Advocating for Coccidioidomycosis to Be a Reportable Disease Nationwide in the United States and Encouraging Disease Surveillance across North and South America
Abstract
1. Introduction
2. Clinical Benefits of Coccidioidomycosis as a Reportable Disease
3. Understanding the Public Health Impact of Valley Fever Can Better Justify Antifungal Drug and Vaccine Development
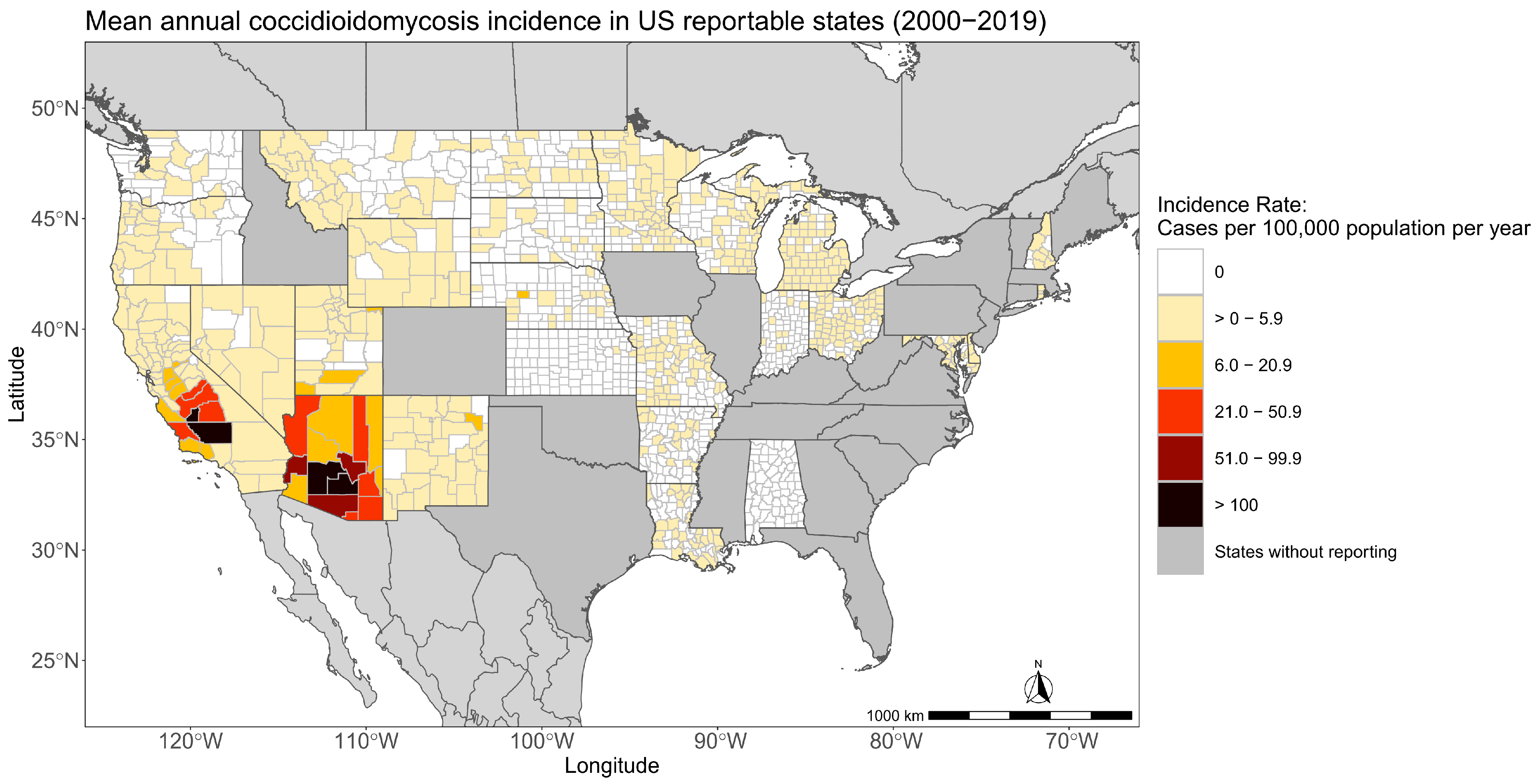
4. Delineating the Environmental Drivers of Coccidioides and Coccidioidomycosis Disease Dynamics and an Estimate of the Current Endemic Area
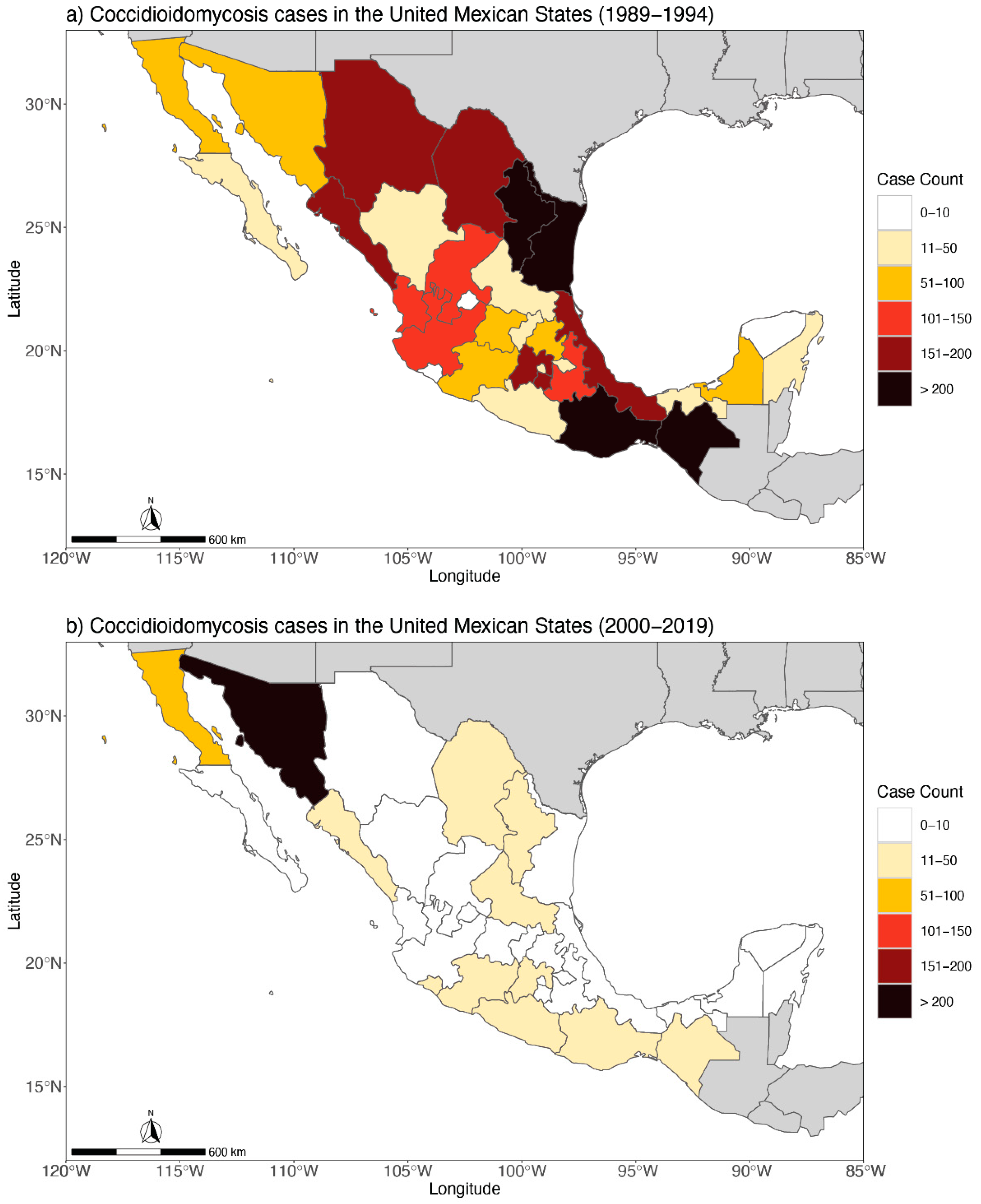
5. Beyond Borders: Reporting Coccidioidomycosis in Mexico
- An epidemiological surveillance program has never been implemented to control or prevent this infection
- From 2010 to 2012, a sub-national survey of intradermal reaction with coccidioidin was carried out in 1081 people from 9 states, and 29.5% of people tested positive for the antigen [84]. The percentage of infection is not negligible, especially if one takes into account that the samples were taken from states with environmental conditions not associated with the presence of Coccidioides
- The Dynamic Cubes [87] of the National Health System continues to register deaths whose diagnosis is coccidioidomycosis
6. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Centers for Disease Control and Prevention. Valley Fever (Coccidioidomycosis) Statistics. 2022. Available online: https://www.cdc.gov/fungal/diseases/coccidioidomycosis/statistics.html (accessed on 1 December 2022).
