The Impact of Perioperative and Predisposing Risk Factors on the Development of Postoperative Delirium and a Possible Gender Difference
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Data Collection
2.3. Statistical Analysis
3. Results
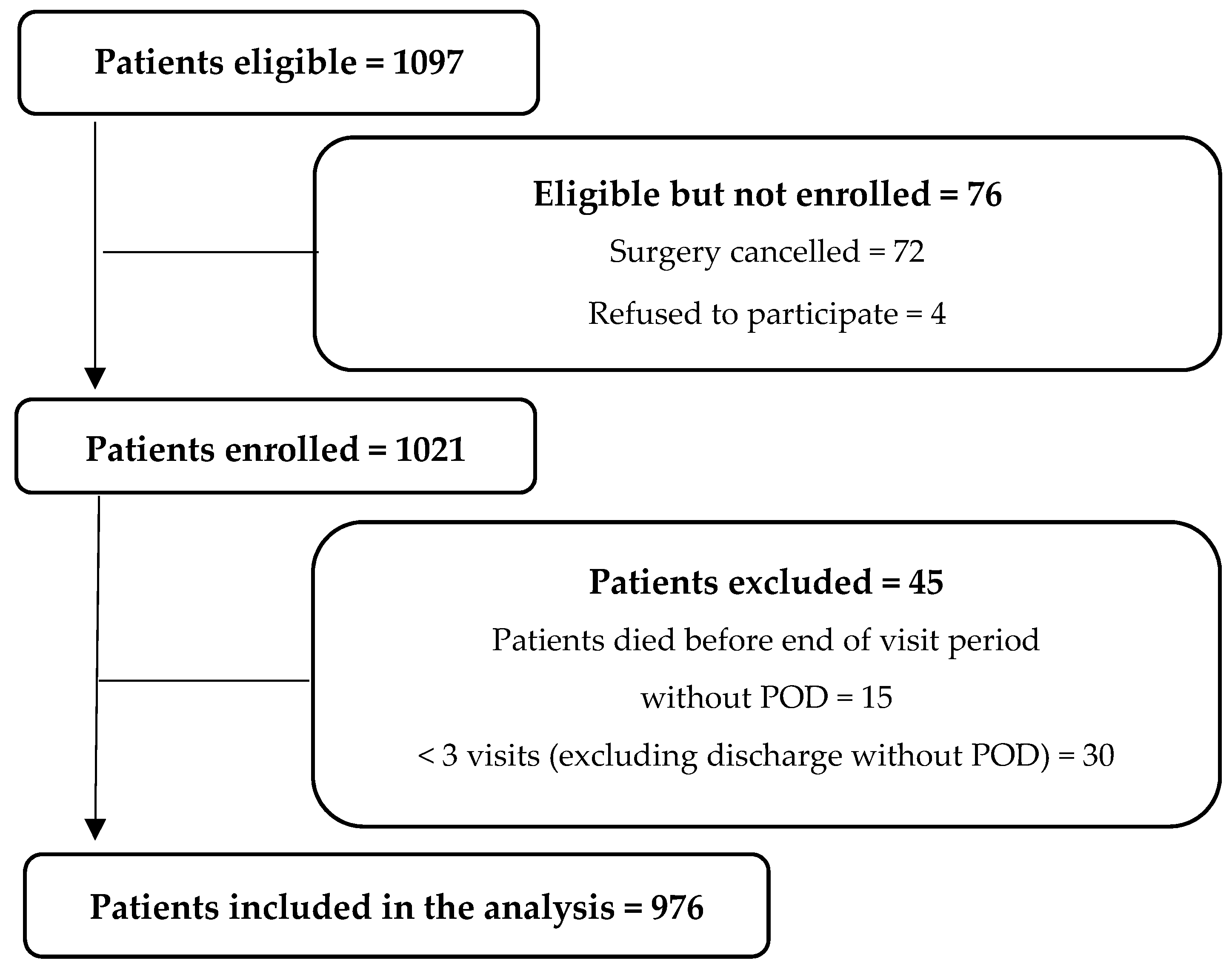
3.1. Participants
3.2. Characteristics Variables Related to POD
3.3. Gender Characteristics in Relation to POD
3.4. Impact of Several Risk Factors on the Development of POD
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Inouye, S.K.; Westendorp, R.G.; Saczynski, J.S. Delirium in Elderly People. Lancet 2014, 383, 911–922. [Google Scholar] [CrossRef] [Green Version]
- Raats, J.W.; van Eijsden, W.A.; Crolla, R.M.P.H.; Steyerberg, E.W.; van der Laan, L. Risk Factors and Outcomes for Postoperative Delirium after Major Surgery in Elderly Patients. PLoS ONE 2015, 10, e0136071. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kirfel, A.; Menzenbach, J.; Guttenthaler, V.; Feggeler, J.; Mayr, A.; Coburn, M.; Wittmann, M. Postoperative Delirium after Cardiac Surgery of Elderly Patients as an Independent Risk Factor for Prolonged Length of Stay in Intensive Care Unit and in Hospital. Aging Clin. Exp. Res. 2021, 33, 3047–3056. [Google Scholar] [CrossRef] [PubMed]
- Lindroth, H.; Bratzke, L.; Purvis, S.; Brown, R.; Coburn, M.; Mrkobrada, M.; Chan, M.T.V.; Davis, D.H.J.; Pandharipande, P.; Carlsson, C.M.; et al. Systematic Review of Prediction Models for Delirium in the Older Adult Inpatient. BMJ Open 2018, 8, e019223. [Google Scholar] [CrossRef] [Green Version]
- Hewitt, J.; Owen, S.; Carter, B.R.; Stechman, M.J.; Tay, H.S.; Greig, M.; McCormack, C.; Pearce, L.; McCarthy, C.; Myint, P.K.; et al. The Prevalence of Delirium in An Older Acute Surgical Population and Its Effect on Outcome. Geriatrics 2019, 4, 57. [Google Scholar] [CrossRef] [Green Version]
- Bickel, H.; Gradinger, R.; Kochs, E.; Förstl, H. High Risk of Cognitive and Functional Decline after Postoperative Delirium. Dement. Geriatr. Cogn. Disord. 2008, 26, 26–31. [Google Scholar] [CrossRef]
- Leslie, D.L.; Zhang, Y.; Holford, T.R.; Bogardus, S.T.; Leo-Summers, L.S.; Inouye, S.K. Premature Death Associated With Delirium at 1-Year Follow-Up. Arch. Intern. Med. 2005, 165, 1657. [Google Scholar] [CrossRef]
- Marcantonio, E.R.; Kiely, D.K.; Simon, S.E.; John Orav, E.; Jones, R.N.; Murphy, K.M.; Bergmann, M.A. Outcomes of Older People Admitted to Postacute Facilities with Delirium: Outcomes of Delirium in Postacute Care. J. Am. Geriatr. Soc. 2005, 53, 963–969. [Google Scholar] [CrossRef]
