Rationally Designed Oral DOX Gels for Colon-Specific Administration
Abstract
1. Introduction
2. Results and Discussion
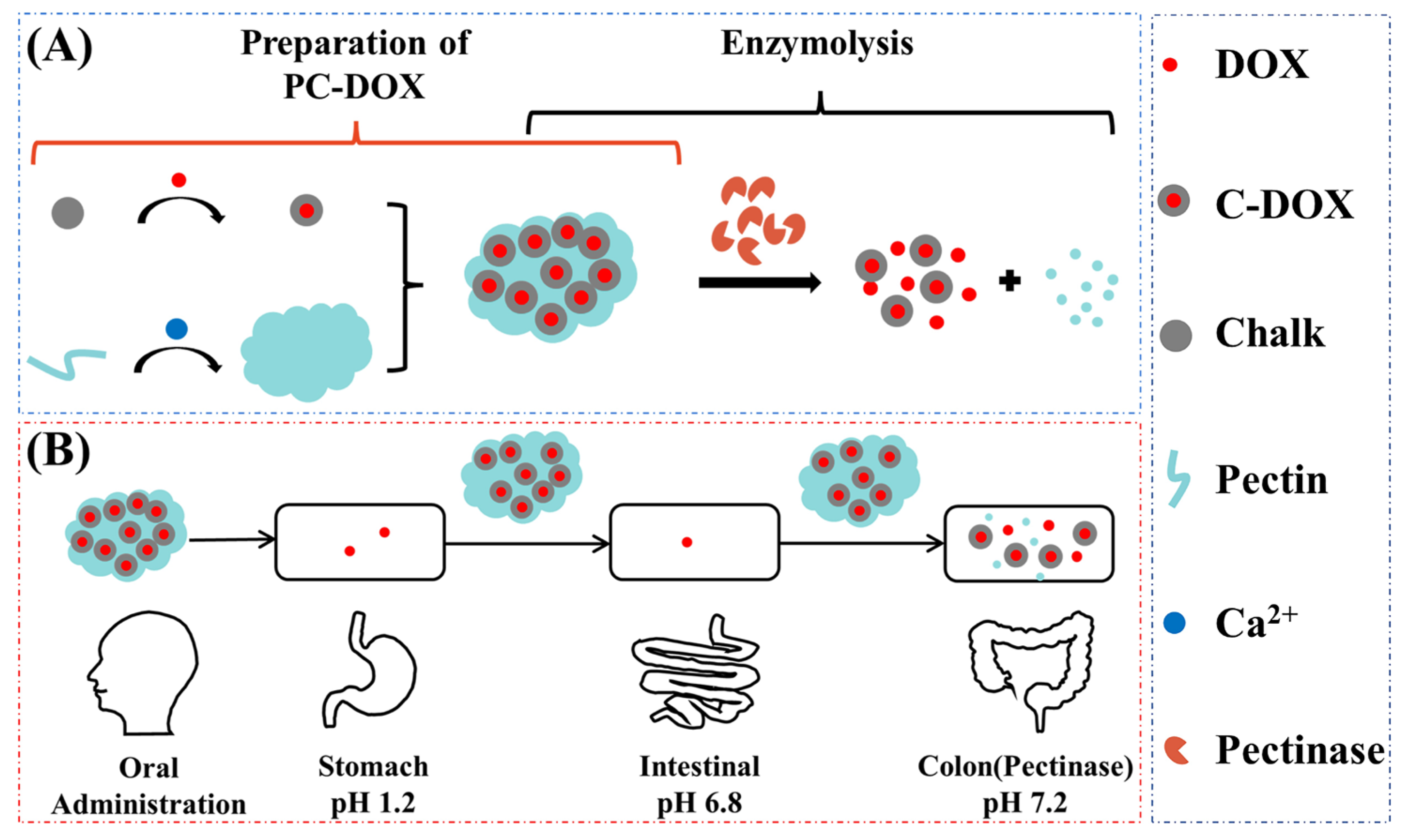
2.1. Preparation and Characterization of Pectin-Chalk DOX Gels (PC–DOX)
2.2. DOX Release Study of PC–DOX
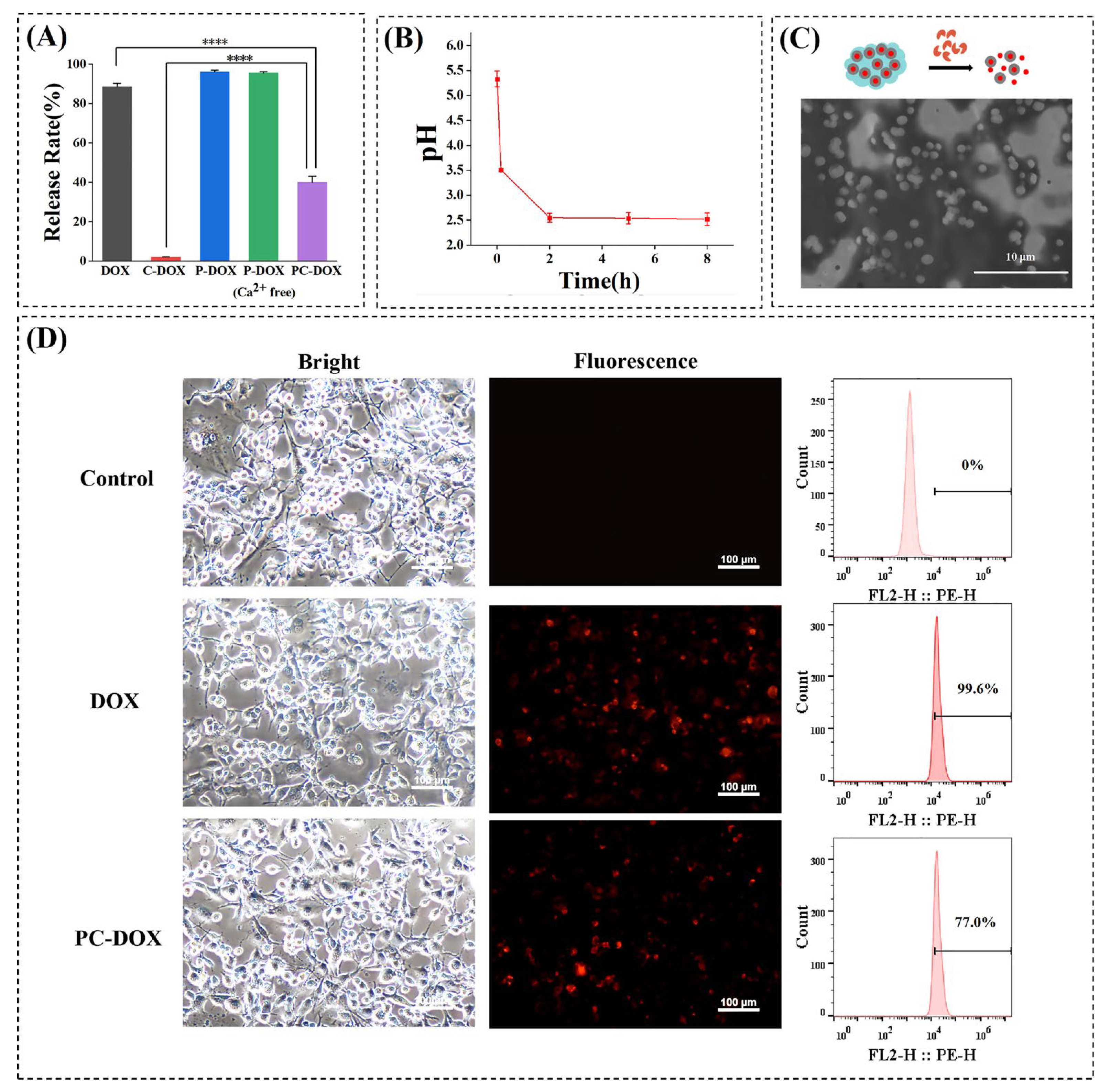
2.3. Enzyme-Responsive Release and Cell Uptake Assay
2.4. Distribution of PC–DOX in the GI Tract
3. Conclusions
4. Materials and Methods
4.1. Materials
4.2. Preparation and Characterization of PC–DOX
4.3. In Vitro Drug Release Experiments
4.4. Pectin Enzymolysis
4.5. Cell Uptake
4.6. In Vivo Drug Release Experiments
4.7. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Conflicts of Interest
References
- Davidson, K.W.; Barry, M.J.; Mangione, C.M.; Cabana, M.; Caughey, A.B.; Davis, E.M.; Donahue, K.E.; Doubeni, C.A.; Krist, A.H.; Kubik, M.; et al. Screening for Colorectal Cancer: US Preventive Services Task Force Recommendation Statement. Jama-J. Am. Med. Assoc. 2021, 325, 1965–1977. [Google Scholar]
- Siegel, R.L.; Miller, K.D.; Sauer, A.G.; Fedewa, S.A.; Butterly, L.F.; Anderson, J.C.; Cercek, A.; Smith, R.A.; Jemal, A. Colorectal cancer statistics, 2020. CA Cancer J. Clin. 2020, 70, 145–164. [Google Scholar] [CrossRef] [PubMed]
- Fakih, M.G. Metastatic Colorectal Cancer: Current State and Future Directions. J. Clin. Oncol. 2015, 33, 1809–1824. [Google Scholar] [CrossRef]
