The Presence of Rabies Virus-Neutralizing Antibody in Wild Boars (Sus scrofa), a Non-Target Bait Vaccine Animal in Korea
Abstract
:1. Introduction
2. Materials and Methods
2.1. Serum Samples
2.2. Fluorescent Antibody Virus Neutralization Test
2.3. Statistical Analysis
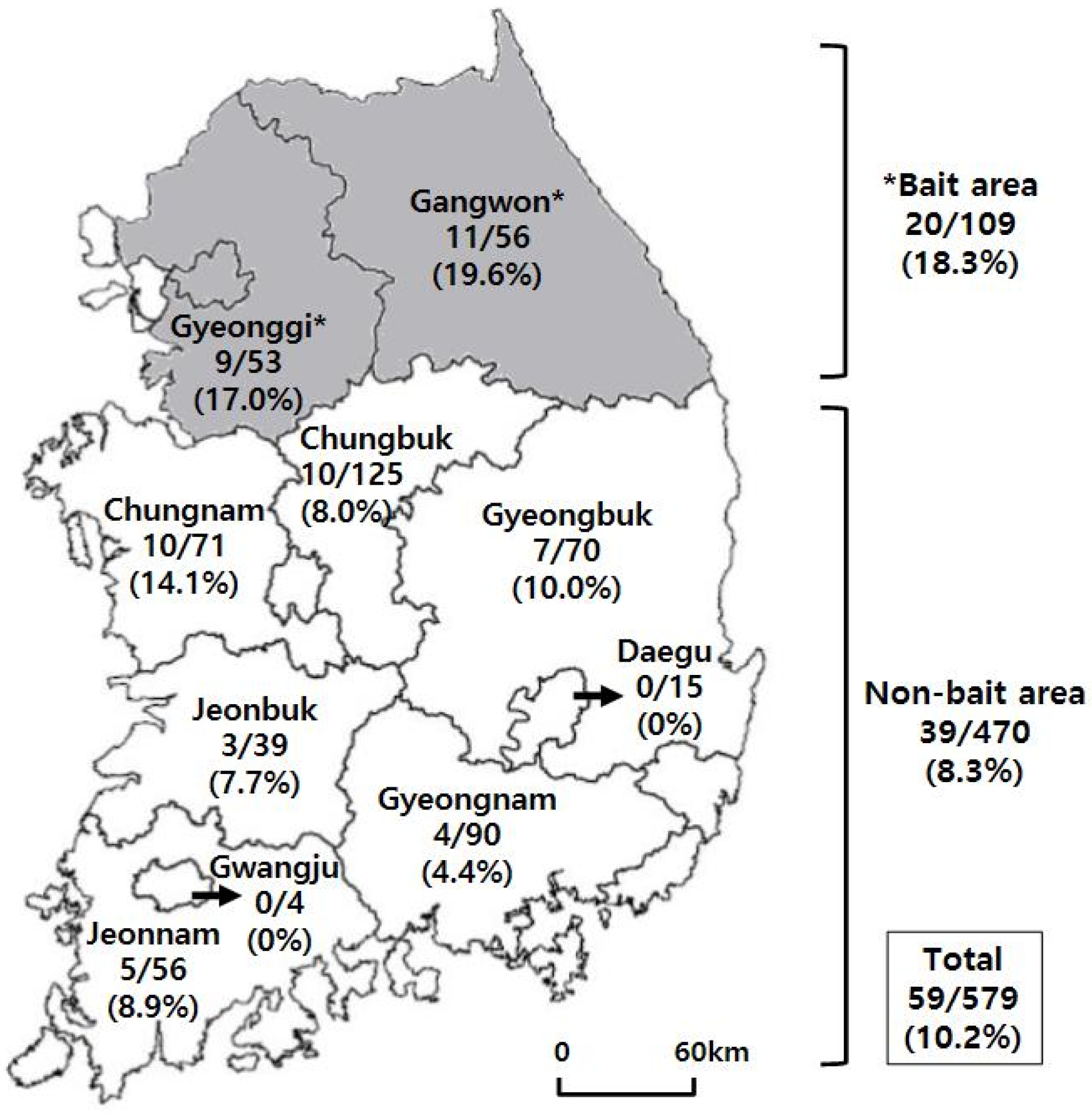
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Cliquet, F.; Robardet, E.; Must, K.; Laine, M.; Peik, K.; Picard-Meyer, E.; Guiot, A.L.; Niin, E. Eliminating rabies in Estonia. PLoS Negl. Trop. Dis. 2012, 6, e1535. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Selhorst, T.; Müller, T.; Schwermer, H.; Ziller, M.; Schlüter, H.; Breitenmoser, U.; Mueller, U.; Brochier, B.; Pastoret, P.P.; Mutinelli, F. Use of an area index to retrospectively analyze the elimination of fox rabies in European countries. Environ. Manage. 2005, 35, 292–302. [Google Scholar] [CrossRef] [PubMed]
- Yang, D.K.; Kim, H.H.; Lee, K.K.; Yoo, J.Y.; Seomun, H.; Cho, I.S. Mass vaccination has led to the elimination of rabies since 2014 in South Korea. Clin. Exp. Vaccine Res. 2017, 6, 111–119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mähl, P.; Cliquet, F.; Guiot, A.L.; Niin, E.; Fournials, E.; Saint-Jean, N.; Aubert, M.; Rupprecht, C.E.; Gueguen, S. Twenty year experience of the oral rabies vaccine SAG2 in wildlife: a global review. Vet. Res. 2014, 45, 77. [Google Scholar] [CrossRef]
