A Novel Metabolic Risk Classification System Incorporating Body Fat, Waist Circumference, and Muscle Strength
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Study Design
2.3. Anthropometric and Body Composition Measurements
2.4. Grip Strength Measurement
2.5. Metabolic Risk Scoring System
2.6. Evaluation of the Predictive Value of a Metabolic Risk Scoring System for Metabolic Syndrome
2.7. Statical Analyses
3. Results
3.1. Anthropometric Characteristics
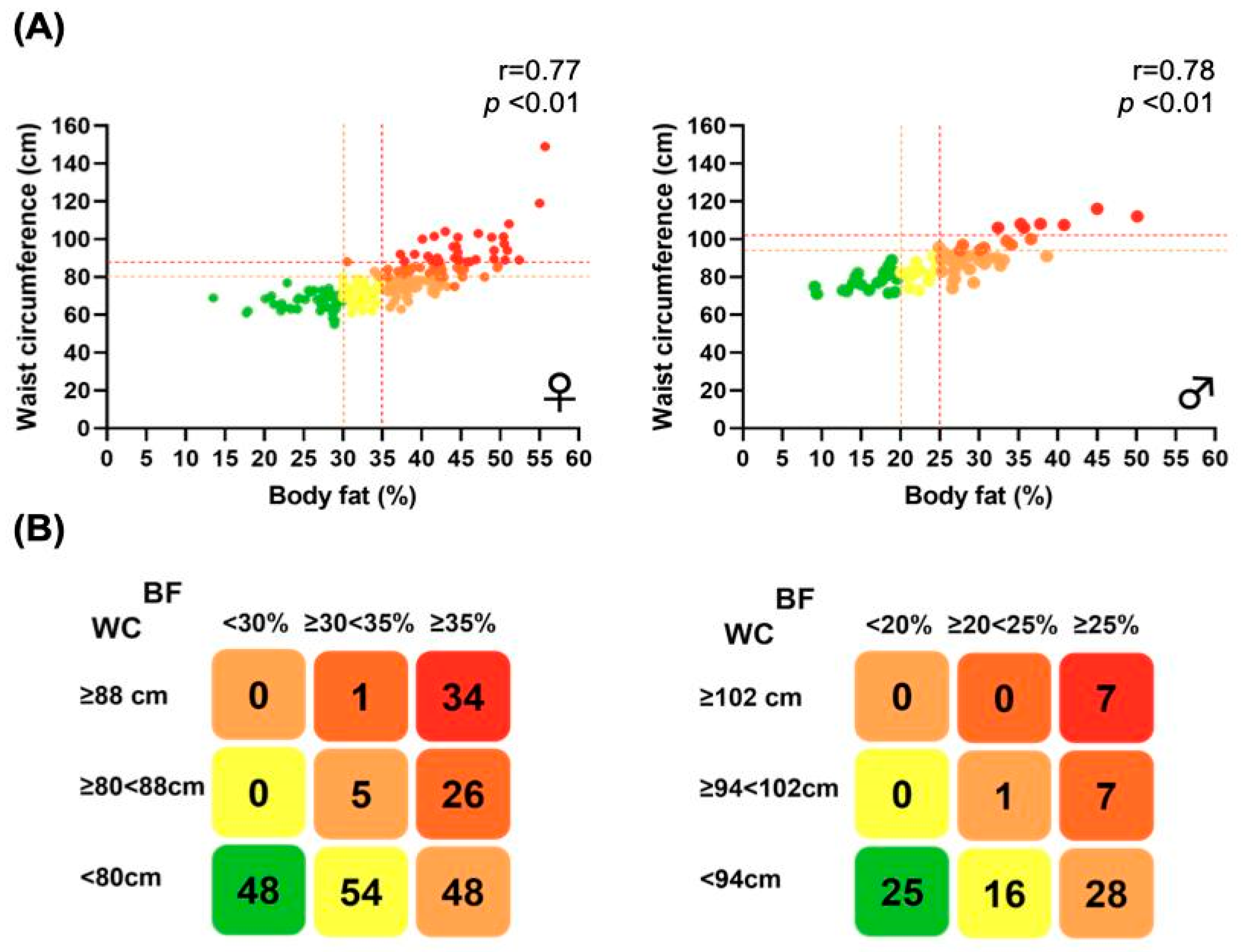
3.2. Distribution of Participants by %BF and WC
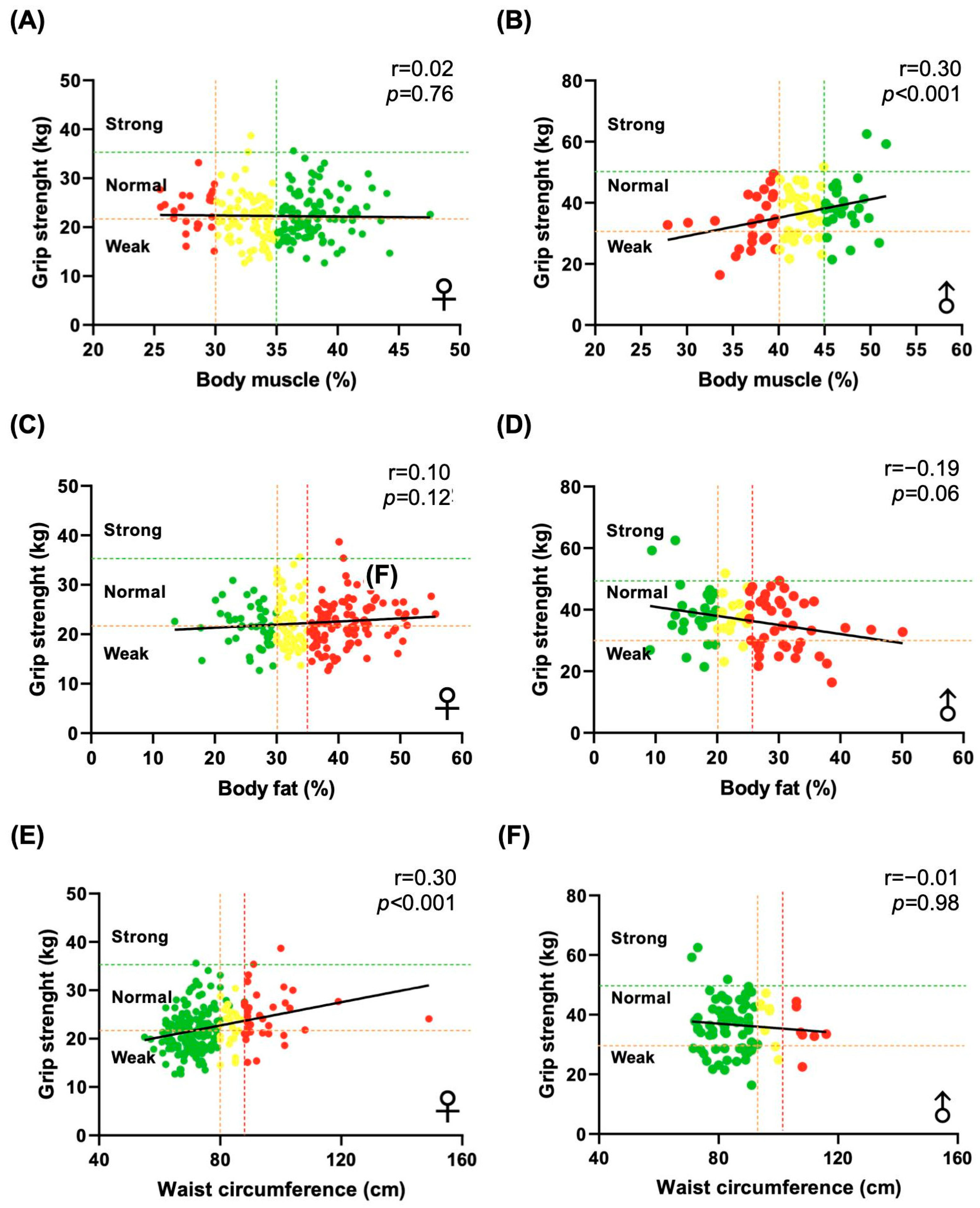
3.3. Grip Strength and Correlations with Anthropometric Measures
3.4. Grip Strength Variation Across Metabolic Risk Categories
3.5. Development and Implementation of a New Metabolic Risk Classification
3.6. Comparison of Phenotyping Systems for People with Obesity Incorporating Muscle Strength
3.7. Validation of the New Classification System in a Broader Population
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| WC | Waist circumference |
| %BF | Body fat percentage |
| GS | Grip strength |
| MetS | Metabolic syndrome |
| BMI | Body mass index |
| BIA | Bioelectrical impedance analysis |
| DXA | Dual-energy X-ray absorptiometry |
Appendix A
| Parameter | Males (n = 84) | Females (n = 216) |
|---|---|---|
| Age (years) | 20.75 ± 2.17 | 20.34 ± 1.46 |
| Weight (kg) | 76.41 ± 12.25 | 62.58 ± 14.38 |
| Height (cm) | 172 ± 7 | 159 ± 6.2 |
| Body Mass Index (kg/m2) | 25.51 ± 3.64 | 24.47 ± 5.21 |
| Body Fat (%) | 24.96 ± 7.7 | 35.43 ± 7.54 |
| Body Fat (kg) | 19.75 ± 8.90 | 22.98 ± 10.07 |
| Body muscle (%) | 42.31 ± 4.51 | 34.83 ± 3.97 |
| Body muscle (kg) | 32.02 ± 4.15 | 21.42 ± 3.47 |
| Visceral Fat | 7.94 ± 4.01 | 10.32 ± 4.78 |
| Waist Circumference (cm) | 86.34 ± 9.82 | 76.42 ± 11.51 |
| Hip Circumference (cm) | 86.34 ± 9.82 | 97.63 ± 11.05 |
| Maximum grip strength (kg) | 36.52 ± 8.61 | 22.29 ± 7.54 |