- Vodenkova, S.; Buchler, T.; Cervena, K.; Veskrnova, V.; Vodicka, P.; Vymetalkova, V. 5-fluorouracil and other fluoropyrimidines in colorectal cancer: Past, present and future. Pharmacol. Ther. 2020, 206, 107447. [Google Scholar] [CrossRef] [PubMed]
- Bruno, P.M.; Liu, Y.; Park, G.Y.; Murai, J.; Koch, C.E.; Eisen, T.J.; Pritchard, J.R.; Pommier, Y.; Lippard, S.J.; Hemann, M.T. A subset of platinum-containing chemotherapeutic agents kills cells by inducing ribosome biogenesis stress. Nat. Med. 2017, 23, 461–471. [Google Scholar] [CrossRef]
- Katona, B.W.; Weiss, J.M. Chemoprevention of Colorectal Cancer. Gastroenterology 2020, 158, 368–388. [Google Scholar] [CrossRef]
- Maroun, J.; Marginean, H.; Jonker, D.; Cripps, C.; Goel, R.; Asmis, T.; Goodwin, R.; Chiritescu, G. A Phase I Study of Irinotecan, Capecitabine (Xeloda), and Oxaliplatin in Patients With Advanced Colorectal Cancer. Clin. Color. Cancer 2018, 17, E257–E268. [Google Scholar] [CrossRef]
- Park, Y.N.; Kojiro, M.; di Tommaso, L.; Dhillon, A.R.; Kondo, F.; Nakano, M.; Sakamoto, M.; Theise, N.D.; Roncalli, M.; Laennec, G.M. Ductular reaction is helpful in defining early stromal invasion, small hepatocellular carcinomas, and dysplastic nodules. Cancer 2007, 109, 915–923. [Google Scholar] [CrossRef]
- Ciombor, K.K.; Wu, C.; Goldberg, R.M. Recent Therapeutic Advances in the Treatment of Colorectal Cancer. Annu. Rev. Med. 2015, 66, 83–95. [Google Scholar] [CrossRef]
- Dienstmann, R.; Salazar, R.; Tabernero, J. Personalizing Colon Cancer Adjuvant Therapy: Selecting Optimal Treatments for Individual Patients. J. Clin. Oncol. 2015, 33, 1787–1796. [Google Scholar] [CrossRef]
