Transformative Effect of COVID-19 Pandemic on Magnetic Resonance Imaging Services in One Tertiary Cardiovascular Center
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Characteristics
2.2. MRI Data Analysis
2.3. Sample Size Calculation
2.4. Statistical Processing of Data
2.5. Study Support
3. Results
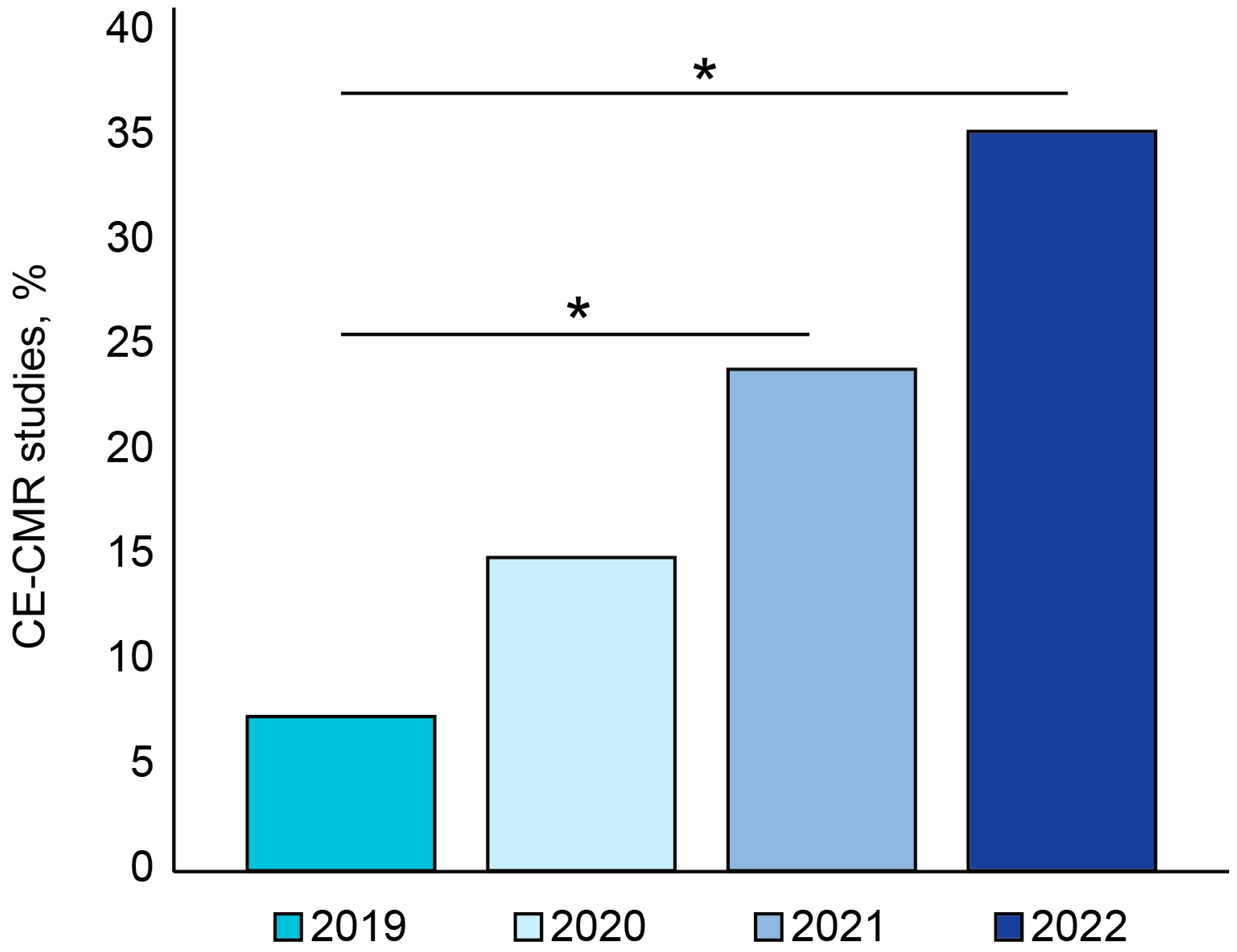
3.1. Temporal Trend in CE-CMR Procedures
3.2. Sex-Related Differences in CE-CMR-Detected Cardiac Pathologies during COVID-19 Pandemic
3.3. Age-Related Distribution of Patients Who Underwent CE-CMR Study during COVID-19 Pandemic
3.4. Year-by-Year Distribution of CE-CMR-Detected Cardiac Pathologies during COVID-19 Pandemic
3.5. CE-CMR-Detected Non-Coronarogenic Myocardial Fibrosis during COVID-19 Pandemic
3.6. Temporal Trends in CE-CMR Administrations and COVID-19 Occurrence during the Pandemic
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kelle, S.; Bucciarelli-Ducci, C.; Judd, R.M.; Kwong, R.Y.; Simonetti, O.; Plein, S.; Raimondi, F.; Weinsaft, J.W.; Wong, T.C.; Carr, J. Society for Cardiovascular Magnetic Resonance (SCMR) recommended CMR protocols for scanning patients with active or convalescent phase COVID-19 infection. J. Cardiovasc. Magn. Reson. 2020, 22, 61. [Google Scholar] [CrossRef]
- Higgins, V.; Sohaei, D.; Diamandis, E.P.; Prassas, I. COVID-19: From an acute to chronic disease? Potential long-term health consequences. Crit. Rev. Clin. Lab. Sci. 2020, 58, 297–310. [Google Scholar] [CrossRef]
- Ussov, W.Y.; Nudnov, N.V.; Ignatenko, G.A.; Fisenko, A.Y.; Gulyaev, V.M.; Maritskii, S.V.; Kalyuzhin, V.V.; Lukyanenok, P.I. Evaluation of lung damage in pneumonia, from chest magnetic resonance imaging, in primary diagnosis and in the follow-up of treatment. Med. Vis. 2020, 24, 63–77. [Google Scholar] [CrossRef]
- Ussov, W.Y.; Nudnov, N.V.; Ignatenko, G.A.; Gulyaev, V.M.; Pervak, M.B.; Shelkovnikova, T.A.; Dubovaya, A.V.; Bergen, T.A. Primary and prospective imaging of the chest using magnetic resonance imaging in patients with viral lung damage in COVID-19. Med. Vis. 2020, 24, 11–26. [Google Scholar] [CrossRef]
- Todorovic, V. Mild SARS-CoV-2 infection leaves long-lasting effects on cardiovascular health. Nat. Cardiovasc. Res. 2022, 1, 870. [Google Scholar] [CrossRef]
