Application of Hyperbaric Oxygen Therapy (HBOT) as a Healing Aid after Extraction of Incisors in the Equine Odontoclastic Tooth Resorption and Hypercementosis Syndrome
Abstract
:1. Introduction
2. Materials and Methods
2.1. Case Presentation
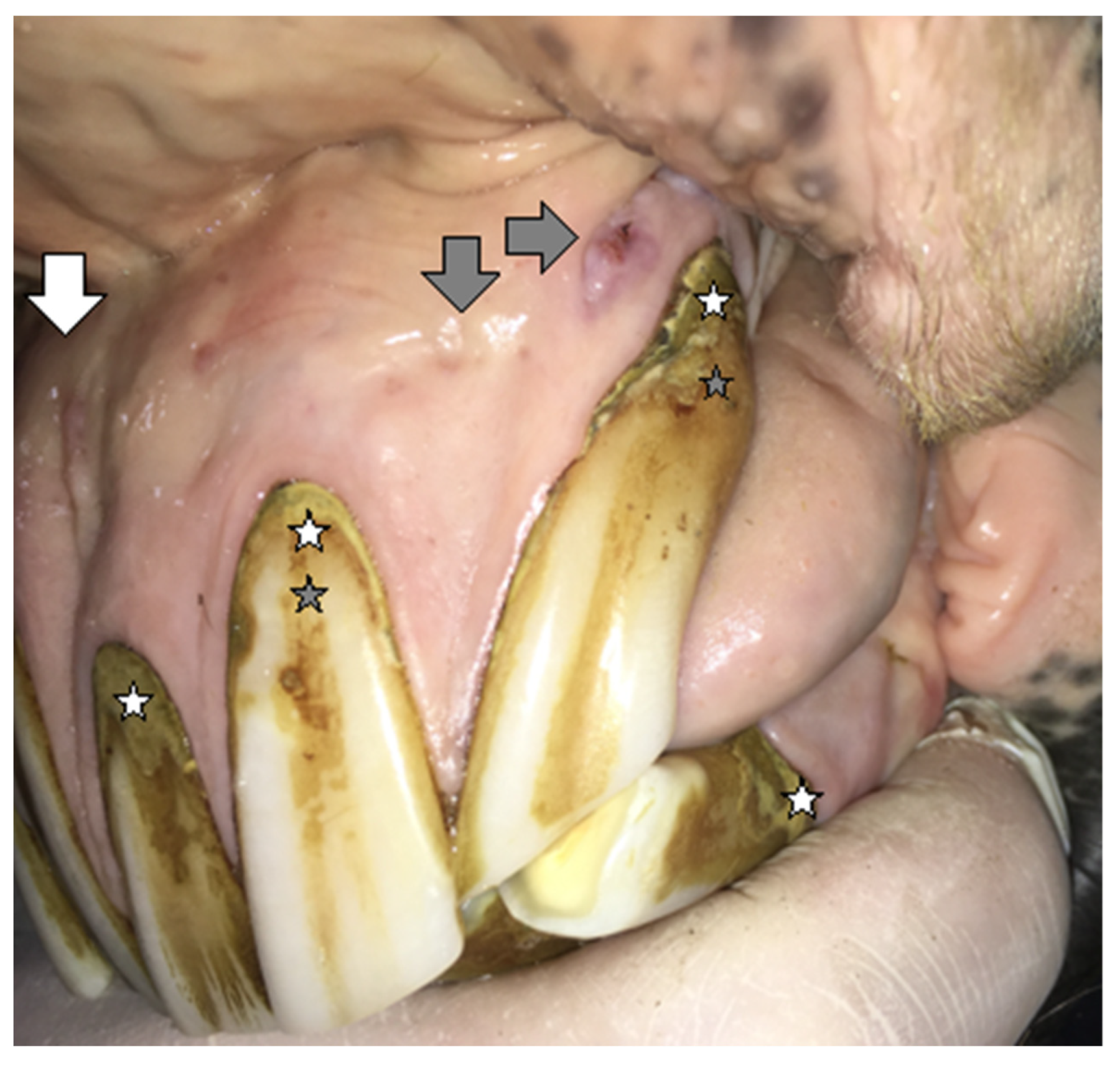
2.1.1. Case 1
2.1.2. Case 2
2.2. Treatment and Postoperative Care
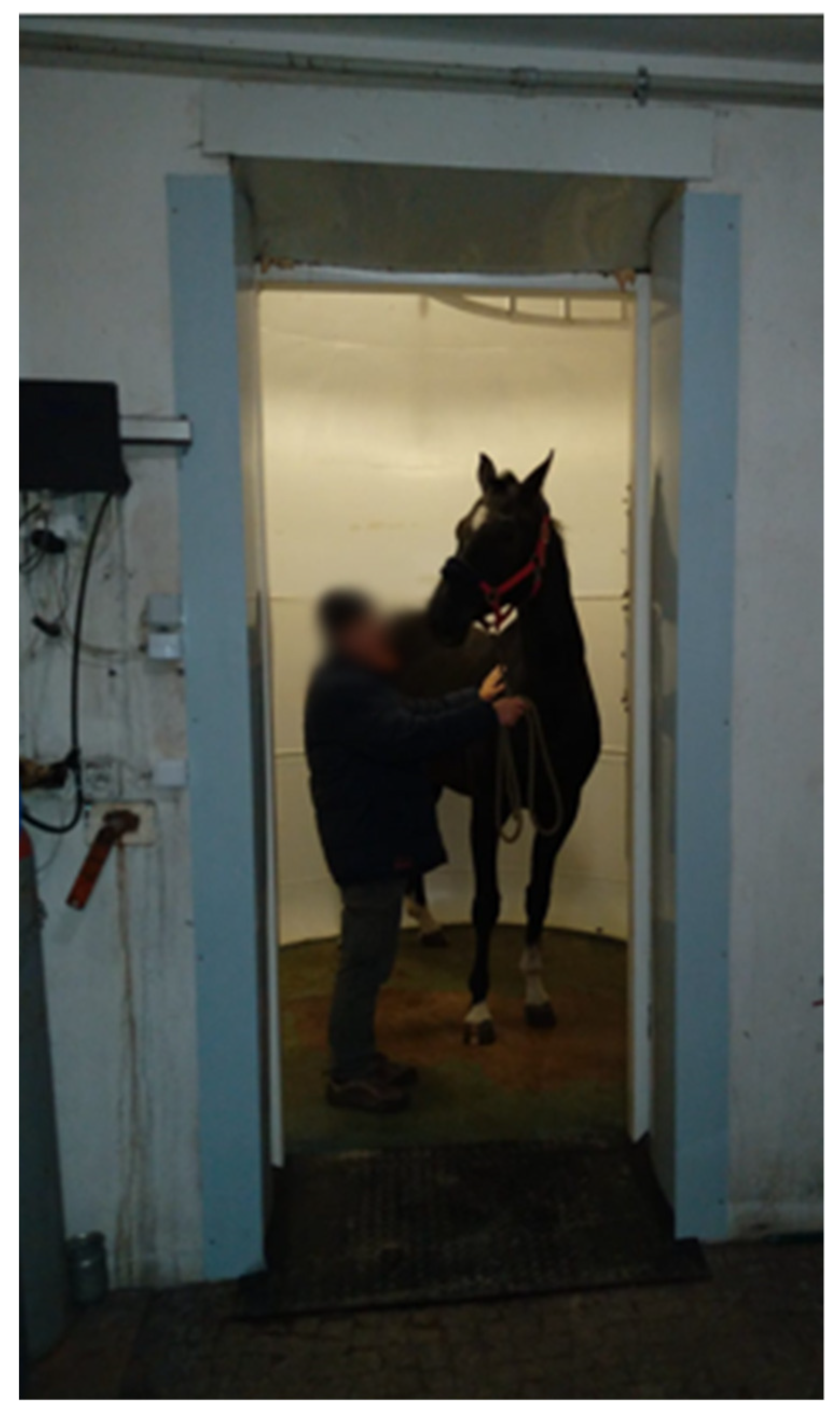
2.3. Hyperbaric Oxygen Therapy
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Slovis, N. Review of Equine Hyperbaric Medicine. J. Equine Vet. Sci. 2008, 28, 760–767. [Google Scholar] [CrossRef]
- Kirby, J.P. Hyperbaric Oxygen Therapy as an Elective Treatment. Mo. Med. 2019, 116, 184–187. [Google Scholar]
- Geiser, D.R. Hyperbaric Oxygen Therapy in Equine Rehabilitation: Putting the Pressure on Disease. Vet. Clin. Equine Pract. 2016, 32, 149–157. [Google Scholar] [CrossRef]
- Health Quality Ontario. Hyperbaric Oxygen Therapy for the Treatment of Diabetic Foot Ulcers: A Health Technology Assessment. Ont. Health Technol. Assess. Ser. 2017, 17, 1–142. [Google Scholar]
- Winaikosol, K.; Punyavong, P.; Jenwitheesuk, K.; Surakunprapha, P.; Mahakkanukrauh, A. Radiation Ulcer Treatment with Hyperbaric Oxygen Therapy and Haemoglobin Spray: Case Report and Literature Review. J. Wound Care 2020, 29, 452–456. [Google Scholar] [CrossRef] [PubMed]
- Deepa, D.; Jain, N. Applications of Hyperbaric Oxygen Therapy in Dentistry: A Mini Review. J. Interdiscip. Dent. 2014, 4, 27. [Google Scholar] [CrossRef]
- Re, K.; Patel, S.; Gandhi, J.; Suh, Y.; Reid, I.; Joshi, G.; Smith, N.; Khan, S. Clinical Utility of Hyperbaric Oxygen Therapy in Dentistry. Med. Gas Res. 2019, 9, 93–100. [Google Scholar] [CrossRef]
- Bennett, M.H.; French, C.; Schnabel, A.; Wasiak, J.; Kranke, P.; Weibel, S. Normobaric and Hyperbaric Oxygen Therapy for the Treatment and Prevention of Migraine and Cluster Headache. Cochrane Database Syst. Rev. 2015. [Google Scholar] [CrossRef]
