Clinical Use of Blood Flow Analysis through 4D-Flow Imaging in Aortic Valve Disease
Abstract
:1. Introduction
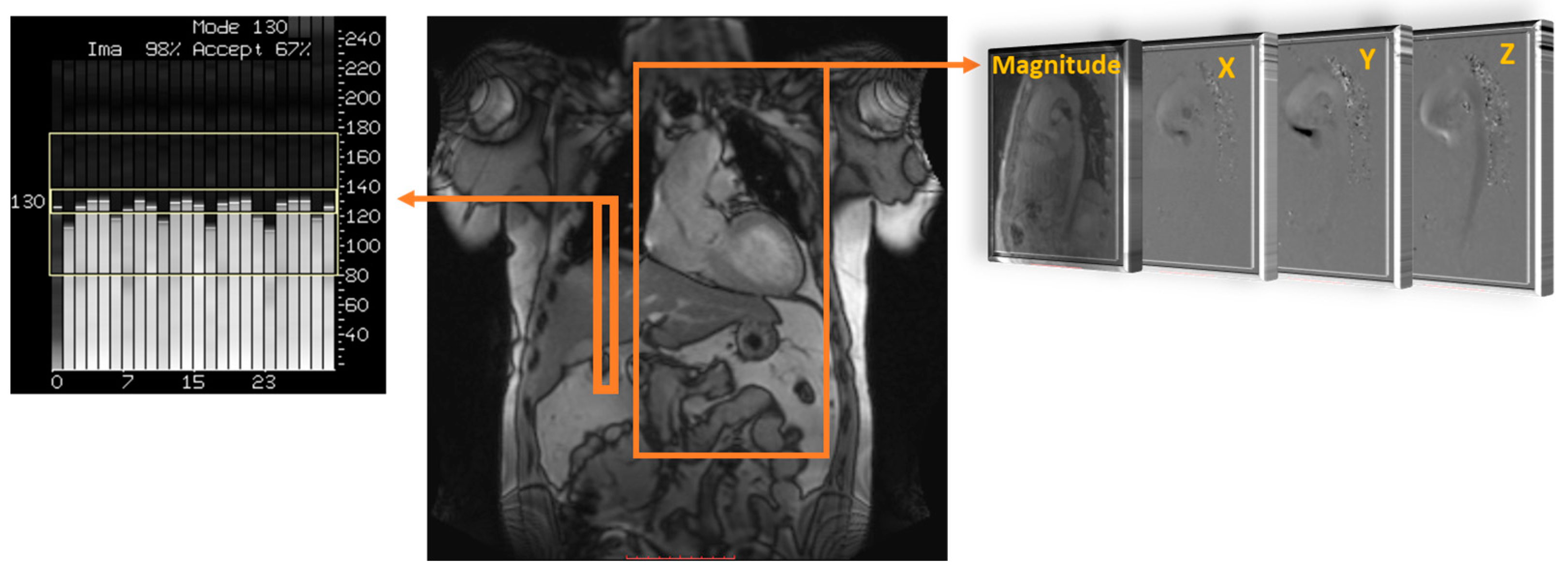
2. Cardiovascular 4D-Flow
3. Clinical Applications in Bicuspid Valve Disease
4. Clinical Applications in Aortic Stenosis (AS)
5. Conclusions and Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kvitting, J.P.E.; Dyverfeldt, P.; Sigfridsson, A.; Franzén, S.; Wigström, L.; Bolger, A.F.; Ebbers, T. In vitro assessment of flow patterns and turbulence intensity in prosthetic heart valves using generalized phase-contrast MRI. J. Magn. Reson. Imaging 2010, 31, 1075–1080. [Google Scholar] [CrossRef]
- Ha, H.; Kvitting, J.P.; Dyverfeldt, P.; Ebbers, T. 4D Flow MRI quantification of blood flow patterns, turbulence and pressure drop in normal and stenotic prosthetic heart valves. Magn. Reson. Imaging 2019, 55, 118–127. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andersson, M.; Ebbers, T.; Karlsson, M. Characterization and estimation of turbulence-related wall shear stress in patient-specific pulsatile blood flow. J. Biomech. 2019, 85, 108–117. [Google Scholar] [CrossRef] [PubMed]
- Freidoonimehr, N.; Arjomandi, M.; Sedaghatizadeh, N.; Chin, R.; Zander, A. Transitional turbulent flow in a stenosed coronary artery with a physiological pulsatile flow. Int. J. Numer. Methods Biomed. Eng. 2020, 28, 36. [Google Scholar] [CrossRef] [PubMed]
- Binter, C.; Gotschy, A.; Sündermann, S.H.; Frank, M.; Tanner, F.C.; Lüscher, T.F.; Manka, R.; Kozerke, S. Turbulent Kinetic Energy Assessed by Multipoint 4-Dimensional Flow Magnetic Resonance Imaging Provides Additional Information Relative to Echocardiography for the Determination of Aortic Stenosis Severity. Circ. Cardiovasc. Imaging 2017, 10, e005486. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dyverfeldt, P.; Hope, M.D.; Tseng, E.E.; Saloner, D. Magnetic resonance measurement of turbulent kinetic energy for the estimation of irreversible pressure loss in aortic stenosis. JACC Cardiovasc. Imaging 2013, 6, 64–71. [Google Scholar] [CrossRef] [Green Version]
- Ha, H.; Ziegler, M.; Welander, M.; Bjarnegård, N.; Carlhäll, C.J.; Lindenberger, M.; Länne, T.; Ebbers, T.; Dyverfeldt, P. Age-Related Vascular Changes Affect Turbulence in Aortic Blood Flow. Front. Physiol. 2018, 9, 36. [Google Scholar] [CrossRef] [Green Version]
- Markl, M.; Frydrychowicz, A.; Kozerke, S.; Hope, M.; Wieben, O. 4D flow MRI. J. Magn. Reson. Imaging 2012, 36, 1015–1036. [Google Scholar] [CrossRef]
- Dyverfeldt, P.; Sigfridsson, A.; Kvitting, J.P.E.; Ebbers, T. Quantification of intravoxel velocity standard deviation and turbulence intensity by generalizing phase-contrast MRI. Magn. Reson. Med. 2006, 56, 850–858. [Google Scholar] [CrossRef] [Green Version]
- Dillinger, H.; McGrath, C.; Guenthner, C.; Kozerke, S. Fundamentals of turbulent flow spectrum imaging. Magn. Reson. Med. 2022, 87, 1231–1249. [Google Scholar] [CrossRef]
