Running-Related Overuse Injuries and Their Relationship with Run and Resistance Training Characteristics in Adult Recreational Runners: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedures
2.3. Statistical Analysis
3. Results
3.1. Participants
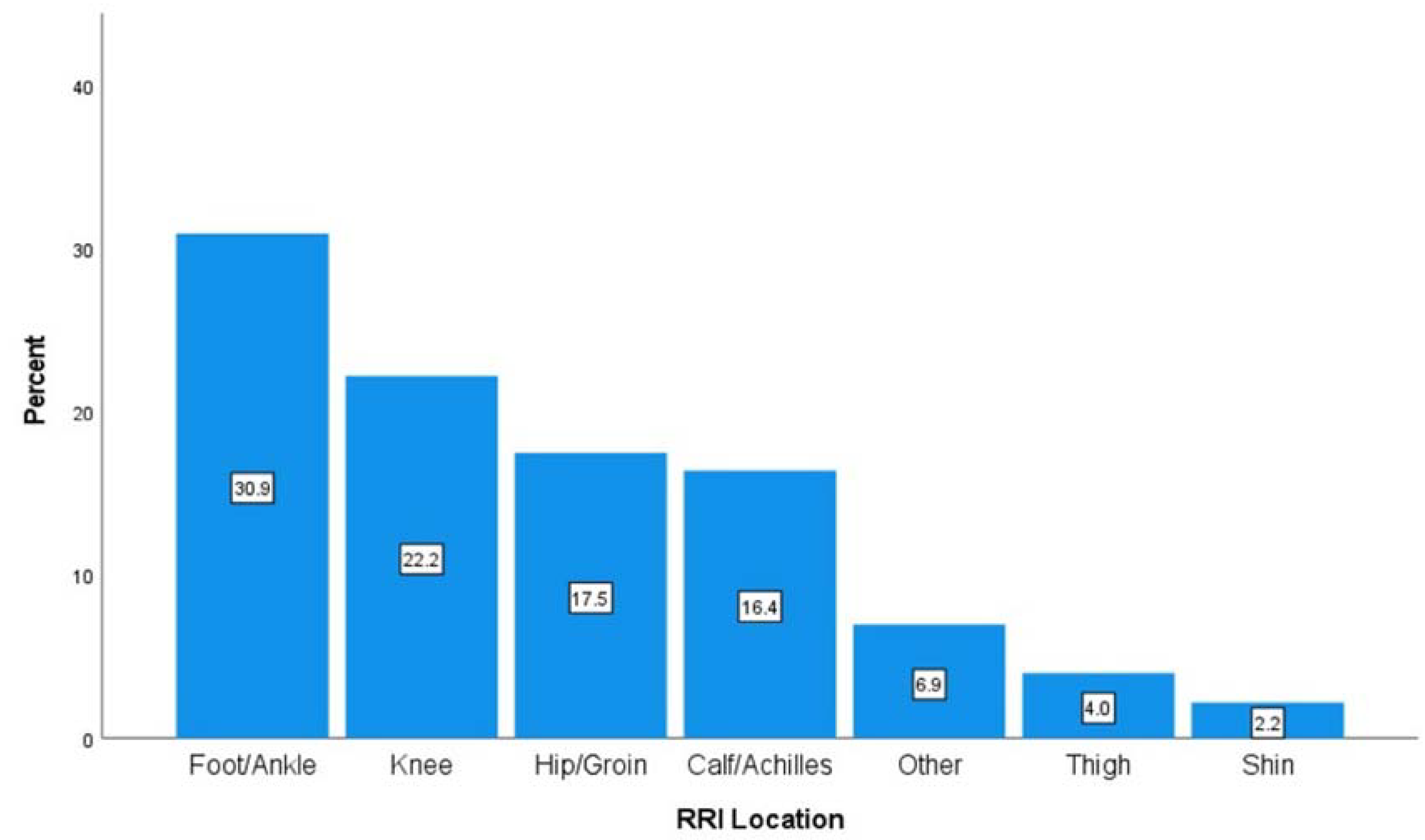
3.2. Injury Prevalence and Characteristics
3.3. Relationships with Resistance Training Characteristics