| Physical activity (%) | 78.6 | 54.6 |
| Smoking (%) | 32.1 | 32.4 |
| Alcohol use (%) | 86.9 | 85.2 |

References
- Lavie, C.J.; McAuley, P.A.; Church, T.S.; Milani, R.V.; Blair, S.N. Obesity and cardiovascular diseases: Implications regarding fitness, fatness, and severity in the obesity paradox. J. Am. Coll. Cardiol. 2014, 63, 1345–1354. [Google Scholar] [CrossRef] [PubMed]
- Janssen, I.; Katzmarzyk, P.T.; Ross, R. Waist circumference and not body mass index explains obesity-related health risk. Am. J. Clin. Nutr. 2004, 79, 379–384. [Google Scholar] [CrossRef]
- DiBonaventura, M.D.; Meincke, H.; Le Lay, A.; Fournier, J.; Bakker, E.; Ehrenreich, A. Obesity in Mexico: Prevalence, comorbidities, associations with patient outcomes, and treatment experiences. Diabetes Metab. Syndr. Obes. 2018, 11, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Rico-Martín, S.; Calderón-García, J.F.; Sánchez-Rey, P.; Franco-Antonio, C.; Martínez Alvarez, M.; Sánchez Muñoz-Torrero, J.F. Effectiveness of body roundness index in predicting metabolic syndrome: A systematic review and meta-analysis. Obes. Rev. 2020, 21, e13023. [Google Scholar] [CrossRef] [PubMed]
- Wijayatunga, N.N.; Dhurandhar, E.J. Normal weight obesity and unaddressed cardiometabolic health risk—A narrative review. Int. J. Obes. 2021, 45, 2141–2155. [Google Scholar] [CrossRef]
- Salmón-Gómez, L.; Catalán, V.; Frühbeck, G.; Gómez-Ambrosi, J. Relevance of body composition in phenotyping the obesities. Rev. Endocr. Metab. Disord. 2023, 24, 809–823. [Google Scholar] [CrossRef]
- Romero-Corral, A.; Somers, V.K.; Sierra-Johnson, J.; Thomas, R.J.; Collazo-Clavell, M.L.; Korinek, J.; Allison, T.G.; Batsis, J.A.; Sert-Kuniyoshi, F.H.; Lopez-Jimenez, F. Accuracy of body mass index in diagnosing obesity in the adult general population. Int. J. Obes. 2008, 32, 959–966. