Abstract
Patients with ST-elevation myocardial infarction (STEMI) treated with primary percutaneous coronary intervention (PCI) may demonstrate distal microvascular embolization of thrombotic materials. We retrospectively examined 20 cases displaying extensive thrombus in the infarct-related artery (IRA), treated either with a two-step procedure, with interim tirofiban infusion, or immediate stent implantation. Distal embolization tended to be more common in the latter strategy, but, overall, the outcome was comparable. Thus, a two-staged procedure may be considered in selected cases of primary PCI associated with high thrombus burden.
Primary PCI is the preferred reperfusion strategy in patients with STEMI; however, its value is compromised by distal micro-embolization, occurring in as many as 10% of cases of apparently successful procedures [1]. The extent of the angiographic thrombus has been identified as a powerful predictor of such events, which are mediated by vasoconstrictors and inflammatory cytokines released from neutrophil-platelet aggregations [2]. In the presence of a high thrombus burden, the approach of acutely restoring blood flow without stenting has been examined [3,4,5], although the results were conflicting. Deferred-stenting was disfavored after the results of a larger trial [6], which showed no effect on major clinical outcomes. Regardless, the debate resurfaced after the findings of three meta-analyses [7,8,9], indicating lower risk for myocardial injury by this approach.
To contribute to the ongoing discussions, we retrospectively examined cases of STEMI treated with primary PCI during the calendar year 2017, displaying extensive thrombus in the infarct-related artery. Of 34 such cases identified, 12 were excluded because of multi-vessel disease, and 2 because of concurrent anticoagulation. A two-stage procedure, consisting of acute restoration of blood flow in the absence of stenting, followed by tirofiban infusion and repeat angiogram after 3 days was followed in 10 cases. These patients, hereafter referred to as deferred-stenting group, were compared with the remaining 10 patients, referred to as immediate-stenting group. As shown in Table 1, the demographic, clinical, and angiographic characteristics were similar in the two groups.

Table 1.
Baseline characteristics (SD: standard deviation; NS: non significant; CABG: coronary artery bypass grafting; LAD: left anterior descending artery; LCx: left circumflex artery; RCA: right coronary artery; TIMI: thrombolysis in myocardial infarction).
All angiograms showed totally occluded IRA, with adequate (TIMI ≥ 2) flow restored after dilatation with a small-diameter balloon. Aspiration thrombectomy as an adjunctive therapy was not used with any patient. All patients referred to significant relief of pain and there was more than 50% ST-segment resolution in the single lead showing maximum ST segment at baseline ECG. The presence of a high thrombus burden (defined as thrombus length ≥ 2× diameter) was confirmed after quantification by the TIMI scoring system. In the deferred-stenting group, the first PCI was followed by an initial bolus tirofiban administration of 25 μg/kg given over a 3-min period in the catheterization laboratory, followed by a continuous intravenous infusion (0.15 μg/kg/min for 24 h) and subcutaneous enoxaparin (1mg/kg every 12 h), based on the previously demonstrated efficacy of this regimen on thrombus burden [3]; repeat coronary angiography was performed after 72 ± 16 h.
We compared angiographic and clinical variables, as well as indices of myocardial necrosis between the two groups. Categorical variables were compared with chi-square, whereas normally distributed continuous variables (as per Kolmogorov–Smirnov) were compared with t-test; significance was set at p < 0.05.
No re-occlusion of the infarct-related artery or major bleeding was recorded during hospital stay. Distal embolization was noted in three patients after immediate-stenting, but was absent after deferred-stenting. However, myocardial blush grades, peak troponin levels, and final left ventricular ejection fraction did not differ between the two groups, as seen in Table 2.

Table 2.
Outcome (SD: standard deviation; NS: non significant).
