Cardiac Magnetic Resonance Relaxometry Parameters, Late Gadolinium Enhancement, and Feature-Tracking Myocardial Longitudinal Strain in Patients Recovered from COVID-19
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
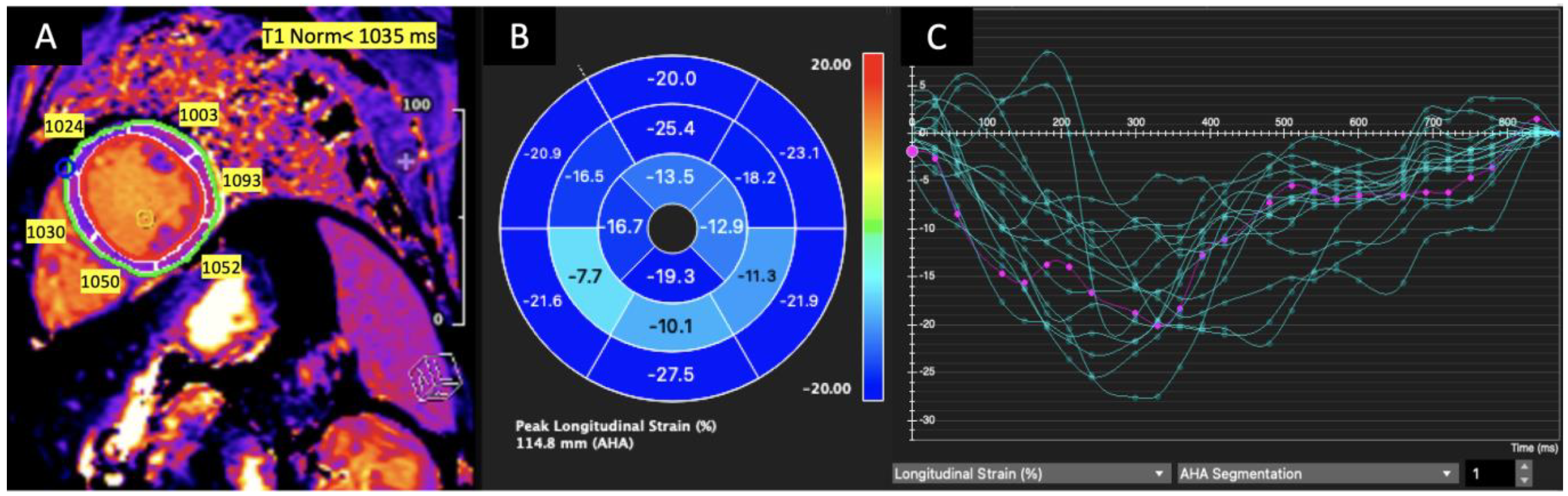
2.2. CMR Image Acquisition and Analysis
2.3. Statistical Analysis
3. Results
4. Discussion
- CMR abnormalities, including myocarditis patterns, are common in patients who have recovered from COVID-19 and presented with protracted symptoms that could have resulted from cardiac involvement.
- Patients with GLS less negative than −15% had significantly lower LVEF and a significantly higher number of segments with prolonged T1.
- Left ventricular GLS was significantly positively correlated with T1 and significantly negatively correlated with LVEF.
