Radiological Comparison of Canal Fill between Collared and Non-Collared Femoral Stems: A Two-Year Follow-Up after Total Hip Arthroplasty
Abstract
:1. Introduction
2. Methods
2.1. Study Design
2.2. Baseline Demographics and Stratification
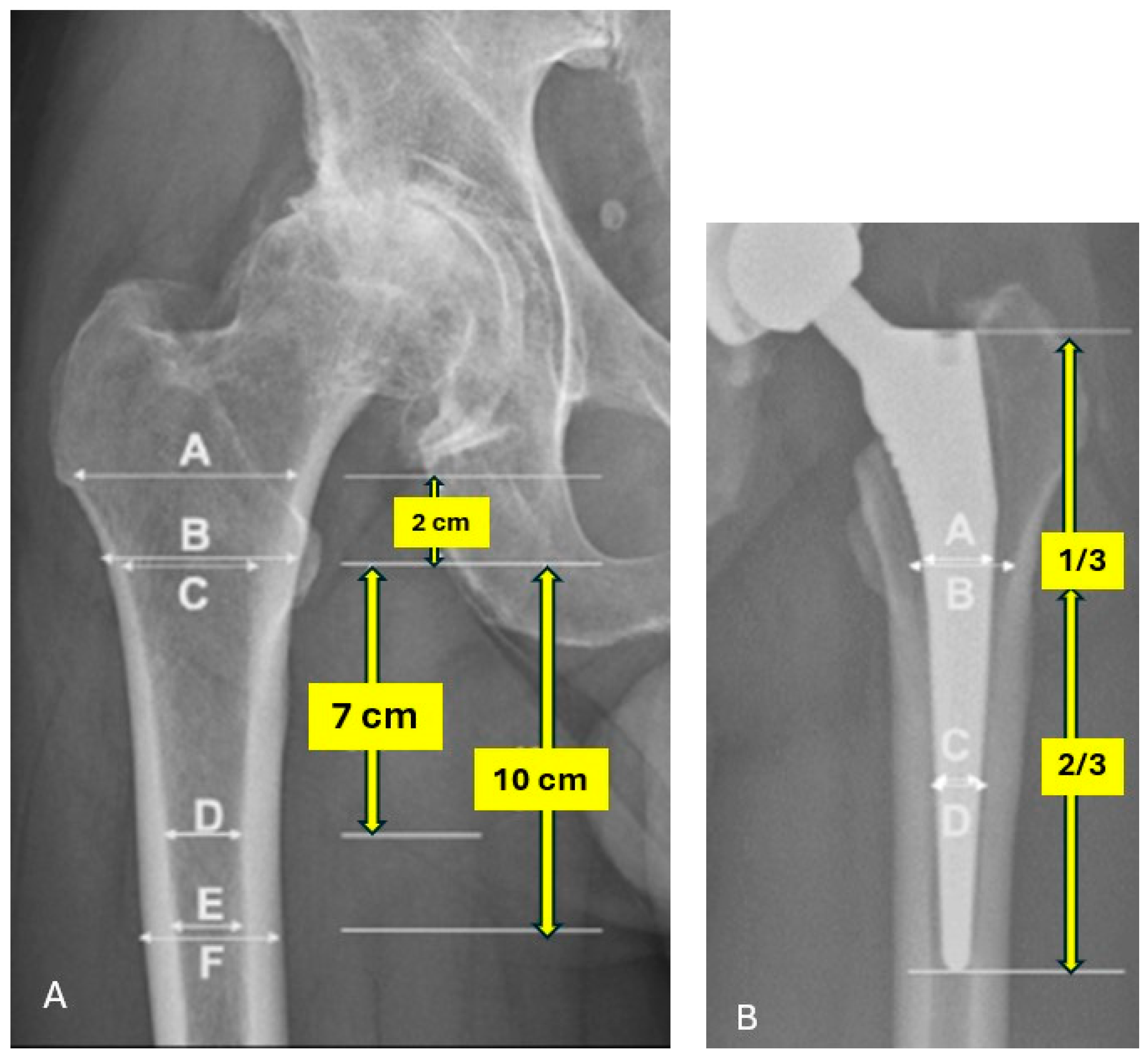
2.3. Preoperative Radiographic Assessment
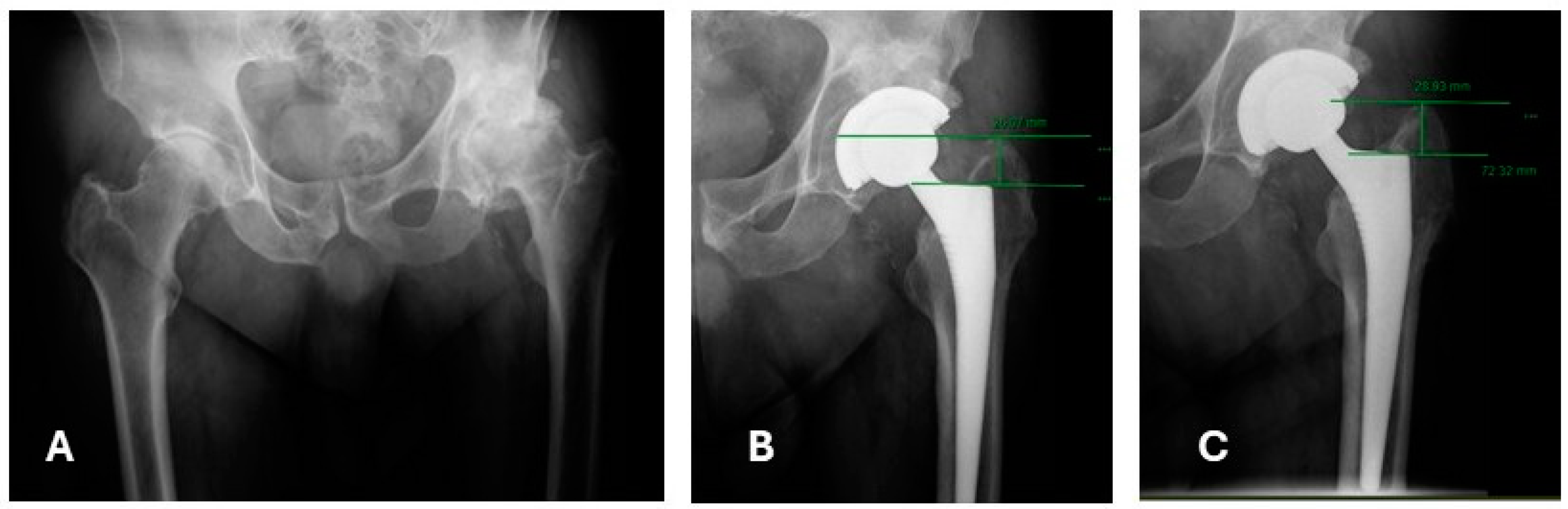
2.4. Postoperative Radiographic Assessment
2.5. Statistical Analysis
3. Results
3.1. Patient Demographics and Preoperative Radiographic Assessment
3.2. Postoperative Radiographic Outcomes at Two-Year Follow-Up
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Learmonth, I.D.; Young, C.; Rorabeck, C. The operation of the century: Total hip replacement. Lancet 2007, 370, 1508–1519. [Google Scholar] [CrossRef] [PubMed]
- Engh, C.A.; McGovern, T.F.; Bobyn, J.D.; Harris, W.H. A quantitative evaluation of periprosthetic bone-remodeling after cementless total hip arthroplasty. J. Bone Jt. Surg.—Ser. A 1992, 74, 1009–1020. [Google Scholar] [CrossRef]
- Shichman, I.; Roof, M.; Askew, N.; Nherera, L.; Rozell, J.C.; Seyler, T.M.; Schwarzkopf, R. Projections and Epidemiology of Primary Hip and Knee Arthroplasty in Medicare Patients to 2040–2060. JBJS Open Access 2023, 8, e22. [Google Scholar] [CrossRef] [PubMed]
- Shichman, I.; Askew, N.; Habibi, A.; Nherera, L.; Macaulay, W.; Seyler, T.; Schwarzkopf, R. Projections and Epidemiology of Revision Hip and Knee Arthroplasty in the United States to 2040–2060. Arthroplast. Today 2023, 21, 101152. [Google Scholar] [CrossRef] [PubMed]
- Toci, G.R.; Magnuson, J.A.; DeSimone, C.A.; Stambough, J.B.; Star, A.M.; Saxena, A. A Systematic Review and Meta-Analysis of Non-database Comparative Studies on Cemented Versus Uncemented Femoral Stems in Primary Elective Total Hip Arthroplasty. J. Arthroplast. 2022, 37, 1888–1894. [Google Scholar] [CrossRef] [PubMed]
- Firestone, D.E.; Callaghan, J.J.; Liu, S.S.; Goetz, D.D.; Sullivan, P.M.; Vittetoe, D.A.; Johnston, R.C. Total hip arthroplasty with a cemented, polished, collared femoral stem and a cementless acetabular component: A follow-up study at a minimum of ten years. J. Bone Jt. Surg. 2007, 89, 126–132. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.; Ksheersagar, V.; Aggarwal, S.; Jindal, K.; Dadra, A.; Kumar, V.; Patel, S. Complications and mid to long term outcomes for hip resurfacing versus total hip replacement: A systematic review and meta-analysis. Eur. J. Orthop. Surg. Traumatol. 2023, 33, 1495–1504. [Google Scholar] [CrossRef] [PubMed]