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Ambrosi, J.; Catalán, V.; Ramírez, B.; Salmón-Gómez, L.; Marugán-Pinos, R.; Rodríguez, A.; Becerril, S.; Aguas-Ayesa, M.; Yárnoz-Esquíroz, P.; Olazarán, L.; et al. Cardiometabolic risk stratification using a novel obesity phenotyping system based on body adiposity and waist circumference. Eur. J. Intern. Med. 2024, 124, 54–60. [Google Scholar] [CrossRef] [PubMed]
- Sampaio, R.A.C.; Sewo Sampaio, P.Y.; Capelo, L.P.; Uchida, M.C.; Arai, H. Editorial: Sarcopenia and frailty: The role of physical activity for better aging. Front. Public Health 2023, 11, 1303223. [Google Scholar] [CrossRef]
- Ahrens, W.; Bammann, K.; Siani, A.; Buchecker, K.; De Henauw, S.; Iacoviello, L.; Hebestreit, A.; Krogh, V.; Lissner, L.; Mårild, S.; et al. The IDEFICS cohort: Design, characteristics and participation in the baseline survey. Int. J. Obes. 2011, 35, S3–S15. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [PubMed]
- Jung, H.N.; Jung, C.H.; Hwang, Y.C. Sarcopenia in youth. Metabolism 2023, 144, 155557. [Google Scholar] [CrossRef]
- Vaishya, R.; Misra, A.; Vaish, A.; Ursino, N.; D’Ambrosi, R. Hand grip strength as a proposed new vital sign of health: A narrative review of evidences. J. Health Popul. Nutr. 2024, 43, 7. [Google Scholar] [CrossRef] [PubMed]
- Ortega, F.B.; Silventoinen, K.; Tynelius, P.; Rasmussen, F. Muscular strength in male adolescents and premature death: Cohort study of one million participants. BMJ 2012, 345, e7279. [Google Scholar] [CrossRef] [PubMed]
- Leong, D.P.; Teo, K.K.; Rangarajan, S.; Lopez-Jaramillo, P.; Avezum, A., Jr.; Orlandini, A.; Seron, P.; Ahmed, S.H.; Rosengren, A.; Kelishadi, R.; et al. Prognostic value of grip strength: Findings from the Prospective Urban Rural Epidemiology (PURE) study. Lancet 2015, 386, 266–273. [Google Scholar] [CrossRef]
- Marfell-Jones, M.; Olds, T.; Stewart, A.; Carter, L.E.L. (Eds.) ISAK Manual, International Standards for Anthropometric Assessment; International Society for the Advancement of Kinanthropometry: Brasilia, Brazil, 2012. [Google Scholar]