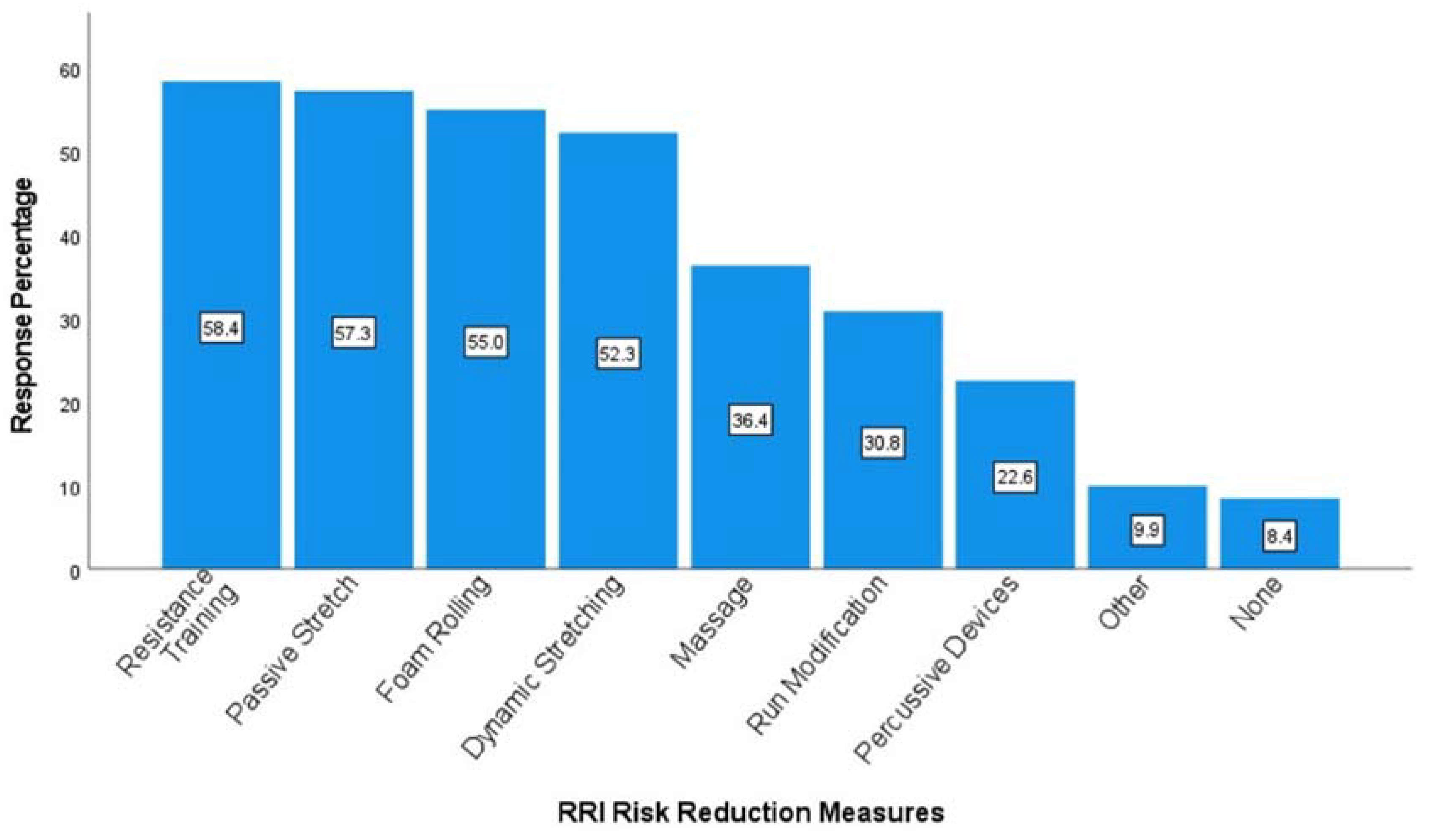
3.4. Strategies for Reducing Injury Risk
4. Discussion
4.1. Injury Prevalence and Location
4.2. Injury Associations with Resistance Training
4.3. Strategies for Reducing Injury Risk
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Andersen, J.; RunRepeat. The State of Running 2019. 2021. Available online: https://runrepeat.com/state-of-running (accessed on 8 July 2022).
