Antimicrobial Susceptibility Profiles of Bacteria Commonly Isolated from Farmed Salmonids in Atlantic Canada (2000–2021)
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Bacterial Culture, Identification, and Antimicrobial Susceptibility Testing
2.3. Data Management
2.4. Statistical Analysis
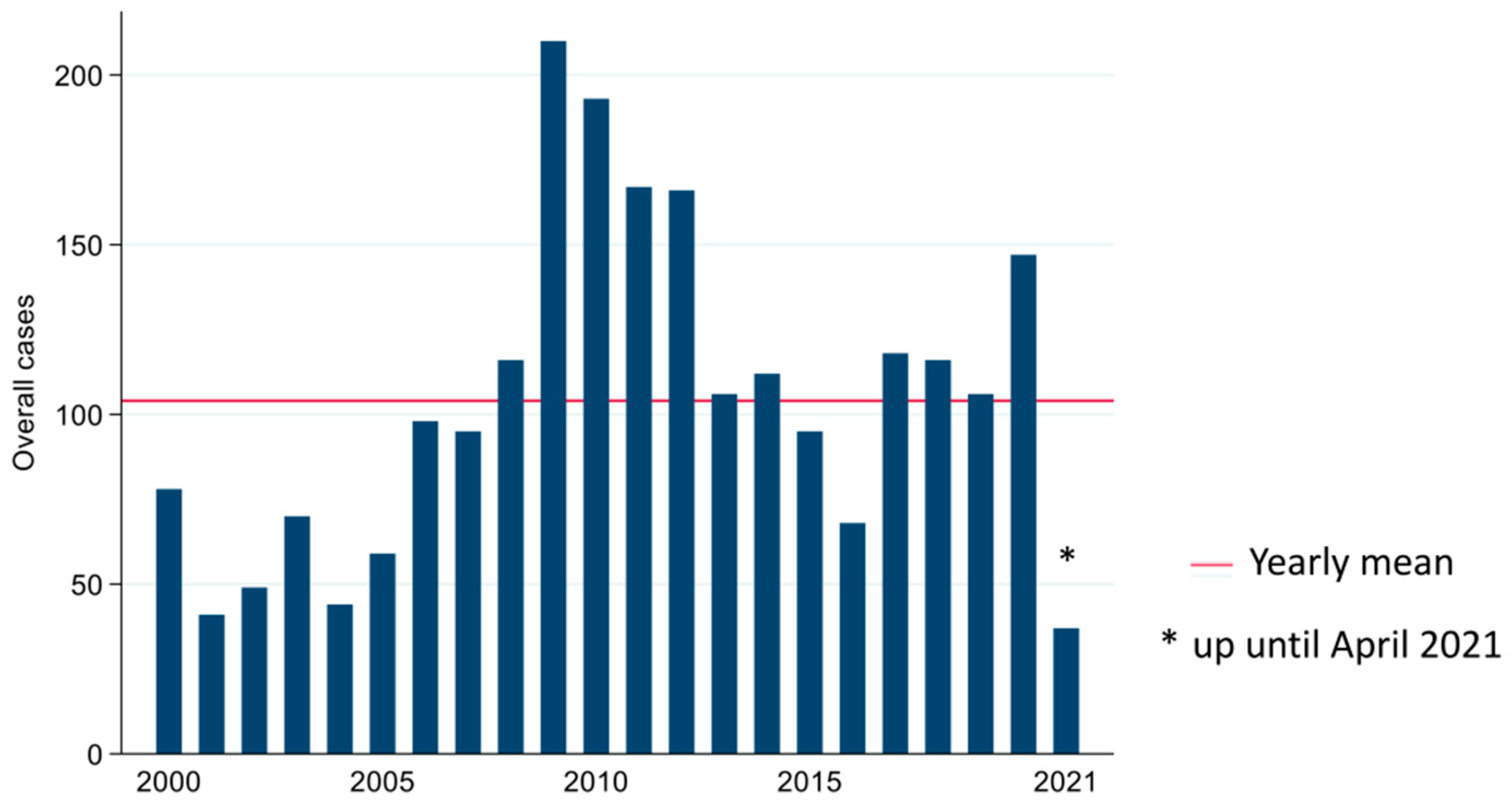
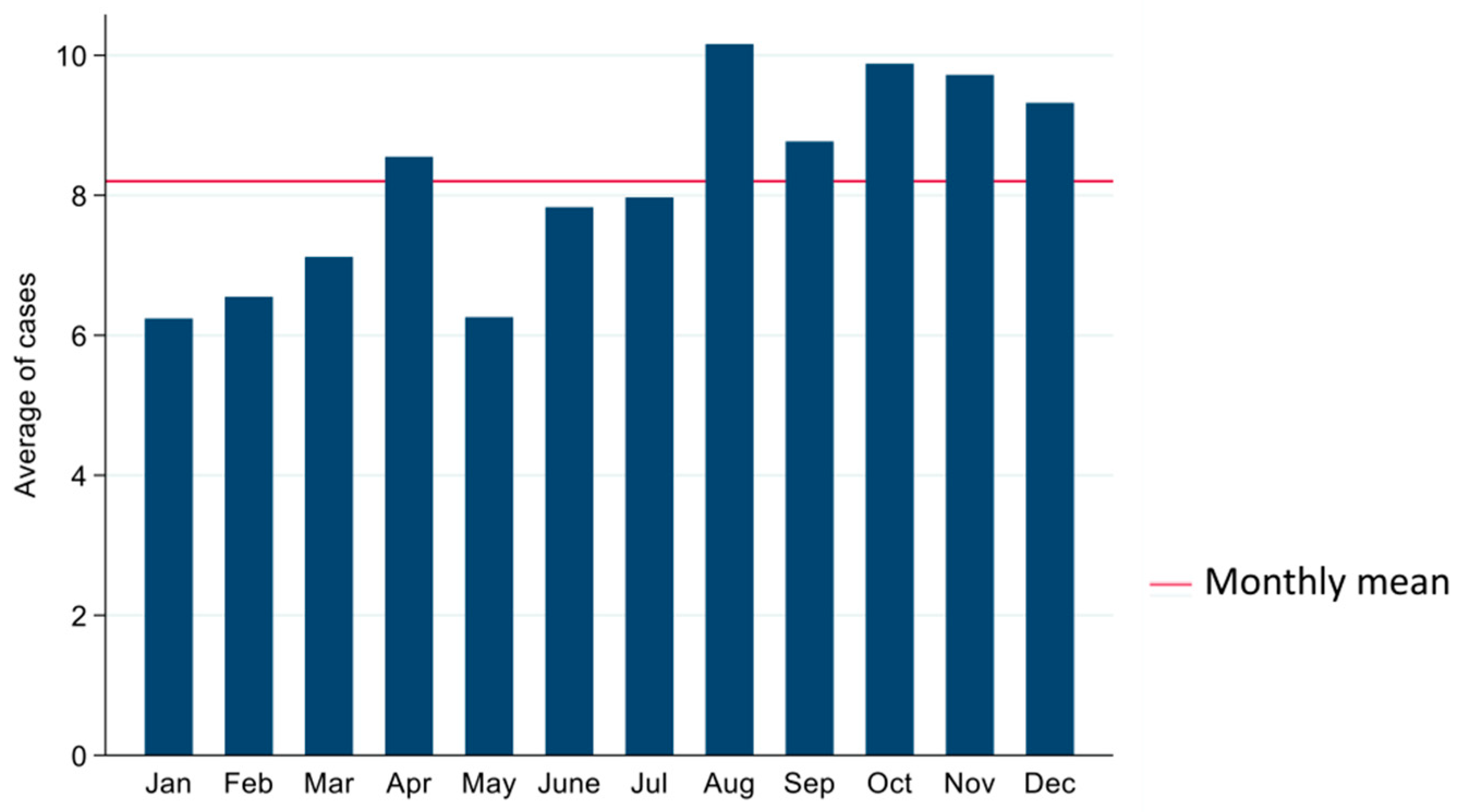
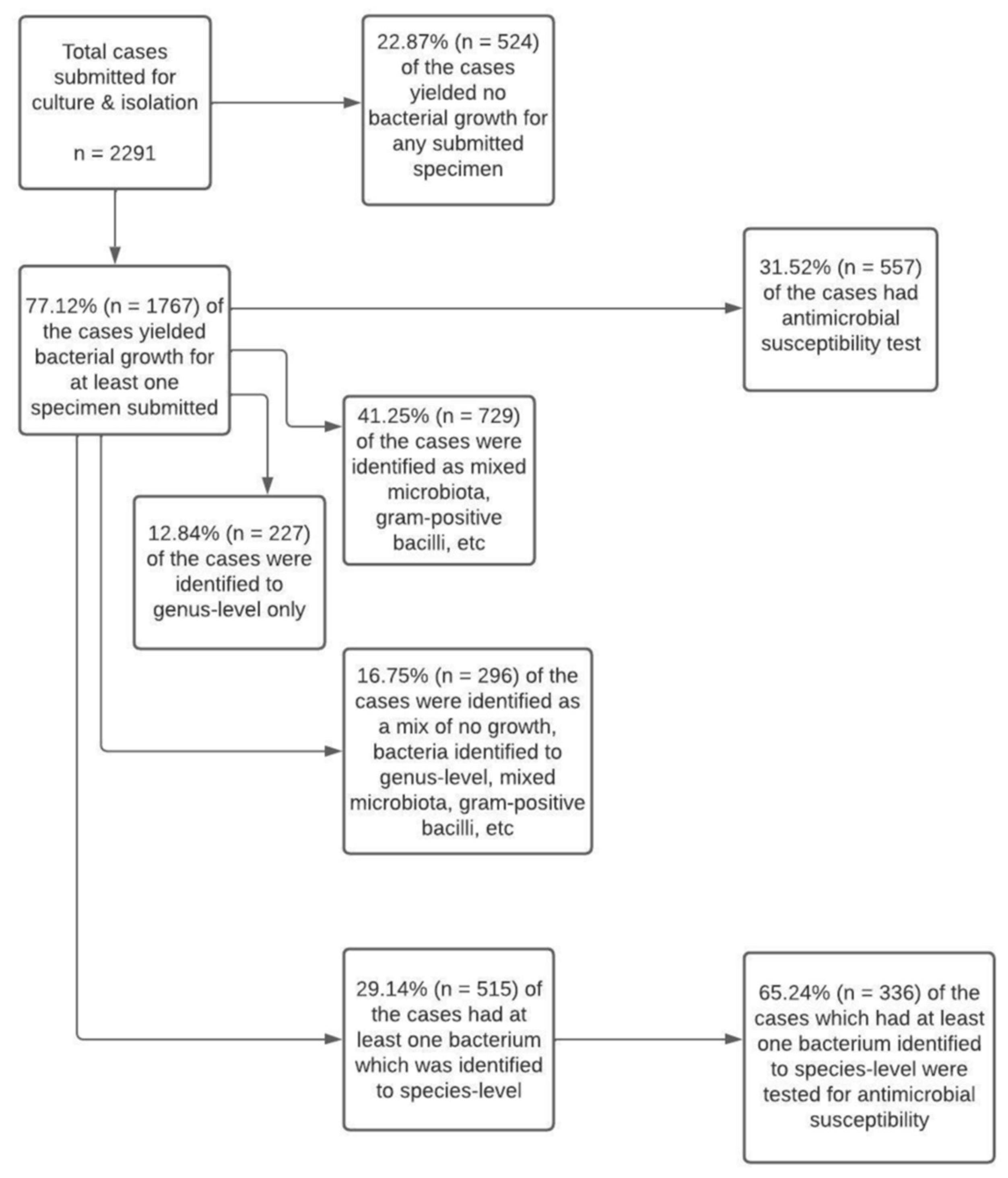
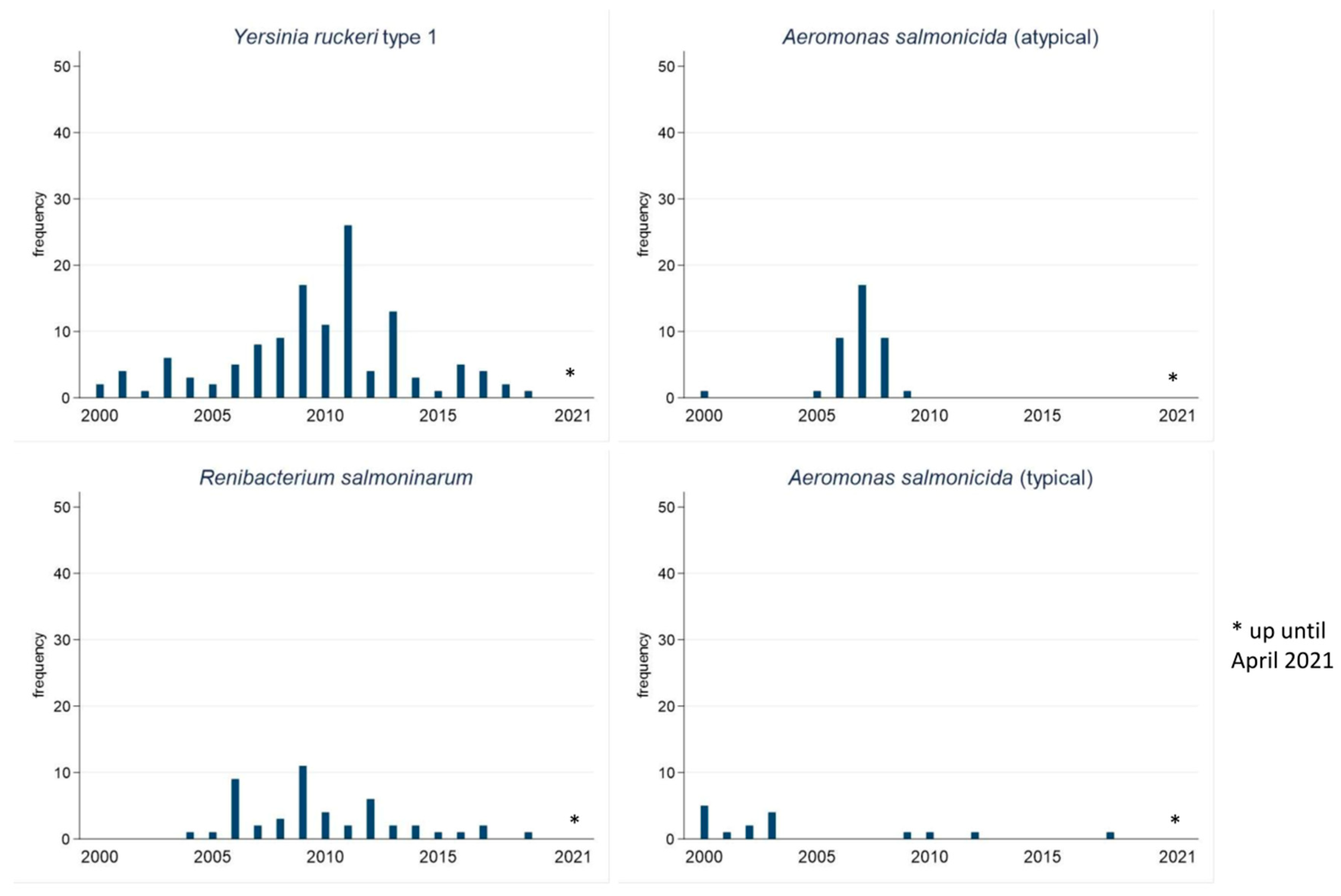
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- FAO. The State of World Fisheries and Aquaculture 2020; Sustainability in Action; FAO: Rome, Italy, 2020. [Google Scholar]
- Plumb, J.A.; Hanson, L.A. Health Maintenance and Principal Microbial Diseases of Cultured Fishes; John Wiley & Sons: Hoboken, NJ, USA, 2010. [Google Scholar] [CrossRef]
- Preena, P.G.; Swaminathan, T.R.; Kumar, V.J.R.; Singh, I.S.B. Antimicrobial resistance in aquaculture: A crisis for concern. Biologia 2020, 75, 1497–1517. [Google Scholar] [CrossRef]