- Kirfel, A.; Guttenthaler, V.; Mayr, A.; Coburn, M.; Menzenbach, J.; Wittmann, M. Postoperative Delirium Is an Independent Factor Influencing the Length of Stay of Elderly Patients in the Intensive Care Unit and in Hospital. J. Anesth. 2022, 36, 341–348. [Google Scholar] [CrossRef]
- Patel, A.S.; Bergman, A.; Moore, B.W.; Haglund, U. The Economic Burden of Complications Occurring in Major Surgical Procedures: A Systematic Review. Appl. Health Econ. Health Policy 2013, 11, 577–592. [Google Scholar] [CrossRef]
- Mc Donnell, S.; Timmins, F. A Quantitative Exploration of the Subjective Burden Experienced by Nurses When Caring for Patients with Delirium: Subjective Burden. J. Clin. Nurs. 2012, 21, 2488–2498. [Google Scholar] [CrossRef] [PubMed]
- Aldecoa, C.; Bettelli, G.; Bilotta, F.; Sanders, R.D.; Audisio, R.; Borozdina, A.; Cherubini, A.; Jones, C.; Kehlet, H.; MacLullich, A.; et al. European Society of Anaesthesiology Evidence-Based and Consensus-Based Guideline on Postoperative Delirium. Eur. J. Anaesthesiol. 2017, 34, 192–214. [Google Scholar] [CrossRef] [PubMed]
- Simeone, S.; Pucciarelli, G.; Perrone, M.; Teresa, R.; Gargiulo, G.; Guillari, A.; Castellano, G.; Tommaso, L.D.; Niola, M.; Iannelli, G. Delirium in ICU Patients Following Cardiac Surgery: An Observational Study. J. Clin. Nurs. 2018, 27, 1994–2002. [Google Scholar] [CrossRef] [PubMed]
- Habeeb-Allah, A.; Alshraideh, J.A. Delirium Post-cardiac Surgery: Incidence and Associated Factors. Nurs. Crit. Care 2019, 26, 150–155. [Google Scholar] [CrossRef]
- Wang, H.; Guo, X.; Zhu, X.; Li, Y.; Jia, Y.; Zhang, Z.; Yuan, S.; Yan, F. Gender Differences and Postoperative Delirium in Adult Patients Undergoing Cardiac Valve Surgery. Front. Cardiovasc. Med. 2021, 8, 751421. [Google Scholar] [CrossRef]
- Hughes, C.G.; Boncyk, C.S.; Culley, D.J.; Fleisher, L.A.; Leung, J.M.; McDonagh, D.L.; Gan, T.J.; McEvoy, M.D.; Miller, T.E. Perioperative Quality Initiative (POQI) 6 Workgroup American Society for Enhanced Recovery and Perioperative Quality Initiative Joint Consensus Statement on Postoperative Delirium Prevention. Anesth. Analg. 2020, 130, 1572–1590. [Google Scholar] [CrossRef]
- Bilotta, F.; Weiss, B.; Neuner, B.; Kramer, S.; Aldecoa, C.; Bettelli, G.; Sanders, R.D.; Delp, S.M.; Spies, C.D. Routine Management of Postoperative Delirium Outside the ICU: Results of an International Survey among Anaesthesiologists. Acta Anaesthesiol. Scand. 2020, 64, 494–500. [Google Scholar] [CrossRef]