- Roberts, H.C.; Denison, H.J.; Martin, H.J.; Patel, H.P.; Syddall, H.; Cooper, C.; Sayer, A.A. A review of the measurement of grip strength in clinical and epidemiological studies: Towards a standardised approach. Age Ageing 2011, 40, 423–429. [Google Scholar] [CrossRef] [PubMed]
- Dodds, R.M.; Syddall, H.E.; Cooper, R.; Benzeval, M.; Deary, I.J.; Dennison, E.M.; Der, G.; Gale, C.R.; Inskip, H.M.; Jagger, C.; et al. Grip strength across the life course: Normative data from twelve British studies. PLoS ONE 2014, 9, e113637. [Google Scholar] [CrossRef]
- Bohannon, R.W. Grip strength: An indispensable biomarker for older adults. Clin. Interv. Aging 2019, 14, 1681–1691. [Google Scholar] [CrossRef] [PubMed]
- Sayer, A.A.; Kirkwood, T.B. Grip strength and mortality: A biomarker of ageing? Lancet 2015, 386, 226–227. [Google Scholar] [CrossRef] [PubMed]
- Hamer, M.; Batty, G.D.; Kivimaki, M. Sarcopenic obesity and risk of new onset depressive symptoms in older adults: English Longitudinal Study of Ageing. Int. J. Obes. 2015, 39, 1717–1720. [Google Scholar] [CrossRef] [PubMed]
- Laukkanen, J.A.; Voutilainen, A.; Kurl, S.; Araujo, C.G.S.; Jae, S.Y.; Kunutsor, S.K. Handgrip strength is inversely associated with fatal cardiovascular and all-cause mortality events. Ann. Med. 2020, 52, 109–119. [Google Scholar] [CrossRef] [PubMed]
- Stenholm, S.; Mehta, N.K.; Elo, I.T.; Heliövaara, M.; Koskinen, S.; Aromaa, A. Obesity and muscle strength as long-term determinants of all-cause mortality—A 33-year follow-up of the Mini-Finland Health Examination Survey. Int. J. Obes. 2014, 38, 1126–1132. [Google Scholar] [CrossRef] [PubMed]
- Volaklis, K.A.; Halle, M.; Meisinger, C. Muscular strength as a strong predictor of mortality: A narrative review. Eur. J. Intern. Med. 2015, 26, 303–310. [Google Scholar] [CrossRef]
