The Relationship between the Contouring Time of the Metal Artifacts Area and Metal Artifacts in Head and Neck Radiotherapy
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Radiotherapy Treatment Planning Computed Tomography Data
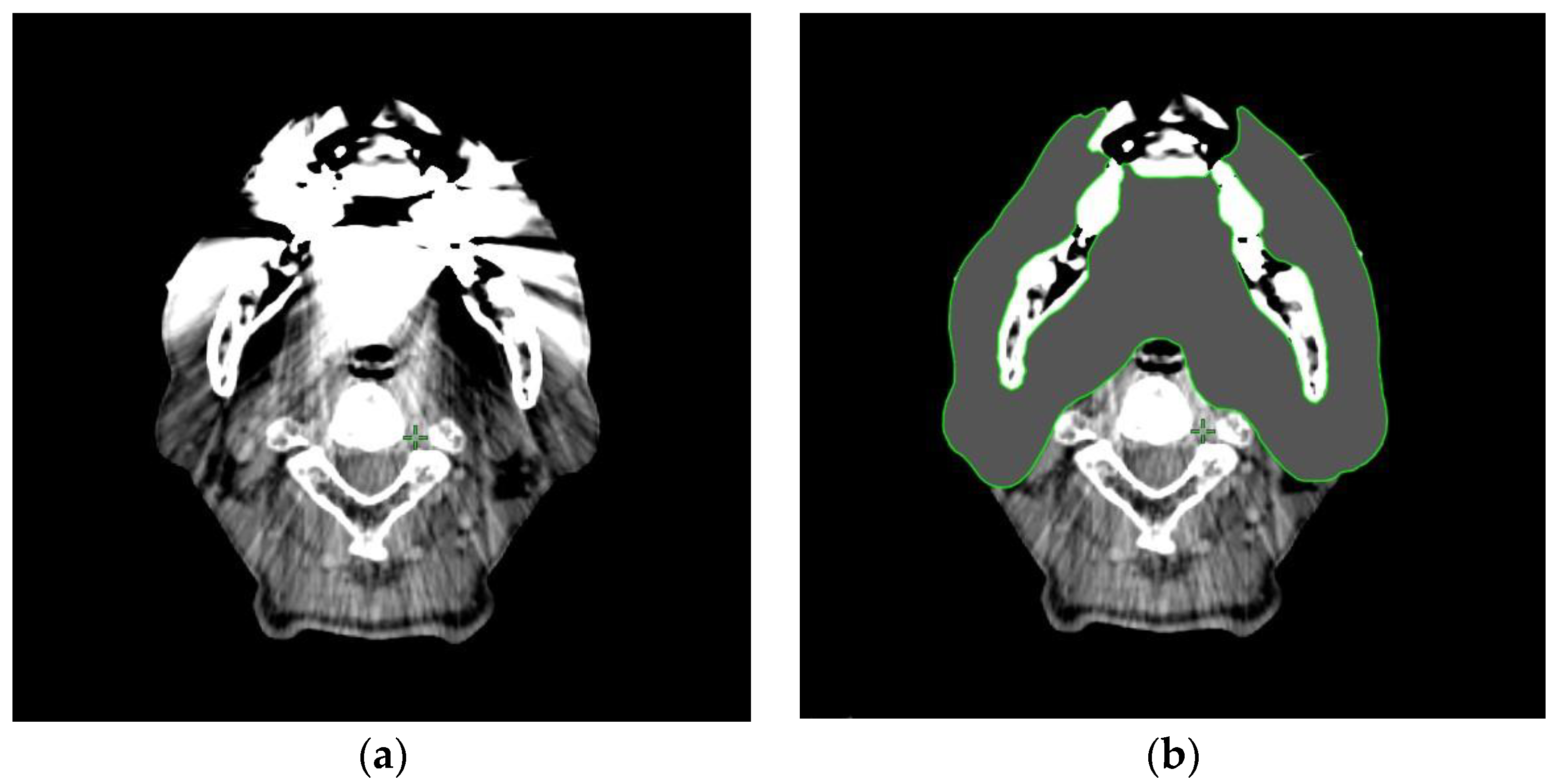
2.3. Contouring of the Dental Metal Artifacts Area
2.4. Evaluation
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- O’Daniel, J.; Rosenthal, D.; Garden, A.; Barker, J.L.; Ahamad, A.; Ang, K.K.; Asper, J.A.; Blanco, A.I.; de Crevoisier, R.; Holsinger, F.C.; et al. The effect of dental artifacts, contrast media, and experience on interobserver contouring variations in head and neck anatomy. Am. J. Clin. Oncol. 2007, 30, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Tomé, W.A.; Bal, M.; McNutt, T.R.; Spies, L. The impact of dental metal artefacts on head and neck IMRT dose distributions. Radiother. Oncol. 2006, 79, 198–202. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.Y.; Followill, D.S.; Howell, R.M.; Liu, X.; Mirkovic, D.; Stingo, F.C.; Kry, S.F. Approaches to reducing photon dose calculation errors near metal implants. Med. Phys. 2016, 43, 5117–5130. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kamomae, T.; Itoh, Y.; Okudaira, K.; Nakaya, T.; Tomida, M.; Miyake, Y.; Oguchi, H.; Shiinoki, T.; Kawamura, M.; Yamamoto, N.; et al. Dosimetric impact of dental metallic crown on intensity-modulated radiotherapy and volumetric-modulated arc therapy for head and neck cancer. J. Appl. Clin. Med. Phys. 2016, 17, 234–245. [Google Scholar] [CrossRef] [PubMed]
- Rousselle, A.; Amelot, A.; Thariat, J.; Jacob, J.; Mercy, G.; De Marzi, L.; Feuvret, L. Metallic implants and CT artifacts in the CTV area: Where are we in 2020? Cancer/Radiothérapie 2020, 24, 658–666. [Google Scholar] [CrossRef] [PubMed]
- Katsura, K.; Soga, Y.; Zenda, S.; Nishi, H.; Soga, M.; Usubuchi, M.; Mitsunaga, S.; Tomizuka, K.; Konishi, T.; Yatsuoka, W.; et al. A cost-minimization analysis of measures against metallic dental restorations for head and neck radiotherapy. J. Radiat. Res. 2021, 62, 374–378. [Google Scholar] [CrossRef] [PubMed]
