Invasive Aspergillosis by Aspergillus flavus: Epidemiology, Diagnosis, Antifungal Resistance, and Management
Abstract
1. Introduction
2. Literature Review
3. Clinical Spectrum and Distribution
3.1. Invasive Aspergillosis
3.1.1. Pulmonary Aspergillosis
3.1.2. CNS Aspergillosis
3.1.3. Endophthalmitis Due to A. flavus
3.1.4. Invasive Fungal Rhinosinusitis
3.1.5. Cardiac Aspergillosis
3.1.6. Cutaneous and Subcutaneous Aspergillosis
3.1.7. Bone and Joint Infections
4. Diagnosis
5. Outbreaks
6. Taxonomy and Identification
7. Molecular Epidemiology
7.1. Genotyping by Random Amplified Polymorphic DNA (RAPD)
7.2. Restriction Fragment Length Polymorphisms (RFLP)
7.3. Single Strand Confirmation Polymorphism (SSCP)
7.4. Amplified Fragment Length Polymorphism (AFLP)
7.5. Multilocus Microsatellite Typing (MLMT)
7.6. Multi-Locus Sequence Typing (MLST)
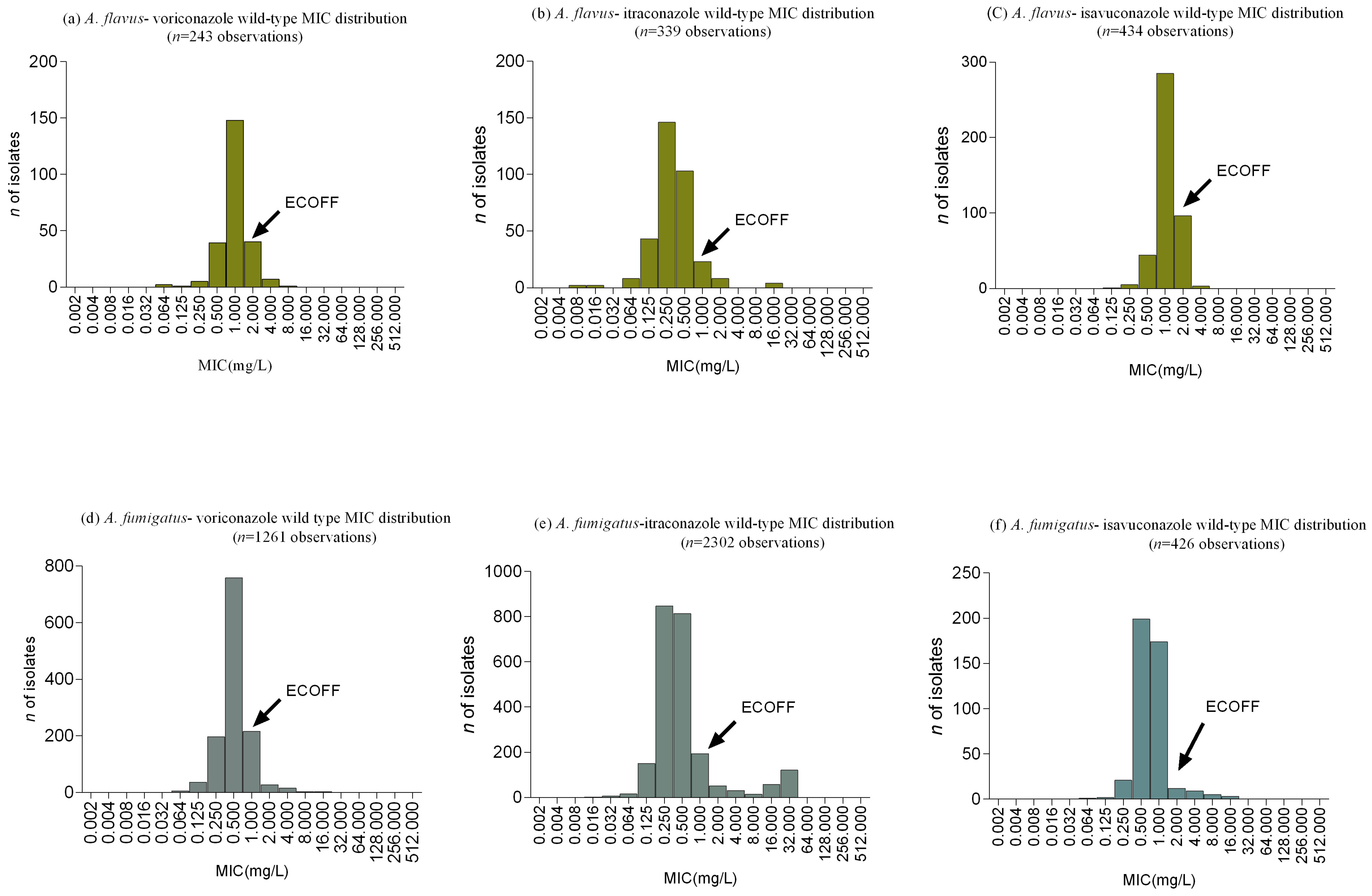
8. Antifungal Susceptibility and Wild Type Distribution
9. Antifungal Resistance
9.1. Mutations in the Cyp51 Gene and Azole Resistance
9.2. Azole Resistance and Gene Expression
9.3. Azole Resistance and Exposure to Environmental Fungicides
9.4. Polyene Resistance
10. Clinical Management of Aspergillosis Due to A. flavus
11. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Sugui, J.A.; Kwon-Chung, K.J.; Juvvadi, P.R.; Latgé, J.-P.; Steinbach, W.J. Aspergillus fumigatus and related species. Cold Spring Harb. Perspect. Med. 2014, 5, a019786. [Google Scholar] [CrossRef] [PubMed]
- Barnes, P.D.; Marr, K.A. Aspergillosis: Spectrum of disease, diagnosis, and treatment. Infect. Dis. Clin. North Am. 2006, 20, 545–561. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, S.; Manavathu, E.K.; Chandrasekar, P.H. Aspergillus flavus: An emerging non- fumigatus Aspergillus species of significance. Mycoses 2009, 52, 206–222. [Google Scholar] [CrossRef] [PubMed]
- Mosquera, J.; Warn, P.A.; Morrissey, J.; Moore, C.B.; Gil-Lamaignere, C.; Denning, D.W. Susceptibility testing of Aspergillus flavus: Inoculum dependence with itraconazole and lack of correlation between susceptibility to amphotericin B in-vitro and outcome in-vivo. Antimicrob. Agents Chemother. 2001, 45, 1456–1462. [Google Scholar] [CrossRef] [PubMed]
- Chakrabarti, A.; Chatterjee, S.S.; Das, A.; Shivaprakash, M.R. Invasive aspergillosis in developing countries. Med. Mycol. 2011, 49, S35–S47. [Google Scholar] [CrossRef] [PubMed]
- Pasqualotto, A.C. Differences in pathogenicity and clinical syndromes due to Aspergillus fumigatus and Aspergillus flavus. Med. Mycol. 2009, 47 (Suppl 1), S261–S270. [Google Scholar] [CrossRef] [PubMed]
- Hyde, K.D.; Al-Hatmi, A.M.S.; Andersen, B.; Boekhout, T.; Buzina, W.; Dawson, T.L., Jr.; Eastwood, D.C.; Jones, E.B.G.; De Hoog, S.; Kang, Y.; et al. The world’s ten most feared fungi. Fungal Divers. 2018, 9, 161–194. [Google Scholar] [CrossRef]
- Engel, T.G.P.; Erren, E.; Melchers, W.J.G.; Reijers, M.H.; Merkus, P.; Verweij, P.E. Aerosol transmission of Aspergillus fumigatus in cystic fibrosis patients in the Netherlands. Emerg. Infect. Dis. 2019, 25, 797–799. [Google Scholar] [CrossRef]
- Abdalla, M.H. Prevalence of airborne Aspergillus flavus in Khartoum (Sudan) airspora with reference to dusty weather and inoculum survival in simulated summer conditions. Mycopathologia 1988, 104, 137–141. [Google Scholar] [CrossRef]
- Adhikari, A.; Sen, M.M.; Gupta-Bhattacharya, S.; Chanda, S. Airborne viable, non-viable, and allergenic fungi in a rural agricultural area of India: A 2-year study at five outdoor sampling stations. Sci. Total Environ. 2004, 326, 123–141. [Google Scholar] [CrossRef]
- Gupta, S.K.; Pereira, B.M.; Singh, A.B. Survey of airborne culturable and non-culturable fungi at different sites in Delhi metropolis. Asian Pacific J. Allergy Immunol. 1993, 11, 19–28. [Google Scholar]
- Rotjanapan, P.; Chen, Y.C.; Chakrabarti, A.; Li, R.Y.; Rudramurthy, S.M.; Yu, J.; Kung, H.C.; Watcharananan, S.; Tan, A.L.; Saffari, S.E.; et al. Epidemiology and clinical characteristics of invasive mould infections: A multicenter, retrospective analysis in five Asian countries. Med. Mycol. 2018, 56, 186–196. [Google Scholar] [CrossRef] [PubMed]
- Chakrabarti, A.; Kaur, H.; Savio, J.; Rudramurthy, S.M.; Patel, A.; Shastri, P.; Pamidimukkala, U.; Karthik, R.; Bhattacharya, S.; Kindo, A.J.; et al. Epidemiology and clinical outcomes of invasive mould infections in Indian intensive care units (FISF study). J. Crit. Care 2019, 51, 64–70. [Google Scholar] [CrossRef] [PubMed]
- Al-Hatmi, A.M.S.; Castro, M.A.; de Hoog, G.S.; Badali, H.; Alvarado, V.F.; Verweij, P.E.; Meis, J.F.; Zago, V.V. Epidemiology of Aspergillus species causing keratitis in Mexico. Mycoses 2019, 62, 144–151. [Google Scholar] [CrossRef]
- Van de Veerdonk, F.L.; Kolwijck, E.; Lestrade, P.P.A.; Hodiamont, C.J.; Rijnders, B.J.A.; van Paassen, J.; Haas, P.-J.; Oliveira dos Santos, C.; Kampinga, G.A.; Bergmans, D.C.J.J.; et al. Influenza-associated aspergillosis in critically ill patients. Am. J. Respir. Crit. Care Med. 2017, 196, 524–527. [Google Scholar] [CrossRef]