- Górski, K.; Tremaine, H.; Obrochta, B.; Buczkowska, R.; Turek, B.; Bereznowski, A.; Rakowska, A.; Polkowska, I. EOTRH Syndrome in Polish Half-Bred Horses-Two Clinical Cases. J. Equine Vet. Sci. 2021, 101, 103428. [Google Scholar] [CrossRef] [PubMed]
- Moore, N.T.; Schroeder, W.; Staszyk, C. Equine Odontoclastic Tooth Resorption and Hypercementosis Affecting All Cheek Teeth in Two Horses: Clinical and Histopathological Findings. Equine Vet. Educ. 2016, 28, 123–130. [Google Scholar] [CrossRef]
- Stefanik, E.; Drewnowska, O.; Lisowska, B.; Turek, B. Causes, Effects and Methods of Monitoring Gas Exchange Disturbances during Equine General Anaesthesia. Animals 2021, 11, 2049. [Google Scholar] [CrossRef] [PubMed]
- Eichhorn, L.; Thudium, M.; Jüttner, B. The Diagnosis and Treatment of Carbon Monoxide Poisoning. Dtsch. Arztebl. Int. 2018, 115, 863–870. [Google Scholar] [CrossRef]
- Rose, J.J.; Wang, L.; Xu, Q.; McTiernan, C.F.; Shiva, S.; Tejero, J.; Gladwin, M.T. Carbon Monoxide Poisoning: Pathogenesis, Management, and Future Directions of Therapy. Am. J. Respir. Crit. Care Med. 2017, 195, 596–606. [Google Scholar] [CrossRef] [PubMed]
- Bonne, S.L.; Kadri, S.S. Evaluation and Management of Necrotizing Soft Tissue Infections. Infect. Dis. Clin. N. Am. 2017, 31, 497–511. [Google Scholar] [CrossRef]
- Narożny, W.; Siebert, J. Możliwości i Ograniczeniastosowania Tlenu Hiperbarycznegow Medycynie. Forum Med. Rodz. 2007, 1, 368–375. [Google Scholar]
- Narożny, W.; Kuczkowski, J.; Kot, J.; Przewozny, T.; Stankiewicz, C.; Lizak, E. Complications of HBO in Otolaryngology. Otolaryngol. Pol. 2009, 63, 25–29. [Google Scholar] [CrossRef]
