Relation between Photogrammetry and Spinal Mouse for Sagittal Imbalance Assessment in Adolescents with Thoracic Kyphosis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design and Participants
2.2. Measurements Instruments
2.2.1. Spine Analysis
2.2.2. Photogrammetric Postural Analysis
2.3. Statistical Procedure
3. Results
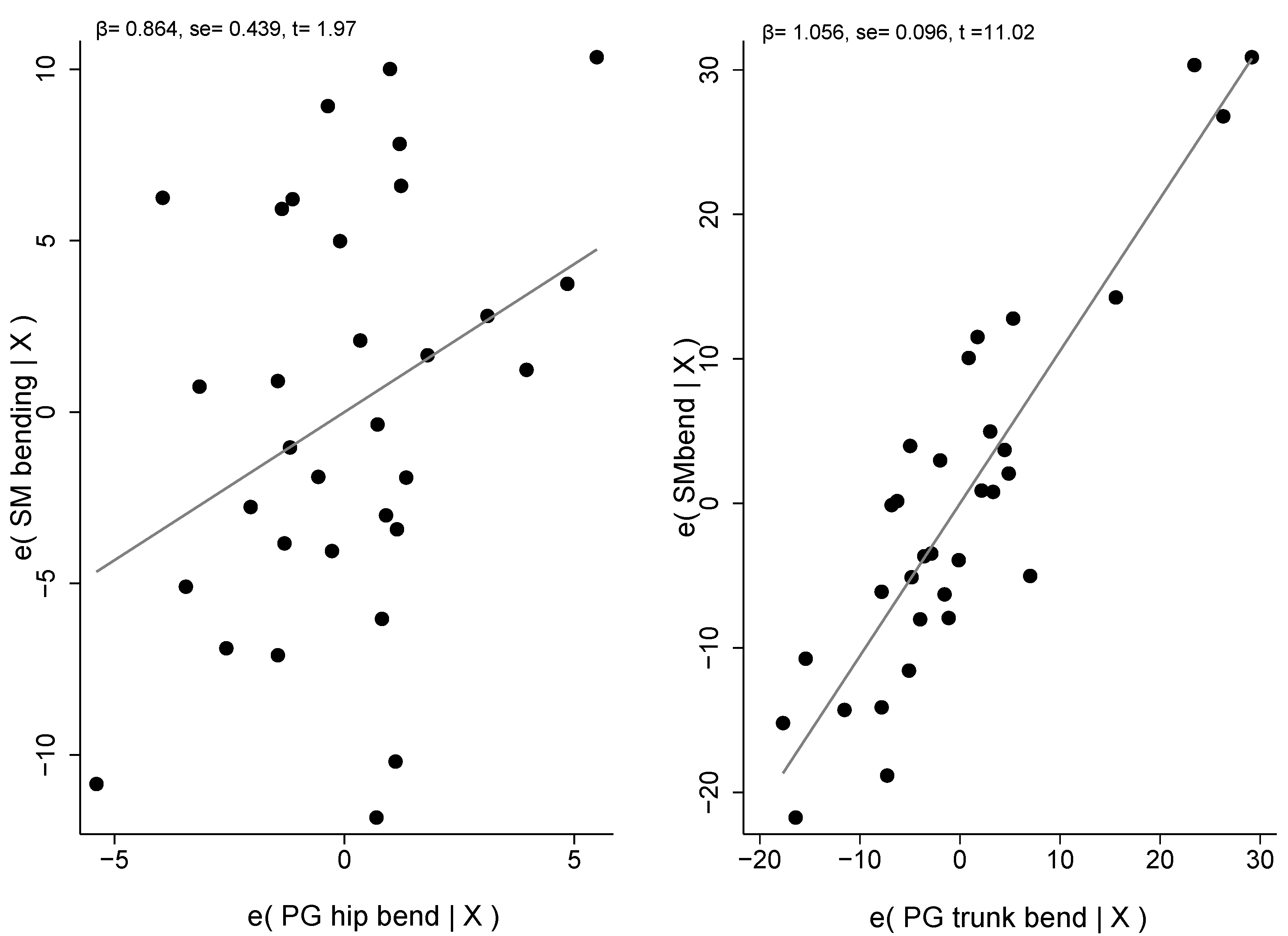
Linear Regression Models
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Feng, Q.; Wang, M.; Zhang, Y.; Zhou, Y. The Effect of a Corrective Functional Exercise Program on Postural Thoracic Kyphosis in Teenagers: A Randomized Controlled Trial. Clin. Rehabil. 2018, 32, 48–56. [Google Scholar] [CrossRef] [PubMed]
- Czaprowski, D.; Stoliński, Ł.; Tyrakowski, M.; Kozinoga, M.; Kotwicki, T. Non-Structural Misalignments of Body Posture in the Sagittal Plane. Scoliosis 2018, 13, 6. [Google Scholar] [CrossRef] [PubMed]
- Le Huec, J.C.; Thompson, W.; Mohsinaly, Y.; Barrey, C.; Faundez, A. Sagittal Balance of the Spine. Eur. Spine J. 2019, 28, 1889–1905. [Google Scholar] [CrossRef] [PubMed]
- Abelin-Genevois, K. Sagittal Balance of the Spine. Orthop. Traumatol. Surg. Res. 2021, 107, 102769. [Google Scholar] [CrossRef]
- Roussouly, P.; Nnadi, C. Sagittal Plane Deformity: An Overview of Interpretation and Management. Eur. Spine J. 2010, 19, 1824–1836. [Google Scholar] [CrossRef]
- Sahrmann, S. Diagnosis and Treatment of Movement Impairment Syndromes, 1st ed.; Mosby: St. Louis, MO, USA, 2001; ISBN 978-0-8016-7205-7. [Google Scholar]
- McCreary, E.K.; Provance, P.G.; Rodgers, M.M.; Romani, W.A.; Kendall, F.P. Muscles: Testing and Function with Posture and Pain, 5th ed.; Lippincott Williams & Wilkins: Baltimore, MD, USA, 2005; ISBN 978-0-7817-4780-6. [Google Scholar]
- Janssen, M.M.A.; Kouwenhoven, J.-W.M.; Schlösser, T.P.C.; Viergever, M.A.; Bartels, L.W.; Castelein, R.M.; Vincken, K.L. Analysis of Preexistent Vertebral Rotation in the Normal Infantile, Juvenile, and Adolescent Spine. Spine 2011, 36, E486–E491. [Google Scholar] [CrossRef]
- Dolphens, M.; Cagnie, B.; Coorevits, P.; Vleeming, A.; Palmans, T.; Danneels, L. Posture Class Prediction of Pre-Peak Height Velocity Subjects According to Gross Body Segment Orientations Using Linear Discriminant Analysis. Eur. Spine J. 2014, 23, 530–535. [Google Scholar] [CrossRef]