- Schauwvlieghe, A.F.A.D.; Rijnders, B.J.A.; Philips, N.; Verwijs, R.; Vanderbeke, L.; Van Tienen, C.; Lagrou, K.; Verweij, P.E.; Van de Veerdonk, F.L.; Gommers, D.; et al. Invasive aspergillosis in patients admitted to the intensive care unit with severe influenza: a retrospective cohort study. Lancet Respir. Med. 2018, 6, 782–792. [Google Scholar] [CrossRef]
- Huang, L.; Zhang, N.; Huang, X.; Xiong, S.; Feng, Y.; Zhang, Y.; Li, M.; Zhan, Q. Invasive pulmonary aspergillosis in patients with influenza infection: A retrospective study and review of the literature. Clin. Respir. J. 2019, 13, 202–211. [Google Scholar] [CrossRef]
- Lueg, E.A.; Ballagh, R.H.; Forte, V. Analysis of the recent cluster of invasive fungal sinusitis at the Toronto Hospital for Sick Children. J. Otolaryngol. 1996, 25, 366–370. [Google Scholar]
- Arnow, P.M.; Sadigh, M.; Costas, C.; Weil, D.; Chudy, R. Endemic and epidemic aspergillosis associated with in-hospital replication of Aspergillus organisms. J. Infect. Dis. 1991, 164, 998–1002. [Google Scholar] [CrossRef]
- Saghrouni, F.; Ben Youssef, Y.; Gheith, S.; Bouabid, Z.; Ben Abdeljelil, J.; Khammari, I.; Fathallah, A.; Khlif, A.; Ben Saïd, M. Twenty-nine cases of invasive aspergillosis in neutropenic patients. Med. Mal. Infect. 2011, 41, 657–662. [Google Scholar] [CrossRef]
- Pasqualotto, A.C.; Denning, D.W. An aspergilloma caused by Aspergillus flavus. Med. Mycol. 2008, 46, 275–278. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Araujo, R.; Rodrigues, A.G. Variability of germinative potential among pathogenic species of Aspergillus. J. Clin. Microbiol. 2004, 42, 4335–4337. [Google Scholar] [CrossRef] [PubMed]
- Zarrinfar, H.; Mirhendi, H.; Makimura, K.; Satoh, K.; Khodadadi, H.; Paknejad, O. Use of mycological, nested PCR, and real-time PCR methods on BAL fluids for detection of Aspergillus fumigatus and A. flavus in solid organ transplant recipients. Mycopathologia 2013, 176, 377–385. [Google Scholar] [CrossRef] [PubMed]
- Staib, F.; Rajendran, C.; Mishra, S.K.; Voigt, R.; Lindlar, F.; Hartmann, C.; Weber, R.; Nowotny, P. An atypical Aspergillus flavus from a case of bronchopulmonary aspergilloma. A contribution to the cultural and serological diagnosis of A. flavus infections. Zentralbl. Bakteriol. Mikrobiol. Hyg. A 1983, 255, 361–367. [Google Scholar] [CrossRef]
- Shankar, S.; Mahadevan, A.; Sundaram, C.; Sarkar, C.; Chacko, G.; Lanjewar, D.; Santosh, V.; Yasha, T.; Radhakrishnan, V. Pathobiology of fungal infections of the central nervous system with special reference to the Indian scenario. Neurol. India 2007, 55, 198–215. [Google Scholar] [CrossRef] [PubMed]
- DeLone, D.R.; Goldstein, R.A.; Petermann, G.; Salamat, M.S.; Miles, J.M.; Knechtle, S.J.; Brown, W.D. Disseminated aspergillosis involving the brain: distribution and imaging characteristics. Am. J. Neuroradiol. 1999, 20, 1597–1604. [Google Scholar]
- Kleinschmidt-DeMasters, B.K. Central nervous system aspergillosis: A 20-year retrospective series. Hum. Pathol. 2002, 33, 116–124. [Google Scholar] [CrossRef]
- Torre-Cisneros, J.; Lopez, O.L.; Kusne, S.; Martinez, A.J.; Starz, T.E.; Simmons, R.L.; Martin, M. CNS aspergillosis in organ transplantation: A clinicopathological study. J. Neurol. Neurosurg. Psychiatry 1993, 56, 188–193. [Google Scholar] [CrossRef]
- Hedayati, M.T.; Pasqualotto, A.C.; Warn, P.A.; Bowyer, P.; Denning, D.W. Aspergillus flavus: Human pathogen, allergen and mycotoxin producer. Microbiology 2007, 153, 1677–1692. [Google Scholar] [CrossRef]
- Chakrabarti, A.; Shivaprakash, M.R.; Singh, R.; Tarai, B.; George, V.K.; Fomda, B.A.; Gupta, A. Fungal endophthalmitis: fourteen years’ experience from a center in India. Retina 2008, 28, 1400–1407. [Google Scholar] [CrossRef]
- Narang, S.; Gupta, A.; Gupta, V.; Dogra, M.R.; Ram, J.; Panday, S.S.; Chakrabarti, A. Fungal endophthalmitis following cataract surgery: Clinical presentation, microbiological spectrum, and outcome. Am. J. Ophthalmol. 2001, 132, 609–617. [Google Scholar] [CrossRef]
- Joseph, J.; Sontam, B.; Guda, S.J.M.; Gandhi, J.; Sharma, S.; Tyagi, M.; Dave, V.P.; Das, T. Trends in microbiological spectrum of endophthalmitis at a single tertiary care ophthalmic hospital in India: A review of 25 years. Eye 2019, s41433-019-0380. [Google Scholar] [CrossRef] [PubMed]
- DeShazo, R.D.; Chapin, K.; Swain, R.E. Fungal Sinusitis. N. Engl. J. Med. 1997, 337, 254–259. [Google Scholar] [CrossRef] [PubMed]
- Michael, R.C.; Michael, J.S.; Ashbee, R.H.; Mathews, M.S. Mycological profile of fungal sinusitis: An audit of specimens over a 7-year period in a tertiary care hospital in Tamil Nadu. Indian J. Pathol. Microbiol. 2008, 51, 493–496. [Google Scholar] [CrossRef] [PubMed]
- Goncer, I.; Denning, D.W. Chronic Aspergillus Sinusitis. Available online: https://www.aspergillus.org.uk/content/chronic-aspergillus-sinusitis (accessed on 10 May 2019).