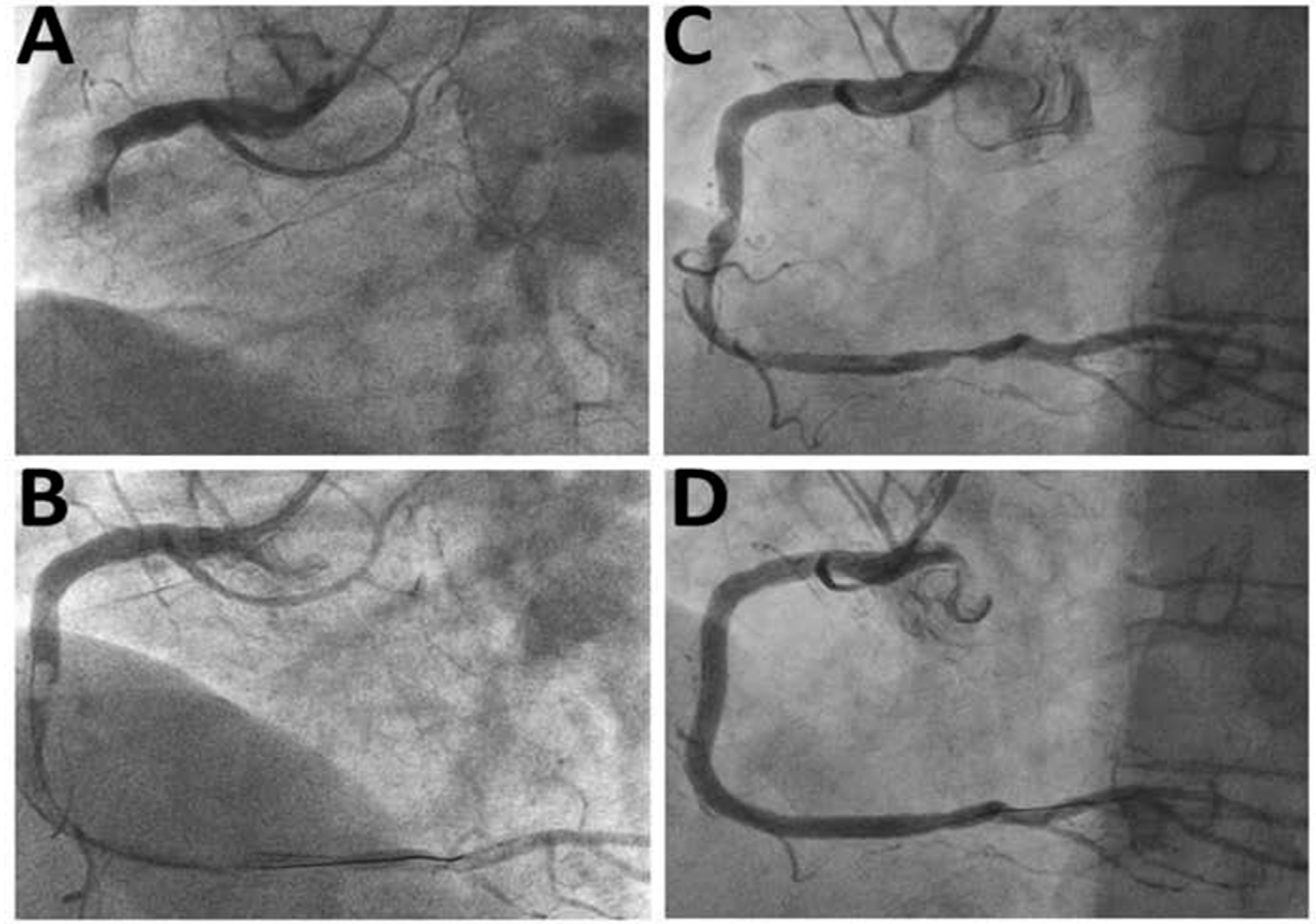
Thrombus burden decreased markedly during the second PCI in the deferred-stenting group, whereas the stenosis severity was lower than the immediate-stenting group. In three patients in the deferred-stenting group displaying stenoses <50%, no stents were implanted during the procedure. Figure 1 shows a representative example from the deferred-stenting group.
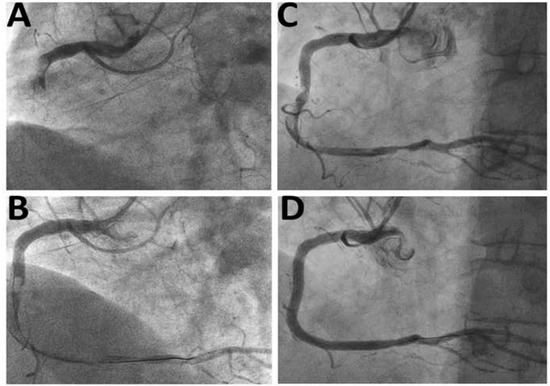
Figure 1.
Representative case managed by deferred-stenting. (A) Presentation with total occlusion of the right coronary artery and high thrombus burden; (B) Restoration of satisfactory coronary flow after dilatation with 2.0 mm balloon. Note the extensive thrombus occupying large part of the right coronary artery; (C) Repeat angiogram after 48 h showing decreased thrombus burden; (D) Final result after stent implantation.
In addition to its retrospective design, the major limitation of the study is the small number of patients; hence, the information provided here should be examined only in the context of previous reports [3,4,5,6,7,8,9], Under this prism, our results indicate that deferred-stenting during STEMI may be considered in the presence of high thrombus burden, provided that an adequate coronary flow is established by minimal intervention during the initial PCI. This approach may decrease distal embolization, albeit without apparent effect on final infarct size or overall left ventricular function. Short-term tirofiban infusion decreases thrombus burden and may obviate the need for stent implantation in some patients. We feel that the deferred-stenting approach is presented as an option in selected cases, deemed at high risk for microvascular obstruction, until further data are available from the ongoing PRIMACY trial [10].