- Tribus, C.B. Scheuermann’s Kyphosis in Adolescents and Adults: Diagnosis and Management. J. Am. Acad. Orthop. Surg. 1998, 6, 36–43. [Google Scholar] [CrossRef]
- Lowe, T.G. Scheuermann’s Kyphosis. Neurosurg. Clin. N. Am. 2007, 18, 305–315. [Google Scholar] [CrossRef]
- Mac-Thiong, J.-M.; Labelle, H.; Roussouly, P. Pediatric Sagittal Alignment. Eur. Spine J. 2011, 20, 586–590. [Google Scholar] [CrossRef]
- Russo, L.; Giustino, V.; Toscano, R.E.; Secolo, G.; Secolo, I.; Iovane, A.; Messina, G. Can Tongue Position and Cervical ROM Affect Postural Oscillations? A Pilot and Preliminary Study. J. Hum. Sport Exerc. 2020, 15, S840–S847, In Proceedings of the Journal of Human Sport and Exercise-2020-Spring Conferences of Sports Science; Universidad de Alicante, 2020. [Google Scholar]
- Russo, L.; Bartolucci, P.; Ardigò, L.P.; Padulo, J.; Pausic, J.; Iacono, A.D. An Exploratory Study on the Acute Effects of Proprioceptive Exercise and/or Neuromuscular Taping on Balance Performance. Asian J. Sport. Med. 2018, 9, e63020. [Google Scholar] [CrossRef]
- Giustino, V.; Parroco, A.M.; Gennaro, A.; Musumeci, G.; Palma, A.; Battaglia, G. Physical Activity Levels and Related Energy Expenditure during COVID-19 Quarantine among the Sicilian Active Population: A Cross-Sectional Online Survey Study. Sustainability 2020, 12, 4356. [Google Scholar] [CrossRef]
- Cohen, L.; Kobayashi, S.; Simic, M.; Dennis, S.; Refshauge, K.; Pappas, E. Non-Radiographic Methods of Measuring Global Sagittal Balance: A Systematic Review. Scoliosis 2017, 12, 30. [Google Scholar] [CrossRef]
- Roggio, F.; Petrigna, L.; Trovato, B.; Zanghì, M.; Sortino, M.; Vitale, E.; Rapisarda, L.; Testa, G.; Pavone, V.; Pavone, P.; et al. Thermography and Rasterstereography as a Combined Infrared Method to Assess the Posture of Healthy Individuals. Sci. Rep. 2023, 13, 4263. [Google Scholar] [CrossRef]
- Roggio, F.; Petrigna, L.; Filetti, V.; Vitale, E.; Rapisarda, V.; Musumeci, G. Infrared Thermography for the Evaluation of Adolescent and Juvenile Idiopathic Scoliosis: A Systematic Review. J. Therm. Biol. 2023, 113, 103524. [Google Scholar] [CrossRef] [PubMed]