- Benedict, K.; Kobayashi, M.; Garg, S.; Chiller, T.; Jackson, B.R. Symptoms in blastomycosis, coccidioidomycosis, and histoplasmosis versus other respiratory illnesses in commercially insured adult outpatients—United States, 2016–2017. Clin. Infect. Dis. 2021, 73, e4336–e4344. [Google Scholar] [CrossRef] [PubMed]
- Smith, C.E.; Whiting, E.G.; Baker, E.E.; Rosenberger, H.G.; Beard, R.R.; Saito, M.T. The use of coccidioidin. Am. Rev. Tuberc. 1948, 57, 330–360. [Google Scholar] [CrossRef] [PubMed]
- Bays, D.J.; Thompson, G.R. Coccidioidomycosis. Infect. Dis. Clin. 2021, 35, 453–469. [Google Scholar] [CrossRef] [PubMed]
- Barker, B.M. Coccidioidomycosis in animals. In Emerging and Epizootic Fungal Infections in Animals; Seyedmousavi, S., de Hoog, G.S., Guillot, J., Verweij, P.E., Eds.; Springer International Publishing: Berlin/Heidelberg, Germany, 2018; pp. 81–114. [Google Scholar] [CrossRef]
- Kollath, D.R.; Miller, K.J.; Barker, B.M. The mysterious desert dwellers: Coccidioides immitis and Coccidioides posadasii, causative fungal agents of coccidioidomycosis. Virulence 2019, 10, 222–233. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Valley Fever Maps. 2020. Available online: https://www.cdc.gov/fungal/diseases/coccidioidomycosis/maps.html (accessed on 1 December 2022).