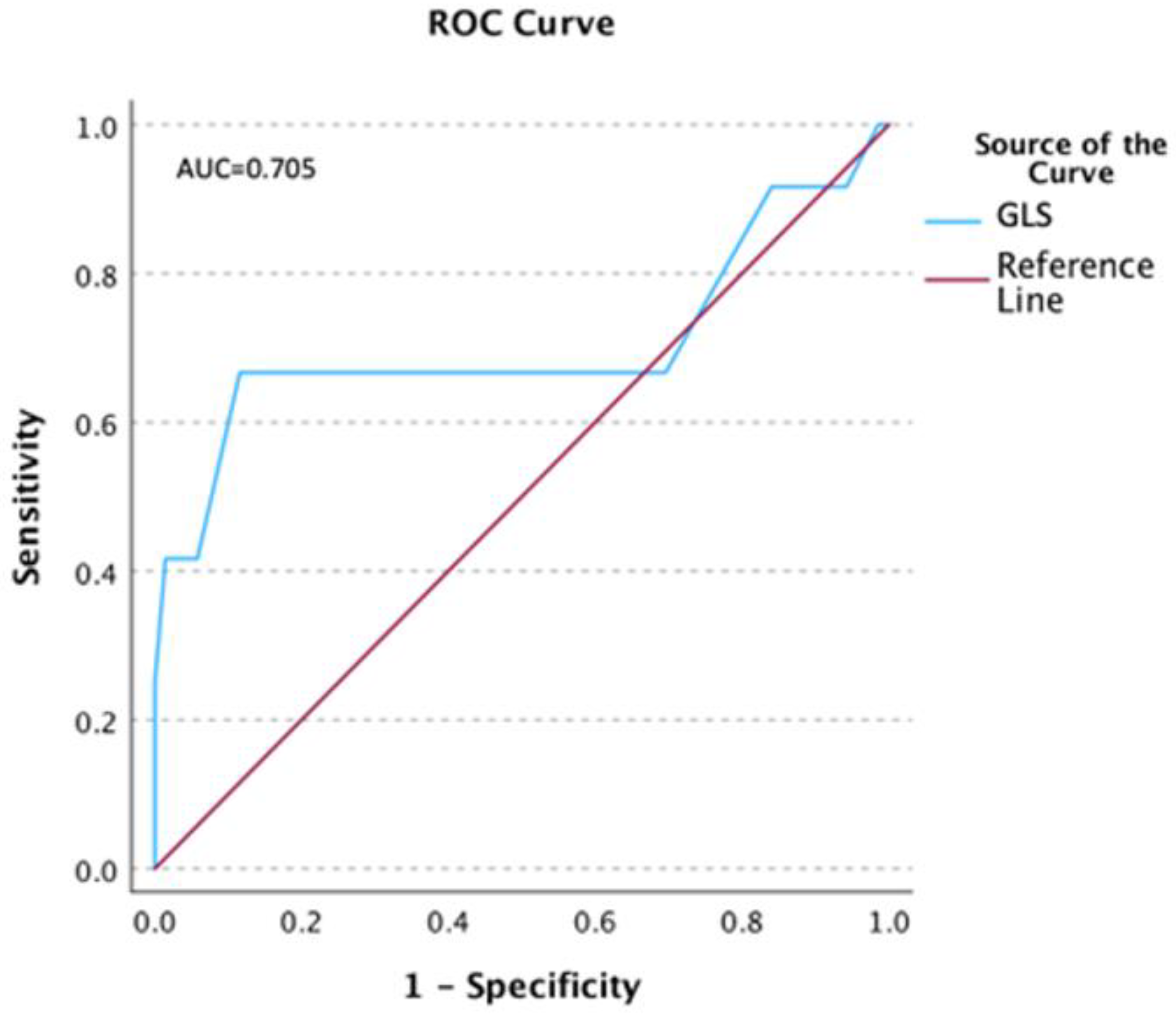
- Left ventricular GLS less negative than −15% was 7.5 times more likely in patients with prolonged T1.
- Reduced longitudinal strain in the basal inferolateral segment had a significant effect on the global left ventricular longitudinal strain.
- ROC results suggested that a GLS of −14.5% predicted prolonged T1 relaxation time with the best combination of sensitivity and specificity.
