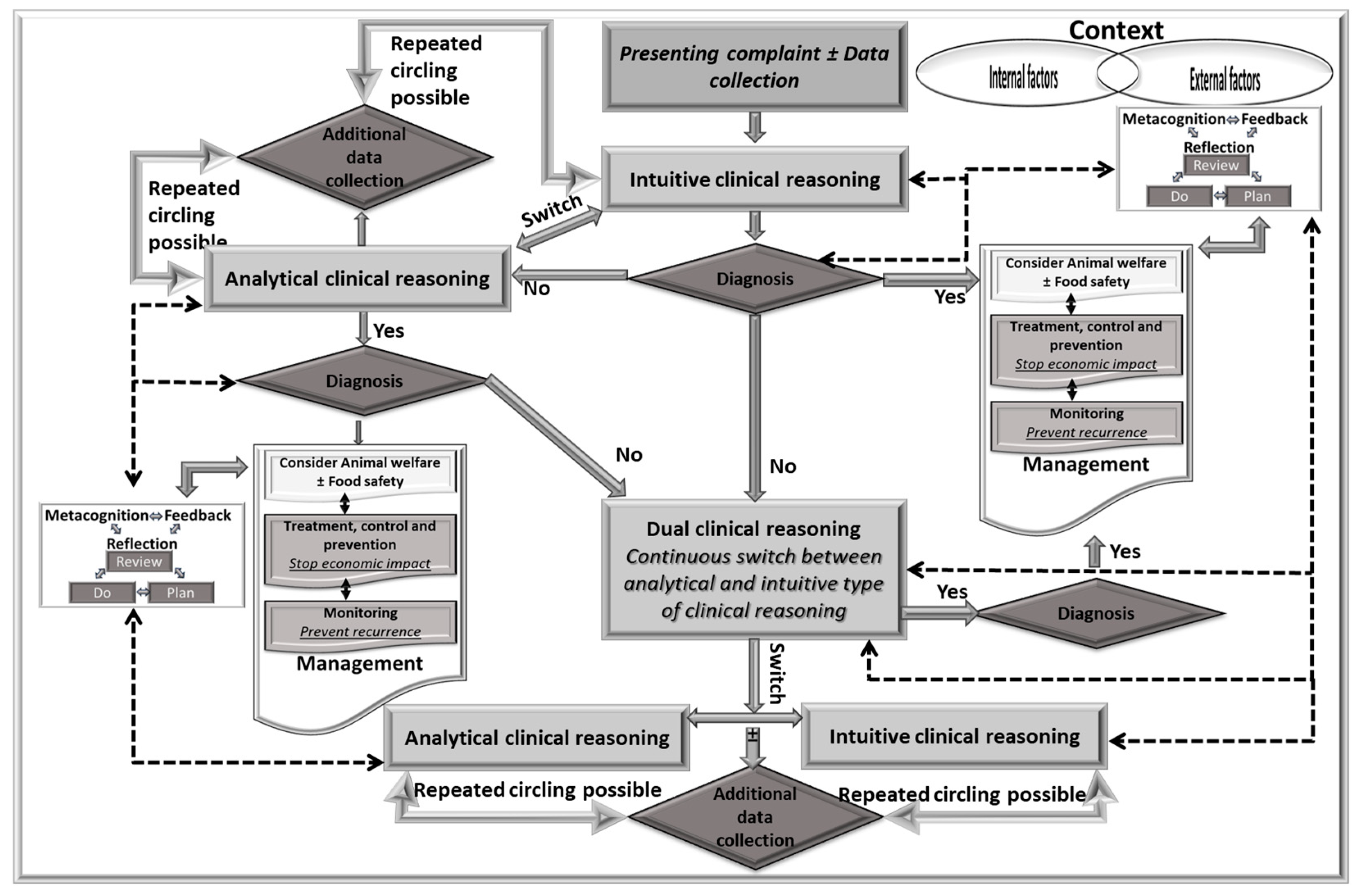
3. Variability in the Use of Types of Clinical Reasoning in the Clinical Practice
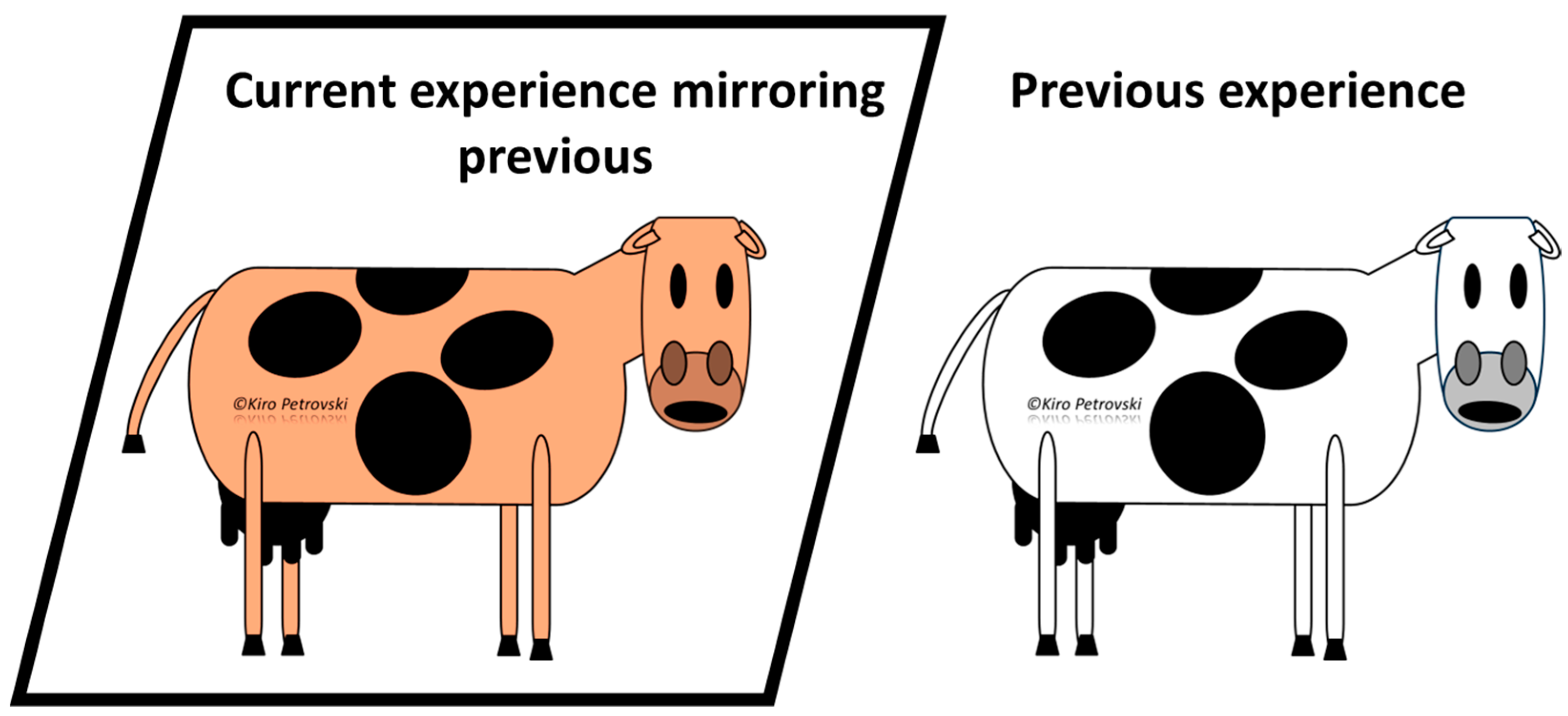
4. Awareness of the Clinical Reasoning Concepts
5. Learning to Collect Clinically Relevant Data
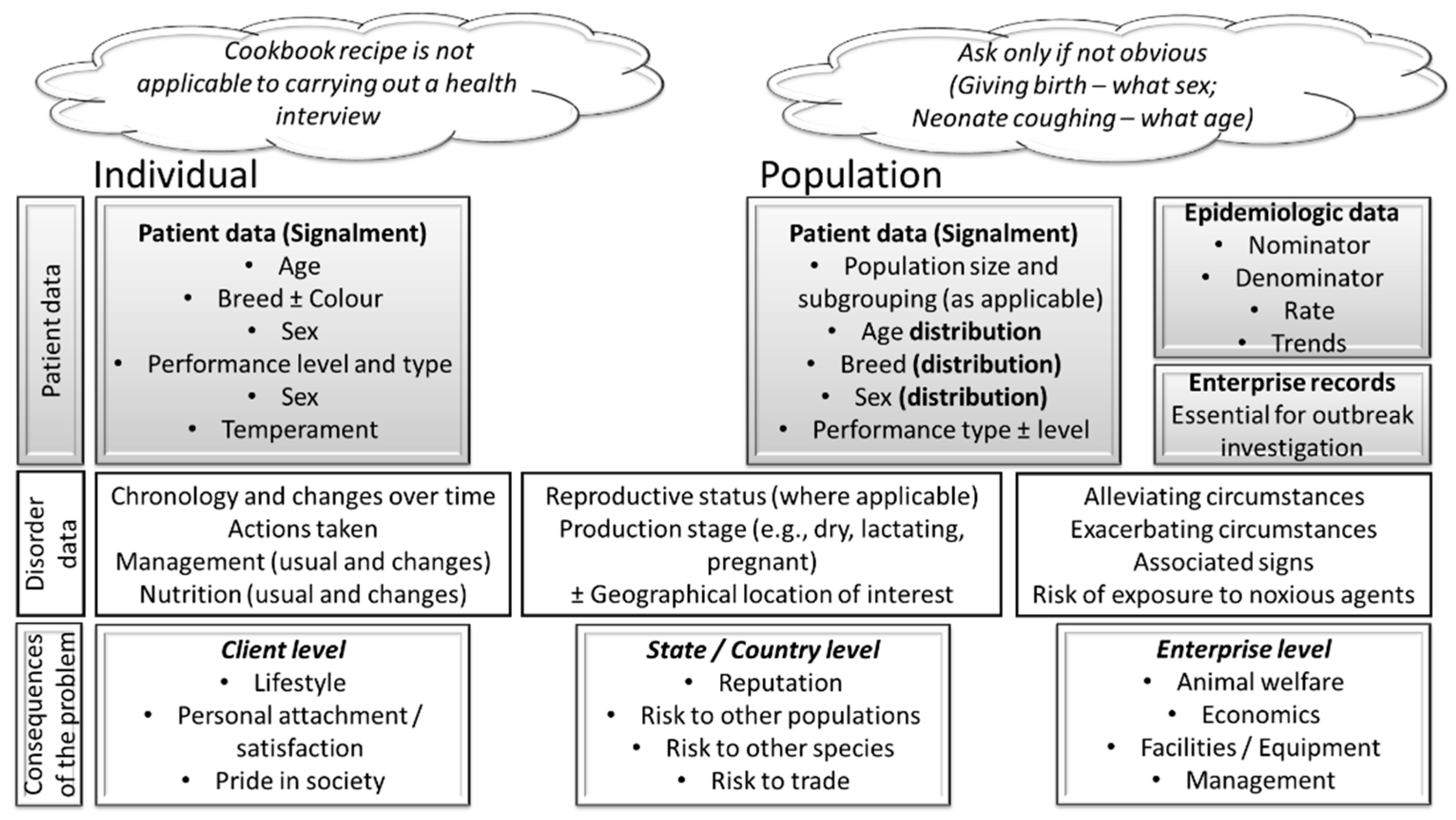
5.1. Learning to Conduct Informative Health Interview
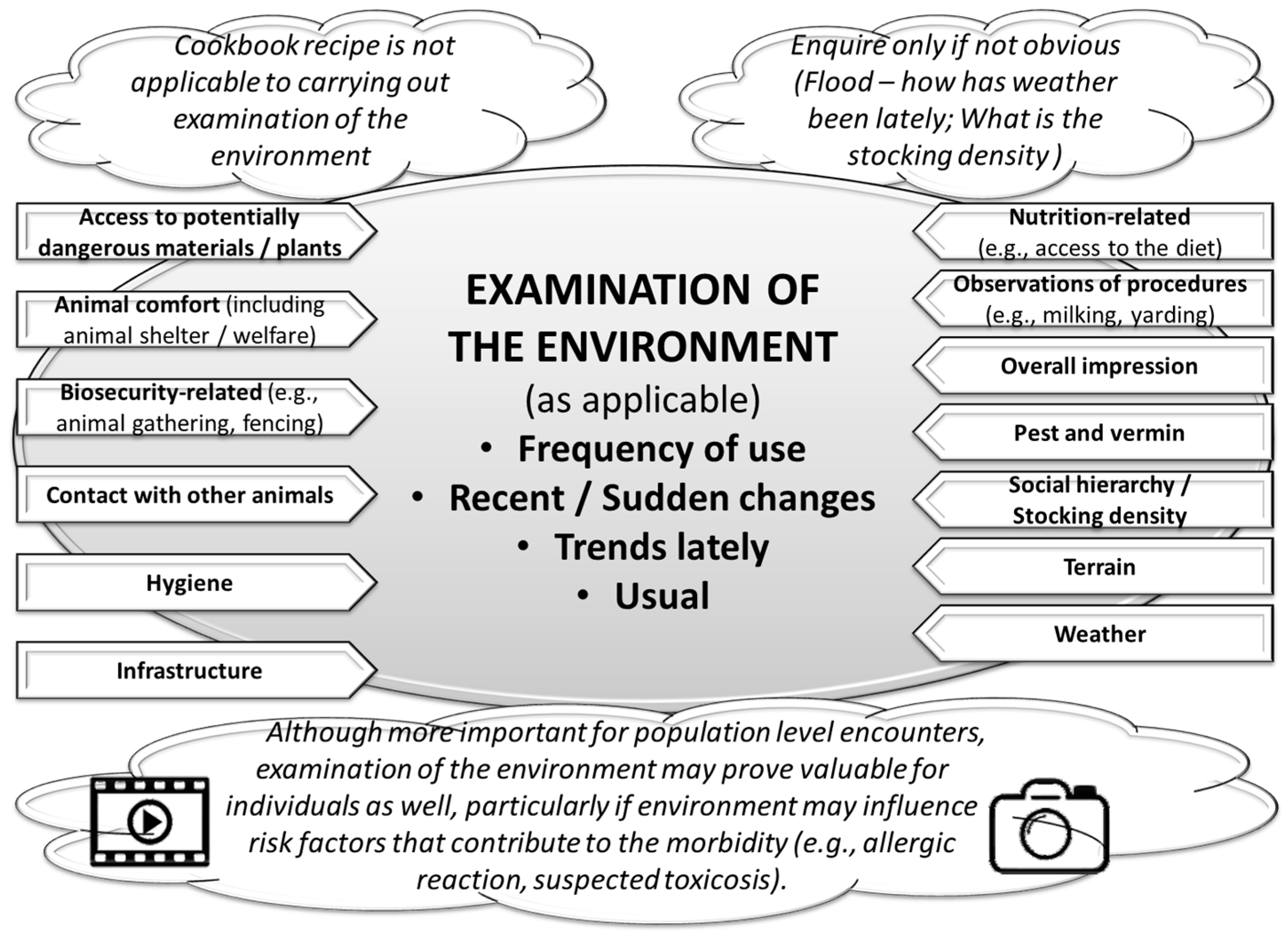
5.2. Learning to Conduct an Informative Examination of the Environment
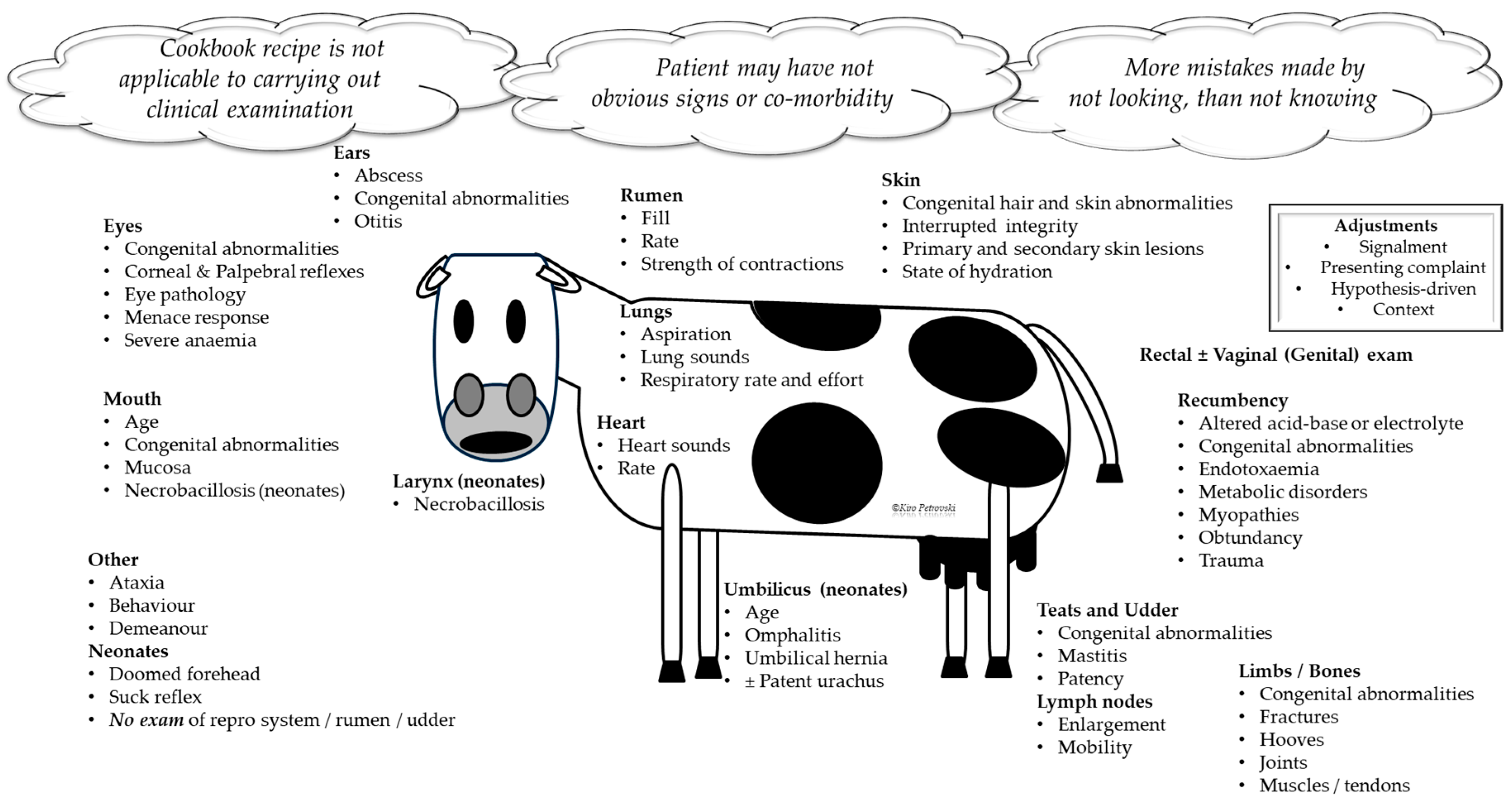
5.3. Learning to Conduct an Informative Clinical Examination
5.4. Learning to Conduct an Informative Post-Mortem Examination
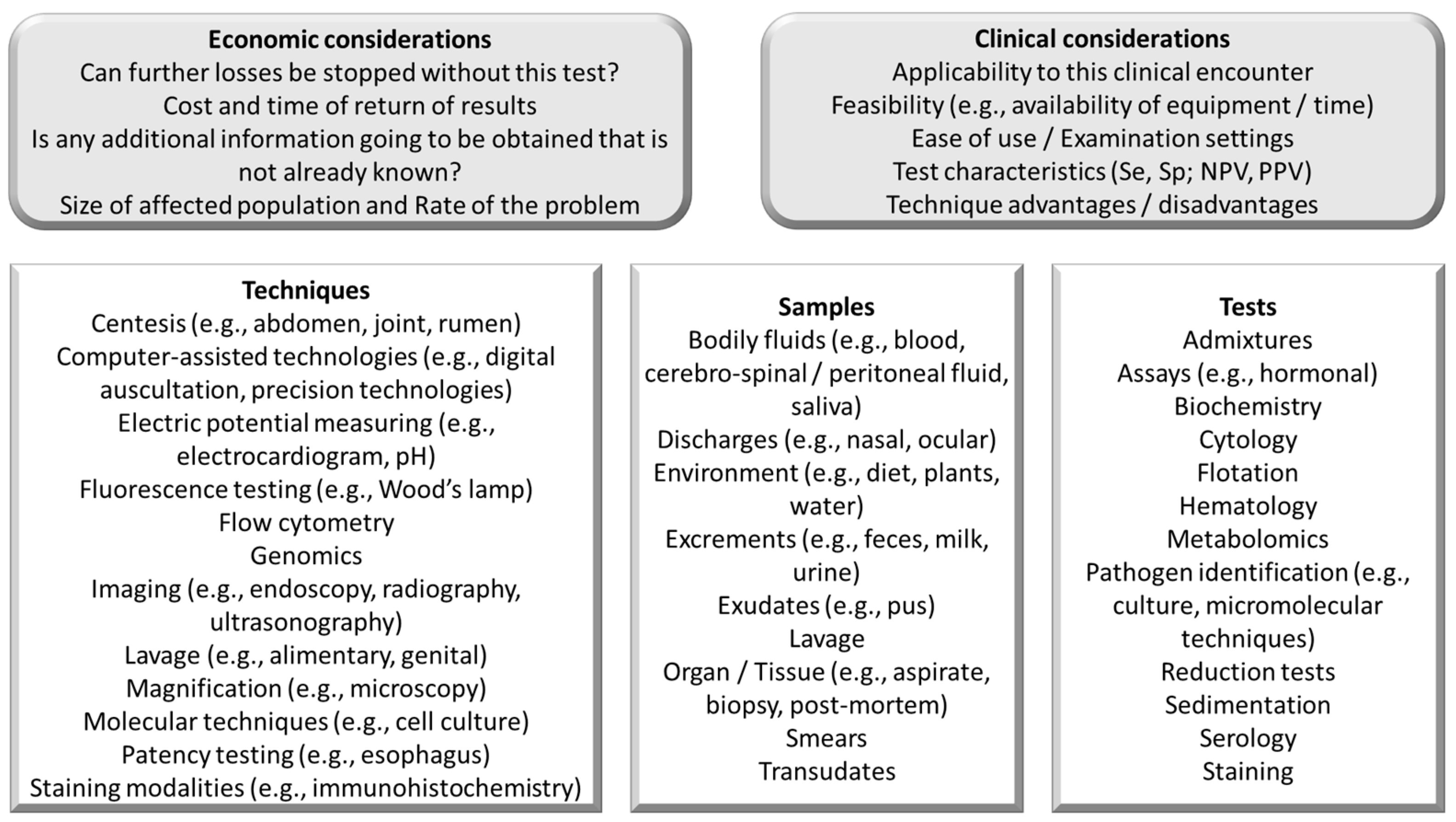
5.5. Learning to Select Informative Ancillary Examination Techniques
6. Learning to Analyze Collected Data, Including Identification of Problems ± Issues
6.1. Learning How to Organize and Cluster Collected Data
6.2. Learning How to Prepare Effective Problem Representation
6.3. Learning How to Prepare an Effective List of Differentials/Management Approaches
6.4. Learning How to Refine the List of Differentials/Management Approaches
7. Learning How to Establish Shared Decision-Making, Including ‘Take Action’
8. Learning How to Evaluate Outcomes
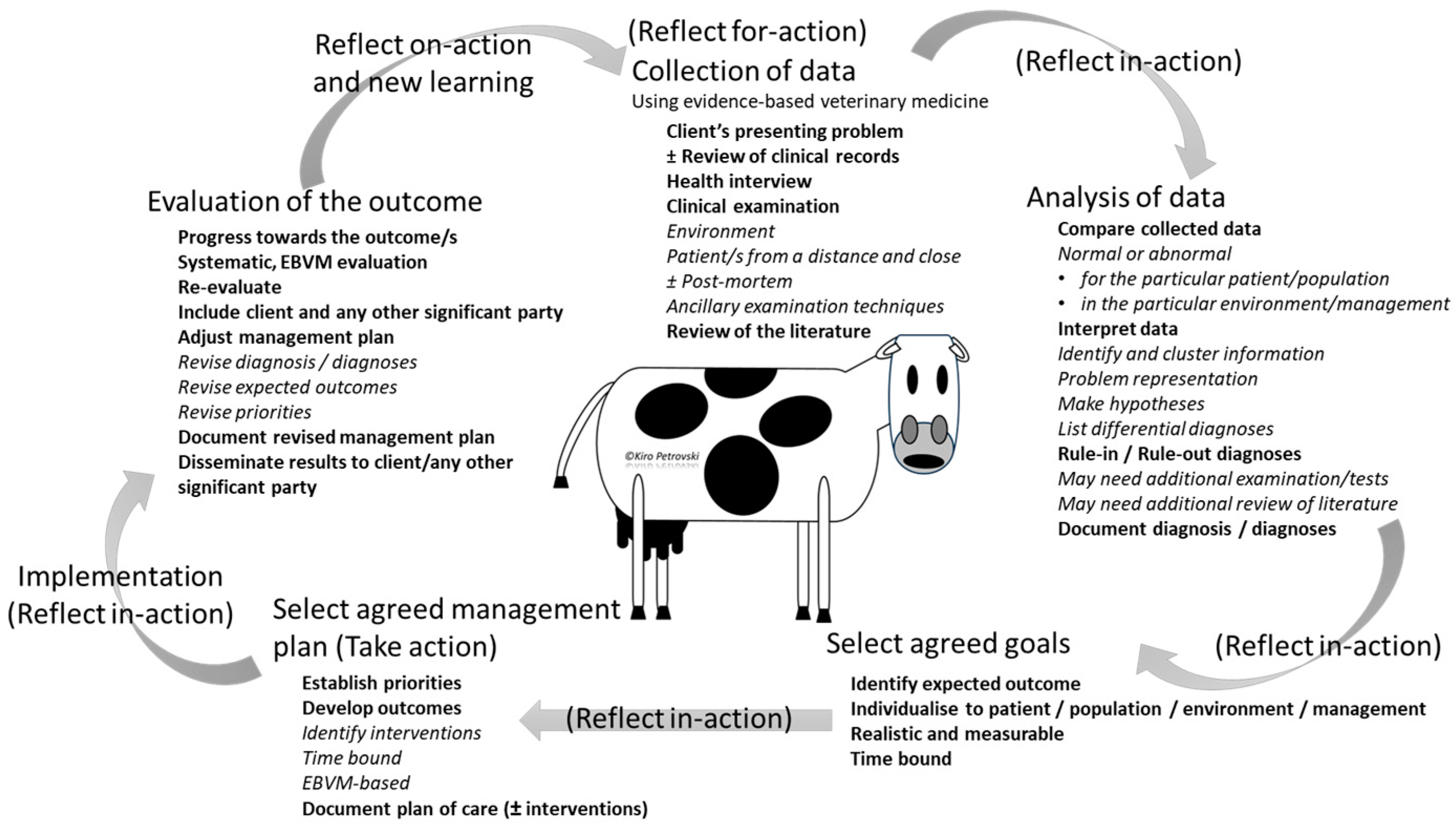
9. Learning How to Reflect -for-, -in-, and -on-Action in a Clinical Encounter and New Learning
10. Discussion
11. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Glossary
| Term | Meaning |
| Analytical type of clinical reasoning | This is based on being more deliberate, explicit, purposeful, rational, and slow, and focuses on hypotheses generation and deductive reasoning that is closer to the cognitive processes associated with problem solving. Common synonyms include ‘Deductive, Deliberate, Rational, Rule-governed or System/Type 2 clinical reasoning’. |