- Williams, S.L.; Chiller, T. Update on the epidemiology, diagnosis, and treatment of coccidioidomycosis. J. Fungi 2022, 8, 666. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Coccidioidomycosis/Valley Fever (Coccidioides spp.). 2021. Available online: https://ndc.services.cdc.gov/conditions/coccidioidomycosis/ (accessed on 1 December 2022).
- McCotter, O.; Kennedy, J.; McCollum, J.; Bartholomew, M.; Iralu, J.; Jackson, B.R.; Haberling, D.; Benedict, K. Coccidioidomycosis among American Indians and Alaska Natives, 2001–2014. Open Forum Infect. Dis. 2019, 6, ofz052. [Google Scholar] [CrossRef]
- Gorris, M.E.; Treseder, K.K.; Zender, C.S.; Randerson, J.T. Expansion of coccidioidomycosis endemic regions in the United States in response to climate change. GeoHealth 2019, 3, 10. [Google Scholar] [CrossRef]
- Laniado-Laborín, R.; Arathoon, E.G.; Canteros, C.; Muñiz-Salazar, R.; Rendon, A. Coccidioidomycosis in Latin America. Med. Mycol. 2019, 57 (Suppl. 1), S46–S55. [Google Scholar] [CrossRef]
- Caldwell, C.T. Coccidioidal granuloma: A report of three cases recognized in Texas. Tex. State J. Med. 1932, 28, 327–333. [Google Scholar]
- Roberts, P.L.; Lisciandro, R.C. A community epidemic of coccidioidomycosis. Am. Rev. Respir. Dis. 1967, 96, 766–772. [Google Scholar] [CrossRef]
- Teel, K.W.; Yow, M.D.; Williams, T.W. A localized outbreak of coccidioidomycosis in southern Texas. J. Pediatr. 1970, 77, 65–73. [Google Scholar] [CrossRef]
- Edwards, P.Q.; Palmer, C.E. Prevalence of sensitivity to coccidioidin, with special reference to specific and nonspecific reactions to coccidioidin and to histoplasmin. Dis. Chest 1957, 31, 35–60. [Google Scholar] [CrossRef] [PubMed]
- Baptista-Rosas, R.C.; Hinojosa, A.; Riquelme, M. Ecological niche modeling of Coccidioides spp. in western North American deserts. Ann. N. Y. Acad. Sci. 2007, 1111, 35–46. [Google Scholar] [CrossRef] [PubMed]
- Dobos, R.R.; Benedict, K.; Jackson, B.R.; McCotter, O.Z. Using soil survey data to model potential Coccidioides soil habitat and inform Valley fever epidemiology. PLoS ONE 2021, 16, e0247263. [Google Scholar] [CrossRef]
- Pena-Ruiz, M.A.; Meza, A.D.; Mulla, Z. Coccidioidomycosis infection in a predominantly Hispanic population. Ann. N. Y. Acad. Sci. 2007, 1111, 122–128. [Google Scholar] [CrossRef] [PubMed]
- Peterson, C.; Chu, V.; Lovelace, J.; Almekdash, M.H.; Lacy, M. Coccidioidomycosis cases at a regional referral center, West Texas, USA, 2013–2019. Emerg. Infect. Dis. 2022, 4, 848. [Google Scholar] [CrossRef]
- Croskerry, P. The importance of cognitive errors in diagnosis and strategies to minimize them. Acad. Med. 2003, 78, 775–780. [Google Scholar] [CrossRef]
- Pruinelli, L.; Westra, B.L.; Yadav, P.; Hoff, A.; Steinbach, M.; Kumar, V.; Delaney, C.W.; Simon, G. Delay within the 3-Hour surviving sepsis campaign guideline on mortality for patients with severe sepsis and septic shock. Crit. Care Med. 2018, 46, 500–505. [Google Scholar] [CrossRef]
- Donovan, F.M.; Wightman, P.; Zong, Y.; Gabe, L.; Majeed, A.; Ynosencio, T.; Bedrick, E.J.; Galgiani, J.N. Delays in coccidioidomycosis diagnosis and associated healthcare utilization, Tucson, Arizona, USA. Emerg. Infect. Dis. 2019, 25, 1745. [Google Scholar] [CrossRef]
- Benedict, K.; Ireland, M.; Weinberg, M.P.; Gruninger, R.J.; Weigand, J.; Chen, L.; Perez-Lockett, K.; Bledsoe, C.; Denny, L.; Cibulskas, K.; et al. Enhanced surveillance for coccidioidomycosis, 14 US States, 2016. Emerg. Infect. Dis. 2018, 24, 1444–1452. [Google Scholar] [CrossRef]
- Carey, A.; Gorris, M.E.; Chiller, T.; Jackson, B.; Beadles, W.; Webb, B.J. Epidemiology, clinical features, and outcomes of coccidioidomycosis, Utah, 2006–2015. Emerg. Infect. Dis. 2021, 27, 2269–2277. [Google Scholar] [CrossRef] [PubMed]