- Sultan, A.; Hanna, G.J.; Margalit, D.N.; Chau, N.; Goguen, L.A.; Marty, F.M.; Rabinowits, G.; Schoenfeld, J.D.; Sonis, S.T.; Thomas, T.; et al. The Use of Hyperbaric Oxygen for the Prevention and Management of Osteoradionecrosis of the Jaw: A Dana-Farber/Brigham and Women’s Cancer Center Multidisciplinary Guideline. Oncologist 2017, 22, 343–350. [Google Scholar] [CrossRef] [Green Version]
- Maeda, T.; Yamamoto, Y.; Tanaka, S.; Hayashi, T. Application of Vacuum-Assisted Closure Therapy and Hyperbaric Oxygen Therapy for an Exposed Titanium Plate after Mandible Reconstruction. J. Craniofacial Surg. 2016, 27, E601–E604. [Google Scholar] [CrossRef]
- Stewart, A.J. Clostridial Myositis and Collapse in a Standardbred Filly. Vet. Clin. Equine Pract. 2006, 22, 127–143. [Google Scholar] [CrossRef]
- Holder, T.E.C.; Schumacher, J.; Donnel, R.J. Effects of Hyperbaric Oxygen on Full-Thickness Meshed Sheet Skin Grafts Applied to Fresh and Granulating Wounds in Horses. Am. J. Vet. Res. 2008, 69, 144–147. [Google Scholar] [CrossRef]
- Bain, F.T.; Hoberg, S. Equine Essentials-Hyperbaric Oxygen Therapy for Horses. Vet. Tech. 2008, 29, 678. [Google Scholar]
- Limone, L.E. Update on Equine Odontoclastic Tooth Resorption and Hypercementosis. Vet. Clin. Equine Pract. 2020, 36, 671–689. [Google Scholar] [CrossRef] [PubMed]
- Staszyk, C.; Bienert, A.; Kreutzer, R.; Wohlsein, P.; Simhofer, H. Equine Odontoclastic Tooth Resorption and Hypercementosis. Vet. J. 2008, 178, 372–379. [Google Scholar] [CrossRef] [PubMed]
- Earley, E.T.; Rawlinson, J.R.; Baratt, R.M.; Galloway, S.S.; Smedley, R.C.; Scarlett, J.M.; Refsal, K.R.; Dotzel, A.R.; Cox, V.S.; Perkins, G.A. Hematologic, Biochemical, and Endocrine Parameters in Horses with Tooth Resorption and Hypercementosis. J. Vet. Dent. 2017, 34, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Earley, E.; Rawlinson, J.T. A New Understanding of Oral and Dental Disorders of the Equine Incisor and Canine Teeth. Vet. Clin. Equine Pract. 2013, 29, 273–300. [Google Scholar] [CrossRef] [PubMed]