- Reverter, M.; Sarter, S.; Caruso, D.; Avarre, J.-C.; Combe, M.; Pepey, E.; Pouyaud, L.; Vega-Heredía, S.; De Verdal, H.; Gozlan, R.E. Aquaculture at the crossroads of global warming and antimicrobial resistance. Nat. Commun. 2020, 11, 1870. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cañada-Cañada, F.; de la Peña, A.M.; Espinosa-Mansilla, A. Analysis of antibiotics in fish samples. Anal. Bioanal. Chem. 2009, 395, 987–1008. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.Q.A.; Cabello, F.C.; L’Abée-Lund, T.M.; Tomova, A.; Godfrey, H.P.; Buschmann, A.H.; Sørum, H. Antimicrobial resistance and antimicrobial resistance genes in marine bacteria from salmon aquaculture and non-aquaculture sites. Environ. Microbiol. 2014, 16, 1310–1320. [Google Scholar] [CrossRef]
- Domínguez, M.; Miranda, C.D.; Fuentes, O.; De La Fuente, M.; Godoy, F.A.; Bello-Toledo, H.; González-Rocha, G. Occurrence of Transferable Integrons and sul and dfr Genes Among Sulfonamide-and/or Trimethoprim-Resistant Bacteria Isolated From Chilean Salmonid Farms. Front. Microbiol. 