Intensive Care Antifungal Stewardship Programme Based on T2Candida PCR and Candida Mannan Antigen: A Prospective Study
Abstract
1. Introduction
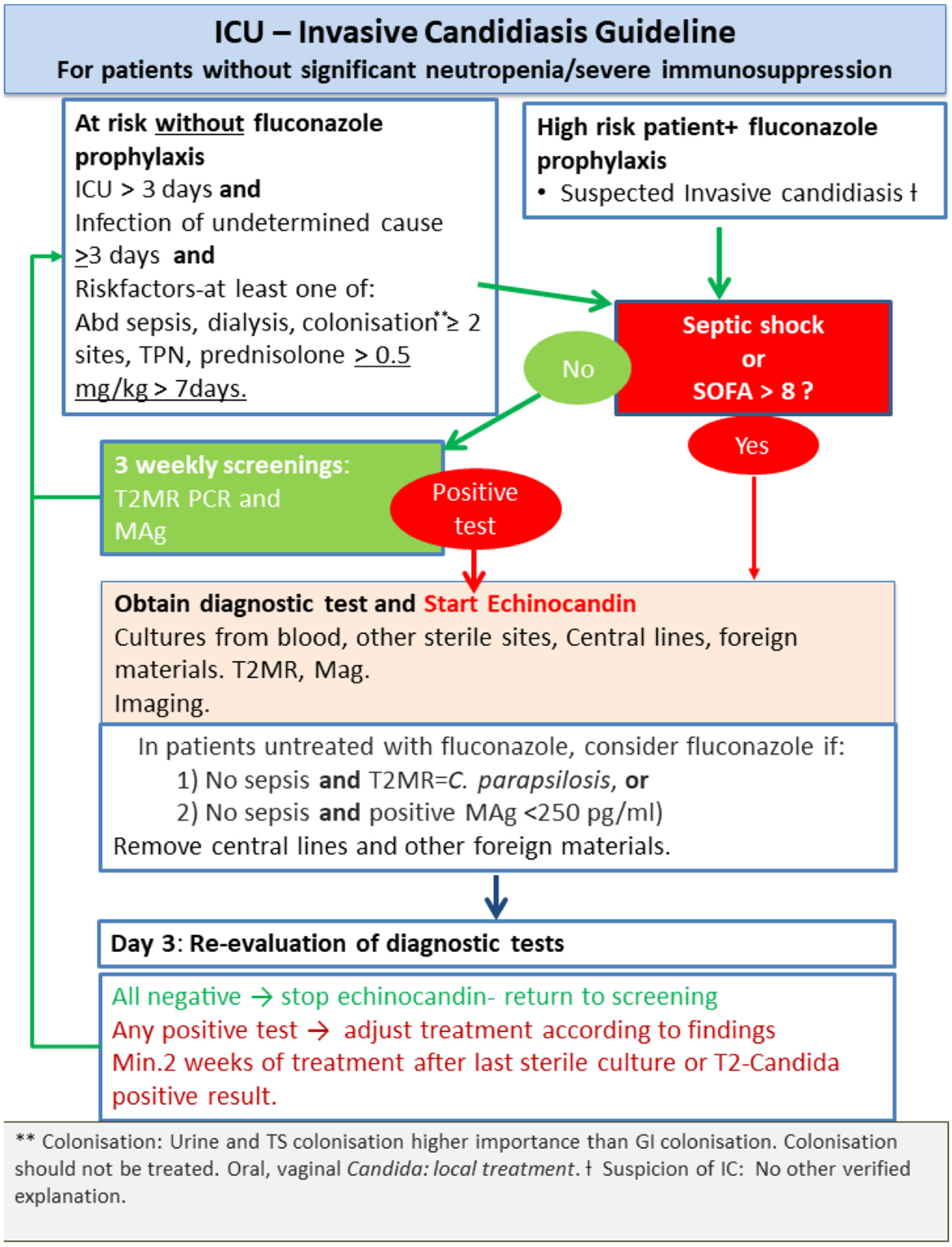
2. Material and Methods
Statistical Analysis
3. Results
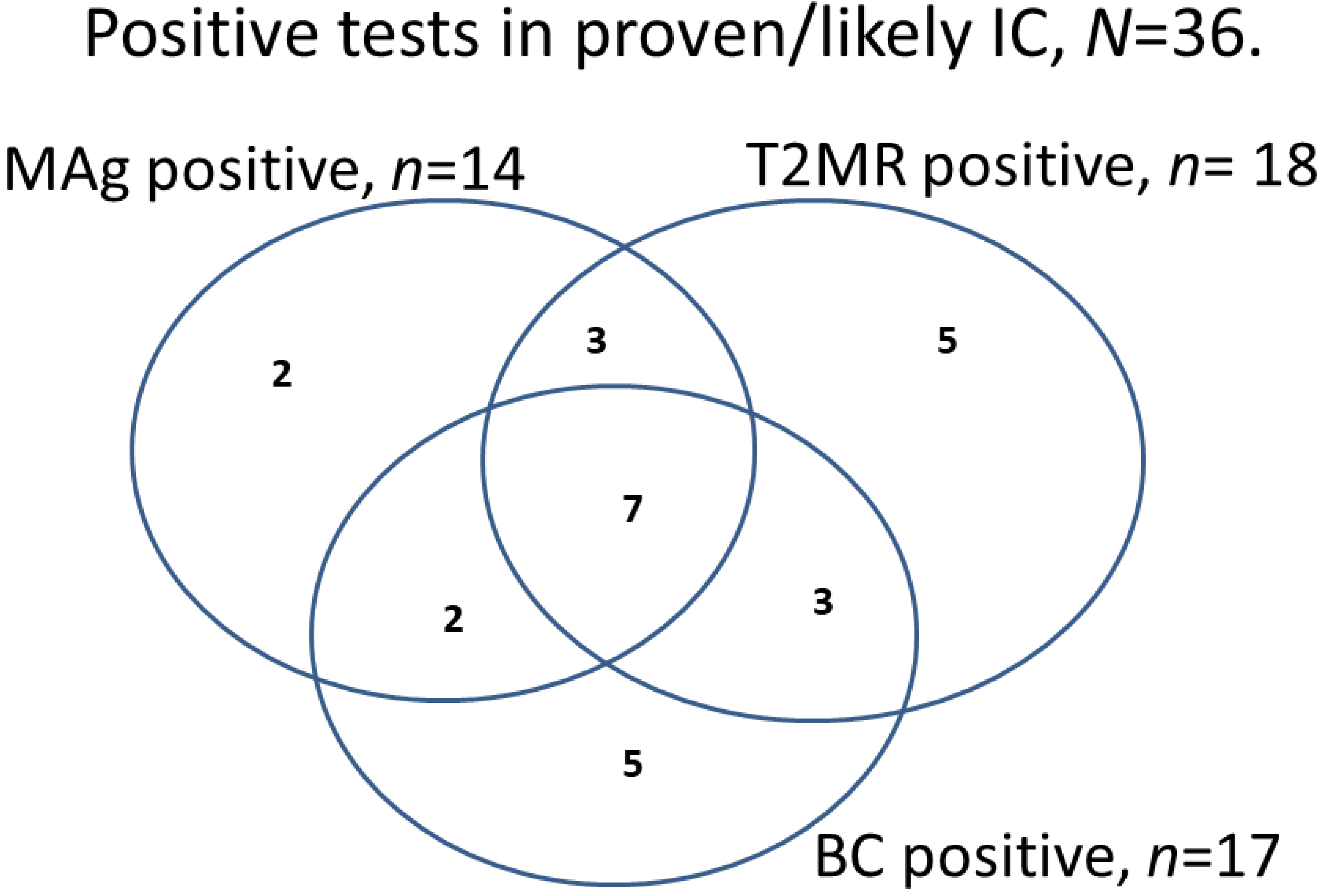
3.1. Diagnostic Performance
3.2. Therapy
4. Discussion
4.1. T2MR
4.2. Mannan Antigen
4.3. Combination Biomarkers to Guide AFT
4.4. Antifungal Use
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pappas, P.G.; Lionakis, M.S.; Arendrup, M.C.; Ostrosky-Zeichner, L.; Kullberg, B.J. Invasive candidiasis. Nat. Rev. Dis. Prim. 2018, 4, 18026. [Google Scholar] [CrossRef]
- Kullberg, B.J.; Arendrup, M.C. Invasive Candidiasis. N. Engl. J. Med. 2015, 373, 1445–1456. [Google Scholar] [CrossRef]
- Clancy, C.J.; Nguyen, M.H. Finding the “Missing 50%” of Invasive Candidiasis: How Nonculture Diagnostics Will Improve Understanding of Disease Spectrum and Transform Patient Care. Clin. Infect. Dis. 2013, 56, 1284–1292. [Google Scholar] [CrossRef] [PubMed]
- Ostrosky-Zeichner, L.; Shoham, S.; Vazquez, J.; Reboli, A.; Betts, R.; Barron, M.A.; Schuster, M.; Judson, M.A.; Revankar, S.G.; Caeiro, J.P.; et al. MSG-01: A randomized, double-blind, placebo-controlled trial of caspofungin prophylaxis followed by preemptive therapy for invasive candidiasis in high-risk adults in the critical care setting. Clin. Infect. Dis. 2014, 58, 1219–1226. [Google Scholar] [CrossRef] [PubMed]
- Knitsch, W.; Vincent, J.-L.; Utzolino, S.; François, B.; Dinya, T.; Dimopoulos, G.; Özgüneş, İ.; Valía, J.C.; Eggimann, P.; León, C.; et al. A randomized, placebo-controlled trial of preemptive antifungal therapy for the prevention of invasive candidiasis following gastrointestinal surgery for intra-abdominal infections. Clin. Infect. Dis. 2015, 61, 1671–1678. [Google Scholar] [CrossRef] [PubMed]
- Timsit, J.-F.; Azoulay, E.; Schwebel, C.; Charles, P.E.; Cornet, M.; Souweine, B.; Klouche, K.; Jaber, S.; Trouillet, J.-L.; Bruneel, F.; et al. Empirical Micafungin Treatment and Survival Without Invasive Fungal Infection in Adults With ICU-Acquired Sepsis, Candida Colonization, and Multiple Organ Failure: The EMPIRICUS Randomized Clinical Trial. JAMA 2016, 316, 1555–1564. [Google Scholar] [CrossRef] [PubMed]