- Dyverfeldt, P.; Bissell, M.; Barker, A.J.; Bolger, A.F.; Carlhäll, C.J.; Ebbers, T.; Francios, C.J.; Frydrychowicz, A.; Geiger, J.; Giese, D.; et al. 4D flow cardiovascular magnetic resonance consensus statement. J. Cardiovasc. Magn. Reson. 2015, 17, 72. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dyverfeldt, P.; Kvitting, J.P.E.; Sigfridsson, A.; Engvall, J.; Bolger, A.F.; Ebbers, T. Assessment of fluctuating velocities in disturbed cardiovascular blood flow: In vivo feasibility of generalized phase-contrast MRI. J. Magn. Reson. Imaging 2008, 28, 655–663. [Google Scholar] [CrossRef] [Green Version]
- Jamalidinan, F.; Hassanabad, A.F.; François, C.J.; Garcia, J. Four-dimensional-flow Magnetic Resonance Imaging of the Aortic Valve and Thoracic Aorta. Radiol. Clin. N. Am. 2020, 58, 753–763. [Google Scholar] [CrossRef] [PubMed]
- Zhuang, B.; Sirajuddin, A.; Zhao, S.; Lu, M. The role of 4D flow MRI for clinical applications in cardiovascular disease: Current status and future perspectives. Quant. Imaging Med. Surg. 2021, 11, 4193–4210. [Google Scholar] [CrossRef]
- Mahadevia, R.; Barker, A.J.; Schnell, S.; Entezari, P.; Kansal, P.; Fedak, P.W.M.; Malaisrie, S.C.; McCarthy, P.; Collins, J.; Carr, J.; et al. Bicuspid aortic cusp fusion morphology alters aortic three-dimensional outflow patterns, wall shear stress, and expression of aortopathy. Circulation 2014, 129, 673–682. [Google Scholar] [CrossRef] [Green Version]
- van Ooij, P.; Markl, M.; Collins, J.D.; Carr, J.C.; Rigsby, C.; Bonow, R.O.; Malaisrie, S.C.; McCarthy, P.M.; Fedak, P.W.; Barker, A.J. Aortic Valve Stenosis Alters Expression of Regional Aortic Wall Shear Stress: New Insights From a 4-Dimensional Flow Magnetic Resonance Imaging Study of 571 Subjects. J. Am. Heart Assoc. 2017, 6, e005959. [Google Scholar] [CrossRef] [PubMed]
- Garcia, J.; Barker, A.J.; Markl, M. The Role of Imaging of Flow Patterns by 4D Flow MRI in Aortic Stenosis. JACC Cardiovasc. Imaging 2019, 12, 252–266. [Google Scholar] [CrossRef]
- Sigovan, M.; Hope, M.D.; Dyverfeldt, P.; Saloner, D. Comparison of four-dimensional flow parameters for quantification of flow eccentricity in the ascending aorta. J. Magn. Reson. Imaging 2011, 34, 1226–1230. [Google Scholar] [CrossRef]
- Garcia, J.; Capoulade, R.; Le Ven, F.; Gaillard, E.; Kadem, L.; Pibarot, P.; Larose, É. Discrepancies between cardiovascular magnetic resonance and Doppler echocardiography in the measurement of transvalvular gradient in aortic stenosis: The effect of flow vorticity. J. Cardiovasc. Magn. Reson. 2013, 15, 84. [Google Scholar] [CrossRef] [Green Version]
- Garcia, J.; Markl, M.; Schnell, S.; Allen, B.; Entezari, P.; Mahadevia, R.; Chris Malaisrie, S.; Pibarot, P.; Carr, J.; Carr, J. 4D Flow Jet Shear Layer Detection Method for the Measurement of Effective Orifice Area and Assessment of Aortic Stenosis Severity. Magn. Reson. Imaging 2014, 32, P241. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ward, C. Clinical significance of the bicuspid aortic valve. Heart 2000, 83, 81–85. [Google Scholar] [CrossRef] [Green Version]
- Quaegebeur, J.M.; Jonas, R.A.; Weinberg, A.D.; Blackstone, E.H.; Kirklin, J.W. Outcomes in seriously ill neonates with coarctation of the aorta. J. Thorac. Cardiovasc. Surg. 1994, 108, 841–854. [Google Scholar] [CrossRef]