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhao, Y.H.; Zhao, L.; Yang, X.C.; Wang, P. Cardiovascular complications of SARS-CoV-2 infection (COVID-19): A systematic review and meta-analysis. Rev. Cardiovasc. Med. 2021, 22, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Huang, D.Q.; Zou, B.; Yang, H.; Hui, W.Z.; Rui, F.; Yee, N.T.S.; Liu, C.; Nerurkar, S.N.; Kai, J.C.Y.; et al. Epidemiology of COVID-19: A systematic review and meta-analysis of clinical characteristics, risk factors, and outcomes. J. Med. Virol. 2021, 93, 1449–1458. [Google Scholar] [CrossRef] [PubMed]
- Wojtowicz, D.; Dorniak, K.; Ławrynowicz, M.; Waz, P.; Fijałkowska, J.; Kulawiak-Gałaska, D.; Rejszel-Baranowska, J.; Knut, R.; Haberka, M.; Szurowska, E.; et al. Cardiac magnetic resonance findings in patients recovered from COVID-19 pneumonia and presenting with persistent cardiac symptoms: The TRICITY-CMR trial. Biology 2022, 11, 1848. [Google Scholar] [CrossRef] [PubMed]
- Friedrich, M.G.; Sechtem, U.; Schulz-Menger, J.; Holmvang, G.; Alakija, P.; Cooper, L.T.; White, J.A.; Abdel-Aty, H.; Gutberlet, M.; Prasad, S.; et al. Cardiovascular magnetic resonance in myocarditis: A JACC White Paper. J. Am. Coll. Cardiol. 2009, 53, 1475–1487. [Google Scholar] [CrossRef] [Green Version]
- Ferreira, V.M.; Schulz-Menger, J.; Holmvang, G.; Kramer, C.M.; Carbone, I.; Sechtem, U.; Kindermann, I.; Gutberlet, M.; Cooper, L.T.; Liu, P.; et al. Cardiovascular magnetic resonance in nonischemic myocardial inflammation: Expert recommendations. J. Am. Coll. Cardiol. 2018, 72, 3158–3176. [Google Scholar] [CrossRef]
- Fijałkowska, J.; Sobolewski, J.; Glińska, A.; Piowodzka, I.; Nowak, R.; Zarczynska-Buchowiecka, M.; Pienkowska, J.; Gruchala, M.; Szurowska, E.; Dorniak, K.; et al. Cardiac abnormalities detected by echocardiography and cardiac magnetic resonance in healthcare professionals recovered from non-severe COVID-19. Kardiol. Pol. 2021, 79, 1256–1258. [Google Scholar] [CrossRef]
- Kim, J.Y.; Han, K.; Suh, Y.J. Prevalence of abnormal cardiovascular magnetic resonance findings in recovered patients from COVID-19: A systematic review and meta-analysis. J. Cardiovasc. Magn. Reson. 2021, 23, 100. [Google Scholar] [CrossRef]
- Krishnasamy, R.; Isbel, N.M.; Hawley, C.M.; Pascoe, E.M.; Burrage, M.; Leano, R.; Haluska, B.A.; Marwick, T.H.; Stanton, T. Left ventricular global longitudinal strain (GLS) is a superior predictor of all-cause and cardiovascular mortality when compared to ejection fraction in advanced chronic kidney disease. PLoS ONE 2015, 10, e0127044. [Google Scholar] [CrossRef]
- Karlsen, S.; Dahlslett, T.; Grenne, B.; Sjoli, B.; Smitseth, O.; Edvardsen, T.; Brunvand, H. Global longitudinal strain is a more reproducible measure of left ventricular function than ejection fraction regardless of echocardiographic training. Cardiovasc. Ultrasound 2019, 17, 18. [Google Scholar] [CrossRef] [Green Version]
- Le, T.-T.; Huang, W.; Singh, G.K.; Toh, D.-F.; Ewe, S.H.; Tang, H.C.; Loo, G.; Bryant, J.A.; Ang, B.; Tay, E.L.-W.; et al. Echocardiographic global longitudinal strain is associated with myocardial fibrosis and predicts outcomes in aortic stenosis. Front. Cardiovasc. Med. 2021, 8, 750016. [Google Scholar] [CrossRef]