- Cortegiani, A.; Russotto, V.; Giarratano, A. Associations of Antifungal Treatments with Prevention of Fungal Infection in Critically Ill Patients without Neutropenia. JAMA 2017, 317, 311–312. [Google Scholar] [CrossRef] [PubMed]
- Falcone, M.; Tiseo, G.; Gutiérrez-Gutiérrez, B.; Raponi, G.; Carfagna, P.; Rosin, C.; Luzzati, R.; Delle Rose, D.; Andreoni, M.; Farcomeni, A.; et al. Impact of Initial Antifungal Therapy on the Outcome of Patients with Candidemia and Septic Shock Admitted to Medical Wards: A Propensity Score-Adjusted Analysis. Open Forum Infect. Dis. 2019, 6, ofz251. [Google Scholar] [CrossRef] [PubMed]
- Playford, E.G.; Lipman, J.; Jones, M.; Lau, A.F.; Kabir, M.; Chen, S.C.-A.; Marriott, D.J.; Seppelt, I.; Gottlieb, T.; Cheung, W.; et al. Problematic Dichotomization of Risk for Intensive Care Unit (ICU)-Acquired Invasive Candidiasis: Results Using a Risk-Predictive Model to Categorize 3 Levels of Risk From a Multicenter Prospective Cohort of Australian ICU Patients. Clin. Infect. Dis. 2016, 63, 1463–1469. [Google Scholar] [CrossRef] [PubMed]
- Bailly, S.; Leroy, O.; Dupont, H.; Timsit, J.-F. Secondarily documented invasive candidiasis is unpredictable using traditional risk factors in non transplant—Non-neutropenic adult ICU patients. Int. J. Infect. Dis. 2017, 54, 31–33. [Google Scholar] [CrossRef] [PubMed]
- Mylonakis, E.; Clancy, C.J.; Ostrosky-Zeichner, L.; Garey, K.W.; Alangaden, G.J.; Vazquez, J.A.; Groeger, J.S.; Judson, M.A.; Vinagre, Y.; Heard, S.O.; et al. T2 magnetic resonance assay for the rapid diagnosis of candidemia in whole blood: A clinical trial. Clin. Infect. Dis. 2015, 60, 892–899. [Google Scholar] [CrossRef] [PubMed]
- Astvad, K.M.T.; Johansen, H.K.; Røder, B.L.; Rosenvinge, F.S.; Knudsen, J.D.; Lemming, L.; Schønheyder, H.C.; Hare, R.K.; Kristensen, L.; Nielsen, L.; et al. Update from a 12-Year Nationwide Fungemia Surveillance: Increasing Intrinsic and Acquired Resistance Causes Concern. J. Clin. Microbiol. 2018, 56, e01564-17. [Google Scholar] [CrossRef]
- Clancy, C.J.; Nguyen, M.H. T2 magnetic resonance for the diagnosis of bloodstream infections: Charting a path forward. J. Antimicrob. Chemother. 2018, 73, iv2–iv5. [Google Scholar] [CrossRef] [PubMed]