2019, 10, 748. [Google Scholar] [CrossRef]
- Miranda, C.D.; Zemelman, R. Bacterial resistance to oxytetracycline in Chilean salmon farming. Aquaculture 2002, 212, 31–47. [Google Scholar] [CrossRef]
- Balta, F.; Sandalli, E.; Kayis, S.; Ozgumus, O. Molecular analysis of antimicrobial resistance in Yersinia ruckeri strains isolated from rainbow trout (Oncorhynchus mykiss) grown in commercial fish farms in Turkey. Bull. Eur. Assoc. Fish Pathol. 2010, 30, 211–219. [Google Scholar]
- Roberts, R.J. Fish Pathology; John Wiley & Sons: Hoboken, NJ, USA, 2012. [Google Scholar]
- Kolde, R. Pheatmap: Pretty Heatmaps. R Package Version 1.0.8. 2015, pp. 1–7. Available online: https://cran.r-project.org/web/packages/pheatmap/pheatmap.pdf (accessed on 28 January 2022).
- Powell, M.; Overturf, K.; Hogge, C.; Johnson, K. Detection of Renibacterium salmoninarum in chinook salmon, Oncorhynchus tshawytscha (Walbaum), using quantitative PCR. J. Fish Dis. 2005, 28, 615–622. [Google Scholar] [CrossRef]
- Du, Y.; Yi, M.; Xiao, P.; Meng, L.; Li, X.; Sun, G.; Liu, Y. The impact of Aeromonas salmonicida infection on innate immune parameters of Atlantic salmon (Salmo salar L). Fish Shellfish Immunol. 2015, 44, 307–315. [Google Scholar] [CrossRef]
- Ormsby, M.J.; Caws, T.; Burchmore, R.; Wallis, T.; Verner-Jeffreys, D.W.; Davies, R.L. Yersinia ruckeri Isolates Recovered from Diseased Atlantic Salmon (Salmo salar) in Scotland Are More Diverse than Those from Rainbow Trout (Oncorhynchus mykiss) and Represent Distinct Subpopulations. Appl. Environ. Microbiol. 2016, 82, 5785–5794. [Google Scholar] [CrossRef] [Green Version]
- Yanong, R.; Francis-Floyd, R. Streptococcal Infections of Fish. Florida Cooperative Extension Service. IFAS, University of Florida. Available online: http://edis.ifas.ufl.edu (accessed on 28 January 2022).