- Schubert, M.S. Allergic fungal sinusitis: Pathophysiology, diagnosis and management. Med. Mycol. 2009, 47, S324–S330. [Google Scholar] [CrossRef] [PubMed]
- Chakrabarti, A.; Rudramurthy, S.M.; Panda, N.; Das, A.; Singh, A. Epidemiology of chronic fungal rhinosinusitis in rural India. Mycoses 2015, 58, 294–302. [Google Scholar] [CrossRef] [PubMed]
- Chakrabarti, A.; Denning, D.W.; Ferguson, B.J.; Ponikau, J.; Buzina, W.; Kita, H.; Marple, B.; Panda, N.; Vlaminck, S.; Kauffmann-Lacroix, C.; et al. Fungal rhinosinusitis: A categorization and definitional schema addressing current controversies. Laryngoscope 2009, 119, 1809–1818. [Google Scholar] [CrossRef]
- Pasqualotto, A.C.; Denning, D.W. Post-operative aspergillosis. Clin. Microbiol. Infect. 2006, 12, 1060–1076. [Google Scholar] [CrossRef]
- Marroni, M.; Cao, P.; Repetto, A.; Prattichizzo, L.; Parlani, G.; Fiorio, M. Aspergillus flavus infection of an aortic bypass. Eur. J. Clin. Microbiol. Infect. Dis. 2001, 20, 439–441. [Google Scholar] [CrossRef]
- Brili, S.; Rokas, C.; Tzannos, K.; Barbetseas, J.; Pirounaki, M.; Stefanadis, C. Fungal ascending aortic aneurysm after cardiac surgery. Echocardiography 2009, 26, 84–87. [Google Scholar] [CrossRef]
- Villate, J.I.; Aldamiz-Echevarria, G.; Gaztelurrutia, L.; Barrenechea, J.I.; de Zárate, P.G. Cardiac aspergillosis. J. Thorac. Cardiovasc. Surg. 2000, 119, 403–404. [Google Scholar] [CrossRef][Green Version]
- Alsobayeg, S.; Alshehri, N.; Mohammed, S.; Fadel, B.M.; Omrani, A.S.; Almaghrabi, R.S. Aspergillus flavus native valve endocarditis following combined liver and renal transplantation: Case report and review of the literature. Transpl. Infect. Dis. 2018, 20, e12891. [Google Scholar] [CrossRef] [PubMed]
- Bernardeschi, C.; Foulet, F.; Ingen-Housz-Oro, S.; Ortonne, N.; Sitbon, K.; Quereux, G.; Lortholary, O.; Chosidow, O.; Bretagne, S. Cutaneous invasive aspergillosis. Medicine (Baltimore) 2015, 94, e1018. [Google Scholar] [CrossRef] [PubMed]
- Florio, M.; Marroni, M.; Morosi, S.; Stagni, G. Nosocomial Aspergillus flavus wound infections following cardiac surgery. Infez. Med. 2004, 12, 270–273. [Google Scholar] [PubMed]
- Nenoff, P.; Horn, L.C.; Schwenke, H.; Mierzwa, M.; Rieske, K.; Haustein, U.F. Invasive mold infections in the university clinics of Leipzig in the period from 1992–1994. Mycoses 1996, 39 (Suppl 1), S107–S112. [Google Scholar] [CrossRef]
- Bassiri-Jahromi, S. Mycetoma in Iran: Causative agents and geographic distribution. Indian J. Dermatol. 2014, 59, 529. [Google Scholar] [CrossRef]
- Mahgoub, E.S. Can Aspergillus flavus cause maduromycetoma? Bull. Soc. Pathol. Exot. Filiales 1973, 66, 390–395. [Google Scholar]
- Padhi, S.; Uppin, S.G.; Uppin, M.S.; Umabala, P.; Challa, S.; Laxmi, V.; Prasad, V.B.N. Mycetoma in South India: retrospective analysis of 13 cases and description of two cases caused by unusual pathogens: Neoscytalidium dimidiatum and Aspergillus flavus. Int. J. Dermatol. 2010, 49, 1289–1296. [Google Scholar] [CrossRef]
- Gabrielli, E.; Fothergill, A.W.; Brescini, L.; Sutton, D.A.; Marchionni, E.; Orsetti, E.; Staffolani, S.; Castelli, P.; Gesuita, R.; Barchiesi, F. Osteomyelitis caused by Aspergillus species: A review of 310 reported cases. Clin. Microbiol. Infect. 2014, 20, 559–565. [Google Scholar] [CrossRef]
- Koehler, P.; Tacke, D.; Cornely, O.A. Aspergillosis of bones and joints—A review from 2002 until today. Mycoses 2014, 57, 323–335. [Google Scholar] [CrossRef]
- Gamaletsou, M.N.; Rammaert, B.; Bueno, M.A.; Sipsas, N.V.; Moriyama, B.; Kontoyiannis, D.P.; Roilides, E.; Zeller, V.; Taj-Aldeen, S.J.; Henry, M.; et al. Aspergillus arthritis: Analysis of clinical manifestations, diagnosis, and treatment of 31 reported cases. Med. Mycol. 2017, 55, 246–254. [Google Scholar] [PubMed]
- Swanink, C.M.A.; Meis, J.F.G.M.; Rijs, A.J.M.M.; Donnelly, J.P.; Verweij, P.E. Specificity of a sandwich enzyme-linked immunosorbent assay for detecting Aspergillus galactomannan. J. Clin. Microbiol. 1997, 35, 257–260. [Google Scholar] [PubMed]
- Xavier, M.O.; Araujo, J.S.V.; Aquino, V.R.; Severo, C.B.; Guazzelli, L.S.; Severo, L.C.; Pasqualotto, A.C. Variability in galactomannan detection by platelia Aspergillus EIATM according to the Aspergillus species. Rev. Inst. Med. Trop. Sao Paulo 2013, 55, 145–147. [Google Scholar] [CrossRef] [PubMed]
- Hachem, R.Y.; Kontoyiannis, D.P.; Chemaly, R.F.; Jiang, Y.; Reitzel, R.; Raad, I. Utility of galactomannan enzyme immunoassay and (1,3) beta-D-glucan in diagnosis of invasive fungal infections: low sensitivity for Aspergillus fumigatus infection in hematologic malignancy patients. J. Clin. Microbiol. 2009, 47, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Taghizadeh-Armaki, M.; Hedayati, M.T.; Moqarabzadeh, V.; Ansari, S.; Mahdavi Omran, S.; Zarrinfar, H.; Saber, S.; Verweij, P.E.; Denning, D.W.; Seyedmousavi, S. Effect of involved Aspergillus species on galactomannan in bronchoalveolar lavage of patients with invasive aspergillosis. J. Med. Microbiol. 2017, 66, 898–904. [Google Scholar] [CrossRef] [PubMed]
- Badiee, P.; Alborzi, A.; Karimi, M.; Pourabbas, B.; Haddadi, P.; Mardaneh, J.; Moieni, M. Diagnostic potential of nested PCR, galactomannan EIA, and beta-D-glucan for invasive aspergillosis in pediatric patients. J. Infect. Dev. Ctries. 2012, 6, 352–357. [Google Scholar] [CrossRef] [PubMed]