- Clancy, C.J.; Pappas, P.G.; Vazquez, J.; Judson, M.A.; Kontoyiannis, D.P.; Thompson, G.R.; Garey, K.W.; Reboli, A.; Greenberg, R.N.; Apewokin, S.; et al. Detecting Infections Rapidly and Easily for Candidemia Trial, Part 2 (DIRECT2): A Prospective, Multicenter Study of the T2Candida Panel. Clin. Infect. Dis. 2018, 66, 1678–1686. [Google Scholar] [CrossRef]
- Hamula, C.L.; Abmm, D.; Hughes, K.; Fisher, B.T.; Zaoutis, T.E.; Singh, I.R.; Velegraki, A. T2Candida Provides Rapid and Accurate Species Identification in Pediatric Cases of Candidemia. Am. J. Clin. Pathol. 2016, 145, 858–861. [Google Scholar] [CrossRef] [PubMed]
- Mylonakis, E.; Zacharioudakis, I.M.; Clancy, C.J.; Nguyen, M.H.; Pappas, P.G. Efficacy of T2 magnetic resonance assay in monitoring candidemia after initiation of antifungal therapy: The serial therapeutic and antifungal monitoring protocol (STAMP) trial. J. Clin. Microbiol. 2018, 56, e01756-17. [Google Scholar] [CrossRef] [PubMed]
- Sendid, B.; Poirot, J.L.; Tabouret, M.; Bonnin, A.; Caillot, D.; Camus, D.; Poulain, D. Combined detection of mannanaemia and anti-mannan antibodies as a strategy for the diagnosis of systemic infection caused by pathogenic Candida species. J. Med. Microbiol. 2002, 51, 433–442. [Google Scholar] [CrossRef] [PubMed]
- Lausch, K.R.; Søgaard, M.; Rosenvinge, F.S.; Johansen, H.K.; Boysen, T.; Røder, B.L.; Mortensen, K.L.; Nielsen, L.; Lemming, L.; Olesen, B.; et al. Treatment of candidemia in a nationwide setting: Increased survival with primary echinocandin treatment. Infect. Drug Resist. 2018, 11, 2449–2459. [Google Scholar] [CrossRef] [PubMed]
- Arendrup, M.C.; Andersen, J.S.; Holten, M.K.; Krarup, K.B.; Reiter, N.; Schierbeck, J.; Helleberg, M. Diagnostic performance of T2Candida among ICU patients with risk factors for invasive candidiasis. Open Forum Infect. Dis. 2019, 6, ofz136. [Google Scholar] [CrossRef] [PubMed]
- Pittet, D.; Monod, M.; Suter, P.M.; Frenk, E.; Auckenthaler, R. Candida colonization and subsequent infections in critically ill surgical patients. Ann. Surg. 1994, 220, 751–758. [Google Scholar] [CrossRef] [PubMed]
- De Pauw, B.; Walsh, T.J.; Donnelly, J.P.; Stevens, D.A.; Edwards, J.E.; Calandra, T.; Pappas, P.G.; Maertens, J.; Lortholary, O.; Kauffman, C.A.; et al. Revised Definitions of Invasive Fungal Disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) C. Clin. Infect. Dis. 2008, 46, 1813–1821. [Google Scholar] [CrossRef] [PubMed]