- Ramadan, M.S.; Bertolino, L.; Zampino, R.; Durante-Mangoni, E.; Iossa, D.; Ursi, M.P.; D’Amico, F.; Karruli, A.; Andini, R.; Bernardo, M.; et al. Cardiac sequelae after coronavirus disease 2019 recovery: A systematic review. Clin. Microbiol. Infect. 2021, 27, 1250–1261. [Google Scholar] [CrossRef]
- Ansheles, A.A.; Sergienko, V.B.; Sinitsyn, E.V.; Vakhromeeva, M.N.; Kokov, A.N.; Zavadovsky, K.V.; Ryzhkova, D.V.; Karalkin, A.V.; Shurupova, I.V.; Pospelov, V.A.; et al. Analysis of the restoration of cardiology diagnostics scope in the Russian Federation during the COVID-19 pandemic: Results of the Russian segment of the INCAPS COVID 2 study under the auspices of the International Atomic Energy Agency. Russ. J. Cardiol. 2022, 27, 5170. (In Russian) [Google Scholar] [CrossRef]
- Sudakov, D.V.; Sudakov, O.V.; Shevtsov, A.N.; Belov, E.V.; Androsova, O.A. Analysis of complications among patients after previous new coronoviral COVID-19 infection. Syst. Anal. Manag. Biomed. Syst. 2021, 20, 15–23. (In Russian) [Google Scholar] [CrossRef]
- Italia, L.; Tomasoni, D.; Bisegna, S.; Pancaldi, E.; Stretti, L.; Adamo, M.; Metra, M. COVID-19 and Heart Failure: From Epidemiology During the Pandemic to Myocardial Injury, Myocarditis, and Heart Failure Sequelae. Front. Cardiovasc. Med. 2021, 8, 713560. [Google Scholar] [CrossRef] [PubMed]
- Fisun, A.Y.; Lobzin, Y.V.; Cherkashin, D.V.; Tyrenko, V.V.; Tkachenko, K.N.; Kachnov, V.A.; Kutelev, G.G.; Rudchenko, I.V.; Sobolev, A.D. Mechanisms of Damage to the Cardiovascular System in COVID-19. Ann. Russ. Acad. Med. Sci. 2021, 76, 287–297. [Google Scholar] [CrossRef]
- Kobelev, E.; Bergen, T.A.; Tarkova, A.R.; Vasiltseva, O.Y.; Kamenskaya, O.V.; Usov, V.Y.; Chernyavsky, A.M. COVID-19 as a cause of chronic pulmonary hypertension: Pathophysiological rationale and potential of instrumental investigations. Cardiovasc. Ther. Prev. 2021, 20, 2844. (In Russian) [Google Scholar] [CrossRef]
- Shelkovnikova, T.A.; Pushnikova, E.Y.; Baev, A.E.; Ryabov, V.V.; Ussov, W.Y. Magnetic resonance syndromes of myocardial damage in patients after new coronavirus infection (COVID-19)—Two typical clinical cases. Sib. J. Clin. Exp. Med. 2022, 37, 135–141. (In Russian) [Google Scholar] [CrossRef]