| Clinical encounter | Any physical or virtual contact with a veterinary patient and client (e.g., owner, employee of an enterprise) with a primary responsibility to carry out clinical assessment or activity. |
| Clinical instructor | In addition to the regular veterinary practitioner’s duties, a clinical instructor should fulfil roles of assessor, facilitator, mentor, preceptor, role-model, supervisor, and teacher of veterinary learners in a clinical teaching environment. It may include any of the following: Apprentice/intern in the upper years, Resident, Veterinary educator/teacher, Veterinary practitioner. |
| Clinical reasoning | The cognitive process interjected with unconscious operations during which a learner or practitioner collects information (clinical and context), processes it, comes to an understanding of the problem presented during a clinical encounter, and prepares a management plan, followed by evaluation of the outcome and self-reflection. Common synonyms: Clinical/Diagnostic/Medical: Acumen/Cognition/Critical thinking/Decision-making/Information processing/Judgment/Problem solving/Rationale/Reasoning. |
| Complete data collection | Checking for the presence of clinical abnormalities, risk factors, and context using a systematic and exhaustive approach. |
| Context | A complex interaction of factors (including but not limited to affective/physical state, client, encounter, environment, finances, patient, and social environment) having effect on the clinical reasoning competence of the learner. |
| Deep learning | Learner aims for mastery of essential academic content; thinking critically and solving complex problems; working collaboratively and communicating effectively; having an academic mindset; and being empowered through self-directed learning. |
| Data clustering | A discovery process usually based on unsupervised deep learning that partitions collected data into clinically relevant clusters/groups with high similarity or distinct properties (e.g., by etiology, anatomic structure, epidemiology, or pathophysiology). |
| Dual type of clinical reasoning | Clinical reasoning that utilizes concurrently the analytical and intuitive types. Common synonyms: Dual-/Mixed—process clinical reasoning/theory. |
| Five microskills model | An instructor-centered model of clinical teaching: (1) Get a commitment; (2) Probe for supporting evidence; (3) Teach general rules; (4) Reinforce what was done well; and (5) Correct mistakes. An additional stage is the ‘Debrief’. |
| Hypothesis-driven data collection | A combination of data collection and clinical reasoning resulting in early generation of hypotheses and resultant data collection is used to rank competing differentials/management approaches, resulting in limited but focused data collection. |
| Illness script | An organized mental summary of the knowledge of a disorder. Common synonyms: Medical scripts, Schema. |
| Intuitive type of clinical reasoning | Based more on cognitive short-cuts (e.g., heuristics) than real intuitive (gestalt effect) processes. Therefore, even the intuitive type of clinical reasoning is not equal to the real meaning of intuitive (‘judgment made quickly and without apparent effort’). Common synonyms: Experiential, ‘Gut feeling’, Inductive, Non-analytical, Tacit, or System/Type 1 clinical reasoning. |