- Menzenbach, J.; Kirfel, A.; Guttenthaler, V.; Feggeler, J.; Hilbert, T.; Ricchiuto, A.; Staerk, C.; Mayr, A.; Coburn, M.; Wittmann, M. PRe-Operative Prediction of Postoperative DElirium by Appropriate SCreening (PROPDESC) Development and Validation of a Pragmatic POD Risk Screening Score Based on Routine Preoperative Data. J. Clin. Anesth. 2022, 78, 110684. [Google Scholar] [CrossRef]
- Menzenbach, J.; Guttenthaler, V.; Kirfel, A.; Ricchiuto, A.; Neumann, C.; Adler, L.; Kieback, M.; Velten, L.; Fimmers, R.; Mayr, A.; et al. Estimating Patients’ Risk for Postoperative Delirium from Preoperative Routine Data—Trial Design of the PRe-Operative Prediction of Postoperative DElirium by Appropriate SCreening (PROPDESC) Study—A Monocentre Prospective Observational Trial. Contemp. Clin. Trials Commun. 2020, 17, 100501. [Google Scholar] [CrossRef]
- Donati, A.; Ruzzi, M.; Adrario, E.; Pelaia, P.; Coluzzi, F.; Gabbanelli, V.; Pietropaoli, P. A New and Feasible Model for Predicting Operative Risk. Br. J. Anaesth. 2004, 93, 393–399. [Google Scholar] [CrossRef] [Green Version]
- Pasternak, R.L. Preanesthesia Evaluation of the Surgical Patient. ASA Refresh. Courses Anesthesiol. 1996, 24, 205–219. [Google Scholar] [CrossRef]
- Günther, U.; Wrigge, H.; Popp, J.; Andorfer, U.; Muders, T.; Putensen, C. Confusion Assessment Method for Intensive Care Unit zur routinemäßigen Kontrolle des Delirs auf Intensivstation. Anästh. Intensivmed. 2009, 50, 592–600. [Google Scholar]
- Sessler, C.N.; Gosnell, M.S.; Grap, M.J.; Brophy, G.M.; O’Neal, P.V.; Keane, K.A.; Tesoro, E.P.; Elswick, R.K. The Richmond Agitation–Sedation Scale: Validity and Reliability in Adult Intensive Care Unit Patients. Am. J. Respir. Crit. Care Med. 2002, 166, 1338–1344. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schuurmans, M.J.; Shortridge-Baggett, L.M.; Duursma, S.A. The Delirium Observation Screening Scale: A Screening Instrument for Delirium. Res. Theory Nurs. Pract. 2003, 17, 31–50. [Google Scholar] [CrossRef] [PubMed]
- Inouye, S.K. Clarifying Confusion: The Confusion Assessment Method: A New Method for Detection of Delirium. Ann. Intern. Med. 1990, 113, 941. [Google Scholar] [CrossRef] [PubMed]
- Bellelli, G.; Morandi, A.; Davis, D.H.J.; Mazzola, P.; Turco, R.; Gentile, S.; Ryan, T.; Cash, H.; Guerini, F.; Torpilliesi, T.; et al. Validation of the 4AT, a New Instrument for Rapid Delirium Screening: A Study in 234 Hospitalised Older People. Age Ageing 2014, 43, 496–502. [Google Scholar] [CrossRef] [Green Version]