- Roggio, F.; Ravalli, S.; Maugeri, G.; Bianco, A.; Palma, A.; Di Rosa, M.; Musumeci, G. Technological Advancements in the Analysis of Human Motion and Posture Management through Digital Devices. World J. Orthop. 2021, 12, 467–484. [Google Scholar] [CrossRef]
- Krott, N.L.; Wild, M.; Betsch, M. Meta-Analysis of the Validity and Reliability of Rasterstereographic Measurements of Spinal Posture. Eur. Spine J. 2020, 29, 2392–2401. [Google Scholar] [CrossRef]
- Elsayed, W.; Farrag, A.; Muaidi, Q.; Almulhim, N. Relationship between Sagittal Spinal Curves Geometry and Isokinetic Trunk Muscle Strength in Adults. Eur. Spine J. 2018, 27, 2014–2022. [Google Scholar] [CrossRef]
- Russo, L.; Padulo, J. Letter to the Editor Concerning “Relationship between Sagittal Spinal Curves Geometry and Isokinetic Trunk Muscle Strength in Adults” by Elsayed W, Farrag A, Muaidi Q, Almulhim N (Eur Spine J [2018] 27:2014–2022). Eur Spine J. 2019, 28, 191–192. [Google Scholar] [CrossRef]
- Mohokum, M.; Mendoza, S.; Udo, W.; Sitter, H.; Paletta, J.R.; Skwara, A. Reproducibility of Rasterstereography for Kyphotic and Lordotic Angles, Trunk Length, and Trunk Inclination: A Reliability Study. Spine 2010, 35, 1353–1358. [Google Scholar] [CrossRef] [PubMed]
- Molinaro, L.; Russo, L.; Cubelli, F.; Taborri, J.; Rossi, S. Reliability Analysis of an Innovative Technology for the Assessment of Spinal Abnormalities. In Proceedings of the 2022 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Messina, Italy, 22–24 June 2022; pp. 1–6. [Google Scholar]
- Roghani, T.; Khalkhali Zavieh, M.; Rahimi, A.; Talebian, S.; Dehghan Manshadi, F.; Akbarzadeh Baghban, A.; King, N.; Katzman, W. The Reliability of Standing Sagittal Measurements of Spinal Curvature and Range of Motion in Older Women With and Without Hyperkyphosis Using a Skin-Surface Device. J. Manip. Physiol. Ther. 2017, 40, 685–691. [Google Scholar] [CrossRef] [PubMed]
- Barrett, E.; McCreesh, K.; Lewis, J. Reliability and Validity of Non-Radiographic Methods of Thoracic Kyphosis Measurement: A Systematic Review. Man. Ther. 2014, 19, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Kellis, E.; Adamou, G.; Tzilios, G.; Emmanouilidou, M. Reliability of Spinal Range of Motion in Healthy Boys Using a Skin-Surface Device. J. Manip. Physiol. Ther. 2008, 31, 570–576. [Google Scholar] [CrossRef] [PubMed]