- Ryu, K.; Kuwabara, H.; Morimoto, K.; Sato, T.; Sanada, T.; Nakamura, N.; Goseki, N.; Koike, M. A Case of BRAF-Mutated Obstructive Colon Cancer with Liver Metastases Treated with Multidisciplinary Therapy, Gan to kagaku ryoho. Cancer Chemother. 2020, 47, 2207–2209. [Google Scholar]
- Rivankar, S. An overview of doxorubicin formulations in cancer therap. J. Cancer Res. Ther. 2014, 10, 853–858. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.; Wang, M.; He, H.; Li, J. Doxorubicin-Loaded Tumor-Targeting Peptide-Decorated Polypeptide Nanoparticles for Treating Primary Orthotopic Colon Cancer. Front. Pharmacol. 2021, 12, 744811. [Google Scholar] [CrossRef]
- Mathews, P.D.; Mertins, O.; Angelov, B.; Angelova, A. Cubosomal lipid nanoassemblies with pH-sensitive shells created by biopolymer complexes: A synchrotron SAXS study. J. Colloid Interface Sci. 2022, 607, 440–451. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Angelova, A.; Angelov, B.; Drechsler, M.; Garamus, V.M.; Willumeit-Roemer, R.; Zou, A. Sterically stabilized spongosomes for multidrug delivery of anticancer nanomedicines. J. Mater. Chem. B 2015, 3, 7734–7744. [Google Scholar] [CrossRef] [PubMed]
- Beukema, M.; Jermendi, E.; Koster, T.; Kitaguchi, K.; de Haan, B.J.; van den Berg, M.A.; Faas, M.M.; Schols, H.A.; de Vos, P. Attenuation of Doxorubicin-Induced Small Intestinal Mucositis by Pectins is Dependent on Pectin’s Methyl-Ester Number and Distribution. Mol. Nutr. Food Res. 2021, 65, 2100222. [Google Scholar] [CrossRef] [PubMed]