- Müller, T.F.; Schröder, R.; Wysocki, P.; Mettenleiter, T.C.; Freuling, C.M. Spatio-temporal use of oral rabies vaccines in fox rabies elimination programmes in Europe. PLoS Negl. Trop. Dis. 2015, 9, e0003953. [Google Scholar] [CrossRef] [Green Version]
- Maki, J.; Guiot, A.L.; Aubert, M.; Brochier, B.; Cliquet, F.; Hanlon, C.A.; King, R.; Oertli, E.H.; Rupprecht, C.E.; Schumacher, C.; et al. Oral vaccination of wildlife using a vaccinia-rabies-glycoprotein recombinant virus vaccine (RABORAL V-RG®): A global review. Vet. Res. 2017, 48, 57. [Google Scholar] [CrossRef] [Green Version]
- Brown, L.J.; Rosatte, R.C.; Fehlner-Gardiner, C.; Taylor, J.S.; Davies, J.C.; Donovan, D. Immune response and protection in raccoons (Procyon lotor) following consumption of baits containing ONRAB®, a human adenovirus rabies glycoprotein recombinant vaccine. J. Wildl. Dis. 2012, 48, 1010–1020. [Google Scholar] [CrossRef] [Green Version]
- Yang, D.K.; Kim, H.H.; Cho, I.S. Strategies to maintain Korea’s animal rabies non-occurrence status. Clin. Exp. Vaccine Res. 2018, 7, 87–92. [Google Scholar] [CrossRef]
- Control of wildlife rabies using RABORAL V-RG®. Boehringer Ingelheim Animal Health (2019). Available online: http://www.raboral.com/sites/raboral/files/docs/Raboral-Brochure-2019.05-rev06_WEB.pdf (accessed on 12 June 2020).