- Mejia-Chew, C.; O’Halloran, J.A.; Olsen, M.A.; Stwalley, D.; Kronen, R.; Lin, C.; Salazar, A.S.; Larson, L.; Hsueh, K.; Powderly, W.G.; et al. Effect of infectious disease consultation on mortality and treatment of patients with candida bloodstream infections: A retrospective, cohort study. Lancet Infect. Dis. 2019, 19, 1336–1344. [Google Scholar] [CrossRef]
- Agrawal, S.; Barnes, R.; Brüggemann, R.J.; Rautemaa-Richardson, R.; Warris, A. The role of the mulidisciplinary team in antifungal stewardship. J. Antimicrob. Chemother. 2016, 71, ii37–ii42. [Google Scholar] [CrossRef]
- Muñoz, P.; Bouza, E.; Alonso, R.; Anaya, F.; Banares, R.; Bustinza, A.; Cáliz, B.; Fernández-Cruz, A.; Escribano, P.; Fernández-Quero, L.; et al. The current treatment landscape: The need for antifungal stewardship programmes. J. Antimicrob. Chemother. 2016, 71, ii5–ii12. [Google Scholar] [CrossRef][Green Version]
- Johnson, M.D.; Lewis, R.E.; Dodds Ashley, E.S.; Ostrosky-Zeichner, L.; Zaoutis, T.; Thompson, G.R.; Andes, D.R.; Walsh, T.J.; Pappas, P.G.; Cornely, O.A.; et al. Core Recommendations for Antifungal Stewardship: A Statement of the Mycoses Study Group Education and Research Consortium. J. Infect. Dis. 2020, 222, S175–S198. [Google Scholar] [CrossRef] [PubMed]
- Monday, L.M.; Acosta, T.P.; Alangaden, G. T2candida for the diagnosis and management of invasive candida infections. J. Fungi 2021, 7, 178. [Google Scholar] [CrossRef] [PubMed]
- Wilson, N.M.; Kenney, R.M.; Tibbetts, R.J.; Alangaden, G.; Davis, S.L.; Samuel, L.P. T2 Magnetic Resonance Improves the Timely Management of Candidemia. J. Antimicrob. Steward. 2017, 24, 1569. [Google Scholar] [CrossRef]
- Patch, M.E.; Weisz, E.; Cubillos, A.; Estrada, S.J.; Pfaller, M.A. Impact of rapid, culture-independent diagnosis of candidaemia and invasive candidiasis in a community health system. J. Antimicrob. Chemother. 2018, 73, iv27–iv30. [Google Scholar] [CrossRef]
- Gill, C.M.; Kenney, R.M.; Hencken, L.; Mlynarek, M.E.; Alangaden, G.J.; Samuel, L.P.; Davis, S.L. T2 Candida versus beta-D-glucan to facilitate antifungal discontinuation in the intensive care unit. Diagn. Microbiol. Infect. Dis. 2019, 95, 162–165. [Google Scholar] [CrossRef] [PubMed]