- Wanasawas, P.; Mitrevej, A.; Sinchaipanid, N. Influence of In Situ Calcium Pectinate Coating on Metoprolol Tartrate Pellets for Controlled Release and Colon-Specific Drug Delivery. Pharmaceutics 2022, 14, 1061. [Google Scholar] [CrossRef] [PubMed]
- Dizaj, S.M.; Barzegar-Jalali, M.; Zarrintan, M.H.; Adibkia, K.; Lotfipour, F. Calcium carbonate nanoparticles as cancer drug delivery system. Expert Opin. Drug Deliv. 2015, 12, 1649–1660. [Google Scholar] [CrossRef]
- Liu, X.Z.; Lu, P.J.; Wang, Y. Research progress of dental machinable materials. Beijing Da Xue Xue Bao Yi Xue Ban J. Peking Univ. Health Sci. 2008, 40, 654–657. [Google Scholar]
- Huuse, M. Detailed morphology of the Top Chalk surface in the eastern Danish North Sea. Pet. Geosci. 1999, 5, 303–314. [Google Scholar] [CrossRef]
- Okhrimenko, D.V.; Dalby, K.N.; Skovbjerg, L.L.; Bovet, N.; Christensen, J.H.; Stipp, S.L.S. The surface reactivity of chalk (biogenic calcite) with hydrophilic and hydrophobic functional groups. Geochim. Cosmochim. Acta 2014, 128, 212–224. [Google Scholar] [CrossRef]
- Cao, L.; Lu, W.; Mata, A.; Nishinari, K.; Fang, Y. Egg-box model-based gelation of alginate and pectin: A review. Carbohydr. Polym. 2020, 242, 116389. [Google Scholar] [CrossRef] [PubMed]