- Bird, S.R.; Hawley, J.A. Update on the effects of physical activity on insulin sensitivity in humans. BMJ Open Sport Exerc. Med. 2016, 2, e000143. [Google Scholar] [CrossRef] [PubMed]
- Chow, L.S.; Gerszten, R.E.; Taylor, J.M.; Pedersen, B.K.; van Praag, H.; Trappe, S.; Febbraio, M.A.; Galis, Z.S.; Gao, Y.; Haus, J.M.; et al. Exerkines in health, resilience and disease. Nat. Rev. Endocrinol. 2022, 18, 273–289. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, B.K.; Febbraio, M.A. Muscle as an endocrine organ: Focus on muscle-derived interleukin-6. Physiol. Rev. 2008, 88, 1379–1406. [Google Scholar] [CrossRef]
- Deutz, N.E.; Bauer, J.M.; Barazzoni, R.; Biolo, G.; Boirie, Y.; Bosy-Westphal, A.; Cederholm, T.; Cruz-Jentoft, A.; Krznariç, Z.; Nair, K.S.; et al. Protein intake and exercise for optimal muscle function with aging: Recommendations from the ESPEN Expert Group. Clin. Nutr. 2014, 33, 929–936. [Google Scholar] [CrossRef] [PubMed]

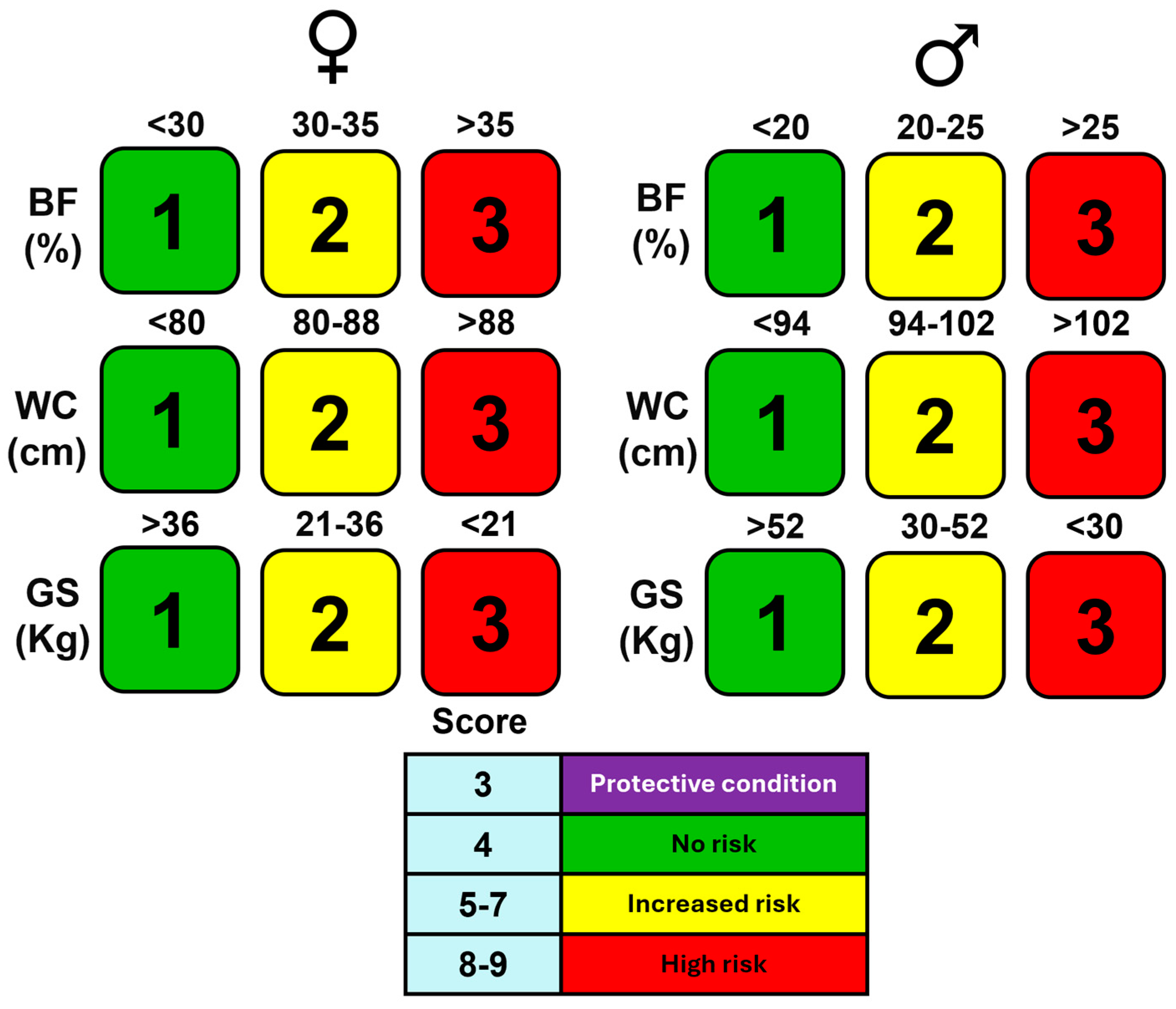


| Category | Points | %BF Cut-Offs | WC Cut-Offs (cm) | GS Cut-Offs (kg) |
|---|---|---|---|---|
| Women | 1 | <30% | <80 cm | >36 kg (strong) |
| 2 | 30–35% | 80–88 cm | 21–36 kg (moderate) | |
| 3 | ≥35% | ≥88 cm | <21 kg (weak) | |
| Men | 1 | <20% | <94 cm | >52 kg (strong) |
| 2 | 20–25% | 94–102 cm | 30–52 kg (moderate) | |
| 3 | ≥25% | ≥102 cm | <30 kg (weak) |
| Parameter | No Risk (n = 73) | Slightly Increased Risk (n = 70) | Increased Risk (n = 82) | High Risk (n = 34) | Very High Risk (n = 41) | p |
|---|---|---|---|---|---|---|
| Age (years) | ||||||
| All subjects | 20.18 ± 1.55 | 20.33 ± 1.44 | 20.79 ± 2.01 | 20.47 ± 1.86 | 20.46 ± 1.45 | 0.234 |
| Males | 20.68 ± 1.65 | 21 ± 2.17 | 20.93 ± 2.92 | 20 ± 0.81 | 20.29 ± 0.95 | 0.02 |
| Females | 19.92 ± 1.45 | 20.11 ± 1.07 | 20.7 ± 1.3 | 20.5 ± 2.04 | 20.5 ± 1.54 | 0.747 |
| Weight (kg) | ||||||