- Verma, S.; Siu, S.C. Aortic dilatation in patients with bicuspid aortic valve. N. Engl. J. Med. 2014, 370, 1920–1929. [Google Scholar] [CrossRef] [Green Version]
- Koenig, S.N.; Lincoln, J.; Garg, V. Genetic basis of aortic valvular disease. Curr. Opin. Cardiol. 2017, 32, 239–245. [Google Scholar] [CrossRef] [PubMed]
- Koenig, S.; Bosse, K.; Nadorlik, H.; Lilly, B.; Garg, V. Evidence of Aortopathy in Mice with Haploinsufficiency of Notch1 in Nos3-Null Background. J. Cardiovasc. Dev. Dis. 2015, 2, 17–30. [Google Scholar] [CrossRef] [Green Version]
- Garg, V.; Muth, A.N.; Ransom, J.F.; Schluterman, M.K.; Barnes, R.; King, I.N.; Grossfeld, P.D.; Srivastava, D. Mutations in NOTCH1 cause aortic valve disease. Nature 2005, 437, 270–274. [Google Scholar] [CrossRef] [PubMed]
- Rees, S.; Somerville, J.; Ward, C.; Martinez, J.; Mohiaddin, R.H.; Underwood, R.; Longmore, D.B. Coarctation of the aorta: MR imaging in late postoperative assessment. Radiology 1989, 173, 499–502. [Google Scholar] [CrossRef]
- Robicsek, F.; Thubrikar, M.J.; Cook, J.W.; Fowler, B. The congenitally bicuspid aortic valve: How does it function? Why does it fail? Ann. Thorac. Surg. 2004, 77, 177–185. [Google Scholar] [CrossRef] [PubMed]
- Borger, M.A.; David, T.E. Management of the Valve and Ascending Aorta in Adults with Bicuspid Aortic Valve Disease. Semin. Thorac. Cardiovasc. Surg. 2005, 17, 143–147. [Google Scholar] [CrossRef] [PubMed]
- Hope, M.D.; Meadows, A.K.; Hope, T.a.; Ordovas, K.G.; Reddy, G.P.; Alley, M.T.; Higgins, C.B. Images in cardiovascular medicine. Evaluation of bicuspid aortic valve and aortic coarctation with 4D flow magnetic resonance imaging. Circulation 2008, 117, 2818–2819. [Google Scholar] [CrossRef]
- Hope, M.D.; Hope, T.A.; Crook, S.E.; Ordovas, K.G.; Urbania, T.H.; Alley, M.T.; Higgins, C.B. 4D flow CMR in assessment of valve-related ascending aortic disease. JACC Cardiovasc. Imaging 2011, 4, 781–787. [Google Scholar] [CrossRef] [Green Version]
- Burris, N.S.; Hope, M.D. 4D Flow MRI Applications for Aortic Disease. Magn. Reson. Imaging Clin. N. Am. 2015, 23, 15–23. [Google Scholar] [CrossRef] [Green Version]
- Bollache, E.; Guzzardi, D.G.; Sattari, S.; Olsen, K.E.; Di Martino, E.S.; Malaisrie, S.C.; van Ooij, P.; Collins, J.; Carr, J.; McCarthy, P.M.; et al. Aortic valve-mediated wall shear stress is heterogeneous and predicts regional aortic elastic fiber thinning in bicuspid aortic valve-associated aortopathy. J. Thorac. Cardiovasc. Surg. 2018, 156, 2112–2120.e2. [Google Scholar] [CrossRef] [PubMed]
- Meierhofer, C.; Schneider, E.P.; Lyko, C.; Hutter, A.; Martinoff, S.; Markl, M.; Hager, A.; Hess, J.; Stern, H.; Fratz, S. Wall shear stress and flow patterns in the ascending aorta in patients with bicuspid aortic valves differ significantly from tricuspid aortic valves: A prospective study. Eur. Heart J. Cardiovasc. Imaging 2013, 14, 797–804. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van Ooij, P.; Potters, W.V.; Collins, J.; Carr, M.; Carr, J.; Malaisrie, S.C.; Fedak, P.; McCarthy, P.M.; Markl, M.; Barker, A. Characterization of Abnormal Wall Shear Stress Using 4D Flow MRI in Human Bicuspid Aortopathy. Ann. Biomed. Eng. 2014, 43, 1385–1397. [Google Scholar] [CrossRef]