- Khan, Z.U.; Ahmad, S.; Mokaddas, E.; Said, T.; Nair, M.P.; Halim, M.A.; Nampoory, M.R.; McGinnis, M.R. Cerebral aspergillosis diagnosed by detection of Aspergillus flavus-specific DNA, galactomannan and (1->3)- -D-glucan in clinical specimens. J. Med. Microbiol. 2007, 56, 129–132. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Walsh, T.J.; Wissel, M.C.; Grantham, K.J.; Petraitiene, R.; Petraitis, V.; Kasai, M.; Francesconi, A.; Cotton, M.P.; Hughes, J.E.; Greene, L.; et al. Molecular detection and species-specific identification of medically important Aspergillus species by Real-Time PCR in experimental invasive pulmonary aspergillosis. J. Clin. Microbiol. 2011, 49, 4150–4157. [Google Scholar] [CrossRef]
- Denning, D.W. Invasive Aspergillosis. Clin. Infect. Dis. 1998, 26, 781–805. [Google Scholar] [CrossRef]
- Kanamori, H.; Rutala, W.A.; Sickbert-Bennett, E.E.; Weber, D.J. Review of fungal outbreaks and infection prevention in healthcare settings during construction and renovation. Clin. Infect. Dis. 2015, 61, 433–444. [Google Scholar] [CrossRef]
- Zeyni, F.; Hedayati, M.T. Study of airbourne fungi in the wards of 3 Teheran hospitals. J. Med. Counc. Islam. Repub. Iran 1995, 13, 17–20. [Google Scholar]
- Hedayati, M.T.; Mayahi, S.; Aghili, R.; Goharimoghadam, K. Airborne fungi in indoor and outdoor of asthmatic patients’ home, living in the city of Sari. Iran. J. Allergy, Asthma Immunol. 2005, 4, 189–191. [Google Scholar]
- Haiduven, D. Nosocomial aspergillosis and building construction. Med. Mycol. 2009, 47, 210–216. [Google Scholar] [CrossRef] [PubMed]
- Rudramurthy, S.; Singh, G.; Hallur, V.; Verma, S.; Chakrabarti, A. High fungal spore burden with predominance of Aspergillus in hospital air of a tertiary care hospital in Chandigarh. Indian J. Med. Microbiol. 2016, 34, 529–532. [Google Scholar] [CrossRef] [PubMed]
- Loo, V.G.; Bertrand, C.; Dixon, C.; Vityé, D.; DeSalis, B.; McLean, A.P.; Brox, A.; Robson, H.G. Control of construction-associated nosocomial aspergillosis in an antiquated hematology unit. Infect. Control Hosp. Epidemiol. 1996, 17, 360–364. [Google Scholar] [CrossRef]
- Thio, C.L.; Smith, D.; Merz, W.G.; Streifel, A.J.; Bova, G.; Gay, L.; Miller, C.B.; Perl, T.M. Refinements of environmental assessment during an outbreak investigation of invasive aspergillosis in a leukemia and bone marrow transplant unit. Infect. Control Hosp. Epidemiol. 2000, 21, 18–23. [Google Scholar] [CrossRef] [PubMed]
- Burwen, D.R.; Lasker, B.A.; Rao, N.; Durry, E.; Padhye, A.A.; Jarvis, W.R. Invasive aspergillosis outbreak on a Hematology-Oncology ward. Infect. Control Hosp. Epidemiol. 2001, 22, 45–48. [Google Scholar] [CrossRef]
- Berthelot, P.; Loulergue, P.; Raberin, H.; Turco, M.; Mounier, C.; Tran Manh Sung, R.; Lucht, F.; Pozzetto, B.; Guyotat, D. Efficacy of environmental measures to decrease the risk of hospital-acquired aspergillosis in patients hospitalised in haematology wards. Clin. Microbiol. Infect. 2006, 12, 738–744. [Google Scholar] [CrossRef][Green Version]
- Vonberg, R.-P.; Gastmeier, P. Nosocomial aspergillosis in outbreak settings. J Hosp Infect 2006, 63, 246–254. [Google Scholar] [CrossRef]
- Amaike, S.; Keller, N.P. Aspergillus flavus. Annu. Rev. Phytopathol. 2011, 49, 107–133. [Google Scholar] [CrossRef]
- Samson, R.A.; Visagie, C.M.; Houbraken, J.; Hong, S.-B.; Hubka, V.; Klaassen, C.H.W.; Perrone, G.; Seifert, K.A.; Susca, A.; Tanney, J.B.; et al. Phylogeny, identification and nomenclature of the genus Aspergillus. Stud. Mycol. 2014, 78, 141–173. [Google Scholar] [CrossRef] [PubMed]
- Visagie, C.M.; Hirooka, Y.; Tanney, J.B.; Whitfield, E.; Mwange, K.; Meijer, M.; Amend, A.S.; Seifert, K.A.; Samson, R.A. Aspergillus, Penicillium and Talaromyces isolated from house dust samples collected around the world. Stud. Mycol. 2014, 78, 63–139. [Google Scholar] [CrossRef] [PubMed]
- Varga, J.; Frisvad, J.C.; Samson, R.A. Two new aflatoxin producing species, and an overview of Aspergillus section Flavi. Stud. Mycol. 2011, 69, 57–80. [Google Scholar] [CrossRef] [PubMed]
- Horn, B.W.; Moore, G.G.; Carbone, I. Sexual reproduction in Aspergillus flavus. Mycologia 2009, 101, 423–429. [Google Scholar] [CrossRef] [PubMed]
- Geiser, D.M.; Pitt, J.I.; Taylor, J.W. Cryptic speciation and recombination in the aflatoxin-producing fungus Aspergillus flavus. Proc. Natl. Acad. Sci. USA 1998, 95, 388–393. [Google Scholar] [CrossRef]
- Payne, G.A.; Nierman, W.C.; Wortman, J.R.; Pritchard, B.L.; Brown, D.; Dean, R.A.; Bhatnagar, D.; Cleveland, T.E.; Machida, M.; Yu, J. Whole genome comparison of Aspergillus flavus and A. oryzae. Med. Mycol. 2006, 44 (Suppl 1), S9–S11. [Google Scholar] [CrossRef] [PubMed]
- Al-Wathiqi, F.; Ahmad, S.; Khan, Z. Molecular identification and antifungal susceptibility profile of Aspergillus flavus isolates recovered from clinical specimens in Kuwait. BMC Infect. Dis. 2013, 13, 126. [Google Scholar] [CrossRef]
- Hadrich, I.; Makni, F.; Ayadi, A.; Ranque, S. Microsatellite typing to trace Aspergillus flavus infections in a hematology unit. J. Clin. Microbiol. 2010, 48, 2396–2401. [Google Scholar] [CrossRef]
- Heinemann, S.; Symoens, F.; Gordts, B.; Jannes, H.; Nolard, N. Environmental investigations and molecular typing of Aspergillus flavus during an outbreak of postoperative infections. J. Hosp. Infect. 2004, 57, 149–155. [Google Scholar] [CrossRef]
- Diaz-Guerra, T.M.; Mellado, E.; Cuenca-Estrella, M.; Gaztelurrutia, L.; Navarro, J.I.V.; Tudela, J.L.R. Genetic similarity among one Aspergillus flavus strain isolated from a patient who underwent heart surgery and two environmental strains obtained from the operating room. J. Clin. Microbiol. 2000, 38, 2419–2422. [Google Scholar]