| All subjects | 57 ± 11 | 59.92 ± 10.1 | 66.24 ± 10.2 | 73.69 ± 10.68 | 88.81 ± 4.67 | <0.001 |
| Males | 68.74 ± 8.59 | 73.6 ± 6.46 | 75.4 ± 8.94 | 91.35 ± 7.13 | 99.38 ± 10.32 | <0.001 |
| Females | 50.9 ± 6.09 | 55.87 ± 7.03 | 61.2 ± 6.95 | 69.1 ± 5.23 | 86.63 ± 14.59 | <0.001 |
| Height (cm) | ||||||
| All subjects | 164.9 ± 9 | 163 ± 9.1 | 162 ± 8.7 | 162 ± 9.27 | 163 ± 7.65 | 0.566 |
| Males | 174 ± 6.2 | 174.5 ± 5.16 | 170 ± 8.04 | 177 ± 7.08 | 171 ± 6.4 | 0.301 |
| Females | 160 ± 5.95 | 159 ± 7.05 | 158 ± 6.05 | 158 ± 4.9 | 161 ± 6.7 | 0.186 |
| Body Mass Index (kg/m2) | ||||||
| All subjects | 20.7 ± 2.31 | 22.38 ± 2.08 | 24.84 ± 2.02 | 27.82 ± 2.14 | 33.24 ± 5.04 | <0.001 |
| Males | 22.6 ± 2.15 | 24.1 ± 1.41 | 25.94 ± 1.81 | 29.12 ± 1.79 | 33.64 ± 2.89 | |
| Females | 19.8 ± 1.77 | 21.8 ± 1.97 | 24.23 ± 1.88 | 27.49 ± 2.12 | 33.1 ± 5.4 | |
| Body Fat (%) | ||||||
| All subjects | 22.5 ± 5.67 | 29.88 ± 4.31 | 34.72 ± 5.26 | 39.41 ± 5.86 | 44.56 ± 5.42 | <0.001 |
| Males | 16.2 ± 3.12 | 22.48 ± 1.59 | 28.71 ± 3.12 | 31.48 ± 3.35 | 39.58 ± 6.18 | <0.001 |
| Females | 25.7 ± 3.57 | 32 ± 1.43 | 38 ± 2.59 | 41.4 ± 4.45 | 45.5 ± 4.72 | <0.001 |
| Body Fat (kg) | ||||||
| All subjects | 12.4 ± 2.76 | 17.61 ± 2.43 | 22.77 ± 3.1 | 28.78 ± 4.34 | 39.84 ± 10.09 | <0.001 |
| Males | 11.25 ± 2.86 | 16.57 ± 2.17 | 21.87 ± 3.2 | 28.76 ± 3.77 | 39.62 ± 9.27 | <0.001 |
| Females | 13.1 ± 2.51 | 17.9 ± 2.43 | 23.2 ± 1.88 | 28.7 ± 4.54 | 39.88 ± 10.38 | <0.001 |
| Body Muscle (%) | ||||||
| All subjects | 42.3 ± 4.38 | 38.16 ± 3.23 | 35.72 ± 3.68 | 33.27 ± 3.74 | 30.66 ± 3.17 | <0.001 |
| Males | 47.3 ± 1.92 | 43.7 ± 0.97 | 40 ± 2.02 | 38.85 ± 2.1 | 34 ± 3.89 | <0.001 |
| Females | 39.7 ± 2.73 | 36.5 ± 1.11 | 33.34 ± 1.62 | 31.83 ± 2.49 | 29.95 ± 2.53 | <0.001 |
| Body Muscle (kg) | ||||||
| All subjects | 24.45 ± 6.75 | 23.12 ± 5.73 | 23.92 ± 5.83 | 24.73 ± 5.96 | 27.13 ± 4.69 | 0.015 |