- Ussov, W.Y.; Ignatenko, G.A.; Nudnov, N.V.; Bergen, T.A.; Gulyaev, V.M.; Pervak, M.B.; Yaroshevsky, S.P.; Dubovaya, A.V.; Karmazanovsky, G.G. Comprehensive MRI of the Chest and Brain in the Diagnosis of Injury to Thoracic Organs, Myocardium, and Brain in COVID-19. The University Clinic 2021. Suppl. I, pp. 144–145. Available online: https://dnmu.ru/wp-content/uploads/2021/02/materConfCovid_010221.pdf (accessed on 29 April 2023). (In Russian).
- Baig, A.M. Chronic COVID syndrome: Need for an appropriate medical terminology for long-COVID and COVID long-haulers. J. Med. Virol. 2020, 93, 2555–2556. [Google Scholar] [CrossRef]
- Baden, L.R.; El Sahly, H.M.; Essink, B.; Kotloff, K.; Frey, S.; Novak, R.; Diemert, D.; Spector, S.A.; Rouphael, N.; Creech, C.B.; et al. Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine. N. Engl. J. Med. 2021, 384, 403–416. [Google Scholar] [CrossRef] [PubMed]
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Pérez Marc, G.; Moreira, E.D.; Zerbini, C.; et al. Safety and Efficacy of the BNT162b2 mRNA COVID-19 vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef] [PubMed]
- Heidenreich, P.A.; Bozkurt, B.; Aguilar, D.; Allen, L.A.; Byun, J.J.; Colvin, M.M.; Deswal, A.; Drazner, M.H.; Dunlay, S.M.; Evers, L.R.; et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2022, 79, e263–e421. [Google Scholar] [CrossRef] [PubMed]
- Petersen, S.E.; Friedrich, M.G.; Leiner, T.; Elias, M.D.; Ferreira, V.M.; Fenski, M.; Flamm, S.D.; Fogel, M.; Garg, R.; Halushka, M.K.; et al. Cardiovascular Magnetic Resonance for Patients with COVID-19. JACC Cardiovasc. Imaging 2021, 15, 685–699. [Google Scholar] [CrossRef]
- Ussov, W.Y.; Mochula, O.V.; Ryumshina, N.I.; Shelkovnikova, T.A.; Sukhareva, A.E.; Maksimova, A.S.; Velichko, O.B.; Vaizov, V.K.; Ovchinnikov, P.P.; Zavadovsky, K.V.; et al. Certificate of the State Registration for Database No. 2022622669 Russian Federation. Register of Magnetic Resonance Imaging Studies: No. 2022622644: Submitted 24.10.2022: Published 28.10.2022; Applicant: Tomsk NRMC.—EDN XWWUWA. Available online: https://www.elibrary.ru/download/elibrary_49774441_46558053.PDF (accessed on 29 April 2023).