- Rose, M.J.; Rigsby, C.K.; Berhane, H.; Bollache, E.; Jarvis, K.; Barker, A.J.; Schnell, S.; Allen, B.D.; Robinson, J.D.; Markl, M. 4-D flow MRI aortic 3-D hemodynamics and wall shear stress remain stable over short-term follow-up in pediatric and young adult patients with bicuspid aortic valve. Pediatr. Radiol. 2019, 49, 57–67. [Google Scholar] [CrossRef] [PubMed]
- Hope, M.D.; Sigovan, M.; Wrenn, S.J.; Saloner, D.; Dyverfeldt, P. MRI hemodynamic markers of progressive bicuspid aortic valve-related aortic disease. J. Magn. Reson. Imaging 2014, 40, 140–145. [Google Scholar] [CrossRef] [Green Version]
- Lewandowski, A.J.; Raman, B.; Banerjee, R.; Milanesi, M. Novel Insights into Complex Cardiovascular Pathologies using 4D Flow Analysis by Cardiovascular Magnetic Resonance Imaging. Curr. Pharm. Des. 2017, 23, 3262–3267. [Google Scholar] [CrossRef] [PubMed]
- Lenz, A.; Petersen, J.; Riedel, C.; Weinrich, J.M.; Kooijman, H.; Schoennagel, B.P.; Adam, G.; Von Kodolitsch, Y.; Reichenspurner, H.; Girdauskas, E.; et al. 4D flow cardiovascular magnetic resonance for monitoring of aortic valve repair in bicuspid aortic valve disease. J. Cardiovasc. Magn. Reson. 2020, 22, 29. [Google Scholar] [CrossRef]
- Soulat, G.; Scott, M.B.; Pathrose, A.; Jarvis, K.; Berhane, H.; Allen, B.; Avery, R.; Alsate, A.R.; Rigsby, C.K.; Markl, M. 4D flow MRI derived aortic hemodynamics multi-year follow-up in repaired coarctation with bicuspid aortic valve. Diagn. Interv. Imaging 2022, 103, 418–426. [Google Scholar] [CrossRef]
- Barker, A.J.; van Ooij, P.; Bandi, K.; Garcia, J.; Albaghdadi, M.; McCarthy, P.; Bonow, R.O.; Carr, J.; Collins, J.; Malaisrie, S.C.; et al. Viscous energy loss in the presence of abnormal aortic flow. Magn. Reson. Med. 2014, 72, 620–628. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adriaans, B.P.; Westenberg, J.J.M.; Cauteren, Y.J.M.; Gerretsen, S.; Elbaz, M.S.M.; Bekkers, S.C.A.M.; Veenstra, L.F.; Crijns, H.J.; Wildberger, J.E.; Schalla, S. Clinical assessment of aortic valve stenosis: Comparison between 4D flow MRI and transthoracic echocardiography. J. Magn. Reson. Imaging 2020, 51, 472–480. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guzzardi, D.G.; Barker, A.J.; Van Ooij, P.; Malaisrie, S.C.; Puthumana, J.J.; Belke, D.D.; Mewhort, H.E.; Svystonyuk, D.A.; Kang, S.; Verma, S.; et al. Valve-Related Hemodynamics Mediate Human Bicuspid Aortopathy. J. Am. Coll. Cardiol. 2015, 66, 892–900. [Google Scholar] [CrossRef] [PubMed] [Green Version]






| Studied Population | Key Parameters | Reported Findings |
|---|---|---|
| Soulat et al., 2022 [40] n = 15 BAV Age = 35 ± 8 years | PV, WSS, PWV | WSS is stable over time in BAV patients. Increased PV at coarctation. |
| Adriaans et al., 2020 [42] n = 20 Age = 69.3 ± 5 years | PV, pressure, AVA | AS revealed higher flow velocities than TTE. |
| Lenz et al., 2020 [39] n = 20 Age = 35 (IQR 29–47) | Flow displacement, WSS | Flow displacement and WSS were reduced after valve repair. |