- Nekouei, O.; Vanderstichel, R.; Ming, T.; Kaukinen, K.H.; Thakur, K.; Tabata, A.; Laurin, E.; Tucker, S.; Beacham, T.D.; Miller, K.M. Detection and Assessment of the Distribution of Infectious Agents in Juvenile Fraser River Sockeye Salmon, Canada, in 2012 and 2013. Front. Microbiol. 2018, 9, 3221. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lewbart, G. Bacteria and ornamental fish. Semin. Avian Exot. Pet Med. 2001, 10, 48–56. [Google Scholar] [CrossRef]
- DFO. Advice from the Assessment of the Risk to Fraser River Sockeye Salmon due to Yersinia ruckeri Transfer from Atlantic Salmon Farms in the Discovery Islands Area, British Columbia; Canadian Science Advisory Secretariat: Ottawa, ON, Canada, 2020. [Google Scholar]
- McGladdery, S.E.; Zurbrigg, R.E. Canada’s Approach to Aquatic Animal Biosecurity. Exp. Evolution. 2005, 31–54. [Google Scholar] [CrossRef]
- Olin, P.; Smith, J.; Nabi, R. Regional Review on Status and Trends in Aquaculture Development in North America: Canada and the United States of America—2010; FAO Fisheries and Aquaculture Circular: Rome, Italy, 2012. [Google Scholar]
- List of Veterinary Drugs That Are Authorized for Sale by Health Canada for Use in Food-Producing Aquatic Animals. Available online: https://www.canada.ca/en/health-canada/services/drugs-health-products/veterinary-drugs/legislation-guidelines/policies/list-veterinary-drugs-that-authorized-sale-health-canada-use-food-producing-aquatic-animals.html (accessed on 28 January 2022).
- Lopez, C.; Garcia, J.J.; Sierra, M.; Díez, M.J.; Pérez, C.; Sahagún, A.M.; Fernández, N. Systemic and mammary gland disposition of enrofloxacin in healthy sheep following intramammary administration. BMC Vet. Res. 2015, 11, 88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aldred, K.J.; McPherson, S.A.; Turnbough, C.L.; Kerns, R.J.; Osheroff, N. Topoisomerase IV-quinolone interactions are mediated through a water-metal ion bridge: Mechanistic basis of quinolone resistance. Nucleic Acids Res. 2013, 41, 4628–4639. [Google Scholar] [CrossRef]
- Hsu, H.-M.; Wooster, G.A.; Bowser, P.R. Efficacy of Enrofloxacin for the Treatment of Salmonids with Bacterial Kidney Disease, Caused byRenibacterium salmoninarum. J. Aquat. Anim. Health 1994, 6, 220–223. [Google Scholar] [CrossRef]
- Tanrıkul, T.; Avsever, M.; Onuk, E.; Didinen, R. Vagococcus salmoninarum, a causative agent of disease in rainbow trout (Oncorhynchus mykiss, Walbaum) broodstocks in the aegean region of Turkey. Etlik Vet. Mikrobiyoloji Derg. 2014, 25, 11–16. [Google Scholar]
- Zgurskaya, H.I.; Nikaido, H. Multidrug resistance mechanisms: Drug efflux across two membranes. Mol. Microbiol. 2000, 37, 219–225. [Google Scholar] [CrossRef]
- Tyagi, I.; Tyagi, K.; Bhutiani, R.; Chandra, K.; Kumar, V. Bacterial diversity assessment of world’s largest sewage-fed fish farms with special reference to water quality: A Ramsar site. Environ. Sci. Pollut. Res. 2021, 28, 42372–42386. [Google Scholar] [CrossRef]
- Köhler, T.; Kok, M.; Michea-Hamzehpour, M.; Plesiat, P.; Gotoh, N.; Nishino, T.; Curty, L.K.; Pechere, J.C. Multidrug efflux in intrinsic resistance to trimethoprim and sulfamethoxazole in Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 1996, 40, 2288–2290. [Google Scholar] [CrossRef] [Green Version]
- Miranda, C.D.; Rojas, R. Occurrence of florfenicol resistance in bacteria associated with two Chilean salmon farms with different history of antibacterial usage. Aquaculture 2007, 266, 39–46. [Google Scholar] [CrossRef]
- Health Canada Categorization of Antimicrobial Drugs. Available online: https://www.amstewardship.ca/wp-content/uploads/2018/07/v-en-03-categorization-of-antimicrobial-drugs-based-on-importance-in-human-medicine-1.pdf (accessed on 28 January 2022).
- WHO List of Critically Important Antimicrobials for Human Medicine (WHO CIA List). Available online: https://www.who.int/foodsafety/publications/cia2017.pdf (accessed on 28 January 2022).