- Diaz, J.H. Travel-related risk factors for coccidioidomycosis. J. Travel Med. 2018, 25, tay027. [Google Scholar] [CrossRef] [PubMed]
- Odio, C.D.; Marciano, B.E.; Galgiani, J.N.; Holland, S.M. Riskfactors for disseminated coccidioidomycosis, United States. Emerg. Infect. Dis. 2017, 23, 308–311. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Trends in aging—United States and worldwide. MMWR. Morb. Mortal. Wkly. Rep. 2003, 52, 101–104, 106. [Google Scholar]
- Fatima, M.; Patel, R.S.; Brunworth, J.R.; Gupta, K.A.; Roach, W.E.; Webeler, P.L.; Mundelein, C.R.; Mansour, M. A case of rapidly progressive coccidioidal meningitis in an immunocompetent patient. Cureus 2022, 14, e28643. [Google Scholar] [CrossRef] [PubMed]
- Gorris, M.E.; Neumann, J.E.; Kinney, P.L.; Sheahan, M.; Sarofim, M.C. Economic valuation of coccidioidomycosis (Valley fever) projections in the United States in response to climate change. Weather. Clim. Soc. 2021, 13, 1. [Google Scholar] [CrossRef]
- Grizzle, A.J.; Wilson, L.; Nix, D.E.; Galgiani, J.N. Clinical and economic burden of Valley fever in Arizona: An incidence-based cost-of-illness analysis. Open Forum Infect. Dis. 2021, 8, ofaa623. [Google Scholar] [CrossRef]
- State of California. Protection from Valley Fever. 2022. Available online: https://www.dir.ca.gov/dosh/valley-fever-home.html (accessed on 1 August 2022).
- Centers for Disease Control and Prevention. Valley Fever (Coccidioidomycosis) Risk & Prevention. 2022. Available online: https://www.cdc.gov/fungal/diseases/coccidioidomycosis/risk-prevention.html (accessed on 1 December 2022).
- James, A.E.; McCall, J.R.; Petersen, K.R.; Wohrle, R.D.; Oltean, H.N. A survey of veterinarians’ knowledge, attitudes and practices regarding an emerging disease: Coccidioidomycosis in Washington state. Zoonoses Public Health 2020, 67, 25–34. [Google Scholar] [CrossRef]
- Gubernot, D.M.; Boyer, B.L.; Moses, M.S. Animals as early detectors of bioevents: Veterinary tools and a framework for animal-human integrated zoonotic disease surveillance. Public Health Rep. 2008, 123, 300–315. [Google Scholar] [CrossRef]
- Johnson, R.H.; Sharma, R.; Kuran, R.; Fong, I.; Heidari, A. Coccidioidomycosis: A review. J. Investig. Med. Off. Publ. Am. Fed. Clin. Res. 2021, 69, 316–323. [Google Scholar] [CrossRef]
- Krogstad, P.; Johnson, R.; Garcia-Lloret, M.I.; Heidari, A.; Butte, M.J. Host-pathogen interactions in coccidioidomycosis: Prognostic clues and opportunities for novel therapies. Clin. Ther. 2019, 41, 1939–1954.e1. [Google Scholar] [CrossRef] [PubMed]
- Louie, L.; Ng, S.; Hajjeh, R.; Johnson, R.; Vugia, D.; Werner, S.B.; Talbot, R.; Klitz, W. Influence of host genetics on the severity of coccidioidomycosis. Emerg. Infect. Dis. 1999, 5, 672–680. [Google Scholar] [CrossRef] [PubMed]
- Seitz, A.E.; Prevots, D.R.; Holland, S.M. Hospitalizations associated with disseminated coccidioidomycosis, Arizona and California, USA. Emerg. Infect. Dis. 2012, 18, 1476–1479. [Google Scholar] [CrossRef] [PubMed]
- Hsu, A.P.; Korzeniowska, A.; Aguilar, C.C.; Gu, J.; Karlins, E.; Oler, A.J.; Chen, G.; Reynoso, G.V.; Davis, J.; Chaput, A.; et al. Immunogenetics associated with severe coccidioidomycosis. JCI Insight 2022, 7, e159491. [Google Scholar] [CrossRef] [PubMed]
- Hung, C.-Y.; Hsu, A.P.; Holland, S.M.; Fierer, J. A review of innate and adaptive immunity to coccidioidomycosis. Med. Mycol. 2019, 57 (Suppl. 1), S85–S92. [Google Scholar] [CrossRef]
- Galgiani, J.N.; Ampel, N.M.; Blair, J.E.; Catanzaro, A.; Geertsma, F.; Hoover, S.E.; Johnson, R.H.; Kusne, S.; Lisse, J.; MacDonald, J.D.; et al. Executive summary: 2016 Infectious Diseases Society of America (IDSA) Clinical Practice Guideline for the Treatment of Coccidioidomycosis. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2016, 63, 717–722. [Google Scholar] [CrossRef]