| Metacognition | Critical awareness of one’s thought processes and learning, and an understanding of the patterns of thinking and learning (‘thinking about thinking’). |
| Problem representation | A one-sentence summary that highlights the defining features of a clinical encounter. Common synonym: summary statement. |
| Reflection | Metacognitive process that may occur before, during or after an encounter with a purpose of developing deeper understanding of the encounter and self ± the team to inform the ongoing and/or future actions, behaviors, and encounters. |
| Reflection for action | A process of self-evaluation of the action to happen, including planning for action and doing the action, anticipating the unexpected, and planning and executing adjustments from before, during and after the encounter. |
| Reflection in action | A process of self-evaluation of the action as it happens resulting in ongoing adjustments during the encounter. |
| Reflection on action | A process of self-evaluation of the action after it has been completed, planning for adjustment in future encounters. |
| Semantic qualifiers | Abstractions expressed using medical rather than lay terminology. Generally, they exist as divergent pairs that aid in comparing and contrasting the hypotheses. Examples of semantic qualifiers include acute or chronic, being affected by XX or previously healthy, bilateral or unilateral, constant or exacerbated by XX, continuous or intermittent, copious or scant, dull or sharp, frequent or rare, generalized or localized, left or right, mild or severe, etc. |
| Team-based learning | A method in which solving an authentic clinical case using clinical reasoning skills. Particularly useful in developing basic science concepts through peer-learning approach (learning occurs within a team but also between teams when activity carried out concurrently with more than one team) and activation of prior knowledge. Learner-centered approach to learning. |
| Work-based learning | An educational method that immerses the learners in the workplace. Common synonyms: Experiential learning; Exposure to practice. |
| Working memory | One of the executive functions of the brain associated with the retention of a small amount of information in a readily accessible form necessary for comprehension, learning, and reasoning |
References
- Neill, C.; Vinten, C.; Maddison, J. Use of inductive, Problem-Based clinical reasoning enhances diagnostic accuracy in final-year veterinary students. J. Vet. Med. Educ. 2020, 47, 506–515. [Google Scholar] [CrossRef] [PubMed]
- Ruczynski, L.I.; van de Pol, M.H.; Schouwenberg, B.J.; Laan, R.F.; Fluit, C.R. Learning clinical reasoning in the workplace: A student perspective. BMC Med. Educ. 2022, 22, 19. [Google Scholar] [CrossRef]
- Carr, A.N.M.; Kirkwood, R.N.; Petrovski, K.R. Effective veterinary clinical teaching in a variety of teaching settings. Vet. Sci. 2022, 9, 17. [Google Scholar] [CrossRef] [PubMed]
- Carr, A.N.; Ferlini Agne, G.; Kirkwood, R.N.; Petrovski, K.R. Teaching clinical reasoning to veterinary medical learners with a case example. Encyclopedia 2024, 4, 753–775. [Google Scholar] [CrossRef]
- National Mastitis Council. Recommended Mastitis Control Program. Available online: https://mdanderson.libanswers.com/faq/26219 (accessed on 15 May 2024).