- Fischer, K.; Obrist, S.J.; Erne, S.A.; Stark, A.W.; Marggraf, M.; Kaneko, K.; Guensch, D.P.; Huber, A.T.; Greulich, S.; Aghayev, A.; et al. Feature tracking myocardial strain incrementally improves prognostication in myocarditis beyond traditional CMR imaging features. JACC Cardiovasc. Imaging 2020, 13, 1891–1901. [Google Scholar] [CrossRef] [PubMed]
- Vo, H.Q.; Marwick, T.H.; Negishi, K. MRI-Derived Myocardial Strain Measures in Normal Subjects. JACC Cardiovasc. Imaging 2018, 11, 196–205. [Google Scholar] [CrossRef] [PubMed]
- Lange, T.; Schuster, A. Quantification of myocardial deformation applying cmrfeature-tracking-all about the left ventricle? Curr. Heart Fail. Rep. 2021, 18, 225–239. [Google Scholar] [CrossRef] [PubMed]
- Baeßler, B.; Treutlein, M.; Schaarschmidt, F.A.; Stehning, C.; Schnackenburg, B.; Michels, G.; Maintz, D.; Bunck, A.C. A novel multiparametric imaging approach to acute myocarditis using T2-mapping and CMR feature tracking. J. Cardiovasc. Magn. Reson. 2017, 19, 71. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kellman, P.; Larson, A.C.; Hsu, L.-Y.; Chung, Y.-C.; Simonetti, O.P.; McVeigh, E.R.; Arai, A.E. Motion-corrected free-breathing delayed enhancement imaging of myocardial infarction. Magn. Reson. Med. 2005, 53, 194–200. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cerqueira, M.D.; Weissman, N.J.; Dilsizian, V.; Jacobs, A.K.; Kaul, S.; Laskey, W.K.; Pennell, D.J.; Rumberger, J.A.; Ryan, T.; American Heart Association Writing Group on Myocardial Segmentation and Registration for Cardiac Imaging; et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 2002, 105, 539–542. [Google Scholar] [CrossRef] [Green Version]
- Messroghli, D.R.; Moon, J.C.; Ferreira, V.M.; Grosse-Wortmann, L.; He, T.; Kellman, P.; Mascherbauer, J.; Nezafat, R.; Salerno, M.; Schelbert, E.B.; et al. Clinical recommendations for cardiovascular magnetic resonance mapping of T1, T2, T2* and extracellular volume: A consensus statement by the society for cardiovascular magnetic resonance (SCMR) endorsed by the European association for cardiovascular imaging (EACVI). J. Cardiovasc. Magn. Reson. 2017, 19, 75. [Google Scholar] [CrossRef] [Green Version]
- Farzaneh-Far, A.; Romano, S. Measuring longitudinal left ventricular function and strain using cardiovascular magnetic resonance imaging. Eur. Heart J. Cardiovasc. Imaging 2019, 20, 1259–1261. [Google Scholar] [CrossRef]
- Lim, C.; Blaszczyk, E.; Riazy, L.; Wiesemann, S.; Schuler, J.; von Knobelsdorff-Brenkenhoff, F.; Schulz-Menger, J. Quantification of myocardial strain assessed by cardiovascular magnetic resonance feature tracking in healthy subjects—Influence of segmentation and analysis software. Eur. Radiol. 2021, 31, 3962–3972. [Google Scholar] [CrossRef]
- Farsalinos, K.E.; Daraban, A.M.; Unlu, S.; Thomas, J.D.; Badano, L.P.; Voigt, J.U. Head-to-head comparison of global longitudinal strain measurements among nine different vendors: The EACVI/ASE Inter-Vendor Comparison Study. J. Am. Soc. Echocardiog. 2015, 28, 1171.e2. [Google Scholar] [CrossRef]