- Bilotta, F.; Lauretta, M.P.; Borozdina, A.; Mizikov, V.M.; Rosa, G. Postoperative Delirium: Risk Factors, Diagnosis and Perioperative Care. Minerva Anestesiol. 2013, 79, 1066–1076. [Google Scholar]
- Oh, E.S.; Sieber, F.E.; Leoutsakos, J.-M.; Inouye, S.K.; Lee, H.B. Sex Differences in Hip Fracture Surgery: Preoperative Risk Factors for Delirium and Postoperative Outcomes. J. Am. Geriatr. Soc. 2016, 64, 1616–1621. [Google Scholar] [CrossRef] [Green Version]
- Brouquet, A.; Cudennec, T.; Benoist, S.; Moulias, S.; Beauchet, A.; Penna, C.; Teillet, L.; Nordlinger, B. Impaired Mobility, ASA Status and Administration of Tramadol Are Risk Factors for Postoperative Delirium in Patients Aged 75 Years or More After Major Abdominal Surgery. Ann. Surg. 2010, 251, 759–765. [Google Scholar] [CrossRef]
- Jain, F.A.; Brooks, J.O.; Larsen, K.A.; Kelly, S.E.; Bode, R.H.; Sweeney, G.A.; Stern, T.A. Individual Risk Profiles for Postoperative Delirium after Joint Replacement Surgery. Psychosomatics 2011, 52, 410–416. [Google Scholar] [CrossRef]
- Al-Mallah, M.H.; Juraschek, S.P.; Whelton, S.; Dardari, Z.A.; Ehrman, J.K.; Michos, E.D.; Blumenthal, R.S.; Nasir, K.; Qureshi, W.T.; Brawner, C.A.; et al. Sex Differences in Cardiorespiratory Fitness and All-Cause Mortality. Mayo Clin. Proc. 2016, 91, 755–762. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Characteristics | Total (n = 976) | Non-POD Group (n = 747) | POD-Group (n = 229) | p Value | Missing Values |
|---|---|---|---|---|---|
| Age (mean, sd) | 72.3 ± 7.3 | 72.0 ± 7.3 | 73.3 ± 7.2 | 0.010 | 0 |
| Sex | <0.001 | 0 | |||
| female | 375 (38.4) | 311 (41.6) | 64 (27.9) | ||
| male | 601 (61.6) | 436 (58.4) | 165 (72.1) | ||
| BMI (mean, sd) | 27.7 ± 5.4 | 27.8 ± 5.5 | 27.5 ± 5.0 | 0.827 | 3 |
| ASA | <0.001 | 0 | |||
| ASA 1 | 25 (2.6) | 21 (2.8) | 4 (1.7) | ||
| ASA 2 | 339 (34.7) | 308 (41.2) | 31 (13.5) | ||
| ASA 3 | 544 (55.7) | 380 (50.9) | 164 (71.6) | ||
| ASA 4 | 68 (7.0) | 38 (5.1) | 30 (13.1) | ||
| NYHA | <0.001 | 0 | |||
| NYHA I | 413 (42.3) | 361 (48.3) | 52 (22.7) | ||
| NYHA II | 336 (34.4) | 252 (33.7) | 84 (36.7) | ||
| NYHA III | 210 (21.5) | 125 (16.7) | 85 (37.1) | ||
| NYHA IV | 17 (1.7) | 9 (1.2) | 8 (3.5) | ||
| rCRI | <0.001 | 0 | |||
| rCRI 1 | 408 (41.8) | 367 (49.1) | 41 (17.9) | ||
| rCRI 2 | 243 (24.9) | 185 (24.8) | 58 (25.3) | ||
| rCRI 3 | 218 (22.3) | 144 (19.3) | 74 (32.3) | ||
| rCRI 4 | 107 (11.0) | 51 (6.8) | 56 (24.5) | ||
| MET | <0.001 | 0 | |||
| MET < 1 | 11 (1.1) | 9 (1.2) | 2 (0.9) | ||
| MET 1–4 | 457 (46.8) | 320 (42.8) | 137 (59.8) | ||