- Vinten, C.E.K. Clinical reasoning in veterinary practice. Vet. Evid. 2020, 5. [Google Scholar] [CrossRef]
- Koufidis, C.; Manninen, K.; Nieminen, J.; Wohlin, M.; Silén, C. Unravelling the polyphony in clinical reasoning research in medical education. J. Eval. Clin. Pract. 2021, 27, 438–450. [Google Scholar] [CrossRef]
- Safi, S.; Hemmati, P.; Shirazi-Beheshtiha, S.H.; Aslani, F.; Taghdiri, M.R.; Abadiyeh, R.; Tsai, T.-C. Developing a clinical presentation curriculum in veterinary education: A cognitive perspective. Comp. Clin. Pathol. 2012, 21, 1521–1526. [Google Scholar] [CrossRef]
- Linn, A.; Khaw, C.; Kildea, H.; Tonkin, A. Clinical reasoning: A guide to improving teaching and practice. Aust. Fam. Physician 2012, 41, 18–20. [Google Scholar]
- Tomlin, J.L.; Pead, M.J.; May, S.A. Attitudes of veterinary faculty to the assessment of clinical reasoning using extended matching questions. J. Vet. Med. Educ. 2008, 35, 622–630. [Google Scholar] [CrossRef]
- Amey, L.; Donald, K.J.; Teodorczuk, A. Teaching clinical reasoning to medical students. Br. J. Hosp. Med. 2017, 78, 399–401. [Google Scholar] [CrossRef]
- Custers, E.J.F.M. Thirty years of illness scripts: Theoretical origins and practical applications. Med. Teach. 2015, 37, 457–462. [Google Scholar] [CrossRef] [PubMed]
- Croskerry, P. A universal model of diagnostic reasoning. Acad. Med. 2009, 84, 1022–1028. [Google Scholar] [CrossRef]
- Cutrer, W.B.; Sullivan, W.M.; Fleming, A.E. Educational strategies for improving clinical reasoning. Curr. Probl. Pediatr. Adolesc. Health Care 2013, 43, 248–257. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, A.; Stragnell, S.; Jester, P. Guide for reflection using the clinical judgment model. J. Nurs. Educ. 2007, 46, 513–516. [Google Scholar] [CrossRef] [PubMed]
- Wainwright, S.F.; Shepard, K.F.; Harman, L.B.; Stephens, J. Novice and experienced physical therapist clinicians: A comparison of how reflection is used to inform the clinical decision-making process. Phys. Ther. 2010, 90, 75–88. [Google Scholar] [CrossRef]
- Schmidt, H.G.; Mamede, S. How to improve the teaching of clinical reasoning: A narrative review and a proposal. Med. Educ. 2015, 49, 961–973. [Google Scholar] [CrossRef]
- Cohen, A.; Sur, M.; Weisse, M.; Moffett, K.; Lancaster, J.; Saggio, R.; Singhal, G.; Thammasitboon, S. Teaching diagnostic reasoning to faculty using an assessment for learning tool: Training the trainer. MedEdPORTAL 2020, 16, 10938. [Google Scholar] [CrossRef]
- Cooper, N.; Bartlett, M.; Gay, S.; Hammond, A.; Lillicrap, M.; Matthan, J.; Singh, M. Consensus statement on the content of clinical reasoning curricula in undergraduate medical education. Med. Teach. 2021, 43, 152–159. [Google Scholar] [CrossRef]
- Harasym, P.H.; Tsai, T.-C.; Hemmati, P. Current trends in developing medical students’ critical thinking abilities. Kaohsiung J. Med. Sci. 2008, 24, 341–355. [Google Scholar] [CrossRef]
- Humm, K.R.; May, S.A. Clinical reasoning by veterinary students in the first-opinion setting: Is it encouraged? Is it practiced? J. Vet. Med. Educ. 2018, 45, 156–162. [Google Scholar] [CrossRef]
- Jessee, M.A. Pursuing improvement in clinical reasoning: The integrated clinical education theory. J. Nurs. Educ. 2018, 57, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Pinnock, R.; Welch, P. Learning clinical reasoning. J. Paediatr. Child Health 2014, 50, 253–257. [Google Scholar] [CrossRef] [PubMed]
- Carr, A.N.; Kirkwood, R.N.; Petrovski, K.R. The art and science of consultations in bovine medicine: Use of Modified Calgary–Cambridge Guides, Part 2. Maced. Vet. Rev. 2023, 46, 5–16. [Google Scholar] [CrossRef]
- Petrovski, K.; McArthur, M. The art and science of consultations in bovine medicine: Use of modified Calgary–Cambridge guides. Maced. Vet. Rev. 2015, 38, 137–147. [Google Scholar] [CrossRef]
- Carr, A.N.; Kirkwood, R.N.; Petrovski, K.R. Practical use of the (Observer)—Reporter—Interpreter—Manager—Expert ((O)RIME) framework in veterinary clinical teaching with a clinical example. Encyclopedia 2022, 2, 1666–1677. [Google Scholar] [CrossRef]
- Graber, M.L. Educational strategies to reduce diagnostic error: Can you teach this stuff? Adv. Health Sci. Educ. Theory Pract. 2009, 14, 63–69. [Google Scholar] [CrossRef]
- Bellezza, F.S. Mnemonic methods to enhance storage and retrieval. In Memory; Elsevier: Amsterdam, The Netherlands, 1996; pp. 345–380. [Google Scholar]
- Petrovski, K.; Williamson, N.; Lopez-Villalobos, N.; Parkinson, T.; Tucker, I. Culture results from milk samples submitted to veterinary diagnostic laboratories from August 2003 to December 2006 in New Zealand. N. Z. Vet. J. 2011, 59, 317–322. [Google Scholar] [CrossRef]
- Graber, M.L.; Kissam, S.; Payne, V.L.; Meyer, A.N.D.; Sorensen, A.; Lenfestey, N.; Tant, E.; Henriksen, K.; LaBresh, K.; Singh, H. Cognitive interventions to reduce diagnostic error: A narrative review. BMJ Qual. Saf. 2012, 21, 535–557. [Google Scholar] [CrossRef]
- Ander, D.S.; Wallenstein, J.; Abramson, J.L.; Click, L.; Shayne, P. Reporter-Interpreter-Manager-Educator (RIME) descriptive ratings as and evaluation tool in an emergency medicine clerkship. J. Emerg. Med. 2012, 43, 720–727. [Google Scholar] [CrossRef]
- Aranda, L.; Mena-Rodríguez, E.; Rubio, L. Basic skills in higher education: An analysis of attributed importance. Front. Psychol. 2022, 13, 752248. [Google Scholar] [CrossRef]
- Fleming, A.; Cutrer, W.; Reimschisel, T.; Gigante, J. You too can teach clinical reasoning. Pediatrics 2012, 130, 795–797. [Google Scholar] [CrossRef] [PubMed]