- Leenders, A.; Van Belkum, A.; Janssen, S.; De Marie, S.; Kluytmans, J.; Wielenga, J.; Lowenberg, B.; Lowenberg, L.; Verbrugh, H. Molecular epidemiology of apparent outbreak of invasive aspergillosis in a hematology ward. J. Clin. Microbiol. 1996, 34, 345–351. [Google Scholar] [PubMed]
- Meunier, J.R.; Grimont, P.A. Factors affecting reproducibility of random amplified polymorphic DNA fingerprinting. Res. Microbiol. 1993, 144, 373–379. [Google Scholar] [CrossRef]
- Moody, S.F.; Tyler, B.M. Restriction enzyme analysis of mitochondrial DNA of the Aspergillus flavus group: A. flavus, A. parasiticus, and A. nomius. Appl. Environ. Microbiol. 1990, 56, 2441–2452. [Google Scholar] [PubMed]
- Bagyalakshmi, R.; Lily Therese, K.; Madhavan, H.N. Nucleotide polymorphisms associated with Internal Transcribed Spacer (ITS) regions of ocular isolates of Aspergillus flavus. J. Microbiol. Methods 2007, 68, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Buffington, J.; Reporter, R.; Lasker, B.A.; McNeil, M.M.; Lanson, J.M.; Ross, L.A.; Mascola, L.; Jarvis, W.R. Investigation of an epidemic of invasive aspergillosis: utility of molecular typing with the use of random amplified polymorphic DNA probes. Pediatr. Infect. Dis. J. 1994, 13, 386–393. [Google Scholar] [CrossRef]
- McAlpin, C.E.; Mannarelli, B. Construction and characterization of a DNA probe for distinguishing strains of Aspergillus flavus. Appl. Environ. Microbiol. 1995, 61, 1068–1072. [Google Scholar] [PubMed]
- Kumeda, Y.; Asao, T. Single-strand conformation polymorphism analysis of PCR-amplified ribosomal DNA internal transcribed spacers to differentiate species of Aspergillus section Flavi. Appl. Environ. Microbiol. 1996, 62, 2947–2952. [Google Scholar]
- Montiel, D.; Dickinson, M.J.; Lee, H.A.; Dyer, P.S.; Jeenes, D.J.; Roberts, I.N.; James, S.; Fuller, L.J.; Matsuchima, K.; Archer, D.B. Genetic differentiation of the Aspergillus section Flavi complex using AFLP fingerprints. Mycol. Res. 2003, 107, 1427–1434. [Google Scholar] [CrossRef]
- Rudramurthy, S.M.; de Valk, H.A.; Chakrabarti, A.; Meis, J.F.; Klaassen, C.H.W. High resolution genotyping of clinical Aspergillus flavus isolates from India using microsatellites. PLoS ONE 2011, 6, e16086. [Google Scholar] [CrossRef]
- Grubisha, L.C.; Cotty, P.J. Genetic isolation among sympatric vegetative compatibility groups of the aflatoxin-producing fungus Aspergillus flavus. Mol. Ecol. 2010, 19, 269–280. [Google Scholar] [CrossRef]
- Taghizadeh-Armaki, M.; Hedayati, M.T.; Ansari, S.; Omran, S.M.; Saber, S.; Rafati, H.; Zoll, J.; van der Lee, H.A.; Melchers, W.J.G.; Verweij, P.E.; et al. Genetic diversity and in vitro antifungal susceptibility of 200 clinical and environmental Aspergillus flavus isolates. Antimicrob. Agents Chemother. 2017, 61, e00004-17. [Google Scholar] [CrossRef] [PubMed]
- Choi, M.J.; Won, E.J.; Joo, M.Y.; Park, Y.-J.; Kim, S.H.; Shin, M.G.; Shin, J.H. Microsatellite typing and resistance mechanism analysis of voriconazole-resistant Aspergillus flavus isolates in South Korean hospitals. Antimicrob. Agents Chemother. 2019, 63, e01610-18. [Google Scholar] [CrossRef] [PubMed]
- Hadrich, I.; Neji, S.; Drira, I.; Trabelsi, H.; Mahfoud, N.; Ranque, S.; Makni, F.; Ayadi, A. Microsatellite typing of Aspergillus flavus in patients with various clinical presentations of aspergillosis. Med. Mycol. 2013, 51, 586–591. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Guarro, J.; Solé, M.; Castany, R.; Cano, J.; Teixidó, A.; Pujol, I.; Gené, J.; Castro, A.; Sarda, P. Use of random amplified microsatellites to type isolates from an outbreak of nosocomial aspergillosis in a general medical ward. Med. Mycol. 2005, 43, 365–371. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wang, D.Y.; Hadj-Henni, L.; Thierry, S.; Arné, P.; Chermette, R.; Botterel, F.; Hadrich, I.; Makni, F.; Ayadi, A.; Ranque, S.; et al. Simple and highly discriminatory VNTR-based multiplex PCR for tracing sources of Aspergillus flavus isolates. PLoS ONE 2012, 7, e44204. [Google Scholar] [CrossRef] [PubMed]
- Klaassen, C.H.W. MLST versus microsatellites for typing Aspergillus fumigatus isolates. Med. Mycol. 2009, 47, 27–33. [Google Scholar] [CrossRef]
- Meis, J.F.; Chowdhary, A.; Rhodes, J.L.; Fisher, M.C.; Verweij, P.E. Clinical implications of globally emerging azole resistance in Aspergillus fumigatus. Philos. Trans. R. Soc. B Biol. Sci. 2016, 371. [Google Scholar] [CrossRef]
- Verweij, P.E.; Chowdhary, A.; Melchers, W.J.G.; Meis, J.F. Azole resistance in Aspergillus fumigatus: Can we retain the clinical use of mold-active antifungal azoles? Clin. Infect. Dis. 2016, 62, 362–368. [Google Scholar] [CrossRef]
- Chowdhary, A.; Sharma, C.; Meis, J.F. Azole-resistant aspergillosis: Epidemiology, molecular mechanisms, and treatment. J. Infect. Dis. 2017, 216, S436–S444. [Google Scholar] [CrossRef]
- Gonçalves, S.S.; Souza, A.C.R.; Chowdhary, A.; Meis, J.F.; Colombo, A.L. Epidemiology and molecular mechanisms of antifungal resistance in Candida and Aspergillus. Mycoses 2016, 59, 198–219. [Google Scholar] [CrossRef]
- Ullmann, A.J.; Aguado, J.M.; Arikan-Akdagli, S.; Denning, D.W.; Groll, A.H.; Lagrou, K.; Lass-Flörl, C.; Lewis, R.E.; Munoz, P.; Verweij, P.E.; et al. Diagnosis and management of Aspergillus diseases: executive summary of the 2017 ESCMID-ECMM-ERS guideline. Clin. Microbiol. Infect. 2018, 24, e1–e38. [Google Scholar] [CrossRef] [PubMed]
- Pfaller, M.; Boyken, L.; Hollis, R.; Kroeger, J.; Messer, S.; Tendolkar, S.; Diekema, D. Use of epidemiological cutoff values to examine 9-Year trends in susceptibility of Aspergillus Species to the triazoles. J. Clin. Microbiol. 2011, 49, 586–590. [Google Scholar] [CrossRef] [PubMed]