| Males | 32.51 ± 4.17 | 32.17 ± 2.76 | 30.27 ± 4.32 | 35.5 ± 3.57 | 33.71 ± 4 | <0.001 |
| Females | 20.2 ± 2.91 | 20.4 ± 2.93 | 20.45 ± 2.86 | 21.93 ± 1.69 | 25.77 ± 3.56 | 0.028 |
| Visceral Fat (AU) | ||||||
| All subjects | 4.6 ± 1.3 | 7.2 ± 1.23 | 10.51 ± 2.08 | 13.76 ± 3.3 | 17.58 ± 2.32 | <0.001 |
| Males | 4 ± 1.35 | 6.6 ± 1.08 | 8.8 ± 1.61 | 12.1 ± 1.86 | 17 ± 2.7 | <0.001 |
| Females | 5 ± 1.13 | 7.3 ± 1.23 | 11.41 ± 1.73 | 14.1 ± 3.51 | 17.7 ± 2.26 | <0.001 |
| Waist Circumference (cm) | ||||||
| All subjects | 70.7 ± 7.2 | 73.27 ± 6.88 | 79.31 ± 7.45 | 86.15 ± 5.87 | 98.3 ± 11.84 | <0.001 |
| Males | 78.3 ± 4.89 | 82.58 ± 5.03 | 87.35 ± 5.06 | 96.68 ± 2.26 | 109 ± 3.65 | <0.001 |
| Females | 66.8 ± 4.63 | 70.5 ± 4.55 | 74.9 ± 4.11 | 83.42 ± 2.24 | 96.09 ± 11.74 | <0.001 |
| Hip Circumference (cm) | ||||||
| All subjects | 91 ± 5.65 | 93.87 ± 6.76 | 98.5 ± 6.19 | 104.32 ± 5.06 | 114.07 ± 11.66 | <0.001 |
| Males | 94.7 ± 5.62 | 99 ± 3.61 | 100.5 ± 5.43 | 109.4 ± 4.75 | 114.1 ± 5.24 | <0.001 |
| Females | 89 ± 4.63 | 92.3 ± 6.74 | 97.5 ± 6.36 | 102.9 ± 4.29 | 114 ± 12.64 | <0.001 |
| Maximum Grip Strength (kg) | ||||||
| All subjects | 27.3 ± 10.46 | 25.52 ± 8.24 | 26.13 ± 9.06 | 25.58 ± 7.66 | 26.61 ± 6.65 | 0.773 |
| Males | 38.6 ± 9.5 | 36.95 ± 6.6 | 34.76 ± 9.35 | 36.94 ± 7.47 | 34.74 ± 7.24 | 0.01 |
| Females | 21.3 ± 4.12 | 22.1 ± 4.98 | 21.41 ± 4.1 | 22.64 ± 4.23 | 24.94 ± 5.21 | 0.671 |
| Physical Activity (%) | ||||||
| All subjects | 60.3 | 68.6 | 64.6 | 58.8 | 46.3 | 0.206 |
| Males | 88 | 93.8 | 69 | 85.7 | 42.9 | 0.339 |
| Females | 45.8 | 61.1 | 62.3 | 51.9 | 47.1 | 0.031 |
| Smoking (%) | ||||||
| All subjects | 32.9 | 31.4 | 30.5 | 41.2 | 29.3 | 0.82 |
| Males | 40 | 25 | 27.6 | 42.9 | 28.6 | 0.87 |
| Females | 29.2 | 33.3 | 32.1 | 40.7 | 29.3 | 0.778 |
| Alcohol Use (%) | ||||||
| All subjects | 86.3 | 90 | 85.4 | 70.6 | 90.2 | 0.088 |
| Males | 92 | 81.3 | 86.2 | 71.4 | 100 | 0.115 |