| MET 5–10 | 475 (48.7) | 389 (52.1) | 86 (37.6) | ||
| MET > 10 | 33 (3.4) | 29 (3.9) | 4 (1.7) | ||
| Surgical discipline | <0.001 | 0 | |||
| Others | 193 (19.8) | 174 (23.3) | 19 (8.3) | ||
| Cardiac Surgery | 274 (28.1) | 136 (18.2) | 138 (60.3) | ||
| Orthopedic Surgery | 337 (34.5) | 294 (39.4) | 43 (18.8) | ||
| Thoracic Surgery | 21 (2.2) | 17 (2.3) | 4 (1.7) | ||
| Abdominal Surgery | 123 (12.6) | 107 (14.3) | 16 (7.0) | ||
| Vascular Surgery | 28 (2.9) | 19 (2.5) | 9 (3.9) | ||
| Surgical risk | <0.001 | 0 | |||
| low | 126 (12.9) | 123 (16.5) | 3 (1.3) | ||
| Intermediate | 430 (44.1) | 360 (48.2) | 70 (30.6) | ||
| high | 420 (43.0) | 264 (35.3) | 156 (68.1) | ||
| Surgery duration (min) (mean, sd) | 218.4 ± 125.4 | 200.0 ± 120.4 | 278.5 ± 122.8 | <0.001 | 1 |
| Ventilation time (h) (mean, sd) | 13.3 ± 56.2 | 7.8 ± 12.6 | 31.4 ± 111.7 | <0.001 | 11 |
| LOS ICU (h) (mean, sd) | 51.3 ± 226.0 | 22.0 ± 61.5 | 147.6 ± 442.1 | <0.001 | 10 |
| Women (n = 375) | Men (n = 601) | |||||
|---|---|---|---|---|---|---|
| Characteristics | Non-POD Group (n = 311) | POD-Group (n = 64) | p Value | Non-POD Group (n = 436) | POD-Group (n = 165) | p Value |
| Age (mean, sd) | 72.8 ± 7.7 | 74.6 ± 6.3 | 0.062 | 71.4 ± 7.0 | 72.8 ± 7.5 | 0.032 |
| BMI (mean, sd) | 27.7 ± 6.3 | 26.8 ± 5.7 | 0.532 | 27.9 ± 4.9 | 27.7 ± 4.6 | 0.843 |
| ASA | <0.001 | <0.001 | ||||
| ASA 1 | 9 (2.9) | 0 (0.0) | 12 (2.8) | 4 (2.4) | ||
| ASA 2 | 144 (46.3) | 11 (17.2) | 164 (37.6) | 20 (12.1) | ||
| ASA 3 | 144 (46.3) | 44 (68.8) | 236 (54.1) | 120 (72.7) | ||
| ASA 4 | 14 (4.5) | 9 (14.1) | 24 (5.5) | 21 (12.7) | ||
| NYHA | 0.001 | <0.001 | ||||
| NYHA I | 142 (45.7) | 19 (29.7) | 219 (50.2) | 33 (20.0) | ||
| NYHA II | 109 (35.0) | 18 (28.1) | 143 (32.8) | 66 (40.0) | ||
| NYHA III | 58 (18.6) | 24 (37.5) | 67 (15.4) | 61 (37.0) | ||
| NYHA IV | 2 (0.6) | 3 (4.7) | 7 (1.6) | 5 (3.0) | ||
| rCRI | <0.001 | <0.001 | ||||
| rCRI 1 | 169 (54.3) | 20 (31.3) | 198 (45.4) | 21 (12.7) | ||
| rCRI 2 | 83 (26.7) | 14 (21.9) | 102 (23.4) | 44 (26.7) | ||
| rCRI 3 | 45 (14.5) | 21 (32.8) | 99 (22.7) | 53 (32.1) | ||
| rCRI 4 | 14 (4.5) | 9 (14.1) | 37 (8.5) | 47 (28.5) | ||
| MET | 0.045 | 0.001 | ||||
| MET < 1 | 5 (1.5) | 0 (0.0) | 4 (0.9) | 2 (1.2) | ||
| MET 1–4 | 149 (47.9) | 43 (67.2) | 171 (39.2) | 94 (57.0) | ||
| MET 5–10 | 146 (46.9) | 20 (31.3) | 243 (55.7) | 66 (40.0) | ||
| MET > 10 | 11 (3.5) | 1 (1.6) | 18 (4.1) | 3 (1.8) | ||
| Surgical discipline | <0.001 | <0.001 | ||||
| Others | 44 (14.1) | 8 (12.5) | 130 (29.8) | 11 (6.7) | ||