- Lubarsky, S.; Dory, V.; Audétat, M.C.; Custers, E.; Charlin, B. Using script theory to cultivate illness script formation and clinical reasoning in health professions education. Can. Med. Educ. J. 2015, 6, e61–e70. [Google Scholar] [CrossRef]
- Chang, R.W.; Bordage, G.; Connell, K.J. The importance of early problem representation during case presentations. Acad. Med. 1998, 73, S109–S111. [Google Scholar] [CrossRef] [PubMed]
- Audétat, M.C.; Laurin, S.; Dory, V.; Charlin, B.; Nendaz, M.R. Diagnosis and management of clinical reasoning difficulties: Part I. Clinical reasoning supervision and educational diagnosis. Med. Teach. 2017, 39, 792–796. [Google Scholar] [CrossRef]
- Weinstein, A.; Gupta, S.; Pinto-Powell, R.; Jackson, J.; Appel, J.; Roussel, D.; Daniel, M. Diagnosing and remediating clinical reasoning difficulties: A faculty development workshop. MedEdPORTAL 2017, 13, 10650. [Google Scholar] [CrossRef]
- Desy, J.; Busche, K.; Cusano, R.; Veale, P.; Coderre, S.; McLaughlin, K. How teachers can help learners build storage and retrieval strength. Med. Teach. 2018, 40, 407–413. [Google Scholar] [CrossRef]
- Mohd Tambeh, S.N.; Yaman, M.N. Clinical reasoning training sessions for health educators—A scoping review. J. Taibah Univ. Med. Sci. 2023, 18, 1480–1492. [Google Scholar] [CrossRef]
- Ramaekers, S.P.J.; Van Beukelen, P.; Kremer, W.D.J.; Van Keulen, H.; Pilot, A. Instructional model for training competence in solving clinical problems. J. Vet. Med. Educ. 2011, 38, 360–372. [Google Scholar] [CrossRef] [PubMed]
- Larsen, D.P.; London, D.A.; Emke, A.R. Using reflection to influence practice: Student perceptions of daily reflection in clinical education. Perspect. Med. Educ. 2016, 5, 285–291. [Google Scholar] [CrossRef]
- Farnsworth, C.C.; Herman, J.D.; Osterstock, J.B.; Porterpan, B.L.; Willard, M.D.; Hooper, R.N.; Roussel, A.J., Jr.; Schmitz, D.G.; Fogelberg, K.; Kochevar, D.T. Assessment of clinical reasoning skills in veterinary students prior to and after the clinical year of training. J. Am. Vet. Med. Assoc. 2008, 233, 879–882. [Google Scholar] [CrossRef]
- May, S.A. Clinical reasoning and Case-Based Decision Making: The fundamental challenge to veterinary educators. J. Vet. Med. Educ. 2013, 40, 200–209. [Google Scholar] [CrossRef] [PubMed]
- Evans, J.S.B.T. Intuition and reasoning: A Dual-Process perspective. Psychol. Inq. 2010, 21, 313–326. [Google Scholar] [CrossRef]
- Bordage, G. Why did I miss the diagnosis? Some cognitive explanations and educational implications. Acad. Med. 1999, 74, S138–S143. [Google Scholar] [CrossRef] [PubMed]
- Rebhun, W.C. Diseases of Dairy Cattle; Williams & Wilkins: Philadelphia, PA, USA, 1995. [Google Scholar]
- Almomani, E.; Sullivan, J.; Saadeh, O.; Mustafa, E.; Pattison, N.; Alinier, G. Reflective learning conversations model for simulation debriefing: A co-design process and development innovation. BMC Med. Educ. 2023, 23, 837. [Google Scholar] [CrossRef]
- Brown, B.; Holt-Macey, S.; Martin, B.; Skau, K.; Vogt, E.M. Developing the reflective practitioner: What, so what, now what. Curr. Pharm. Teach. Learn. 2015, 7, 705–715. [Google Scholar] [CrossRef]
- Byermoen, K.R.; Brembo, E.A.; Egilsdottir, H.Ö.; Heyn, L.G.; Moen, A.; Eide, H. Reflection on actions: Identifying facilitators of and barriers to using physical assessment in clinical practice. Nurse Educ. Pract. 2021, 50, 102913. [Google Scholar] [CrossRef]
- Casapulla, S.; Longenecker, R.; Beverly, E.A. The value of clinical jazz: Teaching critical reflection on, in, and toward action. Fam. Med. 2016, 48, 377–380. [Google Scholar]
- Ferraro, J.M. Reflective Practice and Professional Development; ERIC Digest: Washington, DC, USA, 2000. [Google Scholar]
- Munby, H. Reflection-in-action and reflection-on-action. Curr. Issues Educ. 1989, 9, 31–42. [Google Scholar] [CrossRef]
- Ong, K. Reflection for action in the medical field. Reflective Pract. 2011, 12, 145–149. [Google Scholar] [CrossRef]
- Sandars, J. The use of reflection in medical education: AMEE Guide No. 44. Med. Teach. 2009, 31, 685–695. [Google Scholar] [CrossRef]
- Schon, D.A. The Reflective Practitioner: How Professionals Think in Action; Basic Books: New York, NY, USA, 1984; Volume 5126. [Google Scholar]
- Kolb, D.A. Experiential Learning: Experience as the Source of Learning and Development; FT Press: Upper Saddle River, NJ, USA, 2014. [Google Scholar]
- Carr, A.N.; Kirkwood, R.N.; Petrovski, K.R. Using the five-microskills method in veterinary medicine clinical teaching. Vet. Sci. 2021, 8, 89. [Google Scholar] [CrossRef] [PubMed]
- Sharp, P.; Baillie, S.; Parkes, R.S.V.; Janicke, H.; Kinnison, T.; Routh, J.; Muca, E.; Forrest, N. Setting Up and Running Online Communities of Practice (CoPs) for Veterinary Educators. J. Vet. Med. Educ. 2024, e20230042. [Google Scholar] [CrossRef]
- Boshuizen, H.P.; Schmidt, H.G. On the role of biomedical knowledge in clinical reasoning by experts, intermediates and novices. Cogn. Sci. 1992, 16, 153–184. [Google Scholar] [CrossRef]
- Young, M.; Thomas, A.; Gordon, D.; Gruppen, L.; Lubarsky, S.; Rencic, J.; Ballard, T.; Holmboe, E.; Da Silva, A.; Ratcliffe, T. The terminology of clinical reasoning in health professions education: Implications and considerations. Med. Teach. 2019, 41, 1277–1284. [Google Scholar] [CrossRef] [PubMed]
- Cornell, K.K.; Kopcha, M. Client-veterinarian communication: Skills for client centered dialogue and shared decision making. Vet. Clin. Small Anim. Pract. 2007, 37, 37–47. [Google Scholar] [CrossRef]