- Mannion, A.F.; Knecht, K.; Balaban, G.; Dvorak, J.; Grob, D. A New Skin-Surface Device for Measuring the Curvature and Global and Segmental Ranges of Motion of the Spine: Reliability of Measurements and Comparison with Data Reviewed from the Literature. Eur. Spine J. 2004, 13, 122–136. [Google Scholar] [CrossRef]
- Belli, G.; Toselli, S.; Latessa, P.M.; Mauro, M. Evaluation of Self-Perceived Body Image in Adolescents with Mild Idiopathic Scoliosis. Eur. J. Investig. Health Psychol. Educ. 2022, 12, 319–333. [Google Scholar] [CrossRef]
- Macedo Ribeiro, A.F.; Bergmann, A.; Lemos, T.; Pacheco, A.G.; Mello Russo, M.; Santos de Oliveira, L.A.; de Carvalho Rodrigues, E. Reference Values for Human Posture Measurements Based on Computerized Photogrammetry: A Systematic Review. J. Manip. Physiol. Ther. 2017, 40, 156–168. [Google Scholar] [CrossRef]
- Krawczky, B.; Pacheco, A.G.; Mainenti, M.R.M. A Systematic Review of the Angular Values Obtained by Computerized Photogrammetry in Sagittal Plane: A Proposal for Reference Values. J. Manip. Physiol. Ther. 2014, 37, 269–275. [Google Scholar] [CrossRef]
- Trovato, B.; Roggio, F.; Sortino, M.; Zanghì, M.; Petrigna, L.; Giuffrida, R.; Musumeci, G. Postural Evaluation in Young Healthy Adults through a Digital and Reproducible Method. J. Funct. Morphol. Kinesiol. 2022, 7, 98. [Google Scholar] [CrossRef]
- Russo, L.; Montagnani, E.; Pietrantuono, D.; D’Angona, F.; Fratini, T.; Di Giminiani, R.; Palermi, S.; Ceccarini, F.; Migliaccio, G.M.; Lupu, E.; et al. Self-Myofascial Release of the Foot Plantar Surface: The Effects of a Single Exercise Session on the Posterior Muscular Chain Flexibility after One Hour. Int. J. Environ. Res. Public Health 2023, 20, 974. [Google Scholar] [CrossRef]
- Porto, A.B.; Okazaki, V.H.A. Procedures of Assessment on the Quantification of Thoracic Kyphosis and Lumbar Lordosis by Radiography and Photogrammetry: A Literature Review. J. Bodyw. Mov. Ther. 2017, 21, 986–994. [Google Scholar] [CrossRef] [PubMed]
- Porto, A.B.; Okazaki, V.H.A. Thoracic Kyphosis and Lumbar Lordosis Assessment by Radiography and Photogrammetry: A Review of Normative Values and Reliability. J. Manip. Physiol. Ther. 2018, 41, 712–723. [Google Scholar] [CrossRef] [PubMed]