| Cardiac Surgery | 44 (14.1) | 33 (51.6) | 92 (21.1) | 105 (63.6) | ||
| Orthopedic Surgery | 157 (50.5) | 17 (26.6) | 137 (31.4) | 26 (15.8) | ||
| Thoracic Surgery | 8 (2.6) | 1 (1.6) | 9 (2.1) | 3 (1.8) | ||
| Abdominal Surgery | 52 (16.7) | 2 (3.1) | 55 (12.6) | 14 (8.5) | ||
| Vascular Surgery | 6 (1.9) | 3 (4.7) | 13 (3.0) | 6 (3.6) | ||
| Surgical risk | <0.001 | <0.001 | ||||
| low | 51 (16.4) | 1 (1.6) | 72 (16.5) | 2 (1.2) | ||
| Intermediate | 161 (51.8) | 27 (42.2) | 199 (45.6) | 43 (26.1) | ||
| high | 99 (31.8) | 36 (56.3) | 165 (37.8) | 120 (72.7) | ||
| Surgery duration (min) (mean, sd) | 185.5 ± 118.1 | 250.5 ± 122.1 | <0.001 | 210.3 ± 121.1 | 289.4 ± 121.7 | <0.001 |
| Ventilation time (h) (mean, sd) | 7.6 ± 15.4 | 22.0 ± 54.3 | <0.001 | 7.9 ± 10.1 | 35.0 ± 127.2 | <0.001 |
| LOS ICU (h) (mean, sd) | 69.8 ± 118.0 | 111.4 ± 124.6 | 0.001 | 48.9 ± 64.1 | 208.3 ± 552.9 | <0.001 |
| OR | 95% CI | p-Value | ||
|---|---|---|---|---|
| Sex (ref. women) | 1.84 | 1.34 | 2.55 | <0.001 |
| Adj. OR | 95% CI | p-Value | ||
|---|---|---|---|---|
| Surgery duration (h) | 1.17 | 1.07 | 1.28 | <0.001 |
| Ventilation time (day) | 1.64 | 1.27 | 2.24 | 0.001 |
| Surgery risk | 2.10 | 1.52 | 2.95 | <0.001 |
| Age (10 years) | 1.74 | 1.37 | 2.22 | <0.001 |
| ASA | 1.67 | 1.25 | 2.26 | 0.001 |
| Sex (ref. women) | 1.59 | 1.11 | 2.28 | 0.012 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wittmann, M.; Kirfel, A.; Jossen, D.; Mayr, A.; Menzenbach, J. The Impact of Perioperative and Predisposing Risk Factors on the Development of Postoperative Delirium and a Possible Gender Difference. Geriatrics 2022, 7, 65. https://doi.org/10.3390/geriatrics7030065
Wittmann M, Kirfel A, Jossen D, Mayr A, Menzenbach J. The Impact of Perioperative and Predisposing Risk Factors on the Development of Postoperative Delirium and a Possible Gender Difference. Geriatrics. 2022; 7(3):65. https://doi.org/10.3390/geriatrics7030065
Chicago/Turabian StyleWittmann, Maria, Andrea Kirfel, Diane Jossen, Andreas Mayr, and Jan Menzenbach. 2022. "The Impact of Perioperative and Predisposing Risk Factors on the Development of Postoperative Delirium and a Possible Gender Difference" Geriatrics 7, no. 3: 65. https://doi.org/10.3390/geriatrics7030065
APA StyleWittmann, M., Kirfel, A., Jossen, D., Mayr, A., & Menzenbach, J. (2022). The Impact of Perioperative and Predisposing Risk Factors on the Development of Postoperative Delirium and a Possible Gender Difference. Geriatrics, 7(3), 65. https://doi.org/10.3390/geriatrics7030065