- Orita, K.; Goto, K.; Kuroda, Y.; Kawai, T.; Okuzu, Y.; Takaoka, Y.; Matsuda, S. Long-term outcome of primary total hip arthroplasty with cementless bioactive glass ceramic bottom-coated implants and highly cross-linked polyethylene: A minimum 10-year analysis. J. Orthop. Sci. 2023, 28, 385–390. [Google Scholar] [CrossRef] [PubMed]
- Holappa, E.; Kettunen, J.; Miettinen, H.; Kröger, H.; Miettinen, S. Long-term survival analysis of cementless large-diameter head metal-on-metal total hip arthroplasty. Arch. Orthop. Trauma Surg. 2023, 143, 4437–4446. [Google Scholar] [CrossRef] [PubMed]
- Yoon, B.H.; Park, J.W.; Lee, Y.K.; Koo, K.H.; Chang, C.B. Long-Term Wear-Related Complications of Cross-Linked versus Conventional Polyethylene after Total Hip Arthroplasty: A Meta-Analysis. J. Arthroplast. 2022, 37, 2308–2315.e2. [Google Scholar] [CrossRef] [PubMed]
- Konan, S.; Abdel, M.P.; Haddad, F.S. Cemented versus uncemented hip implant fixation: Should there be age thresholds? Bone Jt. Res. 2019, 8, 604–607. [Google Scholar] [CrossRef]
- Lemme, N.J.; McDonald, C.L.; Hamilton, W.G.; Crisco, J.J.; Cohen, E.M. Uncemented Collared Femoral Stems in Total Hip Arthroplasty. Orthopedics 2022, 45, e122–e126. [Google Scholar] [CrossRef]
- Elbardesy, H.; Anazor, F.; Mirza, M.; Aly, M.; Maatough, A. Cemented versus uncemented stems for revision total hip replacement: A systematic review and meta-analysis. World J. Orthop. 2023, 14, 630–640. [Google Scholar] [CrossRef] [PubMed]
- Gkagkalis, G.; Goetti, P.; Mai, S.; Meinecke, I.; Helmy, N.; Bosson, D.; Kutzner, K.P. Cementless short-stem total hip arthroplasty in the elderly patient—Is it a safe option? A prospective multicentre observational study. BMC Geriatr. 2019, 19, 112. [Google Scholar] [CrossRef] [PubMed]
- Ikemura, S.; Motomura, G.; Hamai, S.; Fujii, M.; Kawahara, S.; Sato, T.; Hara, D.; Shiomoto, K.; Nakashima, Y. Tapered wedge stems decrease early postoperative subsidence following cementless total hip arthroplasty in Dorr type C femurs compared to fit-and-fill stems. J. Orthop. Surg. Res. 2022, 17, 223. [Google Scholar] [CrossRef]