- Romano, S.; Romer, B.; Evans, K.; Trybula, M.; Shenoy, C.; Kwong, R.Y.; Farzaneh-Far, A. Prognostic Implications of Blunted Feature-Tracking Global Longitudinal Strain During Vasodilator Cardiovascular Magnetic Resonance Stress Imaging. JACC Cardiovasc. Imaging 2020, 13, 58–65. [Google Scholar] [CrossRef]
- Shen, M.T.; Yang, Z.G.; Diao, K.Y.; Jiang, L.; Zhang, Y.; Liu, X.; Gao, Y.; Hu, B.Y.; Huang, S.; Guo, Y.K. Left Ventricular Involvement in Arrhythmogenic Right Ventricular Dysplasia/Cardiomyopathy Predicts Adverse Clinical Outcomes: A Cardiovascular Magnetic Resonance Feature Tracking Study. Sci. Rep. 2019, 9, 14235. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, B.H.; Shi, N.N.; Wu, C.W.; An, D.A.; Shi, Y.X.; Wesemann, L.D.; Hu, J.; Xu, J.R.; Shan, F.; Wu, L.M. Early cardiac involvement in patients with acute COVID-19 infection identified by multiparametric cardiovascular magnetic resonance imaging. Eur. Heart J. Cardiovasc. Imaging 2021, 22, 844–851. [Google Scholar] [CrossRef] [PubMed]
- Puntmann, V.O.; Carerj, M.L.; Wieters, I.; Fahim, M.; Arendt, C.; Hoffmann, J.; Shchendrygina, A.; Escher, F.; Vasa-Nicotera, M.; Zeiher, A.M.; et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020, 5, 1265–1273. [Google Scholar] [CrossRef]
- Huang, L.; Zhao, P.; Tang, D.; Zhu, T.; Han, R.; Zhan, C.; Liu, W.; Zeng, H.; Tao, Q.; Xia, L. Cardiac involvement in patients recovered from COVID-2019 identified using magnetic resonance imaging. JACC Cardiovasc. Imaging 2020, 13, 2330–2339. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; Xu, E.; Bowe, B.; Al-Aly, Z. Long-term cardiovascular outcomes of COVID-19. Nat. Med. 2022, 28, 583–590. [Google Scholar] [CrossRef]
- Leitman, M.; Vered, Z.; Tyomkin, V.; Macogon, B.; Moravsky, G.; Peleg, E.; Copel, L. Speckle tracking imaging in inflammatory heart diseases. Int. J. Cardiovasc. Imaging 2018, 34, 787–792. [Google Scholar] [CrossRef]
- Kostakou, P.M.; Kostopoulos, V.S.; Tryfou, E.S.; Giannaris, V.D.; Rodis, I.E.; Olympios, C.D.; Kouris, N.T. Subclinical left ventricular dysfunction and correlation with regional strain analysis in myocarditis with normal ejection fraction. A new diagnostic criteria. Int. J. Cardiol. 2018, 259, 116–121. [Google Scholar] [CrossRef]
- Salehi Ravesh, M.; Eden, M.; Langguth, P.; Piesch, T.C.; Lehmann, J.K.; Lebenatus, A.; Hauttemann, D.; Graessner, J.; Frey, N.; Jansen, O.; et al. Non-contrast enhanced diagnosis of acute myocarditis based on the 17-segment heart model using 2D-feature tracking magnetic resonance imaging. Magn. Reson. Imaging 2020, 65, 155–165. [Google Scholar] [CrossRef]
- Gao, Q.; Yi, W.; Gao, C.; Qi, T.; Li, L.; Xie, K.; Zhao, W.; Chen, W. Cardiac magnetic resonance feature tracking myocardial strain analysis in suspected acute myocarditis: Diagnostic value and association with severity of myocardial injury. BMC Cardiovasc. Disord. 2023, 23, 162. [Google Scholar] [CrossRef]