- Paul, R.A.; Rudramurthy, S.M.; Dhaliwal, M.; Singh, P.; Ghosh, A.K.; Kaur, H.; Varma, S.; Agarwal, R.; Chakrabarti, A. Magnitude of voriconazole resistance in clinical and environmental isolates of Aspergillus flavus and investigation into the role of multidrug efflux pumps. Antimicrob. Agents Chemother. 2018, 62, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Sharma, C.; Kumar, R.; Kumar, N.; Masih, A.; Gupta, D.; Chowdhary, A. Investigation of multiple resistance mechanisms in voriconazole-resistant Aspergillus flavus clinical isolates from a chest hospital surveillance in Delhi, India. Antimicrob. Agents Chemother. 2018, 62, 529. [Google Scholar] [CrossRef] [PubMed]
- Baddley, J.W.; Marr, K.A.; Andes, D.R.; Walsh, T.J.; Kauffman, C.A.; Kontoyiannis, D.P.; Ito, J.I.; Balajee, S.A.; Pappas, P.G.; Moser, S.A. Patterns of susceptibility of Aspergillus isolates recovered from patients enrolled in the transplant-associated infection surveillance network. J. Clin. Microbiol. 2009, 47, 3271–3275. [Google Scholar] [CrossRef] [PubMed]
- Araujo, R.; Pina-Vaz, C.; Rodrigues, A.G. Susceptibility of environmental versus clinical strains of pathogenic Aspergillus. Int. J. Antimicrob. Agents 2007, 29, 108–111. [Google Scholar] [CrossRef] [PubMed]
- Espinel-ingroff, A.; Cuenca-estrella, M.; Cantón, E. EUCAST and CLSI: Working together towards a harmonized method for antifungal susceptibility testing. Curr. Fungal Infect. Rep. 2013, 7, 59–67. [Google Scholar] [CrossRef]
- Espinel-Ingroff, A.; Diekema, D.J.; Fothergill, A.; Johnson, E.; Pelaez, T.; Pfaller, M.A.; Rinaldi, M.G.; Canton, E.; Turnidge, J. Wild-type MIC distributions and epidemiological cutoff values for the triazoles and six Aspergillus spp. for the CLSI broth microdilution method (M38-A2 document). J. Clin. Microbiol. 2010, 48, 3251–3257. [Google Scholar] [CrossRef]
- Lalitha, P.; Sun, C.Q.; Prajna, N.V.; Karpagam, R.; Geetha, M.; O’Brien, K.S.; Cevallos, V.; McLeod, S.D.; Acharya, N.R.; Lietman, T.M.; et al. In vitro susceptibility of filamentous fungal isolates from a corneal ulcer clinical trial. Am. J. Ophthalmol. 2014, 157, 318–326. [Google Scholar] [CrossRef]
- Shivaprakash, M.R.; Geertsen, E.; Chakrabarti, A.; Mouton, J.W.; Meis, J.F. In-vitro susceptibility of 188 clinical and environmental isolates of Aspergillus flavus for the new triazole isavuconazole and seven other antifungal drugs. Mycoses 2011, 54, e583-9. [Google Scholar] [CrossRef]
- Espinel-Ingroff, A.; Chowdhary, A.; Gonzalez, G.M.; Lass-Flörl, C.; Martin-Mazuelos, E.; Meis, J.; Peláez, T.; Pfaller, M.A.; Turnidge, J. Multicenter study of isavuconazole MIC distributions and epidemiological cutoff values for Aspergillus spp. for the CLSI M38-A2 broth microdilution method. Antimicrob. Agents Chemother. 2013, 57, 3823–3828. [Google Scholar] [CrossRef] [PubMed]
- Espinel-Ingroff, A.; Fothergill, A.; Fuller, J.; Johnson, E.; Pelaez, T.; Turnidge, J. Wild-type MIC distributions and epidemiological cutoff values for caspofungin and Aspergillus spp. for the CLSI broth microdilution method (M38-A2 Document). Antimicrob. Agents Chemother. 2011, 55, 2855–2859. [Google Scholar] [CrossRef] [PubMed]
- Espinel-Ingroff, A.; Cuenca-Estrella, M.; Fothergill, A.; Fuller, J.; Ghannoum, M.; Johnson, E.; Pelaez, T.; Pfaller, M.A.; Turnidge, J. Wild-type MIC distributions and epidemiological cutoff values for amphotericin B and Aspergillus spp. for the CLSI broth microdilution method (M38-A2 Document). Antimicrob. Agents Chemother. 2011, 55, 5150–5154. [Google Scholar] [CrossRef] [PubMed]
- Jiwa, S.; Shokoples, S.; Turnbull, L.; Jansen, B.; Fuller, J. Antifungal susceptibility of Aspergillus isolates from a Canadian hospital using epidemiological cut-off values (ECOFFs). Poster presented at 23rd ECCMID 2013, Berlin, Germany, 27–30 April 2013. [Google Scholar]
- Rudramurthy, S.M.; Chakrabarti, A.; Geertsen, E.; Mouton, J.W.; Meis, J.F. In vitro activity of isavuconazole against 208 Aspergillus flavus isolates in comparison with 7 other antifungal agents: assessment according to the methodology of the European Committee on Antimicrobial Susceptibility Testing. Diagn. Microbiol. Infect. Dis. 2011, 71, 370–377. [Google Scholar] [CrossRef] [PubMed]
- Espinel-Ingroff, A.; Turnidge, J.; Alastruey-Izquierdo, A.; Botterel, F.; Canton, E.; Castro, C.; Chen, Y.-C.C.; Chen, Y.-C.C.; Chryssanthou, E.; Dannaoui, E.; et al. Method-dependent epidemiological cutoff values for detection of triazole resistance in Candida and Aspergillus species for the Sensititre Yeastone colorimetric broth and etest agar diffusion methods. Antimicrob. Agents Chemother. 2019, 63, e01651-18. [Google Scholar] [CrossRef] [PubMed]
- Pfaller, M.A.; Boyken, L.; Hollis, R.J.; Kroeger, J.; Messer, S.A.; Tendolkar, S.; Diekema, D.J. Wild-type minimum effective concentration distributions and epidemiologic cutoff values for caspofungin and Aspergillus spp. as determined by Clinical and Laboratory Standards Institute broth microdilution methods. Diagn. Microbiol. Infect. Dis. 2010, 67, 56–60. [Google Scholar] [CrossRef]
- Espinel-Ingroff, A.; Arendrup, M.; Canton, E.; Cordob, S.; Dannaoui, E.; Garcia-Rodriguez, J.; Gonzalez, G.M.; Govender, N.P.; Martin-Mazuelos, E.; Lackner, M.; et al. Multicenter study of method-dependent epidemiological cutoff values for detection of resistance in Candida spp. and Aspergillus spp. to amphotericin B and echinocandins for the etest agar diffusion method. Antimicrob. Agents Chemother. 2017, 61, 1792–1808. [Google Scholar] [CrossRef]