- Lange, D.; Statistica. Running & Jogging—Statistics & Facts. 2020. Available online: https://www.statista.com/topics/1743/running-and-jogging/ (accessed on 8 July 2022).
- Malchrowicz, J.; Malchrowicz-Mośko, E.; Fadigas, A. Age-related motives in mass running events participation. Olimp. J. Olymp. Stud. 2018, 2, 257–273. [Google Scholar] [CrossRef]
- Janssen, M.; Walravens, R.; Thibaut, E.; Scheerder, J.; Brombacher, A.; Vos, S. Understanding different types of recreational runners and how they use running-related technology. Int. J. Environ. Res. Public Health 2020, 17, 2276. [Google Scholar] [CrossRef] [PubMed]
- Hespanhol, L.C., Jr.; Pillay, J.D.; van Mechelen, W.; Verhagen, E. Meta-analyses of the effects of habitual running on indices of health in physically inactive adults. Sports Med. 2015, 45, 1455–1468. [Google Scholar] [CrossRef] [PubMed]
- Quirk, H.; Bullas, A.; Haake, S.; Goyder, E.; Graney, M.; Wellington, C.; Copeland, R.; Reece, L.; Stevinson, C. Exploring the benefits of participation in community-based running and walking events: A cross-sectional survey of parkrun participants. BMC Public Health 2021, 21, 1978. [Google Scholar] [CrossRef]
- Lee, D.; Brellenthin, A.G.; Thompson, P.D.; Sui, X.; Lee, I.M.; Lavie, C.J. Running as a key lifestyle medicine for longevity. Prog. Cardiovasc. Dis. 2017, 60, 45–55. [Google Scholar] [CrossRef] [PubMed]
- Yamato, T.P.; Saragiotto, B.T.; Lopes, A.D. A consensus definition of running-related injury in recreational runners: A modified Delphi approach. J. Orthop. Sports Phys. Ther. 2015, 45, 375–380. Available online: http://www.jospt.org/doi/10.2519/jospt.2015.5741 (accessed on 5 May 2020). [CrossRef] [PubMed]
- Centers for Disease Control and Prevention [CDC]. Trends in Meeting the 2008 Physical Activity Guidelines, 2008–2018; CDC: Atlanta, GA, USA, 2018. [Google Scholar]
- Hespanhol, L.C., Jr.; van Mechelen, W.; Postuma, E.; Verhagen, E. Health and economic burden of running-related injuries in runners training for an event: A prospective cohort study. Scand. J. Med. Sci. Sports 2016, 26, 1091–1099. [Google Scholar] [CrossRef]
- Fokkema, T.; Hartgens, F.; Kluitenberg, B.; Verhagen, E.; Backx, F.J.G.; van der Worp, H.; Bierma-Zeinstra, S.M.; Koes, B.W.; van Middelkoop, M. Reasons and predictors of discontinuation of running after a running program for novice runners. J. Sci. Med. Sport 2019, 22, 106–111. [Google Scholar] [CrossRef]
- Desai, P.; Jungmalm, J.; Borjesson, M.; Karlsson, J.; Grau, S. Recreational runners with a history of injury are twice as likely to sustain a running-related injury as runners with no history of injury: A 1-year prospective cohort study. J. Orthop. Sports Phys. Ther. 2021, 51, 144–150. [Google Scholar] [CrossRef]