- Haberka, M.; Rajewska-Tabor, J.; Wojtowicz, D.; Jankowska, A.; Miszalski-Jamka, K.; Janus, M.; Dorniak, K.; Kulawiak-Gałąska, D.; Stasiow, B.; Rozmiarek, S.; et al. A distinct septal pattern of late gadolinium enhancement specific for COVID-induced myocarditis: A multicenter cardiovascular magnetic resonance study. Kardiol. Pol. 2023, 81, 463–471. [Google Scholar] [CrossRef] [PubMed]
- Løgstrup, B.B.; Nielsen, J.M.; Kim, W.Y.; Poulsen, S.H. Myocardial oedema in acute myocarditis detected by echocardiographic 2D myocardial deformation analysis. Eur. Heart J. Cardiovasc. Imaging 2016, 17, 1018–1026. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luetkens, J.A.; Schlesinger-Irsch, U.; Kuetting, D.L.; Dabir, D.; Homsi, R.; Doerner, J.; Schmeel, F.C.; Fimmers, R.; Sprinkart, A.M.; Naehle, C.P.; et al. Feature-tracking myocardial strain analysis in acute myocarditis: Diagnostic value and association with myocardial oedema. Eur. Radiol. 2017, 27, 4661–4671. [Google Scholar] [CrossRef]
- Baeßler, B.; Schaarschmidt, F.; Dick, A.; Michels, G.; Maintz, D.; Bunck, A.C. Diagnostic implications of magnetic resonance feature tracking derived myocardial strain parameters in acute myocarditis. Eur. J. Radiol. 2016, 85, 218–227. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, V.M.; Piechnik, S.K.; Dall’Armellina, E.; Karamitsos, T.D.; Francis, J.M.; Choudhury, R.P.; Friedrich, M.G.; Robson, M.D.; Neubauer, S. Noncontrast T1-mapping detects acute myocardial edema with high diagnostic accuracy: A comparison to T2-weighted cardiovascular magnetic resonance. J. Cardiovasc. Magn. Reson. 2012, 14, 42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mileva, N.; Paolisso, P.; Gallinoro, E.; Fabbricatore, D.; Munhoz, D.; Bergamaschi, L.; Belmonte, M.; Panayotov, P.; Pizzi, C.; Barbato, E.; et al. Diagnostic and Prognostic Role of Cardiac Magnetic Resonance in MINOCA: Systematic Review and Meta-Analysis. JACC Cardiovasc. Imaging 2023, 16, 376–389. [Google Scholar] [CrossRef]
- Gaibazzi, N.; Bergamaschi, L.; Pizzi, C.; Tuttolomondo, D. Resting global longitudinal strain and stress echocardiography to detect coronary artery disease burden. Eur. Heart J. Cardiovasc. Imaging 2023, 24, e86–e88. [Google Scholar] [CrossRef]
| Age, years | 41.8 ± 10.6 |
| Female, n (%) | 59 (73) |
| BMI, kg/m2 | 25.8 ± 4.4 |
History | |
| Smoking, n (%) | 5 (6.0) |
| Hyperlipidemia, n (%) | 3 (4.0) |
| Chronic kidney disease, n (%) | 1 (1.2) |
| Hypertension, n (%) | 13 (16) |
| Bronchial asthma, n (%) | 5 (6.0) |
| Hyperthyroidism, n (%) | 12 (15) |
Clinical presentation | |
| Respiratory symptoms, n (%) | 43 (53) |
| Chest pain, n (%) | 42 (52) |
| Palpitation, n (%) | 47 (58) |
| Dyspnea, n (%) | 28 (35) |
Initial blood testing | |
| Troponin I, ng/mL | 0.003 ± 0.001 |
| Hemoglobin, g/dL | 13.8 ± 1.3 |
| CRP, mg/L | 3.2 ± 5.2 |
| Hematocrit, (%) | 40.4 ± 3.6 |
| Glucose, mg/dL | 94.3 ± 10.1 |
| LVEF, (%) | 59.4 ± 5.9 |
| GLS More Negative or Equal −15 n = 53 | GLS Less Negative than −15 n = 28 | p | |
|---|---|---|---|
| T1(ms), mean ± SD | 1004.1 ± 23.0 | 1007.7 ± 37.0 | 0.642 |
| T1 > norm, (>1035 ms) | 4 (7.5) | 8 (28.6) | 0.019 |
| T2 (ms), mean ± SD | 47.5 ± 1.8 | 47.6 ± 3.8 | 0.898 |