- Ishii, S.; Homma, Y.; Baba, T.; Ozaki, Y.; Matsumoto, M.; Kaneko, K. Does the Canal Fill Ratio and Femoral Morphology of Asian Females Influence Early Radiographic Outcomes of Total Hip Arthroplasty With an Uncemented Proximally Coated, Tapered-Wedge Stem? J. Arthroplast. 2016, 31, 1524–1528. [Google Scholar] [CrossRef] [PubMed]
- Mirza, S.B.; Dunlop, D.G.; Panesar, S.S.; Naqvi, S.G.; Gangoo, S.; Salih, S. Basic Science Considerations in Primary Total Hip Replacement Arthroplasty. Open Orthop. J. 2010, 4, 169–180. [Google Scholar] [CrossRef] [PubMed]
- Veldman, H.D.; Boymans, T.A.E.J.; van Steenbergen, L.N.; Heyligers, I.C. Age-Associated Changes in Proximal Femur Morphology Affect Femoral Component Sizing in Cementless Hip Arthroplasty. Geriatr. Orthop. Surg. Rehabil. 2022, 13, 21514593221144615. [Google Scholar] [CrossRef] [PubMed]
- Husmann, O.; Rubin, P.J.; Leyvraz, P.F.; De Roguin, B.; Argenson, J.N. Three-dimensional morphology of the proximal femur. J. Arthroplast. 1997, 12, 444–450. [Google Scholar] [CrossRef]
- Flecher, X.; Blanc, G.; Sainsous, B.; Parratte, S.; Argenson, J.N. A customised collared polished stem may reduce the complication rate of impaction grafting in revision hip surgery. J. Bone Jt. Surg.—Ser. B 2012, 94, 609–614. [Google Scholar] [CrossRef]
- Demey, G.; Fary, C.; Lustig, S.; Neyret, P.; Si Selmi, T.A. Does a Collar Improve the Immediate Stability of Uncemented Femoral Hip Stems in Total Hip Arthroplasty? A Bilateral Comparative Cadaver Study. J. Arthroplast. 2011, 26, 1549–1555. [Google Scholar] [CrossRef] [PubMed]
- Tierney, J.; Jackman, E.; Holder, C.; Wall, C.J.; Wilson, C.J. Increased Rates of Late Periprosthetic Fractures in Larger Hydroxyapatite-Coated Cementless Stems: Are Collared Stems a Better Alternative for Total Hip Arthroplasty? J. Arthroplast. 2024, 39, 744–749. [Google Scholar] [CrossRef] [PubMed]
- Lamb, J.N.; Van Duren, B.H.; Redmond, A.; Pandit, H.G.; Baetz, J.; Messer-Hannemann, P.; Morlock, M.M.; Adekanmbi, I.; West, R.M. A calcar collar is protective against early periprosthetic femoral fracture around cementless femoral components in primary total hip arthroplasty: A registry study with biomechanical validation. Bone Jt. J. 2019, 101, 779–786. [Google Scholar] [CrossRef] [PubMed]