- Aoki, T.; Egusa, S.; Kimura, T.; Watanabe, T. Detection of R Factors in Naturally Occurring Aeromonas salmonicida Strains. Appl. Microbiol. 1971, 22, 716–717. [Google Scholar] [CrossRef] [PubMed]
- Son, R.; Rusul, G.; Sahilah, A.M.; Zainuri, A.; Raha, A.R.; Salmah, I. Antibiotic resistance and plasmid profile of Aeromonas hydrophila isolates from cultured fish, Telapia (Telapia mossambica). Lett. Appl. Microbiol. 1997, 24, 479–482. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guz, L.; Kozińska, A. Antibiotic susceptibility of Aeromonas hydrophila and A. sobria isolated from farmed carp (Cyprinus carpio L.). Bull. Vet. Inst. Pulawy 2004, 48, 391–395. [Google Scholar]
- Zhang, D.; Li, A.; Xie, J.; Ji, C. In vitroantibacterial effect of berberine hydrochloride and enrofloxacin to fish pathogenic bacteria. Aquac. Res. 2009, 41, 1095–1100. [Google Scholar] [CrossRef]
- Lukkana, M.; Jantrakajorn, S.; Wongtavatchai, J. Antimicrobial susceptibility and enrofloxacin resistance of streptococcal bacteria from farmed Nile tilapia, Oreochromis niloticus (Linnaeus 1758) in Thailand. Aquac. Res. 2015, 47, 3136–3144. [Google Scholar] [CrossRef]
- Stock, I.; Wiedemann, B.; Henrichfreise, B. Natural antibiotic susceptibility and biochemical profiles of Yersinia enterocolitica-like strains: Y. bercovieri, Y. mollaretii, Y. aldovae and ‘Y. ruckeri’. J. Med. Microbiol. 2002, 51, 56–69. [Google Scholar] [CrossRef]
- Onuk, E.; Didinen, B.; Giftci, B.; Yardimci, B.; Pekmezci, G. Molecular characterisation of antibiotic resistance in Yersinia ruckeri isolates from Turkey. Bull. Eur. Assoc. Fish Pathol. 2019, 39, 145–155. [Google Scholar]
- Mohammed, S.; Nagaraj, G.; Chua, F.; Wang, Y. The use of chemicals in aquaculture in Malaysia and Singapore. In Use of Chemicals in Aquaculture in Asia, Proceedings of the Meeting on the Use of Chemicals in Aquaculture in Asia, Tigbauan, Philippines, 20–22 May 1996; Arthur, J.R., Lavilla-Pitogo, C.R., Eds.; Aquaculture Department, Southeast Asian Fisheries Development Center: Tigbauan, Philippines, 2000; pp. 127–140. [Google Scholar]
- Chang, W.-H.; Yang, S.-Y.; Wang, C.-H.; Tsai, M.-A.; Wang, P.-C.; Chen, T.-Y.; Chen, S.-C.; Lee, G.-B. Rapid isolation and detection of aquaculture pathogens in an integrated microfluidic system using loop-mediated isothermal amplification. Sens. Actuators B Chem. 2011, 180, 96–106. [Google Scholar] [CrossRef]
- Smith, P. The Performance of Antimicrobial Susceptibility Testing Programmes Relevant to Aquaculture and Aquaculture Products; FAO Fisheries and Aquaculture Circular No. 1191: Rome, Italy, 2019; Volume 1191. [Google Scholar]
- Faisal, M.; Eissa, A.E.; Starliper, C.E. Recovery of Renibacterium salmoninarum from naturally infected salmonine stocks in Michigan using a modified culture protocol. J. Adv. Res. 2010, 1, 95–102. [Google Scholar] [CrossRef] [Green Version]