- Van den Bossche, H.; Willemsens, G.; Cools, W.; Lauwers, W.F.; Le Jeune, L. Biochemical effects of miconazole on fungi. II. Inhibition of ergosterol biosynthesis in Candida albicans. Chem.-Biol. Interact. 1978, 21, 59–78. [Google Scholar] [CrossRef]
- Thompson, G.R.; Barker, B.M.; Wiederhold, N.P. Large-scale evaluation of in vitro Amphotericin B, triazole, and echinocandin activity against Coccidioides species from U.S. institutions. Antimicrob. Agents Chemother. 2017, 61, e02634-16. [Google Scholar] [CrossRef]
- Hung, C.-Y.; Yu, J.-J.; Seshan, K.R.; Reichard, U.; Cole, G.T. A parasitic phase-specific adhesin of Coccidioides immitis contributes to the virulence of this respiratory Fungal pathogen. Infect. Immun. 2002, 70, 3443–3456. [Google Scholar] [CrossRef]
- Peláez-Jaramillo, C.A.; Jiménez-Alzate MD, P.; Araque-Marin, P.; Hung, C.-Y.; Castro-Lopez, N.; Cole, G.T. Lipid secretion by parasitic cells of Coccidioides contributes to disseminated disease. Front. Cell. Infect. Microbiol. 2021, 11, 592826. [Google Scholar] [CrossRef]
- Hoenigl, M.; Sprute, R.; Egger, M.; Arastehfar, A.; Cornely, O.A.; Krause, R.; Lass-Flörl, C.; Prattes, J.; Spec, A.; Thompson, G.R.; et al. The antifungal pipeline: Fosmanogepix, Ibrexafungerp, Olorofim, Opelconazole, and Rezafungin. Drugs 2021, 81, 1703–1729. [Google Scholar] [CrossRef] [PubMed]
- Thompson, G.R.; Lewis, J.S.; Nix, D.E.; Patterson, T.F. Current concepts and future directions in the pharmacology and treatment of coccidioidomycosis. Med. Mycol. 2019, 57 (Suppl. 1), S76–S84. [Google Scholar] [CrossRef] [PubMed]
- Wall, G.; Lopez-Ribot, J.L. Screening repurposing libraries for identification of drugs with novel antifungal activity. Antimicrob. Agents Chemother. 2020, 64, e00924-20. [Google Scholar] [CrossRef] [PubMed]
- Wouters, O.J.; McKee, M.; Luyten, J. Estimated research and development investment needed to bring a new medicine to market, 2009–2018. JAMA 2020, 323, 844–853. [Google Scholar] [CrossRef]
- Castro-Lopez, N.; Hung, C.-Y. Immune response to coccidioidomycosis and the development of a vaccine. Microorganisms 2017, 5, 13. [Google Scholar] [CrossRef]
- NIAID Valley Fever Research Working Group. NIAID Strategic Plan for Research to Develop a Valley Fever Vaccine. National Institute of Allergy and Infectious Disease. 2022; pp. 1–21. Available online: https://www.niaid.nih.gov/sites/default/files/niaid-strategic-plan-for-research-to-develop-a-valley-fever-vaccine9.9.22.pdf (accessed on 1 December 2022).
- Pappagianis, D. Evaluation of the protective efficacy of the killed Coccidioides immitis spherule vaccine in humans. The Valley Fever Vaccine Study Group. Am. Rev. Respir. Dis. 1993, 148, 656–660. [Google Scholar] [CrossRef]
- Hung, C.-Y.; Gonzalez, A.; Wüthrich, M.; Klein, B.S.; Cole, G.T. Vaccine immunity to coccidioidomycosis occurs by early activation of three signal pathways of T helper cell response (Th1, Th2, and Th17). Infect. Immun. 2011, 79, 4511–4522. [Google Scholar] [CrossRef]
- Narra, H.P.; Shubitz, L.F.; Mandel, M.A.; Trinh, H.T.; Griffin, K.; Buntzman, A.S.; Frelinger, J.A.; Galgiani, J.N.; Orbach, M.J. A Coccidioides posadasii CPS1 deletion mutant is avirulent and protects mice from lethal infection. Infect. Immun. 2016, 84, 3007–3016. [Google Scholar] [CrossRef]
- Shubitz, L.F.; Robb, E.J.; Powell, D.A.; Bowen, R.A.; Bosco-Lauth, A.; Hartwig, A.; Porter, S.M.; Trinh, H.; Moale, H.; Bielefeldt-Ohmann, H.; et al. Δcps1 vaccine protects dogs against experimentally induced coccidioidomycosis. Vaccine 2021, 39, 6894–6901. [Google Scholar] [CrossRef]
- Xue, J.; Chen, X.; Selby, D.; Hung, C.-Y.; Yu, J.-J.; Cole, G.T. A genetically engineered live attenuated vaccine of Coccidioides posadasii protects BALB/c mice against coccidioidomycosis. Infect. Immun. 2009, 77, 3196–3208. [Google Scholar] [CrossRef]