- Vengušt, G.; Hostnik, P.; Cerovšek, M.; Cilenšek, P.; Malovrh, T. Presence of antibodies against rabies in wild boars. Acta Vet. Hung. 2011, 59, 149–154. [Google Scholar] [CrossRef]
- Vos, A.; Müller, T.; Selhorst, T.; Schuster, P.; Neubert, A.; Schlüter, H. Optimising spring oral vaccination campaigns of foxes against rabies. Dtsch. Tierarztl. Wochenschr. 2001, 108, 55–59. [Google Scholar]
- Dascalu, M.A.; Wasniewski, M.; Picard-Meyer, E.; Servat, A.; Daraban Bocaneti, F.; Tanase, O.I.; Velescu, E.; Cliquet, F. Detection of rabies antibodies in wild boars in north-east Romania by a rabies ELISA test. BMC Vet. Res. 2019, 15, 466. [Google Scholar] [CrossRef] [PubMed]
- Artois, M.; Charlton, K.M.; Tolson, N.D.; Casey, G.A.; Knowles, M.K.; Campbell, J.B. Vaccinia recombinant virus expressing the rabies virus glycoprotein: safety and efficacy trials in Canadian wildlife. Can. J. Vet. Res. 1990, 54, 504–507. [Google Scholar] [PubMed]
- Brochier, B.; Blancou, J.; Thomas, I.; Languet, B.; Artois, M.; Kieny, M.P.; Lecocq, J.P.; Costy, F.; Desmettre, P.; Chappuis, G.; et al. Use of recombinant vaccinia-rabies glycoprotein virus for oral vaccination of wildlife against rabies: innocuity to several non-target bait consuming species. J. Wildl. Dis. 1989, 25, 540–547. [Google Scholar] [CrossRef]
- Oh, S.Y.; Kim, S.A.; Kim, J.Y.; Yoo, H.S.; Lee, K.K.; Shin, N.S. Detection of antibodies against the rabies virus in Korean raccoon dogs (Nyctereutes procyonoides koreensis). J. Zoo Wildl. Med. 2012, 43, 174–176. [Google Scholar] [CrossRef] [PubMed]
- Yang, D.K.; Kim, H.H.; Lee, E.J.; Kim, J.T.; Ahn, S. Rabies immune status in raccoon dogs residing in area where rabies bait vaccine has distributed. Clin. Exp. Vaccine Res. 2019, 8, 132–135. [Google Scholar] [CrossRef] [PubMed]
- World Organization for Animal Health (OIE). Chapter 3.1.17. Rabies (Infection with rabies virus and other lyssaviruses). In Manual of diagnostic tests and vaccines for terrestrial animals; OIE: Paris, France, 2018; pp. 591–594. [Google Scholar]
- Cho, Y.S. 2017 Wildlife Survey; National Institute of Biological Resources: Incheon, Korea, 2017; pp. 13–27. (In Korean) [Google Scholar]
- Fletcher, W.O.; Creekmore, T.E.; Smith, M.S.; Nettles, V.F. A field trial to determine the feasibility of delivering oral vaccines to wild swine. J. Wildl. Dis. 1990, 26, 502–510. [Google Scholar] [CrossRef] [PubMed]
- Brochier, B.; Thomas, I.; Iokem, A.; Ginter, A.; Kalpers, J.; Paquot, A.; Costy, F.; Pastoret, P.P. A field trial in Belgium to control fox rabies by oral immunisation. Vet. Rec. 1988, 123, 618–621. [Google Scholar]
- Paquot, A.; Brochier, B.; Thomas, I.; Pastoret, P.P. Vaccination campaigns of the red fox (Vulpes vulpes) against rabies in Belgium: ingestion of vaccine baits by the red deer (Cervus elaphus), the roe deer (Capreolus capreolus) and the wild boar (Sus scrofa). Ann. Med. Vet. 1988, 132, 679–702. [Google Scholar]
- Berentsen, A.R.; Johnson, S.R.; Gilbert, A.T.; VerCauteren, K.C. Exposure to rabies in small Indian mongooses (Herpestes auropunctatus) from two regions in Puerto Rico. J. Wildl. Dis. 2015, 51, 896–900. [Google Scholar] [CrossRef] [Green Version]
- Gilbert, A.; Johnson, S.; Walker, N.; Wickham, C.; Beath, A.; VerCauteren, K. Efficacy of Ontario Rabies Vaccine Baits (ONRAB) against rabies infection in raccoons. Vaccine 2018, 36, 4919–4926. [Google Scholar] [CrossRef]