- Buller, N. Bacteria from Fish and other Aquatic Animals: A Practical Identification Manual; Centre for Agriculture and Bioscience International: Wallingford, UK, 2004. [Google Scholar]
- Statistics Canada: Canadian Aquaculture Statistics; EUROSTAT Handbook No. 23; Statistics Canada: Ottawa, ON, Canada, 2015; p. 69.
- Mimeault, C.; Wade, J.; Boily, F.; Johnson, S.; Jones, S.; Aubry, P.; Parsons, G. Assessment of the risk to Fraser River Sockeye Salmon due to piscine orthoreovirus (PRV) transfer from Atlantic Salmon farms in the Discovery Islands area, British Columbia. Can. Sci. Advis. Secr. 2020, 36, 45. Available online: http://www.dfo-mpo.gc.ca/csas-sccs/ (accessed on 28 January 2022).

| Bacterial Isolates | Frequency of Cases (n) | Atlantic Salmon n (%) | Rainbow Trout n (%) |
|---|---|---|---|
| Yersinia ruckeri type 1 | 127 | 127 (100.00) | 0 |
| Renibacterium salmoninarum | 48 | 41 (85.40) | 7 (14.60) |
| Aeromonas salmonicida (atypical) | 38 | 38 (100.00) | 0 |
| Pseudomonas fluorescens | 28 | 27 (96.40) | 1 (3.60) |
| Aeromonas salmonicida (typical) | 16 | 16 (100.00) | 0 |
| Edwardsiella piscicida | 14 | 13 (92.90) | 1 (7.10) |
| Flavobacterium columnare | 12 | 11 (91.70) | 1 (8.30) |
| Aliivibrio salmonicida | 9 | 8 (88.90) | 1 (11.10) |
| Aeromonas sobria | 9 | 7 (77.80) | 2 (22.20) |
| Aeromonas hydrophila | 8 | 6 (75.00) | 2 (25.00) |
| Flavobacterium psychrophilum | 7 | 2 (28.60) | 5 (71.40) |
| Vibrio anguillarum type 1 | 6 | 5 (83.30) | 1 (16.70) |
| Anatomic Sites % (95% CI) | ||||
|---|---|---|---|---|
| Bacterial Isolates | Kidney (n = 11,320) | Skin (n = 1517) | Unspecified (n = 3905) | Others (n = 2034) |
| Yersinia ruckeri type 1 | 7.70 (7.20–8.20) | 0.50 (0.20–1.00) | 15.00 (13.90–16.20) | 1.70 (1.20–2.40) |
| Renibacterium salmoninarum | 2.40 (2.10–2.70) | 0.00 (0.00–0.20) | 1.80 (1.40–2.30) | 0.00 (0.00–0.20) |
| Aeromonas salmonicida (atypical) | 6.70 (6.20–7.10) | 2.00 (1.30–2.80) | 2.40 (1.90–2.90) | 0.70 (0.40–1.10) |
| Pseudomonas fluorescens | 0.90 (0.70–1.10) | 2.70 (1.90–3.60) | 3.70 (3.10–4.30) | 2.60 (2.00–3.40) |
| Aeromonas salmonicida (typical) | 0.70 (0.50–0.80) | 0.00 (0.00–0.20) | 3.10 (2.60–3.70) | 0.00 (0.00–0.20) |
| Flavobacterium columnare | 0.00 (0.00–3.30 × 10−2) | 4.60 (3.60–5.80) | 0.40 (0.20–0.70) | 2.20 (1.60–2.90) |
| Flavobacterium psychrophilum | 0.60 (0.40–0.70) | 2.70 (1.90–3.60) | 0.10 (0.00–0.30) | 0.90 (0.60–1.50) |
| Florfenicol | Oxytetracycline | Ormetoprim-Sulfadimethoxine | Trimethoprim-Sulfamethoxazole | Enrofloxacin | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bacterial Isolates | N | n | S | I | R | n | S | I | R | n | S | I | R | N | n | S | I | R | n | S | I | R |
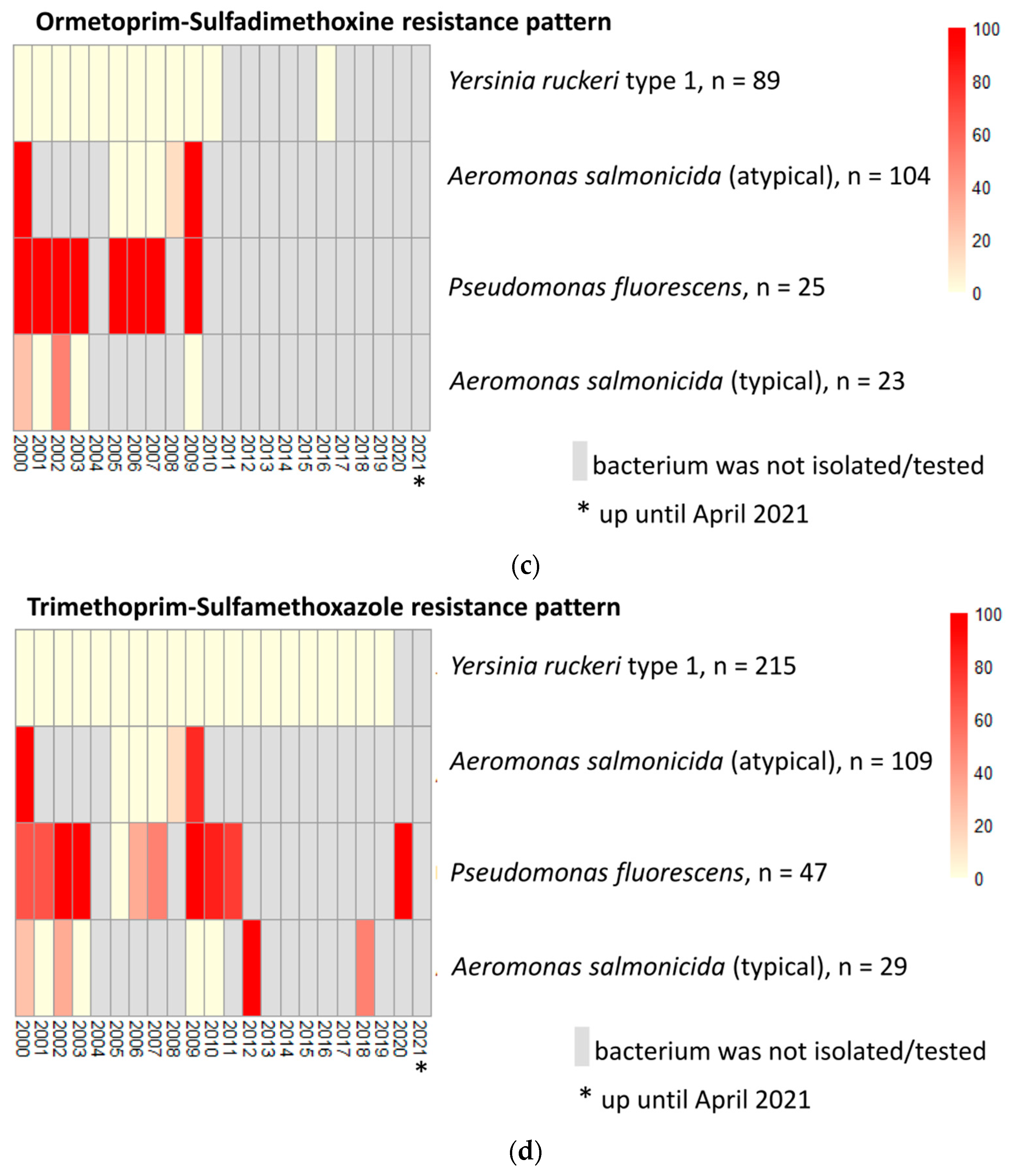
| Yersinia ruckeri type 1 | 215 | 215 | 100.00 | 0.00 | 0.00 | 215 | 99.10 | 0.00 | 0.90 | 89 | 41.40 | 0.00 | 0.00 | 215 | 215 | 100.00 | 0.00 | 0.00 | 215 | 100.00 | 0.00 | 0.00 |