- Post, R.B.; Leferink, V.J.M. Spinal Mobility: Sagittal Range of Motion Measured with the SpinalMouse, a New Non-Invasive Device. Arch. Orthop. Trauma Surg. 2004, 124, 187–192. [Google Scholar] [CrossRef]
- Livanelioglu, A.; Kaya, F.; Nabiyev, V.; Demirkiran, G.; Fırat, T. The Validity and Reliability of “Spinal Mouse” Assessment of Spinal Curvatures in the Frontal Plane in Pediatric Adolescent Idiopathic Thoraco-Lumbar Curves. Eur. Spine J. 2016, 25, 476–482. [Google Scholar] [CrossRef] [PubMed]
- Ardigò, L.P.; Palermi, S.; Padulo, J.; Dhahbi, W.; Russo, L.; Linetti, S.; Cular, D.; Tomljanovic, M. External Responsiveness of the SuperOpTM Device to Assess Recovery After Exercise: A Pilot Study. Front. Sport. Act. Living 2020, 2, 67. [Google Scholar] [CrossRef] [PubMed]
- Russo, L.; Di Capua, R.; Arnone, B.; Borrelli, M.; Coppola, R.; Esposito, F.; Padulo, J. Shoes and Insoles: The Influence on Motor Tasks Related to Walking Gait Variability and Stability. Int. J. Environ. Res. Public Health 2020, 17, 4569. [Google Scholar] [CrossRef]
- Singla, D.; Veqar, Z.; Hussain, M.E. Photogrammetric Assessment of Upper Body Posture Using Postural Angles: A Literature Review. J. Chiropr. Med. 2017, 16, 131–138. [Google Scholar] [CrossRef]
- Saad, K.R.; Colombo, A.S.; Ribeiro, A.P.; João, S.M.A. Reliability of Photogrammetry in the Evaluation of the Postural Aspects of Individuals with Structural Scoliosis. J. Bodyw. Mov. Ther. 2012, 16, 210–216. [Google Scholar] [CrossRef]
- Azadinia, F.; Hosseinabadi, M.; Ebrahimi, I.; Mohseni-Bandpei, M.-A.; Ghandhari, H.; Yassin, M.; Behtash, H.; Ganjavian, M.-S. Validity and Test–Retest Reliability of Photogrammetry in Adolescents with Hyperkyphosis. Physiother. Theory Pract. 2022, 38, 3018–3026. [Google Scholar] [CrossRef]
- Stolinski, L.; Kozinoga, M.; Czaprowski, D.; Tyrakowski, M.; Cerny, P.; Suzuki, N.; Kotwicki, T. Two-Dimensional Digital Photography for Child Body Posture Evaluation: Standardized Technique, Reliable Parameters and Normative Data for Age 7–10 Years. Scoliosis 2017, 12, 38. [Google Scholar] [CrossRef]