- De Pelsemaeker, M.-C.; Guiot, Y.; Vanderveken, J.; Galant, C.; Van Bockstal, M.R. The Impact of the COVID-19 Pandemic and the Associated Belgian Governmental Measures on Cancer Screening, Surgical Pathology and Cytopathology. Pathobiology 2021, 88, 46–55. [Google Scholar] [CrossRef]
- Keizman, E.; Ram, E.; Kachel, E.; Sternik, L.; Raanani, E. The impact of COVID-19 pandemic on cardiac surgery in Israel. J. Cardiothorac. Surg. 2020, 15, 294. [Google Scholar] [CrossRef]
- Saban, M.; Reznik, A.; Shachar, T.; Wilf-Miron, R.; Sivan-Hoffmann, R. The effect of the COVID-19 pandemic on ED referrals and care for stroke patients: A four-year comparative study. J. Crit. Care 2020, 62, 230–234. [Google Scholar] [CrossRef]
- Hartnett, K.P.; Kite-Powell, A.; DeVies, J.; Coletta, M.A.; Boehmer, T.K.; Adjemian, J.; Gundlapalli, A.V. National Syndromic Surveillance Program Community of Practice Impact of the COVID-19 Pandemic on Emergency Department Visits—United States, January 1, 2019–May 30, 2020. MMWR. Morb. Mortal. Wkly. Rep. 2020, 69, 699–704. [Google Scholar] [CrossRef] [PubMed]
- Anfinogenova, N.D.; Trubacheva, I.A.; Popov, S.V.; Efimova, E.V.; Ussov, W.Y. Trends and concerns of potentially inappropriate medication use in patients with cardiovascular diseases. Expert Opin. Drug Saf. 2021, 20, 1191–1206. [Google Scholar] [CrossRef] [PubMed]
- Cattaneo, D.; Pasina, L.; Maggioni, A.P.; Oreni, L.; Conti, F.; Pezzati, L.; Casalini, G.; Bonazzetti, C.; Morena, V.; Ridolfo, A.; et al. Drug–Drug Interactions and Prescription Appropriateness at Hospital Discharge: Experience with COVID-19 Patients. Drugs Aging 2021, 38, 341–346. [Google Scholar] [CrossRef] [PubMed]
- Vakili, S.; Savardashtaki, A.; Jamalnia, S.; Tabrizi, R.; Nematollahi, M.H.; Jafarinia, M.; Akbari, H. Laboratory Findings of COVID-19 Infection are Conflicting in Different Age Groups and Pregnant Women: A Literature Review. Arch. Med. Res. 2020, 51, 603–607. [Google Scholar] [CrossRef]
- Friedrich, M.G.; Sechtem, U.; Schulz-Menger, J.; Holmvang, G.; Alakija, P.; Cooper, L.T.; White, J.A.; Abdel-Aty, H.; Gutberlet, M.; Prasad, S.; et al. Cardiovascular Magnetic Resonance in Myocarditis: A JACC White Paper. J. Am. Coll. Cardiol. 2009, 53, 1475–1487. [Google Scholar] [CrossRef]
- Lagan, J.; Schmitt, M.; Miller, C.A. Clinical applications of multi-parametric CMR in myocarditis and systemic inflammatory diseases. Int. J. Cardiovasc. Imaging 2017, 34, 35–54. [Google Scholar] [CrossRef]
- Liguori, C.; Farina, D.; Vaccher, F.; Ferrandino, G.; Bellini, D.; Carbone, I. Myocarditis: Imaging up to date. La Radiol. Med. 2020, 125, 1124–1134. [Google Scholar] [CrossRef]