- Campuzano, A.; Zhang, H.; Ostroff, G.R.; Dos Santos Dias, L.; Wüthrich, M.; Klein, B.S.; Yu, J.-J.; Lara, H.H.; Lopez-Ribot, J.L.; Hung, C.-Y. CARD9-associated Dectin-1 and Dectin-2 are required for protective immunity of a multivalent vaccine against Coccidioides posadasii infection. J. Immunol. 1950, 204, 3296–3306. [Google Scholar] [CrossRef] [PubMed]
- Hung, C.-Y.; Zhang, H.; Castro-Lopez, N.; Ostroff, G.R.; Khoshlenar, P.; Abraham, A.; Cole, G.T.; Negron, A.; Forsthuber, T.; Peng, T.; et al. Glucan-chitin particles enhance Th17 response and improve protective efficacy of a multivalent antigen (rCpa1) against pulmonary Coccidioides posadasii infection. Infect. Immun. 2018, 86, e00070-18. [Google Scholar] [CrossRef] [PubMed]
- Hurtgen, B.J.; Hung, C.-Y.; Ostroff, G.R.; Levitz, S.M.; Cole, G.T. Construction and evaluation of a novel recombinant T cell epitope-based vaccine against coccidioidomycosis. Infect. Immun. 2012, 80, 3960–3974. [Google Scholar] [CrossRef] [PubMed]
- Das, R.; McNary, J.; Fitzsimmons, K.; Dobraca, D.; Cummings, K.; Mohle-Boetani, J.; Wheeler, C.; McDowell, A.; Iossifova, Y.; Bailey, R.; et al. Occupational coccidioidomycosis in California: Outbreak investigation, respirator recommendations, and surveillance findings. J. Occup. Environ. Med. 2012, 54, 564–571. [Google Scholar] [CrossRef]
- Nielsen-Gammon, J.W. The changing climate of Texas. In The Impact of Global Warming on Texas; University of Texas Press: Austin, TX, USA, 2011; Available online: http://www.jstor.org/stable/10.7560/723306 (accessed on 1 December 2022).
- Abatzoglou, J.T.; Dobrowski, S.Z.; Parks, S.A.; Hegewisch, K.C. TerraClimate, a high-resolution global dataset of monthly climate and climatic water balance from 1958–2015. Sci. Data 2018, 5, 1. [Google Scholar] [CrossRef]
- Sprigg, W.A.; Nickovic, S.; Galgiani, J.N.; Pejanovic, G.; Petkovic, S.; Vujadinovic, M.; Vukovic, A.; Dacic, M.; DiBiase, S.; Prasad, A.; et al. Regional dust storm modeling for health services: The case of valley fever. Aeolian Res. 2014, 14, 53–73. [Google Scholar] [CrossRef]
- Tong, D.Q.; Gorris, M.E.; Gill, T.E.; Ardon-Dryer, K.; Wang, J.; Ren, L. Dust storms, Valley fever, and public awareness. GeoHealth 2022, 6, e2022GH000642. [Google Scholar] [CrossRef]
- Comrie, A.C. No consistent link between dust storms and Valley fever (voccidioidomycosis). GeoHealth 2021, 5, e2021GH000504. [Google Scholar] [CrossRef]
- Smith, C.E.; Beard, R.R.; Rosenberger, H.G.; Whiting, E.G. Effect of season and dust control on coccidioidomycosis. J. Am. Med. Assoc. 1946, 132, 833–838. [Google Scholar] [CrossRef]
- Pappagianis, D.; Einstein, H. Tempest from Tehachapi takes toll or Coccidioides conveyed aloft and afar. West. J. Med. 1978, 129, 527–530. [Google Scholar]
- Williams, P.L.; Sable, D.L.; Mendez, P.; Smyth, L.T. Symptomatic coccidioidomycosis following a severe natural dust storm. An outbreak at the Naval Air Station, Lemoore, Calif. Chest 1979, 76, 566–570. [Google Scholar] [CrossRef] [PubMed]
- Prospero, J.M.; Ginoux, P.; Torres, O.; Nicholson, S.E.; Gill, T.E. Environmental characterization of global sources of atmospheric soil dust identified with the Nimbus 7 Total Ozone Mapping Spectrometer (TOMS) absorbing aerosol product. Rev. Geophys. 2002, 40, 2-1–2-31. [Google Scholar] [CrossRef]
- Baddock, M.C.; Bryant, R.G.; Acosta, M.D.; Gill, T.E. Understanding dust sources through remote sensing: Making a case for CubeSats. J. Arid Environ. 2021, 184, 104335. [Google Scholar] [CrossRef]
- Baddock, M.C.; Gill, T.E.; Bullard, J.E.; Acosta, M.D.; Rivera Rivera, N.I. Geomorphology of the Chihuahuan Desert based on potential dust emissions. J. Maps 2011, 7, 249–259. [Google Scholar] [CrossRef]