| T2 > norm, (>49 ms) | 14 (26.4) | 7 (25.0) | 0.89 |
| ECV (%), mean ± SD | 27.0 ± 2.2 | 28.3 ± 8.9 | 0.519 |
| ECV > norm, (>29%) | 7 (13.2) | 6 (21.4) | 0.356 |
| LVEF (%), mean ± SD | 61.6 ± 4.8 | 53.6 ± 8.9 | <0.001 |
| LGE (+) | 30 (56.6) | 22 (78.6) | 0.05 |
| GLS (%) | ||
|---|---|---|
| r | p | |
| T1 (ms) | 0.303 | 0.006 |
| T2 (ms) | 0.193 | 0.084 |
| ECV (%) | −0.049 | 0.667 |
| LVEF (%) | −0.732 | <0.001 |
| GLS Less Negative than −15% | Univariate Logistic Regression | Multivariate Logistic Regression | ||
|---|---|---|---|---|
| p | p | HR | 95% CI | |
| High global T1 (ms) | 0.017 | 0.028 | 7.62 | 1.25–46.64 |
| High global T2 (ms) | 0.89 | 0.313 | 0.51 | 0.14–1.88 |
| High global ECV (%) | 0.342 | 0.584 | 0.61 | 0.10–3.66 |
| LGE (+) | 0.054 | 0.079 | 2.69 | 0.89–8.16 |
| GLS Less Negative than −15 Continuous Variables | Univariate Logistic Regression | Multivariate Logistic Regression | ||
|---|---|---|---|---|
| p | p | HR | 95% CI | |
| SLS seg 5 | 0.001 | 0.039 | 1.66 | 1.03–2.68 |
| T1 seg 5 | 0.016 | 0.748 | 1.01 | 0.96–1.06 |
| T2 seg 5 | 0.423 | |||
| ECV seg 5 | 0.268 | |||
| SLS seg 6 | 0.01 | 0.279 | 1.17 | 0.88–1.57 |
| T1 seg 6 | 0.009 | 0.409 | 1.03 | 0.97–1.09 |
| T2 seg 6 | 0.655 | |||
| ECV seg 6 | 0.123 | |||
| SLS seg 10 | 0.002 | 0.952 | 0.99 | 0.71–1.39 |
| T1 seg 10 | 0.089 | 0.371 | 0.98 | 0.93–1.03 |
| T2 seg 10 | 0.782 | |||
| ECV seg 10 | 0.232 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fijalkowska, J.; Glinska, A.; Fijalkowski, M.; Sienkiewicz, K.; Kulawiak-Galaska, D.; Szurowska, E.; Pienkowska, J.; Dorniak, K. Cardiac Magnetic Resonance Relaxometry Parameters, Late Gadolinium Enhancement, and Feature-Tracking Myocardial Longitudinal Strain in Patients Recovered from COVID-19. J. Cardiovasc. Dev. Dis. 2023, 10, 278. https://doi.org/10.3390/jcdd10070278
Fijalkowska J, Glinska A, Fijalkowski M, Sienkiewicz K, Kulawiak-Galaska D, Szurowska E, Pienkowska J, Dorniak K. Cardiac Magnetic Resonance Relaxometry Parameters, Late Gadolinium Enhancement, and Feature-Tracking Myocardial Longitudinal Strain in Patients Recovered from COVID-19. Journal of Cardiovascular Development and Disease. 2023; 10(7):278. https://doi.org/10.3390/jcdd10070278
Chicago/Turabian StyleFijalkowska, Jadwiga, Anna Glinska, Marcin Fijalkowski, Katarzyna Sienkiewicz, Dorota Kulawiak-Galaska, Edyta Szurowska, Joanna Pienkowska, and Karolina Dorniak. 2023. "Cardiac Magnetic Resonance Relaxometry Parameters, Late Gadolinium Enhancement, and Feature-Tracking Myocardial Longitudinal Strain in Patients Recovered from COVID-19" Journal of Cardiovascular Development and Disease 10, no. 7: 278. https://doi.org/10.3390/jcdd10070278
APA StyleFijalkowska, J., Glinska, A., Fijalkowski, M., Sienkiewicz, K., Kulawiak-Galaska, D., Szurowska, E., Pienkowska, J., & Dorniak, K. (2023). Cardiac Magnetic Resonance Relaxometry Parameters, Late Gadolinium Enhancement, and Feature-Tracking Myocardial Longitudinal Strain in Patients Recovered from COVID-19. Journal of Cardiovascular Development and Disease, 10(7), 278. https://doi.org/10.3390/jcdd10070278