- Koo, T.K.; Li, M.Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Budach, W.; Bölke, E.; Fietkau, R.; Buchali, A.; Wendt, T.G.; Popp, W.; Matuschek, C.; Sack, H. Evaluation of time, attendance of medical staff, and resources during radiotherapy for head and neck cancer patients: The DEGRO-QUIRO trial. Strahlenther. Onkol. 2011, 187, 449–460. [Google Scholar] [CrossRef] [PubMed]
- Fung, N.T.C.; Hung, W.M.; Sze, C.K.; Lee, M.C.H.; Ng, W.T. Automatic segmentation for adaptive planning in nasopharyngeal carcinoma IMRT: Time, geometrical, and dosimetric analysis. Med. Dosim. 2020, 45, 60–65. [Google Scholar] [CrossRef] [PubMed]
- Teguh, D.N.; Levendag, P.C.; Voet, P.W.; Al-Mamgani, A.; Han, X.; Wolf, T.K.; Hibbard, L.S.; Nowak, P.; Akhiat, H.; Dirkx, M.L.; et al. Clinical validation of atlas-based auto-segmentation of multiple target volumes and normal tissue (swallowing/mastication) structures in the head and neck. Int. J. Radiat. Oncol. Biol. Phys. 2011, 81, 950–957. [Google Scholar] [CrossRef] [PubMed]
- Patel, V.; Patel, D.; Browning, T.; Patel, S.; McGurk, M.; Sassoon, I.; Urbano, T.G.; Fenlon, M. Presenting pre-radiotherapy dental status of head and neck cancer patients in the novel radiation era. Br. Dent. J. 2020, 228, 435–440. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.; Liu, T.; Jennelle, R.L.; Ryu, J.K.; Vijayakumar, S.; Purdy, J.A.; Chen, A.M. Utility of megavoltage Fan-beam CT for treatment planning in a head-and-neck cancer patient with extensive dental fillings undergoing helical tomotherapy. Med. Dosim. 2010, 35, 108–114. [Google Scholar] [CrossRef] [PubMed]
- Bamberg, F.; Dierks, A.; Nikolaou, K.; Reiser, M.F.; Becker, C.R.; Johnson, T.R. Metal artefact reduction by dual energy computed tomography using mono-energetic extrapolation. Eur. Radiol. 2011, 21, 1424–1429. [Google Scholar] [CrossRef]
- Pettersson, E.; Bäck, A.; Björk-Eriksson, T.; Lindencrona, U.; Petruson, K.; Thilander-Klang, A. Structure delineation in the presence of metal–a comparative phantom study using single and dual-energy computed tomography with and without metal artefact reduction. Phys. Imaging Radiat. Oncol. 2019, 9, 43–49. [Google Scholar] [CrossRef] [Green Version]