- Dixit, N.M.; Churchill, A.; Nsair, A.; Hsu, J.J. Post-Acute COVID-19 Syndrome and the cardiovascular system: What is known? Am. Heart J. Plus: Cardiol. Res. Pract. 2021, 5, 100025. [Google Scholar] [CrossRef]
- Awortwe, C.; Cascorbi, I. Meta-analysis on outcome-worsening comorbidities of COVID-19 and related potential drug-drug interactions. Pharmacol. Res. 2020, 161, 105250. [Google Scholar] [CrossRef]
- Ignatenko, G.A.; Pervak, M.B.; Usov, V.Y.; Dubovaya, A.V.; Gerasimenko, V.V. Computed-tomographic evaluation of the lung changes in COVID-19 after 4–6 months: Comparison with the results of the study in the acute period of the disease and clinical data. Arch. Clin. Exp. Med. 2022, 31, 112–118. Available online: https://portal.dnmu.ru/fileadmin/EDITDATA/bibl/AKEHM_2022_No2.pdf (accessed on 29 April 2023).
- Wojtowicz, D.; Dorniak, K.; Ławrynowicz, M.; Wąż, P.; Fijałkowska, J.; Kulawiak-Gałąska, D.; Rejszel-Baranowska, J.; Knut, R.; Haberka, M.; Szurowska, E.; et al. Cardiac Magnetic Resonance Findings in Patients Recovered from COVID-19 Pneumonia and Presenting with Persistent Cardiac Symptoms: The TRICITY-CMR Trial. Biology 2022, 11, 1848. [Google Scholar] [CrossRef]
- Kersten, J.; Baumhardt, M.; Hartveg, P.; Hoyo, L.; Hüll, E.; Imhof, A.; Kropf-Sanchen, C.; Nita, N.; Mörike, J.; Rattka, M.; et al. Long COVID: Distinction between Organ Damage and Deconditioning. J. Clin. Med. 2021, 10, 3782. [Google Scholar] [CrossRef]
- Camastra, G.; Arcari, L.; Ciolina, F.; Danti, M.; Ansalone, G.; Cacciotti, L.; Sbarbati, S. Characterization of COVID-19-Related Lung Involvement in Patients Undergoing Magnetic Resonance T1 and T2 Mapping Imaging: A Pilot Study. J. Imaging 2022, 8, 314. [Google Scholar] [CrossRef] [PubMed]
- Drakos, S.; Chatzantonis, G.; Bietenbeck, M.; Evers, G.; Schulze, A.B.; Mohr, M.; Fonfara, H.; Meier, C.; Yilmaz, A. A cardiovascular magnetic resonance imaging-based pilot study to assess coronary microvascular disease in COVID-19 patients. Sci. Rep. 2021, 11, 15667. [Google Scholar] [CrossRef] [PubMed]
- Adeboye, A.; Alkhatib, D.; Butt, A.; Yedlapati, N.; Garg, N. A Review of the Role of Imaging Modalities in the Evaluation of Viral Myocarditis with a Special Focus on COVID-19-Related Myocarditis. Diagnostics 2022, 12, 549. [Google Scholar] [CrossRef]
- Mester, A.; Benedek, I.; Rat, N.; Tolescu, C.; Polexa, S.A.; Benedek, T. Imaging Cardiovascular Inflammation in the COVID-19 Era. Diagnostics 2021, 11, 1114. [Google Scholar] [CrossRef] [PubMed]
- Sanghvi, S.K.; Schwarzman, L.S.; Nazir, N.T. Cardiac MRI and Myocardial Injury in COVID-19: Diagnosis, Risk Stratification and Prognosis. Diagnostics 2021, 11, 130. [Google Scholar] [CrossRef]
- Das, B.B. SARS-CoV-2 Myocarditis in a High School Athlete after COVID-19 and Its Implications for Clearance for Sports. Children 2021, 8, 427. [Google Scholar] [CrossRef]