- Nerys-Figueroa, J.; Parsa, A.; Curley, A.; Charif, S.; Domb, B.G.; Schinsky, M.F. Slightly reduced early subsidence with similar outcomes and complications rate in collared stems—A systematic review of randomized clinical trials. J. Orthop. 2024, 50, 170–176. [Google Scholar] [CrossRef] [PubMed]
- Ebramzadeh, E.; Sangiorgio, S.N.; Longjohn, D.B.; Buhari, C.F.; Dorr, L.D. Initial Stability of Cemented Femoral Stems as a Function of Surface Finish, Collar, and Stem Size. J. Bone Jt. Surg. 2004, 86, 106–115. [Google Scholar] [CrossRef] [PubMed]
- Weber, E.; Sundberg, M.; Flivik, G. Design modifications of the uncemented Furlong hip stem result in minor early subsidence but do not affect further stability: A randomized controlled RSA study with 5-year follow-up. Acta Orthop. 2014, 85, 556–561. [Google Scholar] [CrossRef] [PubMed]
- Bonin, N.; Gedouin, J.E.; Pibarot, V.; Bejui-Hughues, J.; Bothorel, H.; Saffarini, M.; Batailler, C. Proximal femoral anatomy and collared stems in hip arthroplasty: Is a single collar size sufficient? J. Exp. Orthop. 2017, 4, 32. [Google Scholar] [CrossRef] [PubMed]
- Mulcahy, H.; Chew, F.S. Current concepts of hip arthroplasty for radiologists: Part 1, features and radiographic assessment. Am. J. Roentgenol. 2012, 199, 559–569. [Google Scholar] [CrossRef] [PubMed]
- Doyle, D.J.; Goyal, A.; Garmon, E.H. American Society of Anesthesiologists Classification. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Faundez, J.; Carmona, M.; Klaber, I.; Zamora, T.; Botello, E.; Schweitzer, D. Radiographic Assessment of Bone Quality Using 4 Radiographic Indexes: Canal Diaphysis Ratio Is Superior. J. Arthroplast. 2024, 39, 427–432. [Google Scholar] [CrossRef] [PubMed]
- Wilkerson, J.; Fernando, N.D. Classifications in Brief: The Dorr Classification of Femoral Bone. Clin. Orthop. Relat. Res. 2020, 478, 1939–1944. [Google Scholar] [CrossRef] [PubMed]
- Yeung, Y.; Chiu, K.Y.; Yau, W.P.; Tang, W.M.; Cheung, W.Y.; Ng, T.P. Assessment of the Proximal Femoral Morphology Using Plain Radiograph-Can it Predict the Bone Quality? J. Arthroplast. 2006, 21, 508–513. [Google Scholar] [CrossRef] [PubMed]
- D’Ambrosio, A.; Peduzzi, L.; Roche, O.; Bothorel, H.; Saffarini, M.; Bonnomet, F. Influence of femoral morphology and canal fill ratio on early radiological and clinical outcomes of uncemented total hip arthroplasty using a fully coated stem. Bone Jt. Res. 2020, 9, 182–191. [Google Scholar] [CrossRef] [PubMed]