- McDermott, M.P.; Tischler, V.A.; Cobb, M.A.; Robbé, I.J.; Dean, R.S. Veterinarian–client communication skills: Current state, relevance, and opportunities for improvement. J. Vet. Med. Educ. 2015, 42, 305–314. [Google Scholar] [CrossRef]


| OLDCARTS | OPQRST | SAMPLE | SOCRATES |
|---|---|---|---|
| Onset Location Duration Characteristics Aggravation and Alleviation Related signs and syndromes/Risk factors Treatment tried Severity | Onset Provocation Quality Rate and Risk factors Severity Time/Chronology | Signs and Syndromes Allergy/Autoimmune Medication Past medical history Last oral intake and Diet Events leading to the illness/problem | Signalment and Site Onset Character Rate and Risk factors Alleviation Time/Chronology Exacerbation Severity |
| Type of Data | Description | Examples from the Example Encounter | |
|---|---|---|---|
| Extraneous | Information not related to the disorder/management approach/problem/syndrome | Number of cattle on the enterprise. | |
| Intrinsic (Description: Information related to the disorder/management approach/problem/syndrome) | Non-specific | Information with very little to no effect on the tested hypothesis but it is related to the encounter | Positive California Mastitis Test in the clinically affected quarters. |
| Specific | Relevant information, with a significant effect on the likelihood of the tested hypothesis | At individual patient level: Presence of multiquarter clinical mastitis; and At population level: Presence of otitis in calves. Progressively increasing bulk milk somatic cell count. | |
| Semi-specific | Relevant information with little effect on the likelihood of the tested hypothesis | Mild mastitis with small flecks in the secretion. | |
| Positive | Making a tested hypothesis very likely | Finding the pathogen in culture | |
| Negative | Making a tested hypothesis very unlikely | Yielding negative culture in the on-farm culture system. | |
| Step 1 | Step 2 | Step 3 | |
|---|---|---|---|
| List of Context/Clinical Data Collected | Data Categorization | Clinically Relevant Data Clustering | |
| Category | Information | Indicative of | |
| Experienced dairy farmer | Extraneous | Margery, 5-year-old, Holstein cow | Signalment |
| Margery, 5-year-old, Holstein cow | Signalment | Margery is valuable Used as an embryo donor | |
| Recurrent mastitis | Specific | ||
| Changes in milk composition but otherwise healthy | Specific | Recurrent mastitis | Involvement of the mammary gland |
| A previous bout of mastitis 3 weeks ago | Specific | Changes in milk composition but otherwise healthy | |
| Both rear quarters affected. No other recorded health problems | Specific | A previous bout of mastitis 3 weeks ago | |
| Purchased 10 cows from another producer (old shed and increasing somatic cell count) | Extraneous | ||
| The current herd consists of 600 milking cows | Non-specific | ||
| Other cows with clinical mastitis and 3 replacement neonatal calves with fever and head tilt, euthanized | Specific | ||
| NAD Environment | Extraneous | ||
| NAD husbandry (Milking machine thoroughly washed after each cycle) | Extraneous | Margery is bright and alert | No generalized malaise; No fever |
| Margery is bright and alert | Non-specific | TPR + mentation NAD | |
| No increased heat, pain, or swelling in the affected quarters | Non-specific | No signs of pain | |
| Milk composition from both rear quarters: watery with small flecks | Specific | Immunized against common BRD pathogens | |
| Mrs Do concerned with Margery’s welfare | Extraneous | The current herd consists of 600 milking cows | Likely to be contagious |
| Margery is valuable Used as an embryo donor | Signalment | Other cows with clinical mastitis and 3 replacement neonatal calves with fever and head tilt, euthanized | |
| Purchased 10 cows from another producer (old shed and increasing somatic cell count) | |||
| Skill | Description—Part of the Reflective Practice Characterized by … |
|---|---|
| Self-analysis | Reflective self-assessment of the performance versus goals for the encounter. |
| Self-awareness | Acceptance of constructive criticism and/or recognition of self-limitations. |
| Self-confidence | an ability to speak in an awkward situation. |
| Self-efficacy | Spending time to self-reflect and avoid/change/enhance actions in ongoing and/or future encounters. |
| Self-esteem | Believing in yourself. |
| Self-evaluation/monitoring | Recheck every decision to be, or already made, with the aim of adjusting it. |
| Self-regulation | Controlling the behavior and expressions of the affective state. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferlini Agne, G.; Carr, A.N.; Kirkwood, R.N.; Petrovski, K.R. Assisting the Learning of Clinical Reasoning by Veterinary Medical Learners with a Case Example. Vet. Sci. 2024, 11, 433. https://doi.org/10.3390/vetsci11090433
Ferlini Agne G, Carr AN, Kirkwood RN, Petrovski KR. Assisting the Learning of Clinical Reasoning by Veterinary Medical Learners with a Case Example. Veterinary Sciences. 2024; 11(9):433. https://doi.org/10.3390/vetsci11090433
Chicago/Turabian StyleFerlini Agne, Gustavo, Amanda (Mandi) Nicole Carr, Roy Neville Kirkwood, and Kiro Risto Petrovski. 2024. "Assisting the Learning of Clinical Reasoning by Veterinary Medical Learners with a Case Example" Veterinary Sciences 11, no. 9: 433. https://doi.org/10.3390/vetsci11090433
APA StyleFerlini Agne, G., Carr, A. N., Kirkwood, R. N., & Petrovski, K. R. (2024). Assisting the Learning of Clinical Reasoning by Veterinary Medical Learners with a Case Example. Veterinary Sciences, 11(9), 433. https://doi.org/10.3390/vetsci11090433