- Bomkamp, J.P.; Sulaiman, R.; Hartwell, J.L.; Desai, A.; Winn, V.C.; Wrin, J.; Kussin, M.L.; Hiles, J.J. Evaluation of a rapid fungal detection panel for identification of candidemia at an academic medical center. J. Clin. Microbiol. 2020, 58, e01408-19. [Google Scholar] [CrossRef]
- White, P.L.; Barnes, R.A.; Gorton, R.; Cruciani, M.; Loeffler, J. Comment on: T2Candida MR as a predictor of outcome in patients with suspected invasive candidiasis starting empirical antifungal treatment: A prospective pilot study. J. Antimicrob. Chemother. 2019, 74, 532–533. [Google Scholar] [CrossRef]
- Muñoz, P.; Vena, A.; Machado, M.; Martínez-Jiménez, M.C.; Gioia, F.; Gómez, E.; Origüen, J.; Orellana, M.Á.; López-Medrano, F.; Pérez-Granda, M.-J.; et al. T2MR contributes to the very early diagnosis of complicated candidaemia. A prospective study. J. Antimicrob. Chemother. 2018, 73, iv13–iv19. [Google Scholar] [CrossRef]
- Mikulska, M.; Calandra, T.; Sanguinetti, M.; Poulain, D.; Viscoli, C. The use of mannan antigen and anti-mannan antibodies in the diagnosis of invasive candidiasis: Recommendations from the Third European Conference on Infections in Leukemia. Crit. Care 2010, 14, R222. [Google Scholar] [CrossRef]
- Chumpitazi, B.F.F.; Lebeau, B.; Faure-Cognet, O.; Hamidfar-Roy, R.; Timsit, J.F.; Pavese, P.; Thiebaut-Bertrand, A.; Quesada, J.L.; Pelloux, H.; Pinel, C. Characteristic and clinical relevance of Candida mannan test in the diagnosis of probable invasive candidiasis. Med. Mycol. 2014, 52, 462–471. [Google Scholar] [CrossRef]
- Wang, K.; Luo, Y.; Zhang, W.; Xie, S.; Yan, P.; Liu, Y.; Li, Y.; Ma, X.; Xiao, K.; Fu, H.; et al. Diagnostic value of Candida mannan antigen and anti-mannan IgG and IgM antibodies for Candida infection. Mycoses 2020, 63, 181–188. [Google Scholar] [CrossRef] [PubMed]
- León, C.; Ruiz-Santana, S.; Saavedra, P.; Castro, C.; Loza, A.; Zakariya, I.; Úbeda, A.; Parra, M.; Macías, D.; Tomás, J.I.; et al. Contribution of Candida biomarkers and DNA detection for the diagnosis of invasive candidiasis in ICU patients with severe abdominal conditions. Crit. Care 2016, 20, 149. [Google Scholar] [CrossRef]
- Duettmann, W.; Koidl, C.; Krause, R.; Lackner, G.; Woelfler, A.; Hoenigl, M. Specificity of mannan antigen and anti-mannan antibody screening in patients with haematological malignancies at risk for fungal infection. Mycoses 2016, 59, 374–378. [Google Scholar] [CrossRef] [PubMed]