- Liu, W.; Sun, Y.; Chen, W.; Liu, W.; Wan, Z.; Bu, D.; Li, R. The T788G Mutation in the cyp51C gene confers voriconazole resistance in Aspergillus flavus causing aspergillosis. Antimicrob. Agents Chemother. 2012, 56, 2598–2603. [Google Scholar] [CrossRef]
- Krishnan-Natesan, S.; Chandrasekar, P.H.; Alangaden, G.J.; Manavathu, E.K. Molecular characterisation of cyp51A and cyp51B genes coding for P450 14α-lanosterol demethylases A (CYP51Ap) and B (CYP51Bp) from voriconazole-resistant laboratory isolates of Aspergillus flavus. Int. J. Antimicrob. Agents 2008, 32, 519–524. [Google Scholar] [CrossRef]
- Paul, R.A.; Rudramurthy, S.M.; Meis, J.F.; Mouton, J.W.; Chakrabarti, A. A novel Y319H substitution in cyp51C associated with azole resistance in Aspergillus flavus. Antimicrob. Agents Chemother. 2015, 59, 6615–6619. [Google Scholar] [CrossRef]
- Coleman, J.J.; Mylonakis, E. Efflux in fungi: La pièce de résistance. PLoS Pathog. 2009, 5, e1000486. [Google Scholar] [CrossRef] [PubMed]
- Fattahi, A.; Zaini, F.; Kordbacheh, P.; Rezaie, S.; Safara, M.; Fateh, R.; Farahyar, S.; Kanani, A.; Heidari, M. Evaluation of mRNA expression levels of cyp51A and mdr1, candidate genes for voriconazole resistance in Aspergillus flavus. Jundishapur J. Microbiol. 2015, 8, e26990. [Google Scholar] [CrossRef] [PubMed]
- Natesan, S.K.; Lamichchane, A.K.; Swaminathan, S.; Wu, W. Differential expression of ATP-binding cassette and/or major facilitator superfamily class efflux pumps contributes to voriconazole resistance in Aspergillus flavus. Diagn. Microbiol. Infect. Dis. 2013, 76, 458–463. [Google Scholar] [CrossRef] [PubMed]
- Fraczek, M.G.; Bromley, M.; Buied, A.; Moore, C.B.; Rajendran, R.; Rautemaa, R.; Ramage, G.; Denning, D.W.; Bowyer, P. The cdr1B efflux transporter is associated with non-cyp51A-mediated itraconazole resistance in Aspergillus fumigatus. J. Antimicrob. Chemother. 2013, 68, 1486–1496. [Google Scholar] [CrossRef] [PubMed]
- Ukai, Y.; Kuroiwa, M.; Kurihara, N.; Naruse, H.; Homma, T.; Maki, H.; Naito, A. Contributions of yap1 mutation and subsequent atrF upregulation to voriconazole resistance in Aspergillus flavus. Antimicrob. Agents Chemother. 2018, 62, e01216-18. [Google Scholar] [CrossRef] [PubMed]
- Lass-Flörl, C.; Kofler, G.; Kropshofer, G.; Hermans, J.; Kreczy, A.; Dierich, M.P.; Niederwieser, D. In vitro testing of susceptibility to amphotericin B is a reliable predictor of clinical outcome in invasive aspergillosis. J. Antimicrob. Chemother. 1998, 42, 497–502. [Google Scholar] [CrossRef] [PubMed]
- Hadrich, I.; Makni, F.; Neji, S.; Cheikhrouhou, F.; Bellaaj, H.; Elloumi, M.; Ayadi, A.; Ranque, S. Amphotericin B in vitro resistance is associated with fatal Aspergillus flavus infection. Med. Mycol. 2012, 50, 829–834. [Google Scholar] [CrossRef]
- Badiee, P.; Alborzi, A.; Moeini, M.; Haddadi, P.; Farshad, S.; Japoni, A.; Ziyaeyan, M. Antifungal susceptibility of the Aspergillus species by Etest and CLSI reference methods. Arch. Iran. Med. 2012, 15, 429–432. [Google Scholar]
- Reichert-Lima, F.; Lyra, L.; Pontes, L.; Moretti, M.L.; Pham, C.D.; Lockhart, S.R.; Schreiber, A.Z. Surveillance for azoles resistance in Aspergillus spp. highlights a high number of amphotericin B-resistant isolates. Mycoses 2018, 61, 360–365. [Google Scholar] [CrossRef]
- Taylor, E.; Ferreira, G.; Freitas, G.; Ferreira, R.; de Assis Santos, D.; de Resende-Stoianoff, M. Screening of antifungal susceptibility in cave-dwelling aspergilli and report of an amphotericin B-resistant Aspergillus flavus. Int. J. Speleol. 2017, 46, 369–378. [Google Scholar] [CrossRef]
- European Committee on Antimicrobial Susceptibility Testing. Data from the EUCAST MIC Distribution. Available online: http://www.eucast.org (accessed on 30 May 2019).
- Arendrup, M.C.; Cuenca-Estrella, M.; Lass-Flörl, C.; Hope, W.; European Committee on Antimicrobial Susceptibility Testing Subcommittee on Antifungal Susceptibility Testing (EUCAST-AFST). EUCAST Technical Note on Aspergillus and amphotericin B, itraconazole, and posaconazole. Clin. Microbiol. Infect. 2012, 18, E248–E250. [Google Scholar] [CrossRef] [PubMed]
- CLSI. Epidemiological Cuttoff Values for Antifungal Susceptibility Testing, 2nd ed.; CLSI supplement M59; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2018. [Google Scholar]
- Walsh, T.J.; Anaissie, E.J.; Denning, D.W.; Herbrecht, R.; Kontoyiannis, D.P.; Marr, K.A.; Morrison, V.A.; Segal, B.H.; Steinbach, W.J.; Stevens, D.A.; et al. Treatment of Aspergillosis: Clinical Practice Guidelines of the Infectious Diseases Society of America. 2008, 46, 327–360. [Google Scholar] [CrossRef] [PubMed]
- Patterson, T.F.; Nguyen, M.H.; Segal, B.H.; Steinbach, W.J.; Stevens, D.A.; Walsh, T.J.; Wingard, J.R.; Young, J.-A.H.; Bennett, J.E.; Thompson, G.R., III; et al. Practice guidelines for the diagnosis and management of aspergillosis: 2016 update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2016, 63, e1–e60. [Google Scholar] [CrossRef] [PubMed]
- Rudramurthy, S.M.; Seyedmousavi, S.; Dhaliwal, M.; Chakrabarti, A.; Meis, J.F.; Mouton, J.W. Pharmacodynamics of voriconazole against wild-type and azole-resistant Aspergillus flavus isolates in a nonneutropenic murine. Antimicrob. Agents Chemother. 2017, 61, e01491-16. [Google Scholar] [CrossRef] [PubMed]
- Ananda-Rajah, M.R.; Kontoyiannis, D. Isavuconazole: A new extended spectrum triazole for invasive mold diseases. Future Microbiol. 2015, 10, 693–708. [Google Scholar] [CrossRef] [PubMed]