- Lee, J.A.; Gill, T.E.; Mulligan, K.R.; Dominguez Acosta, M.; Perez, A.E. Land use/land cover and point sources of the 15 December 2003 dust storm in southwestern North America. Geomorphology 2009, 105, 18–27. [Google Scholar] [CrossRef]
- Rivera Rivera, N.I.; Gill, T.E.; Bleiweiss, M.P.; Hand, J.L. Source characteristics of hazardous Chihuahuan Desert dust outbreaks. Atmos. Environ. 2010, 44, 2457–2468. [Google Scholar] [CrossRef]
- Kandakji, T.; Gill, T.E.; Lee, J.A. Drought and land use/land cover impact on dust sources in Southern Great Plains and Chihuahuan Desert of the U.S.: Inferring anthropogenic effect. Sci. Total Environ. 2021, 755, 142461. [Google Scholar] [CrossRef]
- Kandakji, T.; Gill, T.E.; Lee, J.A. Identifying and characterizing dust point sources in the southwestern United States using remote sensing and GIS. Geomorphology 2020, 353, 107019. [Google Scholar] [CrossRef]
- Lee, J.A.; Baddock, M.C.; Mbuh, M.J.; Gill, T.E. Geomorphic and land cover characteristics of aeolian dust sources in West Texas and eastern New Mexico, USA. Aeolian Res. 2012, 3, 459–466. [Google Scholar] [CrossRef]
- Kaplan, M.L.; Vellore, R.K.; Lewis, J.M.; Underwood, S.J.; Pauley, P.M.; Martin, J.E.; Rabin, R.M.; Krishnan, R. Subtropical-polar jet interactions in Southern Plains dust storms. J. Geophys. Res. Atmos. 2013, 118, 893–12914. [Google Scholar] [CrossRef]
- Schultz, J.A.; Meisner, B.N. The 24 February 2007 North Texas wind and dust storm: An impact weather event. Natl. Weather Dig. 2009, 33, 165–184. [Google Scholar]
- Ponette-González, A.G.; Collins, J.D.; Manuel, J.E.; Byers, T.A.; Glass, G.A.; Weathers, K.C.; Gill, T.E. Wet dust deposition across Texas during the 2012 drought: An overlooked pathway for elemental flux to ecosystems. J. Geophys. Res. Atmos. 2018, 123, 8238–8254. [Google Scholar] [CrossRef]
- Park, S.H.; Gong, S.L.; Zhao, T.L.; Vet, R.J.; Bouchet, V.S.; Gong, W.; Makar, P.A.; Moran, M.D.; Stroud, C.; Zhang, J. Simulation of entrainment and transport of dust particles within North America in April 2001 (“Red Dust Episode”). J. Geophys. Res. Atmos. 2007, 112, D20209. [Google Scholar] [CrossRef]
- Sprigg, W.A.; Gill, T.E.; Tong, D.Q.; Li, J.; Ren, L.; Pelt RS, V. Are opportunities to apply airborne dust research being missed? Bull. Am. Meteorol. Soc. 2022, 103, E1587–E1594. [Google Scholar] [CrossRef]
- Doggett, A.L.; Gill, T.E.; Peterson, R.E.; Bory, A.J.M.; Biscaye, P.E. Meteorological characteristics of a severe wind and dust emission event; southwestern USA, 6–7 April 2001. In Proceedings of the 21st Conference on Severe Local Storms, San Antonio, TX, USA, 11 August 2002; pp. 78–80. Available online: https://ams.confex.com/ams/pdfpapers/47573.pdf (accessed on 1 December 2022).
- Castañón-Olivares, L.R.; Mexican Coccidioidomycosis Study Group. Coccidiodin skin testing survey in México. In Proceedings of the 56th Coccidioidomycosis Study Group Meeting, Tucson, AZ, USA, 24 March 2012. [Google Scholar]
- Castañón Olivares, L.R.; Millán Chiu, B.; Valera Bermejo, A.; Zavala Velázquez, N.; Sánchez Paredes, E.; Aroch Calderón, A. Cases of Coccidioidomycosis in the Estados Unidos Mexicanos during the Period 1965–2004; 49th Coccidioidomycosis Study Group: Bass Lake, CA, USA, 2 April 2005. [Google Scholar]
- Gastélum-Cano, J.M.; Dautt-Castro, M.; García-Galaz, A.; Felix-Murray, K.; Rascón-Careaga, A.; Cano-Rangel, M.A.; Islas-Osuna, M.A. The clinical laboratory evolution in coccidioidomycosis detection: Future perspectives. J. Med. Mycol. 2021, 31, 101159. [Google Scholar] [CrossRef]
- Dirección General de Información en Salud. Cubos Dinámicos. 2022. Available online: http://www.dgis.salud.gob.mx/contenidos/basesdedatos/BD_Cubos_gobmx.html (accessed on 1 July 2022).