- Kluitenberg, B.; van Middelkoop, M.; Verhagen, E.; Hartgens, F.; Huisstede, B.; Diercks, R.; van der Worp, H. The impact of injury definition on injury surveillance in novice runners. J. Sci. Med. Sport 2016, 19, 470–475. [Google Scholar] [CrossRef]
- Francis, P.; Whatman, C.; Sheerin, K.; Hume, P.; Johnson, M.I. The proportion of lower limb running injuries by gender, anatomical location and specific pathology: A systematic review. J. Sports Sci. Med. 2019, 18, 21–31. [Google Scholar] [PubMed]
- Hollander, K.; Baumann, A.; Zech, A.; Verhagen, E. Prospective monitoring of health problems among recreational runners preparing for a half marathon. BMJ Open Sport Exerc. Med. 2018, 4, 308. [Google Scholar] [CrossRef] [PubMed]
- Soligard, T.; Schwellnus, M.; Alonso, J.M.; Bahr, R.; Clarsen, B.; Dijkstra, H.P.; Gabbett, T.; Gleeson, M.; Hägglund, M.; Hutchinson, M.R.; et al. How much is too much? (Part 1) International Olympic Committee consensus statement on load in sport and risk of injury. Br. J. Sports Med. 2016, 50, 1030–1041. [Google Scholar] [CrossRef]
- Brund, R.B.K.; Rasmussen, S.; Nielsen, R.O.; Kersting, U.G.; Laessoe, U.; Voigt, M. The association between eccentric hip abduction strength and hip and knee angular movements in recreational male runners: An explorative study. Scand. J. Med. Sci. Sports 2018, 28, 473–478. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, A.S.; de Oliveira Silva, D.; Barton, C.J.; Briani, R.V.; Taborda, B.; Pazzinatto, M.F.; de Azevedo, F.M. Impaired isometric, concentric, and eccentric rate of torque development at the hip and knee in patellofemoral pain. J. Strength Cond. Res. 2019, 35, 2492–2497. [Google Scholar] [CrossRef] [PubMed]
- Palmer, K.; Hebron, C.; Williams, J.M. A randomised trial into the effect of an isolated hip abductor strengthening programme and a functional motor control programme on knee kinematics and hip muscle strength. BMC Musculoskelet. Disord. 2015, 16, 105. [Google Scholar] [CrossRef] [PubMed]
- Radzak, K.N.; Stickley, C.D. Fatigue-induced hip-abductor weakness and changes in biomechanical risk factors for running-related injuries. J. Athl. Train. 2020, 55, 1270–1276. [Google Scholar] [CrossRef] [PubMed]
- Ramskov, D.; Barton, C.; Nielsen, R.O.; Rasmussen, S. High eccentric hip abduction strength reduces the risk of developing patellofemoral pain among novice runners initiating a self-structured running program: A 1-year observational study. J. Orthop. Sports Phys. Ther. 2015, 45, 153–161. [Google Scholar] [CrossRef]
- Brachman, A.; Kamieniarz, A.; Michalska, J.; Pawłowski, M.; Słomka, K.J.; Juras, G. Balance training programs in athletes-A systematic review. J. Hum. Kinet. 2017, 58, 45–64. [Google Scholar] [CrossRef]
- Sudhakar, S.; Veena Kirthika, S.; Padmanabhan, K.; Senthil Nathan, C.V.; Ramachandran, S.; Rajalaxmi, V.; Sowmiya, S.; Selvam, P.S. Which is efficient in improving postural control among the novice runners? Isolated ankle strengthening or functional balance training programme: A randomized controlled trial. Res. J. Pharm. Technol. 2018, 11, 1461–1466. [Google Scholar] [CrossRef]