- Aydin, N.; Bezer, M.; Akgulle, A.H.; Saygi, B.; Kocaoǧlu, B.; Guven, O. Comparison of distal and proximal centralising devices in hip arthroplasty. Int. Orthop. 2009, 33, 945–948. [Google Scholar] [CrossRef] [PubMed]
- Bornes, T.D.; Radomski, L.R.; Bonello, J.P.; Mortensen-Truscott, L.; Safir, O.A.; Gross, A.E.; Kuzyk, P.R.T. Subsidence of a Single-Taper Femoral Stem in Primary Total Hip Arthroplasty: Characterization, Associated Factors, and Sequelae. J. Arthroplast. 2023, 38, S174–S178. [Google Scholar] [CrossRef] [PubMed]
- Shrout, P.E.; Fleiss, J.L. Intraclass correlations: Uses in assessing rater reliability. Psychol. Bull. 1979, 86, 420–428. [Google Scholar] [CrossRef] [PubMed]
- Giovanoulis, V.; Kenanidis, E.; Aïm, F.; Gamie, Z.; Marmor, S.; Potoupnis, M.; Lustig, S.; Tsiridis, E. Collared versus collarless hydroxyapatite-coated stems for primary cementless total hip arthroplasty; a systematic review of comparative studies. Is there any difference in survival, functional, and radiographic outcomes? SICOT J. 2024, 10, 8. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, R.; Mishima, H.; Totsuka, S.; Nishino, T.; Yamazaki, M. Primary Stability of Collared and Collarless Cementless Femoral Stems—A Finite Element Analysis Study. Arthroplast. Today 2023, 21, 101140. [Google Scholar] [CrossRef] [PubMed]
- Meding, J.B.; Ritter, M.A.; Keating, E.M.; Faris, P.M. Comparison of collared and collarless femoral components in primary uncemented total hip arthroplasty. J. Arthroplast. 1997, 12, 273–280. [Google Scholar] [CrossRef] [PubMed]
- Gema, A.; Irianto, K.A.; Setiawati, R. Femoral stem subsidence and its associated factors after cementless bipolar hemiarthroplasty in geriatric patients. Malays. Orthop. J. 2021, 15, 63–71. [Google Scholar] [CrossRef] [PubMed]
- Johnson, A.J.; Desai, S.; Zhang, C.; Koh, K.; Zhang, L.Q.; Costales, T.; O’Toole, R.V.; Manson, T.T. A Calcar Collar Is Protective Against Early Torsional/ Spiral Periprosthetic Femoral Fracture A Paired Cadaveric Biomechanical Analysis. J. Bone Jt. Surg. 2020, 102, 1427–1433. [Google Scholar] [CrossRef] [PubMed]