| Aeromonas salmonicida (atypical) | 111 | 108 | 85.60 | 0.00 | 11.70 | 109 | 2.70 | 0.00 | 95.50 | 104 | 82.90 | 0.00 | 10.80 | 111 | 109 | 85.60 | 0.00 | 12.60 | 109 | 98.20 | 0.00 | 0.00 |
| Pseudomonas fluorescens | 47 | 47 | 2.10 | 0.00 | 97.90 | 47 | 72.40 | 2.10 | 25.50 | 25 | 0.00 | 0.00 | 53.20 | 47 | 47 | 21.30 | 6.40 | 72.30 | 45 | 95.70 | 4.30 | 0.00 |
| Aeromonas salmonicida (typical) | 29 | 29 | 72.40 | 0.00 | 27.60 | 29 | 41.40 | 0.00 | 58.60 | 23 | 65.50 | 0.00 | 13.80 | 29 | 29 | 72.40 | 3.50 | 24.10 | 29 | 100.00 | 0.00 | 0.00 |
| Edwardsiella piscicida | 24 | 24 | 100.00 | 0.00 | 0.00 | 24 | 75.00 | 0.00 | 25.00 | 1 | 4.20 | 0.00 | 0.00 | 24 | 24 | 100.00 | 0.00 | 0.00 | 24 | 100.00 | 0.00 | 0.00 |
| Flavobacterium columnare | 20 | 20 | 100.00 | 0.00 | 0.00 | 20 | 90.00 | 5.00 | 5.00 | 12 | 5.00 | 0.00 | 55.00 | 20 | 20 | 55.00 | 0.00 | 45.00 | 20 | 100.00 | 0.00 | 0.00 |
| Aliivibrio salmonicida | 11 | 11 | 100.00 | 0.00 | 0.00 | 11 | 100.00 | 0.00 | 0.00 | 11 | 63.60 | 0.00 | 36.40 | 11 | 11 | 63.60 | 0.00 | 36.40 | 11 | 100.00 | 0.00 | 0.00 |
| Vibrio anguillarum type 1 | 10 | 10 | 100.00 | 0.00 | 0.00 | 10 | 100.00 | 0.00 | 0.00 | 10 | 100.00 | 0.00 | 0.00 | 10 | 10 | 100.00 | 0.00 | 0.00 | 10 | 100.00 | 0.00 | 0.00 |
| Aeromonas hydrophila | 9 | 9 | 100.00 | 0.00 | 0.00 | 9 | 77.80 | 0.00 | 22.20 | 4 | 44.40 | 0.00 | 0.00 | 9 | 9 | 100.00 | 0.00 | 0.00 | 9 | 100.00 | 0.00 | 0.00 |
| Flavobacterium psychrophilum | 8 | 8 | 87.50 | 0.00 | 12.50 | 8 | 100.00 | 0.00 | 0.00 | 0 | 0.00 | 0.00 | 0.00 | 8 | 8 | 75.00 | 0.00 | 25.00 | 8 | 87.50 | 0.00 | 12.50 |
| Vibrio anguillarum type 2 | 7 | 7 | 100.00 | 0.00 | 0.00 | 7 | 100.00 | 0.00 | 0.00 | 4 | 57.10 | 0.00 | 0.00 | 7 | 7 | 100.00 | 0.00 | 0.00 | 7 | 100.00 | 0.00 | 0.00 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ojasanya, R.A.; Gardner, I.A.; Groman, D.B.; Saksida, S.; Saab, M.E.; Thakur, K.K. Antimicrobial Susceptibility Profiles of Bacteria Commonly Isolated from Farmed Salmonids in Atlantic Canada (2000–2021). Vet. Sci. 2022, 9, 159. https://doi.org/10.3390/vetsci9040159
Ojasanya RA, Gardner IA, Groman DB, Saksida S, Saab ME, Thakur KK. Antimicrobial Susceptibility Profiles of Bacteria Commonly Isolated from Farmed Salmonids in Atlantic Canada (2000–2021). Veterinary Sciences. 2022; 9(4):159. https://doi.org/10.3390/vetsci9040159
Chicago/Turabian StyleOjasanya, Rasaq Abiola, Ian A. Gardner, David B. Groman, Sonja Saksida, Matthew E. Saab, and Krishna Kumar Thakur. 2022. "Antimicrobial Susceptibility Profiles of Bacteria Commonly Isolated from Farmed Salmonids in Atlantic Canada (2000–2021)" Veterinary Sciences 9, no. 4: 159. https://doi.org/10.3390/vetsci9040159
APA StyleOjasanya, R. A., Gardner, I. A., Groman, D. B., Saksida, S., Saab, M. E., & Thakur, K. K. (2022). Antimicrobial Susceptibility Profiles of Bacteria Commonly Isolated from Farmed Salmonids in Atlantic Canada (2000–2021). Veterinary Sciences, 9(4), 159. https://doi.org/10.3390/vetsci9040159