- Abdelrahman, T.M.; Qin, X.; Li, D.; Senosy, I.A.; Mmby, M.; Wan, H.; Li, J.; He, S. Pectinase-responsive carriers based on mesoporous silica nanoparticles for improving the translocation and fungicidal activity of prochloraz in rice plants. Chem. Eng. J. 2021, 404, 126440. [Google Scholar] [CrossRef]
- Grassino, A.N.; Barba, F.J.; Brnčić, M.; Lorenzo, J.M.; Lucini, L.; Brnčić, S.R. Analytical tools used for the identification and quantification of pectin extracted from plant food matrices, wastes and by-products: A review. Food Chem. 2018, 266, 47–55. [Google Scholar] [CrossRef]
- Pathikonda, M.; Sachdeva, P.; Malhotra, N.; Fisher, R.S.; Maurer, A.H.; Parkman, H.P. Gastric Emptying Scintigraphy Is Four Hours Necessary? J. Clin. Gastroenterol. 2012, 46, 209–215. [Google Scholar] [CrossRef]
- Pathikonda, M.; Kantor, S.; Fisher, R.S.; Knight, L.C.; Maurer, A.H.; Parkman, H.P. Regional Analysis of Gastric Emptying Scintigraphy Provides Better Correlation of Dyspeptic Symptoms With Abnormal Gastric Emptying. Gastroenterology 2011, 140, S25. [Google Scholar] [CrossRef]
- Jakulj, L.; Vissers, M.N.; van Roomen, C.P.; van der Veen, J.N.; Vrins, C.L.J.; Kunne, C.; Stellaard, F.; Kastelein, J.J.P.; Groen, A.K. Ezetimibe stimulates faecal neutral sterol excretion depending on abcg8 function in mice. FEBS Lett. 2010, 584, 3625–3628. [Google Scholar] [CrossRef]
- Sudareva, N.; Suvorova, O.; Saprykina, N.; Vlasova, H.; Vilesov, A. Doxorubicin delivery systems based on doped CaCO3 cores and polyanion drug conjugates. J. Microencapsul. 2021, 38, 164–176. [Google Scholar] [CrossRef]