- Artico, J.; Shiwani, H.; Moon, J.C.; Gorecka, M.; McCann, G.P.; Roditi, G.; Morrow, A.; Mangion, K.; Lukaschuk, E.; Shanmuganathan, M.; et al. Myocardial Involvement After Hospitalization for COVID-19 Complicated by Troponin Elevation: A Prospective, Multicenter, Observational Study. Circulation 2023, 147, 364–374. [Google Scholar] [CrossRef]
- Hassan, O.K.A.; Sheng, C.C.; Wang, T.K.M.; Cremer, P.C. SARS-CoV-2 Myocarditis: Insights Into Incidence, Prognosis, and Therapeutic Implications. Curr. Cardiol. Rep. 2021, 23, 129. [Google Scholar] [CrossRef]
- Seidel, F.; Kuehne, T.; Kelle, S.; Doeblin, P.; Zieschang, V.; Tschoepe, C.; Al-Wakeel-Marquard, N.; Nordmeyer, S. Cardiovascular magnetic resonance findings in non-hospitalized paediatric patients after recovery from COVID-19. ESC Heart Fail. 2021, 8, 5583–5588. [Google Scholar] [CrossRef] [PubMed]
- Hubacek, J. Effects of Selected Inherited Factors on Susceptibility to SARS-CoV-2 Infection and COVID-19 Progression. Physiol. Res. 2021, 70 (Suppl. S2), S125–S134. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Liu, B.; Zhang, S.; Huang, N.; Zhao, T.; Lu, Q.; Cui, F. Differences in incidence and fatality of COVID-19 by SARS-CoV-2 Omicron variant versus Delta variant in relation to vaccine coverage: A world-wide review. J. Med. Virol. 2022, 95, e28118. [Google Scholar] [CrossRef] [PubMed]






Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shelkovnikova, T.A.; Maksimova, A.S.; Ryumshina, N.I.; Mochula, O.V.; Vaizov, V.K.; Ussov, W.Y.; Anfinogenova, N.D. Transformative Effect of COVID-19 Pandemic on Magnetic Resonance Imaging Services in One Tertiary Cardiovascular Center. J. Imaging 2023, 9, 108. https://doi.org/10.3390/jimaging9060108
Shelkovnikova TA, Maksimova AS, Ryumshina NI, Mochula OV, Vaizov VK, Ussov WY, Anfinogenova ND. Transformative Effect of COVID-19 Pandemic on Magnetic Resonance Imaging Services in One Tertiary Cardiovascular Center. Journal of Imaging. 2023; 9(6):108. https://doi.org/10.3390/jimaging9060108
Chicago/Turabian StyleShelkovnikova, Tatiana A., Aleksandra S. Maksimova, Nadezhda I. Ryumshina, Olga V. Mochula, Valery K. Vaizov, Wladimir Y. Ussov, and Nina D. Anfinogenova. 2023. "Transformative Effect of COVID-19 Pandemic on Magnetic Resonance Imaging Services in One Tertiary Cardiovascular Center" Journal of Imaging 9, no. 6: 108. https://doi.org/10.3390/jimaging9060108
APA StyleShelkovnikova, T. A., Maksimova, A. S., Ryumshina, N. I., Mochula, O. V., Vaizov, V. K., Ussov, W. Y., & Anfinogenova, N. D. (2023). Transformative Effect of COVID-19 Pandemic on Magnetic Resonance Imaging Services in One Tertiary Cardiovascular Center. Journal of Imaging, 9(6), 108. https://doi.org/10.3390/jimaging9060108