- McGill, E.A.; Montel, I. (Eds.) NASM Essentials of Sports Performance Training, 2nd ed.; Jones & Bartlett Learning: Burlington, MA, USA, 2019. [Google Scholar]
- Haff, G.G.; Triplett, N.T. (Eds.) Essentials of Strength Training and Conditioning, 4th ed.; Human Kinetics: Champaign, IL, USA, 2016. [Google Scholar]
- Lauersen, J.B.; Andersen, T.E.; Andersen, L.B. Strength training as superior, dose-dependent and safe prevention of acute and overuse sports injuries: A systematic review, qualitative analysis and meta-analysis. Br. J. Sports Med. 2018, 52, 1557–1563. [Google Scholar] [CrossRef] [PubMed]
- Toresdahl, B.G.; McElheny, K.; Metzl, J.; Ammerman, B.; Chang, B.; Kinderknecht, J. A randomized study of a strength training program to prevent injuries in runners of the New York City Marathon. Sports Health 2020, 12, 74–79. [Google Scholar] [CrossRef]
- Voight, A.M.; Roberts, B.; Lunos, S.; Chow, L. Pre- and postmarathon training habits of nonelite runners. Open Access J. Sports Med. 2011, 2, 13. Available online: www.dovepress.com (accessed on 21 June 2022). [PubMed]
- Bampton, E.A.; Johnson, S.T.; Vallance, J.K. Correlates and preferences of resistance training among older adults in Alberta, Canada. Can. J. Public Health 2016, 107, e272–e277. [Google Scholar] [CrossRef] [PubMed]
- Blagrove, R.C.; Brown, N.; Howatson, G.; Hayes, P.R. Strength and conditioning habits of competitive distance runners. J. Strength Cond. Res. 2020, 34, 1392–1399. [Google Scholar] [CrossRef] [PubMed]
- Fokkema, T.; De Vos, R.J.; Bierma-Zeinstra, S.M.A.; Van Middelkoop, M. Opinions, barriers, and facilitators of injury prevention in recreational runners. J. Orthop. Sports Phys. Ther. 2019, 49, 736–745. [Google Scholar] [CrossRef]
- García-Pinillos, F.; Lago-Fuentes, C.; Jaén-Carrillo, D.; Bujalance-Moreno, P.; Latorre-Román, P.Á.; Roche-Seruendo, L.E.; Ramirez-Campillo, R. Strength training habits in amateur endurance runners in Spain: Influence of athletic level. Int. J. Environ. Res. Public Health 2020, 17, 8184. [Google Scholar] [CrossRef]
- Hespanhol Junior, L.C.; Costa, L.O.P.; Carvalho, A.C.A.; Lopes, A.D. A description of training characteristics and its association with previous musculoskeletal injuries in recreational runners: A cross-sectional study. Braz. J. Phys. Ther. 2012, 16, 46–53. [Google Scholar] [CrossRef]
- Hespanhol Junior, L.C.; Pena Costa, L.O.; Lopes, A.D. Previous injuries and some training characteristics predict running-related injuries in recreational runners: A prospective cohort study. J. Physiother. 2013, 59, 263–269. [Google Scholar] [CrossRef]
- Linton, L.; Valentin, S. Running with injury: A study of UK novice and recreational runners and factors associated with running related injury. J. Sci. Med. Sport 2018, 21, 1221–1225. [Google Scholar] [CrossRef]