- Hole, S.L.; Staszyk, C. Equine Odontoclastic Tooth Resorption and Hypercementosis. Equine Vet. Educ. 2018, 30, 386–391. [Google Scholar] [CrossRef]
- Pearson, A.M.; Mansfield, G.; Conaway, M.; Koput, K. Associated Risk Factors of Equine Odontoclastic Tooth Resorption and Hypercementosis. In Proceedings of the 59th Annual Convention of the American Association of Equine Practitioners, Nashville, TN, USA, 7–11 December 2013; Volume 59, pp. 65–70. [Google Scholar]
- Sykora, S.; Pieber, K.; Simhofer, H.; Hackl, V.; Brodesser, D.; Brandt, S. Isolation of Treponema and Tannerella Spp. Equine Vet. J. 2014, 46, 358–363. [Google Scholar] [CrossRef] [PubMed]
- Velnar, T.; Bailey, T.; Smrkolj, V. The Wound Healing Process: An Overview of the Cellular and Molecular Mechanisms. J. Int. Med. Res. 2009, 37, 1528–1542. [Google Scholar] [CrossRef] [PubMed]













Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Górski, K.; Stefanik, E.; Bereznowski, A.; Polkowska, I.; Turek, B. Application of Hyperbaric Oxygen Therapy (HBOT) as a Healing Aid after Extraction of Incisors in the Equine Odontoclastic Tooth Resorption and Hypercementosis Syndrome. Vet. Sci. 2022, 9, 30. https://doi.org/10.3390/vetsci9010030
Górski K, Stefanik E, Bereznowski A, Polkowska I, Turek B. Application of Hyperbaric Oxygen Therapy (HBOT) as a Healing Aid after Extraction of Incisors in the Equine Odontoclastic Tooth Resorption and Hypercementosis Syndrome. Veterinary Sciences. 2022; 9(1):30. https://doi.org/10.3390/vetsci9010030
Chicago/Turabian StyleGórski, Kamil, Elżbieta Stefanik, Andrzej Bereznowski, Izabela Polkowska, and Bernard Turek. 2022. "Application of Hyperbaric Oxygen Therapy (HBOT) as a Healing Aid after Extraction of Incisors in the Equine Odontoclastic Tooth Resorption and Hypercementosis Syndrome" Veterinary Sciences 9, no. 1: 30. https://doi.org/10.3390/vetsci9010030