- Castillo-López, M.; Castañón Olivares, L.R.; Ponce-Rosas, R. El impacto de las condiciones ambientales en la respuesta a la intradermorreacción con coccidioidina en personas de Hermosillo, Son. In Proceedings of the IX Congreso Nacional de Micología Médica, Guadalajara, Jalisco, Mexico, 18–21 October 2017. [Google Scholar]
- Candolfi Arballo, O.; Cabañillas, L.; Castañón-Olivares, L.R. Resultados preliminares de la Intradermorreacción con Coccidioidina en cuatro zonas del Estado de Baja California; X Congreso Nacional de Micología Médica: Oaxtepec, Mexico, 2019. [Google Scholar]
- Texas Demographic Center. Demographic Trends and Population Projections for Texas and the North Texas Region. 2021. Available online: https://demographics.texas.gov/resources/presentations/osd/2021/2021_01_15_leadershipnorthtexas.pdf (accessed on 1 August 2022).
- US Census Bureau. QuickFacts Texas. 2022. Available online: https://www.census.gov/quickfacts/TX (accessed on 1 August 2022).
- US Census Bureau. Annual Estimates of the Resident Population for Counties in Arizona: April 1, 2010 to July 1, 2019 (CO-EST2019-ANNRES-04). 2020. Available online: https://www.census.gov/data/tables/time-series/demo/popest/2010s-counties-total.html (accessed on 1 August 2022).
- Texas Department of State Health Services. Table I Reported Diseases—Texas, 2009–2018; 2021. Available online: https://www.dshs.texas.gov/idps-home/infectious-disease-data-statistics/texas-annual-reports/texas-annual-reports-2010s/2018-annual-report (accessed on 1 August 2022).
- Mayo Clinic. Brucellosis. 2021. Available online: https://www.mayoclinic.org/diseases-conditions/brucellosis/symptoms-causes/syc-20351738 (accessed on 1 December 2022).
- Chow, N.A.; Kangiser, D.; Gade, L.; McCotter, O.Z.; Hurst, S.; Salamone, A.; Wohrle, R.; Clifford, W.; Kim, S.; Salah, Z.; et al. Factors influencing distribution of Coccidioides immitis in soil, Washington state, 2016. Msphere 2021, 6, e00598-21. [Google Scholar] [CrossRef]
- Litvintseva, A.P.; Marsden-Haug, N.; Hurst, S.; Hill, H.; Gade, L.; Driebe, E.M.; Ralston, C.; Roe, C.; Barker, B.M.; Goldoft, M.; et al. Valley fever: Finding new places for an old disease: Coccidioides immitis found in Washington state soil associated with recent human infection. Clin. Infect. Dis. 2015, 60, e1–e3. [Google Scholar] [CrossRef]
- Han, W.; Yang, Z.; Di, L.; Mueller, R. CropScape: A Web service based application for exploring and disseminating US conterminous geospatial cropland data products for decision support. Comput. Electron. Agric. 2012, 84, 111–123. [Google Scholar] [CrossRef]
- Horrigan, L.; Lawrence, R.S.; Walker, P. How sustainable agriculture can address the environmental and human health harms of industrial agriculture. Environ. Health Perspect. 2002, 110, 445–456. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gorris, M.E.; Ardon-Dryer, K.; Campuzano, A.; Castañón-Olivares, L.R.; Gill, T.E.; Greene, A.; Hung, C.-Y.; Kaufeld, K.A.; Lacy, M.; Sánchez-Paredes, E. Advocating for Coccidioidomycosis to Be a Reportable Disease Nationwide in the United States and Encouraging Disease Surveillance across North and South America. J. Fungi 2023, 9, 83. https://doi.org/10.3390/jof9010083
Gorris ME, Ardon-Dryer K, Campuzano A, Castañón-Olivares LR, Gill TE, Greene A, Hung C-Y, Kaufeld KA, Lacy M, Sánchez-Paredes E. Advocating for Coccidioidomycosis to Be a Reportable Disease Nationwide in the United States and Encouraging Disease Surveillance across North and South America. Journal of Fungi. 2023; 9(1):83. https://doi.org/10.3390/jof9010083
Chicago/Turabian StyleGorris, Morgan E., Karin Ardon-Dryer, Althea Campuzano, Laura R. Castañón-Olivares, Thomas E. Gill, Andrew Greene, Chiung-Yu Hung, Kimberly A. Kaufeld, Mark Lacy, and Edith Sánchez-Paredes. 2023. "Advocating for Coccidioidomycosis to Be a Reportable Disease Nationwide in the United States and Encouraging Disease Surveillance across North and South America" Journal of Fungi 9, no. 1: 83. https://doi.org/10.3390/jof9010083
APA StyleGorris, M. E., Ardon-Dryer, K., Campuzano, A., Castañón-Olivares, L. R., Gill, T. E., Greene, A., Hung, C.-Y., Kaufeld, K. A., Lacy, M., & Sánchez-Paredes, E. (2023). Advocating for Coccidioidomycosis to Be a Reportable Disease Nationwide in the United States and Encouraging Disease Surveillance across North and South America. Journal of Fungi, 9(1), 83. https://doi.org/10.3390/jof9010083