| Rose et al., 2019 [36] n = 19 Age = 14.0 ± 5.7 years | PV, WSS, aortic Z-scores | Stable hemodynamic markers over short-term follow-up despite significant aortic growth using Z-scores. Baseline aortic PV was a predictor of aortic dilation. |
| Bollache et al., 2018 [33] Patients: n = 27 Age = 52 ± 15 years Controls: n = 20 Age = 48 ± 14 years | WSS, Elastic fibers size, Aortic diameter | BAV showed increased WSS associated with elastic fiber thinning. Elastic fiber thinning correlates with impaired tissue biomechanics. |
| Binter et al., 2017 [5] Patients: n = 51 Age = 67 ± 15 years Controls: n = 10 Age = 69 ± 5 years | TKE | Elevated TKE implies higher energy losses associated with BAV. TKE may help to distinguish within the heterogeneous population of patients with moderate to severe AS. |
| van Ooij et al., 2015 [35] Patients: n = 13 Age = 51 ± 17 years Controls: n = 10 Age = 50 ± 14 years | WSS | Elevated WSS was elevated in the ascending aorta and correlated with PV. |
| Barker et al., 2014 [41] Patients with aortic dilation: n = 16 Age = 52 ± 8 years Patients with AV stenosis (age-sex matched): n = 14 Age = 46 ± 15 years Controls: n = 12 Age = 37 ± 10 years | Viscous energy loss | Viscous energy loss was significantly elevated in the thoracic aorta for patients with dilated aorta and patients with aortic stenosis compared to healthy volunteers. Viscous energy loss in patient cohorts was significantly elevated and indicates that cardiac afterload is increased due to abnormal flow. |
| Hope et al., 2014 [37] Patients: n = 13 Age = 26.5 (17–43) years Patients: n = 12 Age = 30.7 (17–64) years | Flow displacement, WSS | Flow displacement is a simple and reproducible hemodynamic marker that shows good correlation with aortic growth in patients with BAV. |
| Meierhofer et al., 2013 [34] Patients: n = 18 Age = 25 (10–44) years Controls: n = 18 Age = 25 (8–42) years | WSS | WSS and flow patterns in the ascending aorta in BAV patients without concomitant valve or vessel disease are significantly different compared with tricuspid aortic valve. Higher shear forces may have an impact on the development of aortic dilation in patients with BAVs. |
| Hope et al., 2011 [31] BAV patients with normal flow: n = 7 Age = 20.4 ± 7.9 years BAV patients with abnormal flow: n = 19 Age = 30.5 ± 12.6 years Controls: n = 20 Age = 26.9 ± 10.4 years | WSS, Eccentric Flow | BAV and eccentric systolic blood flow was found to have elevated WSS. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mansoor, O.; Garcia, J. Clinical Use of Blood Flow Analysis through 4D-Flow Imaging in Aortic Valve Disease. J. Cardiovasc. Dev. Dis. 2023, 10, 251. https://doi.org/10.3390/jcdd10060251
Mansoor O, Garcia J. Clinical Use of Blood Flow Analysis through 4D-Flow Imaging in Aortic Valve Disease. Journal of Cardiovascular Development and Disease. 2023; 10(6):251. https://doi.org/10.3390/jcdd10060251
Chicago/Turabian StyleMansoor, Omer, and Julio Garcia. 2023. "Clinical Use of Blood Flow Analysis through 4D-Flow Imaging in Aortic Valve Disease" Journal of Cardiovascular Development and Disease 10, no. 6: 251. https://doi.org/10.3390/jcdd10060251