- Winkler, W.G.; Jenkins, S.R. Raccoon rabies. In The Natural History of Rabies, 2nd ed.; Baer, G.M., Ed.; CRC Press: Boca Raton, FL, USA, 1991; pp. 325–340. [Google Scholar]
- Slate, D.; Chipman, R.B.; Algeo, T.P.; Mills, S.A.; Nelson, K.M.; Croson, C.K.; Dubovi, E.J.; Vercauteren, K.; Renshaw, R.W.; Atwood, T.; et al. Safety and immunogenicity of Ontario Rabies Vaccine Bait (ONRAB) in the first us field trial in raccoons (Procyon lotor). J. Wildl. Dis. 2014, 50, 582–595. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, D.K.; Lee, S.H.; Kim, H.H.; Kim, J.T.; Ahn, S.; Cho, I.S. Detection of viral infections in wild Korean raccoon dogs (Nyctereutes procyonoides koreensis). Korean J. Vet. Res. 2017, 57, 209–214. [Google Scholar]
- Massei, G.; Genov, P.V. The environmental impact of wild boar. Galemys 2004, 16, 135–145. [Google Scholar]
- Jo, Y.S.; Baccus, J.T.; Koprowski, J.L. Wild boar. In Mammals of Korea, 1st ed.; National Institute of Biological Resources: Incheon, Korea, 2018; pp. 284–286. [Google Scholar]
- Hanlon, C.A.; Niezgoda, M.; Hamir, A.N.; Schumacher, C.; Koprowski, H.; Rupprecht, C.E. First North American field release of a vaccinia-rabies glycoprotein recombinant virus. J. Wildl. Dis. 1998, 34, 228–239. [Google Scholar] [CrossRef]
- Sattler, A.C.; Krogwold, R.A.; Wittum, T.E.; Rupprecht, C.E.; Algeo, T.P.; Slate, D.; Smith, K.A.; Hale, R.L.; Nohrenberg, G.A.; Lovell, C.D.; et al. Influence of oral rabies vaccine bait density on rabies seroprevalence in wild raccoons. Vaccine 2009, 27, 7187–7193. [Google Scholar] [CrossRef]
- Yang, D.K.; Kim, H.H.; Choi, S.S.; Lee, S.H.; Cho, I.S. A recombinant rabies virus (ERAGS) for use in a bait vaccine for swine. Clin. Exp. Vaccine Res. 2016, 5, 169–174. [Google Scholar] [CrossRef] [Green Version]
| Season | Seropositivity 1 (%) (No. Positive/No. Total Samples) | Month | Seropositivity 1 (%) (No. Positive/No. Total Samples) |
|---|---|---|---|
| Spring | 24.6 (16/65) | March | 41.7 (5/12) |
| April | 11.1 (3/27) | ||
| May | 30.8 (8/26) | ||
| Summer | 13.5 (7/52) | June | 9.1 (2/22) |
| July | 17.9 (5/28) | ||
| August | 0 (0/2) | ||
| Fall | 8.4 (34/407) | September | 1.8 (2/112) |
| October | 2.0 (2/102) | ||
| November | 15.5 (30/193) | ||
| Winter | 3.6 (2/55) | December | 0 (0/51) |
| January | 50 (2/4) | ||
| Total | 10.2 (59/579) | Total | 10.2 (59/579) |
| p value 2 | <0.0001 | p value 2 | 0.0003 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, H.-H.; Yang, D.-K.; Wang, J.-Y.; An, D.-J. The Presence of Rabies Virus-Neutralizing Antibody in Wild Boars (Sus scrofa), a Non-Target Bait Vaccine Animal in Korea. Vet. Sci. 2020, 7, 90. https://doi.org/10.3390/vetsci7030090
Kim H-H, Yang D-K, Wang J-Y, An D-J. The Presence of Rabies Virus-Neutralizing Antibody in Wild Boars (Sus scrofa), a Non-Target Bait Vaccine Animal in Korea. Veterinary Sciences. 2020; 7(3):90. https://doi.org/10.3390/vetsci7030090
Chicago/Turabian StyleKim, Ha-Hyun, Dong-Kun Yang, Ja-Young Wang, and Dong-Jun An. 2020. "The Presence of Rabies Virus-Neutralizing Antibody in Wild Boars (Sus scrofa), a Non-Target Bait Vaccine Animal in Korea" Veterinary Sciences 7, no. 3: 90. https://doi.org/10.3390/vetsci7030090