- Al-Dirini, R.M.A.; Huff, D.; Zhang, J.; Besier, T.; Clement, J.G.; Taylor, M. Influence of collars on the primary stability of cementless femoral stems: A finite element study using a diverse patient cohort. J. Orthop. Res. 2018, 36, 1185–1195. [Google Scholar] [CrossRef] [PubMed]
- Shichman, I.; Lawrence, K.W.; Berzolla, E.; Hernandez, C.S.; Man-El, R.; Warschawski, Y.; Snir, N.; Schwarzkopf, R.; Hepinstall, M.S. Comparison of canal fill and radiolucent line formation between two fully coated, hydroxyapatite tapered stems: A 2-year follow-up after total hip arthroplasty. Arch. Orthop. Trauma Surg. 2023, 143, 6945–6954. [Google Scholar] [CrossRef] [PubMed]
- Hu, C.Y.; Yoon, T.R. Recent updates for biomaterials used in total hip arthroplasty. Biomater. Res. 2018, 22, 33. [Google Scholar] [CrossRef] [PubMed]
- Savin, L.; Pinteala, T.; Mihai, D.N.; Mihailescu, D.; Miu, S.S.; Sirbu, M.T.; Veliceasa, B.; Popescu, D.C.; Sirbu, P.D.; Forna, N. Updates on Biomaterials Used in Total Hip Arthroplasty (THA). Polymers 2023, 15, 3278. [Google Scholar] [CrossRef] [PubMed]
- Holt, G.; Smith, R.; Duncan, K.; Hutchison, J.D.; Reid, D. Changes in population demographics and the future incidence of hip fracture. Injury 2009, 40, 722–726. [Google Scholar] [CrossRef] [PubMed]
- Baker, P.N.; Salar, O.; Ollivere, B.J.; Forward, D.P.; Weerasuriya, N.; Moppett, I.K.; Moran, C.G. Evolution of the hip fracture population: Time to consider the future? A retrospective observational analysis. BMJ Open 2014, 4, e004405. [Google Scholar] [CrossRef] [PubMed]
| Overall | Non-Collared | Collared | p-Value | |
|---|---|---|---|---|
| Number of patients | 202 | 99 | 103 | |
| Sex (Men), n (%) | 82 (41.6) | 45 (45.5) | 37 (35.9) | 0.34 |
| Mean Age (SD) | 63.94 (13.9) | 61.7 (15.2) | 66.4 (12.1) | 0.02 |
| Mean BMI (SD) | 28.7 (5) | 29 (5.1) | 28.6 (4.9) | 0.55 |
| ASA, n (%) | 0.01 | |||
| 1 | 13 (6.6) | 11 (11.1) | 2 (2.0) | |
| 2 | 144 (73.1) | 64 (64.6) | 80 (81.6) | |
| 3 | 40 (20.3) | 24 (24.2) | 16 (16.3) | |
| Primary Dx., n (%) | 0.23 | |||
| AVN | 17 (8.6) | 8 (8.1) | 9 (9.2) | |
| DDH | 6 (3.0) | 6 (6.1) | 0 (0.0) | |
| OA | 167 (84.8) | 81 (81.8) | 86 (87.8) | |
| AVN and OA | 3 (1.5) | 1 (1.0) | 2 (2.0) | |
| Other | 4 (2.0) | 3 (3.0) | 1 (1.0) | |
| Mean CCR (E/C) (SD) * | 0.5 (0.1) | 0.47 (0.8) | 0.44 (0.4) | 0.14 |