- Luckin, K.; Badenhorst, C.; Hoyne, G.; Cripps, A.; Landers, G.; Merrells, R. Strength training in long-distance triathletes: Barriers and characteristics. J. Strength Cond. Res. 2018, 21, S30. [Google Scholar] [CrossRef]
- Shakespear-Druery, J.; De Cocker, K.; Biddle, S.J.H.; Bennie, J. Muscle-Strengthening Exercise Questionnaire (MSEQ): An assessment of concurrent validity and test-retest reliability. BMJ Open Sport Exerc. Med. 2022, 8, e001225. [Google Scholar] [CrossRef] [PubMed]
- Taunton, J.E.; Ryan, M.B.; Clement, D.B.; McKenzie, D.C.; Lloyd-Smith, D.R.; Zumbo, B.D. A prospective study of running injuries: The Vancouver Sun Run “In Training” clinics. Br. J. Sports Med. 2003, 37, 239–244. [Google Scholar] [CrossRef] [PubMed]
- Van Gent, R.N.; Siem, D.; Van Middelkoop, M.; Van Os, A.G.; Bierma-Zeinstra, S.M.A.; Koes, B.W. Incidence and determinants of lower extremity running injuries in long distance runners: A systematic review. Br. J. Sports Med. 2007, 41, 469–480. [Google Scholar] [CrossRef] [PubMed]
- Dempster, J.; Dutheil, F.; Ugbolue, U.C. The prevalence of lower extremity injuries in running and associated risk factors: A systematic review. Phys. Act. Health 2021, 5, 133–145. [Google Scholar] [CrossRef]
- van Poppel, D.; van der Worp, M.; Slabbekoorn, A.; van den Heuvel, S.S.P.; van Middelkoop, M.; Koes, B.W.; Verhagen, A.P.; Scholten-Peeters, G.G. Risk factors for overuse injuries in short- and long-distance running: A systematic review. J. Sport Health Sci. 2021, 10, 14–28. [Google Scholar] [CrossRef]
- Van Middelkoop, M.; Kolkman, J.; Van Ochten, J.; Bierma-Zeinstra, S.M.A.; Koes, B. Prevalence and incidence of lower extremity injuries in male marathon runners. Scand. J. Med. Sci. Sports 2008, 18, 140–144. [Google Scholar] [CrossRef]
- van Poppel, D.; Scholten-Peeters, G.G.M.; van Middelkoop, M.; Verhagen, A.P. Prevalence, incidence and course of lower extremity injuries in runners during a 12-month follow-up period. Scand. J. Med. Sci. Sports 2014, 24, 943–949. [Google Scholar] [CrossRef]
- Karp, J.R. Training characteristics of qualifiers for the U.S. Olympic Marathon Trials. Int. J. Sports Physiol. Perform. 2007, 2, 72–92. [Google Scholar] [CrossRef]
- Tenforde, A.; Hoenig, T.; Saxena, A.; Hollander, K. Bone stress injuries in runners using carbon fiber plate footwear. Sports Med. 2023, 53, 1499–1505. [Google Scholar] [CrossRef]
- Clark, M.; Lucett, S.; Sutton, B. (Eds.) NASM Essentials of Corrective Exercise Training; Jones & Bartlett Learning: Burlington, MA, USA, 2014. [Google Scholar]
- Lauersen, J.B.; Bertelsen, D.M.; Andersen, L.B. The effectiveness of exercise interventions to prevent sports injuries: A systematic review and meta-analysis of randomised controlled trials. Br. J. Sports Med. 2014, 48, 871–877. [Google Scholar] [CrossRef] [PubMed]