- Dupuis, C.; Le Bihan, C.; Maubon, D.; Calvet, L.; Ruckly, S.; Schwebel, C.; Bouadma, L.; Azoulay, E.; Cornet, M.; Timsit, J.F. Performance of Repeated Measures of (1-3)-β-D-Glucan, Mannan Antigen, and Antimannan Antibodies for the Diagnosis of Invasive Candidiasis in ICU Patients: A Preplanned Ancillary Analysis of the EMPIRICUS Randomized Clinical Trial. Open Forum Infect. Dis. 2021, 8, ofab080. [Google Scholar] [CrossRef] [PubMed]
- Rouzé, A.; Loridant, S.; Poissy, J.; Dervaux, B.; Sendid, B.; Cornu, M.; Nseir, S. Biomarker-based strategy for early discontinuation of empirical antifungal treatment in critically ill patients: A randomized controlled trial. Intensive Care Med. 2017, 43, 1668–1677. [Google Scholar] [CrossRef] [PubMed]
- Lamoth, F.; Clancy, C.J.; Tissot, F.; Squires, K.; Eggimann, P.; Flückiger, U.; Siegemund, M.; Orasch, C.; Zimmerli, S.; Calandra, T.; et al. Performance of the T2Candida Panel for the Diagnosis of Intra-abdominal Candidiasis. Open Forum Infect. Dis. 2020, 7, ofaa075. [Google Scholar] [CrossRef]
- Clancy, C.J.; Nguyen, M.H. Diagnosing invasive candidiasis. J. Clin. Microbiol. 2018, 56, e01909-17. [Google Scholar] [CrossRef] [PubMed]
- Muñoz, P.; Vena, A.; Machado, M.; Gioia, F.; Martínez-Jiménez, M.C.; Gómez, E.; Origüen, J.; Orellana, M.Á.; López-Medrano, F.; Fernández-Ruiz, M.; et al. T2Candida MR as a predictor of outcome in patients with suspected invasive candidiasis starting empirical antifungal treatment: A prospective pilot study. J. Antimicrob. Chemother. 2018, 73, iv6–iv12. [Google Scholar] [CrossRef] [PubMed]
- Zurl, C.; Prattes, J.; Zollner-Schwetz, I.; Valentin, T.; Rabensteiner, J.; Wunsch, S.; Hoenigl, M.; Krause, R. T2Candida magnetic resonance in patients with invasive candidiasis: Strengths and limitations. Med. Mycol. 2019, 58, 632–638. [Google Scholar] [CrossRef] [PubMed]
| Baseline Characteristics, N (%) | Years/Days (IQR) or N (%) |
|---|---|
| Demography and underlying diseases | |
| Age, median years | 63 (IQR 52–72) |
| Male sex | 152 (69%) |
| Previous SOT or BMT | 18 (8%) |
| Malignancy | 50 (23%) |
| IDDM | 15 (7%) |
| Type of ICU, ventilation and pressor support | |
| General ICU | 141 (64%) |
| Thoracic ICU | 78 (36%) |
| Days of mechanical ventilation, median (IQR) | 11 (6–15) |
| Vasopressors at inclusion | 102 (61%) |