| Mean CFI (A/E) (SD) * | 3.4 (0.6) | 3.4 (0.6) | 3.5 (0.7) | 0.12 |
| Mean MCI (B/D) (SD) * | 2.8 (0.4) | 2.7 (0.4) | 2.8 (0.4) | 0.26 |
| Mean CBR (E/F) (SD) * | 0.5 (0.1) | 0.5 (0.1) | 0.5 (0.1) | 0.50 |
| Dorr Classification, n (%) | 0.15 | |||
| A | 140 (69.3) | 64 (64.6) | 76 (73.8) | |
| B | 62 (30.7) | 35 (35.4) | 27 (26.3) | |
| C | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Collared (n = 103) | Non-Collared (n = 99) | p-Value | |
|---|---|---|---|
| Spot Welds, n (%) | 20 (19.4) | 14 (14.1) | 0.35 |
| Pedestal Sign, n (%) | 0 (0.0) | 1 (1.0) | 0.49 |
| Stress Shielding, n (%) | 29 (28.2) | 31 (31.3) | 0.65 |
| Subsidence ≥ 5 mm, n (%) | 12 (11.7) | 19 (19.2) | 0.17 |
| Median A/B Ratio [IQR] * | 1.1 [1.06, 1.2] | 1.1 [1.05, 1.18] | 0.59 |
| Median C/D Ratio [IQR] * | 1.9 [1.8, 2.1] | 1.9 [1.75, 2.16] | 0.27 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ashkenazi, I.; Benady, A.; Ben Zaken, S.; Factor, S.; Abadi, M.; Shichman, I.; Morgan, S.; Gold, A.; Snir, N.; Warschawski, Y. Radiological Comparison of Canal Fill between Collared and Non-Collared Femoral Stems: A Two-Year Follow-Up after Total Hip Arthroplasty. J. Imaging 2024, 10, 99. https://doi.org/10.3390/jimaging10050099
Ashkenazi I, Benady A, Ben Zaken S, Factor S, Abadi M, Shichman I, Morgan S, Gold A, Snir N, Warschawski Y. Radiological Comparison of Canal Fill between Collared and Non-Collared Femoral Stems: A Two-Year Follow-Up after Total Hip Arthroplasty. Journal of Imaging. 2024; 10(5):99. https://doi.org/10.3390/jimaging10050099
Chicago/Turabian StyleAshkenazi, Itay, Amit Benady, Shlomi Ben Zaken, Shai Factor, Mohamed Abadi, Ittai Shichman, Samuel Morgan, Aviram Gold, Nimrod Snir, and Yaniv Warschawski. 2024. "Radiological Comparison of Canal Fill between Collared and Non-Collared Femoral Stems: A Two-Year Follow-Up after Total Hip Arthroplasty" Journal of Imaging 10, no. 5: 99. https://doi.org/10.3390/jimaging10050099
APA StyleAshkenazi, I., Benady, A., Ben Zaken, S., Factor, S., Abadi, M., Shichman, I., Morgan, S., Gold, A., Snir, N., & Warschawski, Y. (2024). Radiological Comparison of Canal Fill between Collared and Non-Collared Femoral Stems: A Two-Year Follow-Up after Total Hip Arthroplasty. Journal of Imaging, 10(5), 99. https://doi.org/10.3390/jimaging10050099