- Leppänen, M.; Aaltonen, S.; Parkkari, J.; Heinonen, A.; Kujala, U.M. Interventions to prevent sports related injuries: A systematic review and meta-analysis of randomised controlled trials. Sports Med. 2014, 44, 473–486. [Google Scholar] [CrossRef] [PubMed]
| Variable | All | Female | Male |
|---|---|---|---|
| Total | 616 (100%) | 473 (76.8%) | 143 (23.2%) |
| Age (y) | 42.3 ± 10.5 | 42.3 ± 10.1 | 42.3 ± 11.8 |
| BMI (kg∙m−2) | 23.6 ± 3.6 | 23.3 ± 3.7 | 24.9 ± 3.2 *** |
| Education | |||
| High school or equivalent | 29 (4.7%) | 14 (3%) | 15 (10.5%) ** |
| Trade/technical | 20 (3.2%) | 15 (3.2%) | 5 (3.5%) |
| Associates | 22 (3.6%) | 14 (3%) | 8 (5.6%) |
| Bachelors | 202 (32.8%) | 155 (32.8%) | 47 (32.9%) |
| Masters/doctorate | 342 (55.5%) | 275 (58.1%) | 67 (46.9%) |
| Community | |||
| Urban | 130 (21.1%) | 97 (20.5%) | 33 (23.1%) |
| Suburban | 374 (60.7%) | 295 (62.4%) | 79 (55.2%) |
| Rural | 111 (18%) | 81 (17.1%) | 30 (21%) |
| Race | |||
| Asian/Pacific Islander | 12 (1.9%) | 7 (1.5%) | 5 (3.5%) |
| Black/African American | 5 (0.8%) | 5 (1.1%) | - |
| Native American/Alaskan | 1 (0.2%) | - | 1 (0.7%) |
| White/Caucasian | 565 (91.7%) | 436 (92.2%) | 129 (90.2%) |
| Bi- or multi-racial | 13 (2.1%) | 10 (2.1%) | 3 (2.1%) |
| Other | 19 (3.1%) | 14 (3.0%) | 5 (3.5%) |
| Run experience (y) | 12.8 ± 9.6 | 13.3 ± 9.6 * | 11.3 ± 9.7 |
| Frequency (d/wk) | 3.95 ± 1.3 | 3.9 ± 1.2 | 4.3 ± 1.4 ** |
| Weekly distance (miles) | |||
| ≤19 | 298 (48.4%) | 242 (51.2%) | 56 (39.2%) |
| >19 | 318 (51.6%) | 231 (48.8%) | 87 (60.8%) * |
| Weekly duration (h) | |||
| 1–2 | 79 (12.8%) | 60 (12.7%) | 19 (13.3%) |
| 3–4 | 22 8 (37%) | 186 (39.3%) | 42 (29.4%) |
| 5–6 | 18 1 (29.4%) | 136 (28.8%) | 45 (31.5%) |
| 7+ | 128 (20.8%) | 91 (19.2%) | 37 (25.9%) |
| Variable | Category (n) | History of RRI | RRI in the Past Year |
|---|---|---|---|
| Total (n = 616) | 520 (84.4%) | 275 (44.6%) | |
| Sex | F (n = 473) | 398 (84.1%) | 202 (42.7%) |
| M (n = 143) | 122 (85.3%) | 73 (51.0%) | |
| p | 0.74 | 0.08 | |
| Age | 18–34 (n = 144) | 120 (83.3%) | 71 (49.3%) |
| 35–50 (n = 327) | 277 (84.7%) | 140 (42.8%) | |
| 51–65 (n = 145) | 123 (84.8%) | 64 (44.1%) | |
| p | 0.92 | 0.42 | |
| Run (miles/wk) | <19 (n = 298) | 250 (83.9%) | 121 (40.6%) |
| 19+ (n = 318) | 270 (84.9%) | 154 (48.4%) * | |
| p | 0.73 | 0.05 |
| RRI in Past Year | p | RRI Severity | p | ||||
|---|---|---|---|---|---|---|---|
| Yes | No | Mild | Moderate | Major | |||
| All | 0.49 | 0.13 | |||||
| Yes | 195 (45.6%) | 233 (54.4%) | 57 (29.2%) | 73 (37.4%) | 65 (33.3%) | ||
| No | 80 (42.6%) | 108 (57.4%) | 30 (37.5%) | 20 (25.0%) | 30 (37.5%) | ||
| Sex | |||||||
| Female | 0.08 | 0.37 | |||||
| Yes | 156 (45.1%) | 190 (54.9%) | 47 (30.1%) | 61 (39.1%) | 48 (30.8%) | ||
| No | 46 (36.2%) | 81 (63.8%) | 15 (32.6%) | 13 (28.3%) | 18 (39.1%) | ||