| Surgery | |
| Surgery during hospital stay (%) | 173 (79%) |
| Emergency gastrointestinal/hepatobiliary surgery and/or gastrointestinal perforation | 46 (21%) |
| Thoracic surgery | 78 (36%) |
| Other risk factors | |
| Renal-replacement therapy | 77 (45%) |
| Total parenteral nutrition | 63 (29%) |
| Chemotherapy ≤ 3 months | 18 (8%) |
| Corticosteroid > 25 mg daily | 27 (12%) |
| Other immunosuppressive treatment | 20 (9%) |
| Blood transfusion receipt | 157 (72%) |
| Candida colonisation | 186 (85%) |
| Candida colonisation index ≥ 0.5 * | 114 (52%) |
| Invasive Candidiasis (IC) | n/Totals (%) |
|---|---|
| General ICU, n. proven/likely/possible cases | 39/141 (28%) |
| Thoracic ICU, n. proven/likely/possible cases | 9/78 (12%) |
| IC classification | |
| Proven | 29/219 (13.2%) |
| Likely | 7/219 (3.2%) |
| Possible | 12/219 (5.5%) |
| Unlikely | 171/219 (78%) |
| Clinical outcome | |
| In hospital mortality | 89/219 (41%) |
| Mortality in patients with proven/likely IC | 21/36 (58%) |
| Mortality in patients without proven/likely IC | 65/171 (38%) |
| Early Death (<5 days) with proven/likely IC | 5/36 (13.9%) |
| Length of AFT a, proven/likely IC, median days (IQR) | 18 (11–38) |
| Length of AFT, no IC, median days (IQR) | 10 (5–19) |
| Sites of Infection | Total IC (n = 48) | Proven IC (n = 29) | Likely IC (n = 7) | Possible IC (n = 12) |
|---|---|---|---|---|
| Blood (candidaemia) a | 17 (35%) | 17 (59%) | 0 | 0 |
| Blood stream only | 6 | 6 | 0 | 0 |
| Abdominal a | 25 (52%) | 16 (55%) | 4 | 5 (42%) |
| Deep-seated only | 18 | 10 | 3 | 5 |
| Thoracic/cardiac a | 10 (21%) | 6 (21%) | 3 | 1 (8%) |
| Deep-seated only | 7 | 3 | 3 | 1 |
| Burns a | 2 (4%) | 1 (3%) | 0 | 1 (8%) |
| Burns only | 1 | 0 | 0 | 1 |
| Other and/or multiple foci | 5 (10%) | 0 | 0 | 5 (42%) |
| Deep-seated only | 5 | 0 | 0 | 5 |
| Species | N of Patients with | |
|---|---|---|
| Candidaemia | Proven/Likely IC, without Candidemia * | |
| C. albicans | 9 | 11 |
| C. tropicalis | 1 | 2 |
| C. glabrata | 1 | 3 |
| C. krusei | 1 | 1 |
| C. parapsilosis | 1 | 0 |
| C. dubliniensis | 3 | 0 |
| Other Candida species | 1 | 2 |
| Total number of culture positive | 17 | 19 |
| Diagnostic Test and Results | Patients with Positive Tests, N | Candidaemia N of Positive Patients | Proven/Likely IC, No Candidemia N of Positive Patients |