- Berardi, A.; Castells-Graells, R.; Lomonossoff, G.P. High stability of plant-expressed virus-like particles of an insect virus in artificial gastric and intestinal fluids. Eur. J. Pharm. Biopharm. 2020, 155, 103–111. [Google Scholar] [CrossRef]

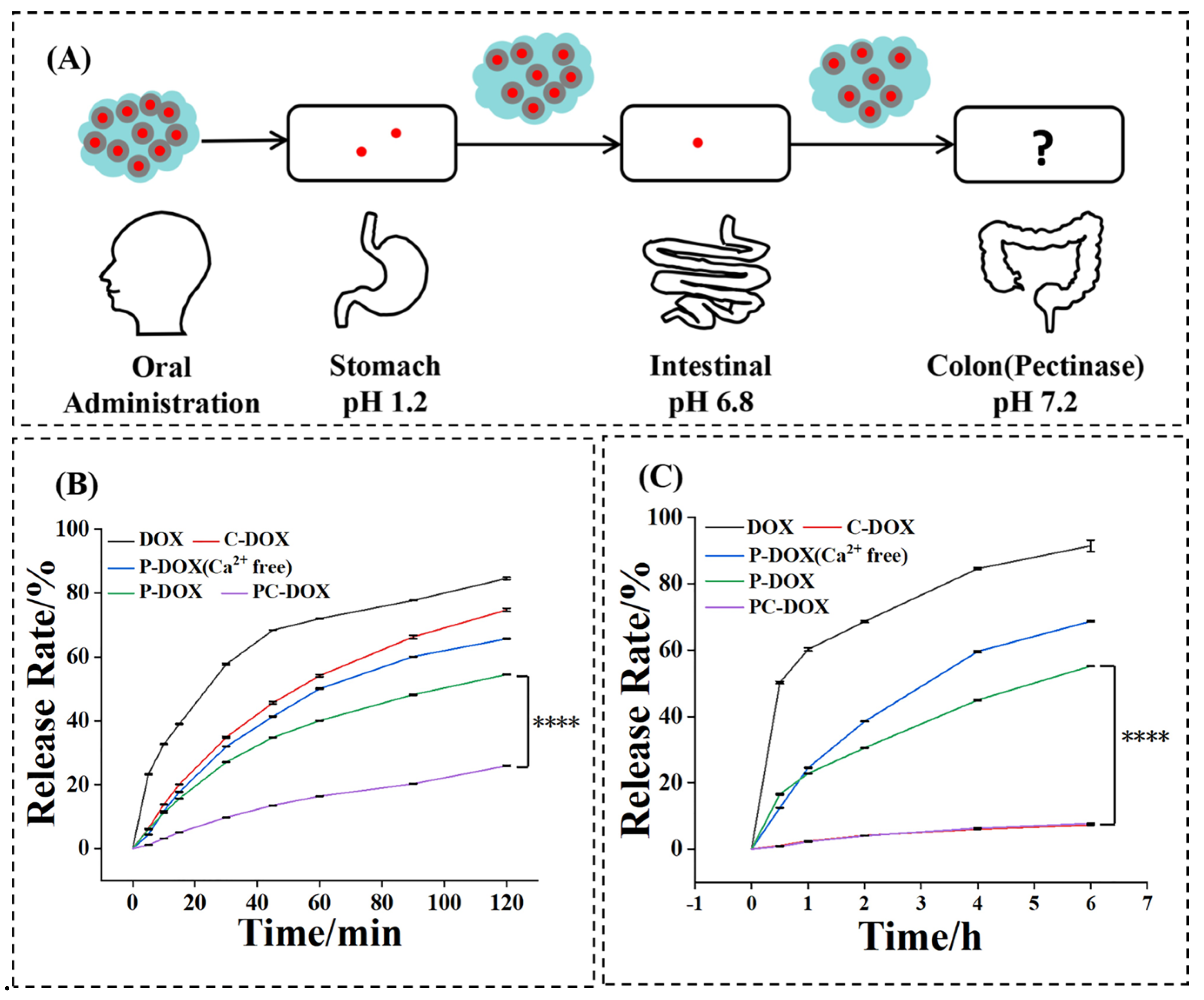

| Stomach (%) | Intestinal (%) | Colon-Targeting Efficiency (%) | |
|---|---|---|---|
| DOX C–DOX P–DOX (Ca2+ free) | 84.58 | 91.40 | 1.33 |
| 74.69 | 7.28 | 23.47 | |
| 65.67 | 68.69 | 10.75 | |
| P–DOX | 54.48 | 55.19 | 20.42 |
| PC–DOX | 25.93 | 7.80 | 68.29 |
| pH Value | |
|---|---|
| 3% pectin | 3.55 |
| 3% pectin adjusted to neutral | 6.99 |
| 2% pectinase | 5.4 |
| 10% CaCl2 | 9.0 |
| Pectin-Ca2+ gel | 7.99 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, J.; Ma, L.; Wang, C.; Jiang, P.; Cui, P.; Wang, J. Rationally Designed Oral DOX Gels for Colon-Specific Administration. Gels 2022, 8, 759. https://doi.org/10.3390/gels8120759
Li J, Ma L, Wang C, Jiang P, Cui P, Wang J. Rationally Designed Oral DOX Gels for Colon-Specific Administration. Gels. 2022; 8(12):759. https://doi.org/10.3390/gels8120759
Chicago/Turabian StyleLi, Jie, Luping Ma, Cheng Wang, Pengju Jiang, Pengfei Cui, and Jianhao Wang. 2022. "Rationally Designed Oral DOX Gels for Colon-Specific Administration" Gels 8, no. 12: 759. https://doi.org/10.3390/gels8120759
APA StyleLi, J., Ma, L., Wang, C., Jiang, P., Cui, P., & Wang, J. (2022). Rationally Designed Oral DOX Gels for Colon-Specific Administration. Gels, 8(12), 759. https://doi.org/10.3390/gels8120759