| Male | 0.33 | 0.24 | |||||
| Yes | 39 (47.6%) | 43 (52.4%) | 10 (25.6%) | 12 (30.8%) | 17 (43.6%) | ||
| No | 34 (55.7%) | 27 (44.3%) | 15 (44.1%) | 7 (20.6%) | 12 (35.3%) | ||
| Age | |||||||
| 18–34 | |||||||
| Yes | 51 (50.0%) | 51 (50.0%) | 0.80 | 14 (27.5%) | 14 (27.5%) | 23 (45.1%) | 0.33 |
| No | 20 (47.6%) | 22 (52.4%) | 9 (45.0%) | 5 (25.0%) | 6 (30.0%) | ||
| 35–50 | |||||||
| Yes | 98 (43.2%) | 129 (56.8%) | 0.84 | 32 (32.7%) | 36 (36.7%) | 30 (30.6%) | 0.03 |
| No | 42 (42.0%) | 58 (58.0%) | 18 (42.9%) | 6 (14.3%) * | 18 (42.9%) | ||
| 51–65 | |||||||
| Yes | 46 (46.5%) | 53 (53.5%) | 0.41 | 11 (23.9%) | 23 (50.0%) | 12 (26.1%) | 0.76 |
| No | 18 (39.1%) | 28 (60.9%) | 3 (16.7%) | 9 (50.0%) | 6 (33.3%) | ||
| Run Distance (miles) | |||||||
| ≤19 | |||||||
| Yes | 89 (41.8%) | 124 (58.2%) | 0.51 | 31 (34.8%) | 36 (40.4%) | 22 (24.7%) | 0.06 |
| No | 32 (37.6%) | 53 (62.4%) | 9 (28.1%) | 8 (25.0%) | 15 (46.9%) | ||
| >19 miles | |||||||
| Yes | 106 (57.3%) | 79 (42.7%) | 0.65 | 26 (24.5%) | 37 (34.9%) | 43 (40.6%) | 0.06 |
| No | 48 (49.3%) | 55 (53.4%) | 21 (43.8%) | 12 (25.0%) | 15 (31.3%) | ||
| Characteristics | RRI in Past Year | p | |
|---|---|---|---|
| Yes (n = 195) | No (n = 233) | ||
| RT experience (y) | 8.6 ± 9.1 | 9.5 ± 9.0 | 0.32 |
| RT frequency (d/wk) | 2.6 ± 1.2 | 2.5 ± 1.1 | 0.44 |
| RT min/session | 30–44 (72, 44.7%) | 30–44 (89, 55.3%) | 0.62 |
| Repetition range | 7–12 (128, 46.4%) | 7–12 (148, 53.6%) | 0.99 |
| Effort level (0–10) | 6.2 ± 1.4 | 6.2 ± 1.4 | 0.66 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stenerson, L.R.; Melton, B.F.; Bland, H.W.; Ryan, G.A. Running-Related Overuse Injuries and Their Relationship with Run and Resistance Training Characteristics in Adult Recreational Runners: A Cross-Sectional Study. J. Funct. Morphol. Kinesiol. 2023, 8, 128. https://doi.org/10.3390/jfmk8030128
Stenerson LR, Melton BF, Bland HW, Ryan GA. Running-Related Overuse Injuries and Their Relationship with Run and Resistance Training Characteristics in Adult Recreational Runners: A Cross-Sectional Study. Journal of Functional Morphology and Kinesiology. 2023; 8(3):128. https://doi.org/10.3390/jfmk8030128
Chicago/Turabian StyleStenerson, Lea R., Bridget F. Melton, Helen W. Bland, and Greg A. Ryan. 2023. "Running-Related Overuse Injuries and Their Relationship with Run and Resistance Training Characteristics in Adult Recreational Runners: A Cross-Sectional Study" Journal of Functional Morphology and Kinesiology 8, no. 3: 128. https://doi.org/10.3390/jfmk8030128
APA StyleStenerson, L. R., Melton, B. F., Bland, H. W., & Ryan, G. A. (2023). Running-Related Overuse Injuries and Their Relationship with Run and Resistance Training Characteristics in Adult Recreational Runners: A Cross-Sectional Study. Journal of Functional Morphology and Kinesiology, 8(3), 128. https://doi.org/10.3390/jfmk8030128