Author Contributions
Conceptualization, X.M.S. and D.N.N.; methodology, X.M.S. and D.N.N.; software, X.M.S. and G.I.K.; validation, X.M.S., A.P.E., and D.G.S.; formal analysis, X.M.S., K.V.S., and S.D.P.; investigation, X.M.S. and D.N.N.; data curation, X.M.S. and D.N.N.; writing—original draft preparation, X.M.S.; writing—review and editing, T.M.K. and D.N.N.; visualization, T.M.K. and D.N.N.; supervision, T.M.K.; project administration, D.N.N. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of University Hospital of Ioannina.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available within the article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Niccoli, G.; Scalone, G.; Lerman, A.; Crea, F. Coronary microvascular obstruction in acute myocardial infarction. Eur. Heart J. 2016, 37, 1024–1033. [Google Scholar] [CrossRef] [PubMed]
- Nikas, D.N.; Chatziathanasiou, G.; Kotsia, A.; Papamichael, N.; Thomas, C.; Papafaklis, M.; Naka, K.K.; Kazakos, N.; Milionis, H.J.; Vakalis, K.; et al. Effect of intravenous administration of antioxidants alone and in combination on myocardial reperfusion injury in an experimental pig model. Curr. Ther. Res. Clin. Exp. 2008, 69, 423–439. [Google Scholar] [CrossRef] [PubMed]
- Carrick, D.; Oldroyd, K.G.; McEntegart, M.; Haig, C.; Petrie, M.C.; Eteiba, H.; Hood, S.; Owens, C.; Watkins, S.; Layland, J.; et al. A randomized trial of deferred stenting versus immediate stenting to prevent no- or slow-reflow in acute ST-segment elevation myocardial infarction (DEFER-STEMI). J. Am. Coll. Cardiol. 2014, 63, 2088–2098. [Google Scholar] [CrossRef]
- Belle, L.; Motreff, P.; Mangin, L.; Rangé, G.; Marcaggi, X.; Marie, A.; Ferrier, N.; Dubreuil, O.; Zemour, G.; Souteyrand, G.; et al. Comparison of Immediate With Delayed Stenting Using the Minimalist Immediate Mechanical Intervention Approach in Acute ST-Segment-Elevation Myocardial Infarction: The MIMI Study. Circ. Cardiovasc. Interv. 2016, 9, e003388. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.S.; Lee, H.J.; Woong Yu, C.; Kim, Y.M.; Hong, S.J.; Park, J.H.; Choi, R.K.; Choi, Y.J.; Park, J.S.; Kim, T.H.; et al. INNOVATION Study (Impact of Immediate Stent Implantation Versus Deferred Stent Implantation on Infarct Size and Microvascular Perfusion in Patients With ST-Segment-Elevation Myocardial Infarction). Circ. Cardiovasc. Interv. 2016, 9. [Google Scholar] [CrossRef] [PubMed]
- Kelbæk, H.; Høfsten, D.E.; Køber, L.; Helqvist, S.; Kløvgaard, L.; Holmvang, L.; Jørgensen, E.; Pedersen, F.; Saunamäki, K.; De Backer, O.; et al. Deferred versus conventional stent implantation in patients with ST-segment elevation myocardial infarction (DANAMI 3-DEFER): An open-label, randomised controlled trial. Lancet 2016, 387, 2199–2206. [Google Scholar] [CrossRef]
- Qiao, J.; Pan, L.; Zhang, B.; Wang, J.; Zhao, Y.; Yang, R.; Du, H.; Jiang, J.; Jin, C.; Xiong, E. Deferred Versus Immediate Stenting in Patients With ST-Segment Elevation Myocardial Infarction: A Systematic Review and Meta-Analysis. J. Am. Heart Assoc. 2017, 6. [Google Scholar] [CrossRef]
- De Maria, G.L.; Alkhalil, M.; Oikonomou, E.K.; Wolfrum, M.; Choudhury, R.P.; Banning, A.P. Role of deferred stenting in patients with ST elevation myocardial infarction treated with primary percutaneous coronary intervention: A systematic review and meta-analysis. J. Interv. Cardiol. 2017, 30, 264–273. [Google Scholar] [CrossRef]
- Cassese, S.; Belle, L.; Ndrepepa, G.; Bosson, J.L.; Fusaro, M.; Lønborg, J.; Ahtarovski, K.A.; Kelbæk, H. Deferred vs Immediate Stenting in Primary Percutaneous Coronary Intervention: A Collaborative Meta-analysis of Randomized Trials With Cardiac Magnetic Resonance Imaging Data. Can. J. Cardiol. 2018, 34, 1573–1580. [Google Scholar] [CrossRef] [PubMed]
- Jolicoeur, E.M.; Dendukuri, N.; Belisle, P.; Range, G.; Souteyrand, G.; Bouisset, F.; Zemour, G.; Delarche, N.; Harbaoui, B.; Schampaert, E.; et al. Immediate vs Delayed Stenting in ST-Elevation Myocardial Infarction: Rationale and Design of the International PRIMACY Bayesian Randomized Controlled Trial. Can. J. Cardiol. 2020, 36, 1805–1814. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).