- Dodge, Y. The Concise Encyclopedia of Statistics, 2010th ed.; Springer: Philadelphia, PA, USA, 2008; ISBN 978-0-397-51837-1. [Google Scholar]
- Bland, J.M.; Altman, D.G. Statistical Methods for Assessing Agreement between Two Methods of Clinical Measurement. Lancet 1986, 1, 307–310. [Google Scholar] [CrossRef] [PubMed]
- Cirillo Totera, J.I.; Fleiderman Valenzuela, J.G.; Garrido Arancibia, J.A.; Pantoja Contreras, S.T.; Beaulieu Lalanne, L.; Alvarez-Lemos, F.L. Sagittal Balance: From Theory to Clinical Practice. EFORT Open Rev. 2021, 6, 1193–1202. [Google Scholar] [CrossRef] [PubMed]
- Demir, E.; Güzel, N.; Çobanoğlu, G.; Kafa, N. The Reliability of Measurements with the Spinal Mouse Device in Frontal and Sagittal Planes in Asymptomatic Female Adolescents. Ann. Clin. Anal. Med. 2020, 11, 146–149. [Google Scholar] [CrossRef]
- Muyor, J.M.; López-Miñarro, P.A.; Alacid, F. The Relationship between Hamstring Muscle Extensibility and Spinal Postures Varies with the Degree of Knee Extension. J. Appl. Biomech. 2013, 29, 678–686. [Google Scholar] [CrossRef]
- Furlanetto, T.S.; Sedrez, J.A.; Candotti, C.T.; Loss, J.F. Photogrammetry as a Tool for the Postural Evaluation of the Spine: A Systematic Review. World J. Orthop. 2016, 7, 136–148. [Google Scholar] [CrossRef]
- López-Miñarro, P.A.; Vaquero-Cristóbal, R.; Alacid, F.; Isorna, M.; Muyor, J.M. Comparison of Sagittal Spinal Curvatures and Pelvic Tilt in Highly Trained Athletes from Different Sport Disciplines. Kinesiology 2017, 49, 109–116. [Google Scholar] [CrossRef]
- Rabieezadeh, A.; Hovanloo, F.; Khaleghi, M.; Akbari, H. The relationship of height, weight and body mass index with curvature of spine kyphosis and lordosis in 12–15-year old male adolescents of Tehran. Turk. J. Sport Exe. 2016, 18, 42–46. [Google Scholar]
- Hazar, Z.; Karabicak, G.O.; Tiftikci, U. Reliability of Photographic Posture Analysis of Adolescents. J. Phys. Ther. Sci. 2015, 27, 3123–3126. [Google Scholar] [CrossRef]
- Carregaro, R.L.; Silva, L.; Gil Coury, H.J.C. Comparison between Two Clinical Tests for Evaluating the Flexibility of the Posterior Muscles of the Thigh. Braz. J. Phys. Ther. 2007, 11, 139–145. [Google Scholar] [CrossRef]