- Kwon, H.; Kim, K.S.; Chun, Y.M.; Wu, H.-G.; Carlson, J.N.K.; Park, J.M.; Kim, J.-I. Evaluation of a commercial orthopaedic metal artefact reduction tool in radiation therapy of patients with head and neck cancer. Br. J. Radiol. 2015, 88, 13–22. [Google Scholar] [CrossRef] [Green Version]
- Bär, E.; Schwahofer, A.; Kuchenbecker, S.; Häring, P. Improving radiotherapy planning in patients with metallic implants using the iterative metal artifact reduction (iMAR) algorithm. Biomed. Phys. Eng. Exp. 2015, 1, 025206. [Google Scholar] [CrossRef]
- Hansen, C.R.; Christiansen, R.; Lorenzen, E.L.; Bertelsen, A.S.; Asmussen, J.T.; Gyldenkerne, N.; Eriksen, J.G.; Johansen, J.; Brink, C. Contouring and dose calculation in head and neck cancer radiotherapy after reduction of metal artifacts in CT images. Acta Oncol. 2017, 56, 874–878. [Google Scholar] [CrossRef] [PubMed]
- Sillanpaa, J.; Lovelock, M.; Mueller, B. The effects of the orthopedic metal artifact reduction (O–MAR) algorithm on contouring and dosimetry of head and neck radiotherapy patients. Med. Dosim. 2020, 45, 92–96. [Google Scholar] [CrossRef] [PubMed]
- Van Dijk, L.V.; Van den Bosch, L.; Aljabar, P.; Peressutti, D.; Both, S.; Steenbakkers, R.J.; Langendijk, J.A.; Gooding, M.J.; Brouwer, C.L. Improving automatic delineation for head and neck organs at risk by deep learning contouring. Radiother. Oncol. 2020, 142, 115–123. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | N = 9 |
|---|---|
| Age, range (median) | 55–76 years (66) |
| Gender | |
| Male Female | 9 0 |
| Primary tumor site | |
| Nasopharynx Oropharynx Larynx Maxillary sinus | 2 4 2 1 |
| Tumor classification | |
| T1 T2 T3 T4a T4b | 3 2 2 1 1 |
| Node classification | |
| N0 N1 N2b N2c | 1 4 3 1 |
| Cancer stage | |
| I II III IVA IVB | 1 2 2 3 1 |
| Number of CT images | |
| Oral cavity, range (median) MAs, range (median) | 21–26 images (24) 4–18 images (11) |
| Volume of extracted MAs, range (median) | 16.8–245.4 cc (105.3) |
| Contouring time of MAs area (median) | 6.4–72.7 min (19.3) |
| Severities of MAs | ||||
|---|---|---|---|---|
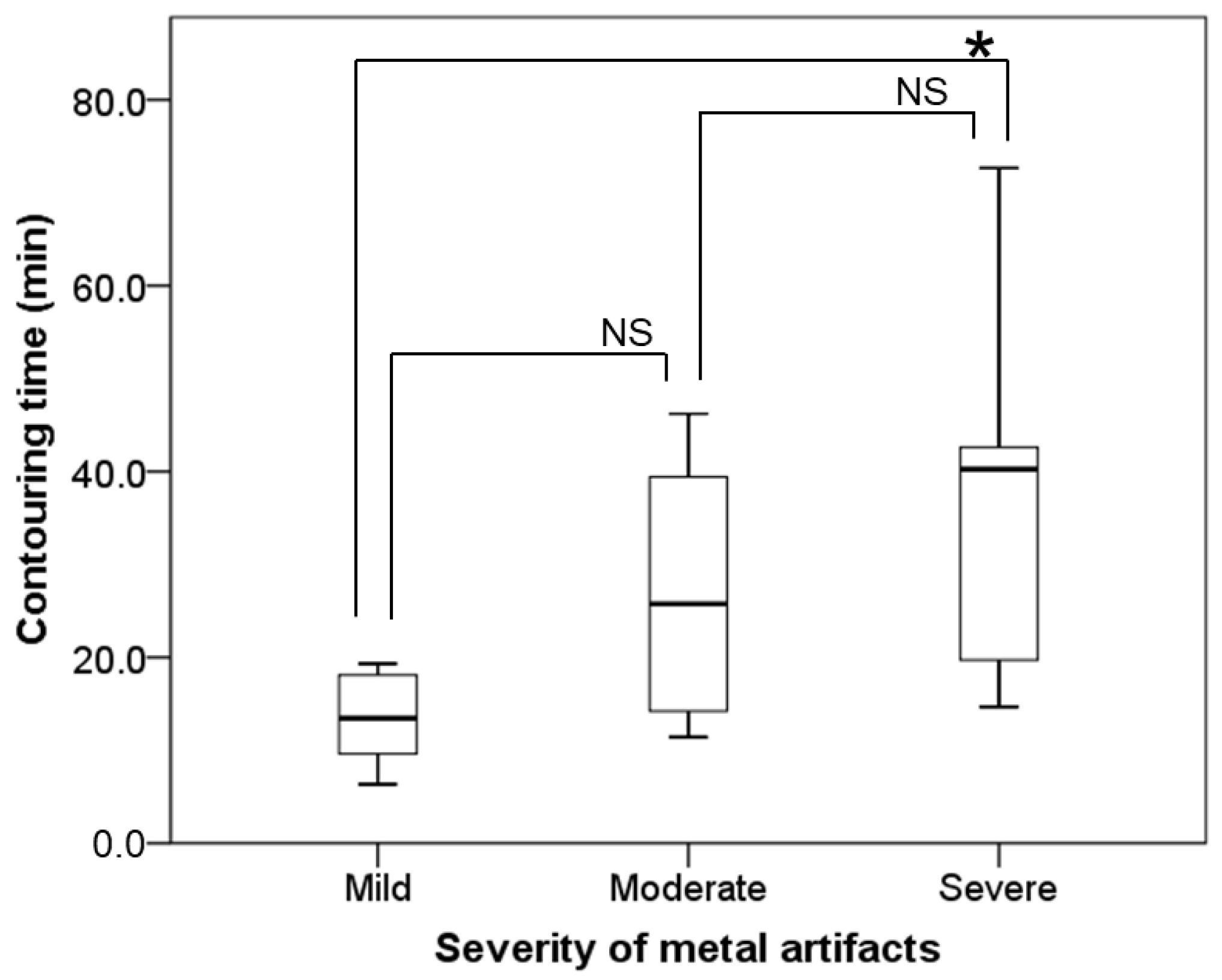
| Mild (<25%) Median (Range) | Moderate (25–75%) Median (Range) | Severe (>75%) Median (Range) | p | |