| Females | 83.3 | 92.6 | 84.9 | 70.4 | 88.2 | 0.469 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Robledo-Millán, C.R.; Diaz-Domínguez, M.R.; Castañeda-Ramírez, A.E.; Quiñones-Lara, E.; Valencia-Marín, S.; Suárez-García, R.X.; López-Desiderio, N.G.; Ramos-Cortés, C.A.; Gaytán Gómez, A.M.; Bello-López, J.M.; et al. A Novel Metabolic Risk Classification System Incorporating Body Fat, Waist Circumference, and Muscle Strength. J. Funct. Morphol. Kinesiol. 2025, 10, 72. https://doi.org/10.3390/jfmk10010072
Robledo-Millán CR, Diaz-Domínguez MR, Castañeda-Ramírez AE, Quiñones-Lara E, Valencia-Marín S, Suárez-García RX, López-Desiderio NG, Ramos-Cortés CA, Gaytán Gómez AM, Bello-López JM, et al. A Novel Metabolic Risk Classification System Incorporating Body Fat, Waist Circumference, and Muscle Strength. Journal of Functional Morphology and Kinesiology. 2025; 10(1):72. https://doi.org/10.3390/jfmk10010072
Chicago/Turabian StyleRobledo-Millán, Carlos Raúl, María Regina Diaz-Domínguez, Ari Evelyn Castañeda-Ramírez, Efrén Quiñones-Lara, Sebastián Valencia-Marín, Ricardo Xopán Suárez-García, Nely Gisela López-Desiderio, Claudio Adrían Ramos-Cortés, Areli Marlene Gaytán Gómez, Juan Manuel Bello-López, and et al. 2025. "A Novel Metabolic Risk Classification System Incorporating Body Fat, Waist Circumference, and Muscle Strength" Journal of Functional Morphology and Kinesiology 10, no. 1: 72. https://doi.org/10.3390/jfmk10010072
APA StyleRobledo-Millán, C. R., Diaz-Domínguez, M. R., Castañeda-Ramírez, A. E., Quiñones-Lara, E., Valencia-Marín, S., Suárez-García, R. X., López-Desiderio, N. G., Ramos-Cortés, C. A., Gaytán Gómez, A. M., Bello-López, J. M., & Saldívar-Cerón, H. I. (2025). A Novel Metabolic Risk Classification System Incorporating Body Fat, Waist Circumference, and Muscle Strength. Journal of Functional Morphology and Kinesiology, 10(1), 72. https://doi.org/10.3390/jfmk10010072