- Navarro, I.J.R.L.; Candotti, C.T.; do Amaral, M.A.; Dutra, V.H.; Gelain, G.M.; Loss, J.F. Validation of the Measurement of the Angle of Trunk Rotation in Photogrammetry. J. Manip. Physiol. Ther. 2020, 43, 50–56. [Google Scholar] [CrossRef]




| Variable (n = 34) | Mean | Std | Min | Max |
|---|---|---|---|---|
| Age [year] | 13.06 | 1.84 | 10 | 18 |
| Height [cm] | 158.56 | 12.73 | 139 | 189 |
| Weight [kg] | 47.03 | 12.19 | 26 | 75 |
| PG mall-tragus [°] | 2.79 | 1.20 | 1 | 6 |
| PG trunk bend [°] | 91.71 | 13.35 | 68 | 121 |
| PG sacrum bend [°] | 37.15 | 12.02 | 4 | 55 |
| PG hip bend [°] | 8.71 | 2.69 | 3 | 15 |
| SM stand [°] | 1.68 | 2.81 | −6 | 7 |
| SM bend [°] | 90.56 | 13.16 | 65 | 122 |
| SM fixed stand [°] | 45.94 | 8.24 | 29 | 62 |
| SM phys. stand [°] | 48.29 | 9.14 | 30 | 69 |
| SM fixed bend [°] | 63.71 | 10.23 | 45 | 87 |
| SM phys. bend [°] | 63.41 | 9.45 | 46 | 82 |
| SM Rachid stand [mm] | 457.18 | 44.02 | 394 | 593 |
| SM Rachid bend [mm] | 538.44 | 51.33 | 449 | 673 |
| PG Mall–Tragus | PG Trunk Bend | PG Sacrum Bend | PG Hip Bend | SM Stand | SM Bend | SM Fixed Stand | SM Phys. Stand | SM Fixed Bend | SM Phys. Bend | SM Rachid Stand | SM Rachid Bend | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PG mall–tragus | - | |||||||||||
| PG trunk bend | 0.003 | - | ||||||||||
| PG sacrum bend | −0.076 | −0.860 * | - | |||||||||
| PG hip bend | −0.176 | −0.479 * | 0.327 | - | ||||||||
| SM stand | −0.045 | −0.059 | 0.061 | 0.379 * | - | |||||||
| SM bend | −0.041 | 0.839 * | −0.732 * | −0.237 | 0.119 | - | ||||||
| SM fixed stand | 0.013 | −0.204 | 0.330 | −0.151 | −0.098 | −0.29 | - | |||||
| SM phys. stand | 0.036 | −0.024 | 0.195 | −0.182 | −0.020 | −0.17 | 0.908 * | - | ||||
| SM fixed bend | 0.138 | −0.526 * | 0.559 * | −0.063 | −0.076 | −0.61 * | 0.403 * | 0.251 | - | |||
| SM phys. bend | 0.060 | −0.316 | 0.350 * | 0.024 | −0.149 | −0.41 * | 0.404 * | 0.420 * | 0.637 * | - | ||
| SM Rachid stand | 0.392 * | 0.000 | 0.042 | −0.222 | −0.102 | −0.08 | 0.206 | 0.319 | 0.121 | 0.272 | - | |
| SM Rachid bend | 0.273 | −0.014 | 0.065 | −0.243 | −0.258 | −0.1 | 0.180 | 0.243 | 0.228 | 0.332 | 0.914 * | - |
| Source | SS | df | MS | n | F(2, 28) | p | R2 | Adj. R2 | Root MSE |
|---|---|---|---|---|---|---|---|---|---|
| Model | 4513.86 | 2 | 2256.93 | 32 | 64.44 | <0.001 | 0.816 | 0.804 | 5.918 |