| Volume of extracted MAs | 49.2 cc (16.8–72.4) | 108.8 cc (53.9–142.7) | 209.8 cc (98.3–245.4) | <0.001 |
| Contouring time of MAs area | 16.1 min. (6.4–32.7) | 25.8 min. (11.4–46.2) | 40.3 min. (14.7–72.7) | <0.014 |
| Contouring Time of MAs Area | p | |
|---|---|---|
| Volume of extracted MAs | r = 0.535 | 0.004 |
| Number of CT slices containing MAs | r = 0.596 | <0.001 |
| Volume of Extracted MAs | Contouring Times of MAs Area | |||||
|---|---|---|---|---|---|---|
| Observer (Clinical Experience) | Volume Median (Range) | ICC | 95% CI | Contouring Time Median (Range) | ICC | 95% CI |
| A (1 year) | 96.9 cc (19.2–245.4) | 0.934 | 0.78–0.98 | 40.4 min. (16.1–53.2) | 0.312 | −0.01–0.72 |
| B (4 years) | 112.9 cc (22.9–243.6) | 14.1 min. (6.4–25.4) | ||||
| C (12 years) | 127.6 cc (31.2–283.5) | 18.5 min. (9.1–90.9) | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Katsura, K.; Tanabe, S.; Nakano, H.; Sakai, M.; Ohta, A.; Kaidu, M.; Soga, M.; Kobayashi, T.; Takamura, M.; Hayashi, T. The Relationship between the Contouring Time of the Metal Artifacts Area and Metal Artifacts in Head and Neck Radiotherapy. Tomography 2023, 9, 98-104. https://doi.org/10.3390/tomography9010009
Katsura K, Tanabe S, Nakano H, Sakai M, Ohta A, Kaidu M, Soga M, Kobayashi T, Takamura M, Hayashi T. The Relationship between the Contouring Time of the Metal Artifacts Area and Metal Artifacts in Head and Neck Radiotherapy. Tomography. 2023; 9(1):98-104. https://doi.org/10.3390/tomography9010009
Chicago/Turabian StyleKatsura, Kouji, Satoshi Tanabe, Hisashi Nakano, Madoka Sakai, Atsushi Ohta, Motoki Kaidu, Marie Soga, Taichi Kobayashi, Masaki Takamura, and Takafumi Hayashi. 2023. "The Relationship between the Contouring Time of the Metal Artifacts Area and Metal Artifacts in Head and Neck Radiotherapy" Tomography 9, no. 1: 98-104. https://doi.org/10.3390/tomography9010009
APA StyleKatsura, K., Tanabe, S., Nakano, H., Sakai, M., Ohta, A., Kaidu, M., Soga, M., Kobayashi, T., Takamura, M., & Hayashi, T. (2023). The Relationship between the Contouring Time of the Metal Artifacts Area and Metal Artifacts in Head and Neck Radiotherapy. Tomography, 9(1), 98-104. https://doi.org/10.3390/tomography9010009