|---|---|---|---|
| T2MR Candida species | |||
| C. albicans/C. tropicalis | 22 | 8/10 | 6/8 |
| C. glabrata/C. krusei | 6 | 1/2 | 2/2 |
| C. parapsilosis | 2 | 1/1 | 0/0 |
| Mannan antigen positive | |||
| ≥125 ng/L | 24 | 9/17 | 5/10 |
| Antifungal Prescriptions | N (% of All) |
|---|---|
| No antifungal treatment | 52 (24%) |
| Clinical indication for initial therapy | |
| Invasive candidiasis | 26 (12%) |
| Other fungal infection | 5 (2%) |
| Empiric anti-fungal treatment initiated | 96 (44%) |
| Prophylactic antifungal treatment initiated | 40 (18%) |
| Antifungal agents | |
| Fluconazole only | 51 (23%) |
| Echinocandin only | 48 (22%) |
| Mould-active azole or Ambisome * | 26 (12%) |
| ≥2 different antifungals given during admission | 68 (31%) |
| De-escalation from echinocandin to fluconazole | 34 (16%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Helweg-Larsen, J.; Steensen, M.; Møller Pedersen, F.; Bredahl Jensen, P.; Perch, M.; Møller, K.; Riis Olesen, B.; Søderlund, M.; Cavling Arendrup, M. Intensive Care Antifungal Stewardship Programme Based on T2Candida PCR and Candida Mannan Antigen: A Prospective Study. J. Fungi 2021, 7, 1044. https://doi.org/10.3390/jof7121044
Helweg-Larsen J, Steensen M, Møller Pedersen F, Bredahl Jensen P, Perch M, Møller K, Riis Olesen B, Søderlund M, Cavling Arendrup M. Intensive Care Antifungal Stewardship Programme Based on T2Candida PCR and Candida Mannan Antigen: A Prospective Study. Journal of Fungi. 2021; 7(12):1044. https://doi.org/10.3390/jof7121044
Chicago/Turabian StyleHelweg-Larsen, Jannik, Morten Steensen, Finn Møller Pedersen, Pia Bredahl Jensen, Michael Perch, Kirsten Møller, Birthe Riis Olesen, Mathias Søderlund, and Maiken Cavling Arendrup. 2021. "Intensive Care Antifungal Stewardship Programme Based on T2Candida PCR and Candida Mannan Antigen: A Prospective Study" Journal of Fungi 7, no. 12: 1044. https://doi.org/10.3390/jof7121044
APA StyleHelweg-Larsen, J., Steensen, M., Møller Pedersen, F., Bredahl Jensen, P., Perch, M., Møller, K., Riis Olesen, B., Søderlund, M., & Cavling Arendrup, M. (2021). Intensive Care Antifungal Stewardship Programme Based on T2Candida PCR and Candida Mannan Antigen: A Prospective Study. Journal of Fungi, 7(12), 1044. https://doi.org/10.3390/jof7121044