| Residual | 1015.64 | 29 | 35.02 | ||||||
| Total | 5529.5 | 31 | 178.37 | ||||||
| SM bending | β | SE | t | p | 95% CI | ||||
| PG hip bend | 0.86413 | 0.4394 | 1.97 | 0.059 | −0.0346 | 1.763 | |||
| PG trunk bend | 1.0557 | 0.0958 | 11.02 | <0.001 | 0.86 | 1.252 | |||
| Intercept | −12.749 | 10.874 | −1.17 | 0.251 | −34.99 | 9.491 | |||
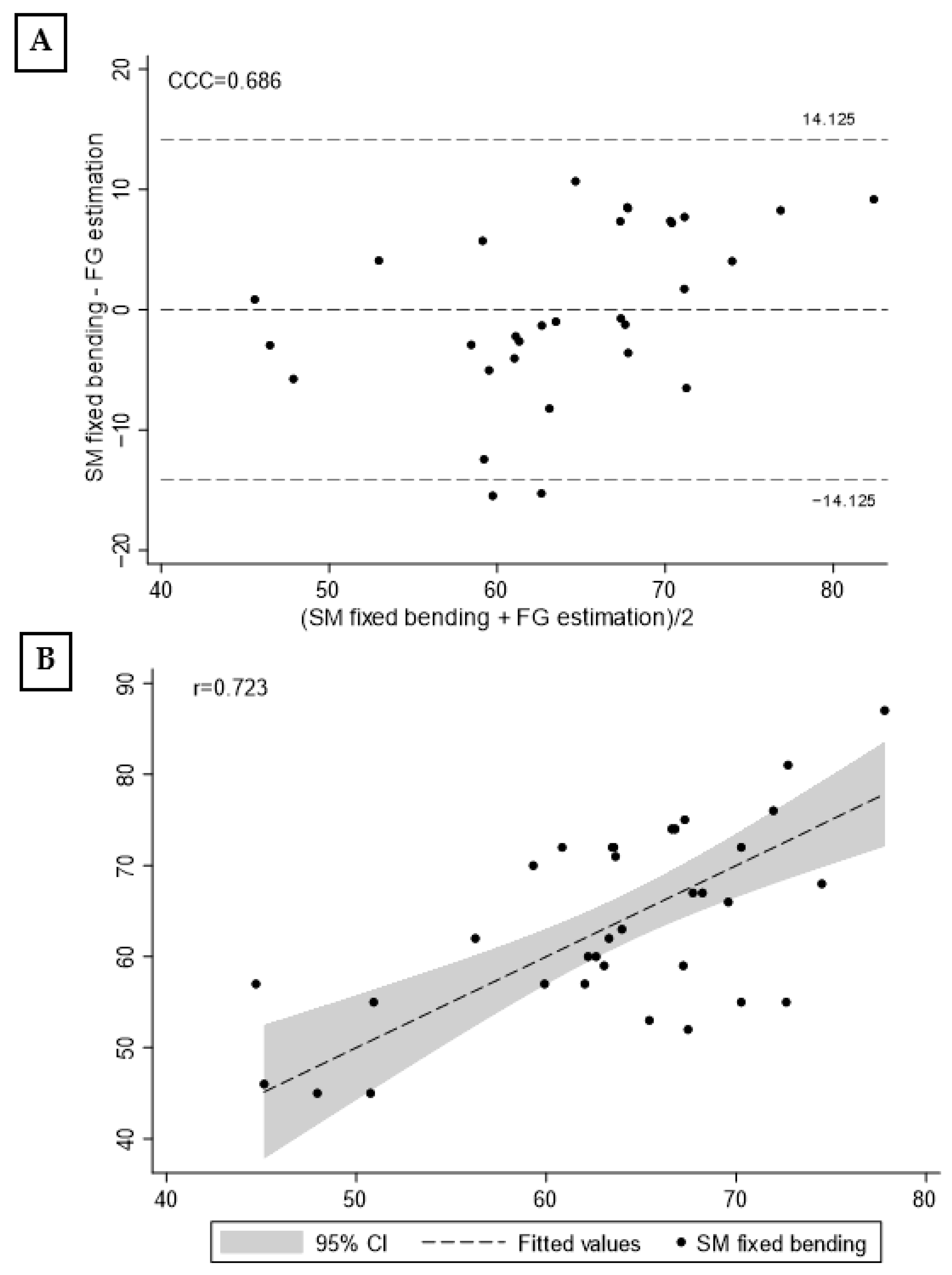
| Source | SS | df | MS | n | F(2, 28) | p | R2 | Adj. R2 | Root MSE |
|---|---|---|---|---|---|---|---|---|---|
| Model | 1701.8126 | 2 | 850.90628 | 31 | 15.29 | <0.001 | 0.522 | 0.488 | 7.46 |
| Residual | 1558.0584 | 28 | 55.644943 | ||||||
| Total | 3259.871 | 30 | 108.66237 | ||||||
| SM fixed bending | β | SE | t | p | [95% conf. | interval] | |||
| PG hip bend | −2.122705 | 0.6704444 | −3.17 | 0.004 | −3.496048 | −0.749361 | |||
| PG trunk bend | −0.678946 | 0.1232905 | −5.51 | <0.001 | −0.931495 | −0.426397 | |||
| Intercept | 144.2784 | 15.00178 | 9.62 | <0.001 | 113.5486 | 175.0081 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Belli, G.; Toselli, S.; Mauro, M.; Maietta Latessa, P.; Russo, L. Relation between Photogrammetry and Spinal Mouse for Sagittal Imbalance Assessment in Adolescents with Thoracic Kyphosis. J. Funct. Morphol. Kinesiol. 2023, 8, 68. https://doi.org/10.3390/jfmk8020068
Belli G, Toselli S, Mauro M, Maietta Latessa P, Russo L. Relation between Photogrammetry and Spinal Mouse for Sagittal Imbalance Assessment in Adolescents with Thoracic Kyphosis. Journal of Functional Morphology and Kinesiology. 2023; 8(2):68. https://doi.org/10.3390/jfmk8020068
Chicago/Turabian StyleBelli, Guido, Stefania Toselli, Mario Mauro, Pasqualino Maietta Latessa, and Luca Russo. 2023. "Relation between Photogrammetry and Spinal Mouse for Sagittal Imbalance Assessment in Adolescents with Thoracic Kyphosis" Journal of Functional Morphology and Kinesiology 8, no. 2: 68. https://doi.org/10.3390/jfmk8020068
APA StyleBelli, G., Toselli, S., Mauro, M., Maietta Latessa, P., & Russo, L. (2023). Relation between Photogrammetry and Spinal Mouse for Sagittal Imbalance Assessment in Adolescents with Thoracic Kyphosis. Journal of Functional Morphology and Kinesiology, 8(2), 68. https://doi.org/10.3390/jfmk8020068