- Maertens, J.A.; Raad, I.I.; Marr, K.A.; Patterson, T.F.; Kontoyiannis, D.P.; Cornely, O.A.; Bow, E.J.; Rahav, G.; Neofytos, D.; Aoun, M.; et al. Isavuconazole versus voriconazole for primary treatment of invasive mould disease caused by Aspergillus and other filamentous fungi (SECURE): a phase 3, randomised-controlled, non-inferiority trial. Lancet 2016, 387, 760–769. [Google Scholar] [CrossRef]
- Jørgensen, K.M.; Astvad, K.M.T.; Hare, R.K.; Arendrup, M.C. EUCAST Determination of olorofim (F901318) susceptibility of mold species, method validation, and MICs. Antimicrob. Agents Chemother. 2018, 62, e00487-18. [Google Scholar] [CrossRef]
- Negri, C.E.; Johnson, A.; McEntee, L.; Box, H.; Whalley, S.; Schwartz, J.A.; Ramos-Martín, V.; Livermore, J.; Kolamunnage-Dona, R.; Colombo, A.L.; et al. Pharmacodynamics of the novel antifungal agent F901318 for acute sinopulmonary aspergillosis caused by Aspergillus flavus. J. Infect. Dis. 2018, 217, 1118–1127. [Google Scholar] [CrossRef]
- Rivero-Menendez, O.; Cuenca-Estrella, M.; Alastruey-Izquierdo, A. In-vitro activity of olorofim (F901318) against clinical isolates of cryptic species of Aspergillus by EUCAST and CLSI methodologies. J. Antimicrob. Chemother. 2019, dkz078. [Google Scholar] [CrossRef]
- Calvo, E.; Pastor, F.J.; Mayayo, E.; Salas, V.; Guarro, J. In-vitro activity and in-vivo efficacy of anidulafungin in murine infections by Aspergillus flavus. Antimicrob. Agents Chemother. 2011, 55, 1290–1292. [Google Scholar] [CrossRef]
| Study (Reference) | Testing Method | Number of Isolates | Antifungal | MIC Range | Modal MIC | ECV/ECOFF (95%/97.5%/99%) | % Above ECV/ECOFF (95%/97.5%/99%) | Comments |
|---|---|---|---|---|---|---|---|---|
| Values in μg/mL | ||||||||
| Espinel-Ingroff et al. [112] | CLSI -BMD | 444 | ISA | 0.06–2 | 0.5 | 1.0/1.0/2 | 3.2/3.2/0.2 | Modal MIC more than POS and VOR |
| Espinel-Ingroff et al. [108] | CLSI -BMD | 793 | AMB | 1 | ≤2 | |||
| Espinel-Ingroff et al. [109] | CLSI -BMD | 536 | ITR | 0.03–2 | 0.5 | 1 | 0.4 | ITR EUCAST R-BP >2 |
| 321 | POS | ≤0.03–2 | 0.06 | 0.25 | 5.3 | |||
| 590 | VOR | 0.06–4 | 0.5 | 1 | 0.9 | |||
| Espinel-Ingroff et al. [113] | CLSI BMD | 432 | CAS | 0.5 | 1.6 | |||
| Espinel-Ingroff et al. [114] | Combined CLSI EUCAST | 793 | AMB | 0.032–8 | 1 | 2/4/4 | ||
| Pfaller et al. [103] | CLSI BMD | 538 | ITR | 0.03–≥4 | 0.5 | 1/-/- | 0.4/-/- | |
| 444 | POS | ≤0.03–≥4 | 0.06 | 0.5/-/- | 0.9/-/- | |||
| 592 | VOR | 0.06–≥4 | 0.5 | 1/-/- | 1.7/-/- | |||
| Jiwa et al. [115] | CLSI -BMD | 50 | AMB | 0.12–2 | 0.5 | 2 | 0 | All isolates are from multiple centers from Canada |
| POS | 0.06–1 | 0.25 | 0.25 | 28 | ||||
| VOR | 0.5–16 | 1 | 1 | 40 | ||||
| ITR | 0.12–2 | 0.5 | 1 | 2 | ||||
| CAS | 0.03–0.5 | 0.125 | 0.25 | 4 | ||||
| Rudramurthy et al. [116] | CLSI and EUCAST | 208 | AMB | 1.0–16 | -/-/16 | -/-/0 | All isolates are from India | |
| ITR | 0.12–1 | -/-/0.5 | -/-/1.4 | |||||
| VOR | 0.25–4 | -/-/4 | -/-/0 | |||||
| POS | 0.12–0.5 | -/-/0.5 | -/-/0 | |||||
| ISA | 0.2–4 | -/-/2 | -/-/1.1 | |||||
| CAS | 0.25–1 | -/-/1 | -/-/0 | |||||
| ANI | 0.008–0.016 | -/-/0.016 | -/-/0 | |||||
| MFG | 0.008–0.2 | -/-/0.125 | -/-/1.4 | |||||
| Paul et al. [104] | CLSI | 189 | ITR | 0.03–16 | 1 | 1.6 | Included both clinical (n = 121) and environmental (n = 68) isolates | |
| VOR | 0.03–8.0 | 1 | 3.17 | |||||
| POS | 0.015–0.5 | 0.25 | 0.5 | |||||
| Espinel-Ingroff et al. [117] | SYO | 389 | VOR | 0.008–≥16 | 0.25 | 1 | ||
| E-test | 250 | ITR | 0.01–2 | 0.25 | 1 | |||
| E-test | 257 | VOR | 0.01–≥16 | 0.25 | 0.5 | |||
| E-test | 204 | POS | 0.01–1 | 0.25 | 0.5 | |||
| Pfaller et al. [118] | CLSI BMD | 188 | CAS | 0.007–0.12 | 0.016 | 0.06 | 0.5 | |
| Espinel-Ingroff et al. [119] | E-Test CLSI EUCAST | 238 | AMB | 0.12–32 | 2 | 8 (E-test) 4 (CLSI and EUCAST) | ||
| Taghizadeh-Armaki et al. [92] | EUCAST | 200 | AMB | 1–16 | 4.0 | |||
| ITR | 0.031–4 | 1.5 | ||||||
| VOR | 0.063–2 | 0 | ||||||
| POS | 0.031–1 | 0.5 | ||||||
| ISA | 0.125–4 | 2 | ||||||
| Antifungal | EUCAST | CLSI | ||
|---|---|---|---|---|
| A. flavus | A. fumigatus | A. flavus | A. fumigatus | |
| Itraconazole | 1.0 | 1.0 | 1.0 | 1.0 |
| Voriconazole | 2.0 | 1.0 | 2.0 | 1.0 |
| Posaconazole | 0.5 | 0.25 | 0.5 | - |
| Isavuconazole | 2.0 | 2.0 | 1.0 | 1.0 |
| Caspofungin | - | - | 0.5 | 0.5 |
| Amphotericin B | 4.0 | 1.0 | 4.0 | 2.0 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rudramurthy, S.M.; Paul, R.A.; Chakrabarti, A.; Mouton, J.W.; Meis, J.F. Invasive Aspergillosis by Aspergillus flavus: Epidemiology, Diagnosis, Antifungal Resistance, and Management. J. Fungi 2019, 5, 55. https://doi.org/10.3390/jof5030055
Rudramurthy SM, Paul RA, Chakrabarti A, Mouton JW, Meis JF. Invasive Aspergillosis by Aspergillus flavus: Epidemiology, Diagnosis, Antifungal Resistance, and Management. Journal of Fungi. 2019; 5(3):55. https://doi.org/10.3390/jof5030055
Chicago/Turabian StyleRudramurthy, Shivaprakash M., Raees A. Paul, Arunaloke Chakrabarti, Johan W. Mouton, and Jacques F. Meis. 2019. "Invasive Aspergillosis by Aspergillus flavus: Epidemiology, Diagnosis, Antifungal Resistance, and Management" Journal of Fungi 5, no. 3: 55. https://doi.org/10.3390/jof5030055
APA StyleRudramurthy, S. M., Paul, R. A., Chakrabarti, A., Mouton, J. W., & Meis, J. F. (2019). Invasive Aspergillosis by Aspergillus flavus: Epidemiology, Diagnosis, Antifungal Resistance, and Management. Journal of Fungi, 5(3), 55. https://doi.org/10.3390/jof5030055





