Net Heart Rate for Estimating Oxygen Consumption in Active Adults
Abstract
1. Introduction
2. Materials and Methods
2.1. Global Study Design
2.2. Subjects and Samples
2.3. Data Collection
2.4. Resting Heart Rate and Resting Oxygen Consumption
2.5. Treadmill Protocol
2.6. Cyclo-Ergometer Protocol
2.7. StepTest4all Protocol
2.8. Statistical Analysis
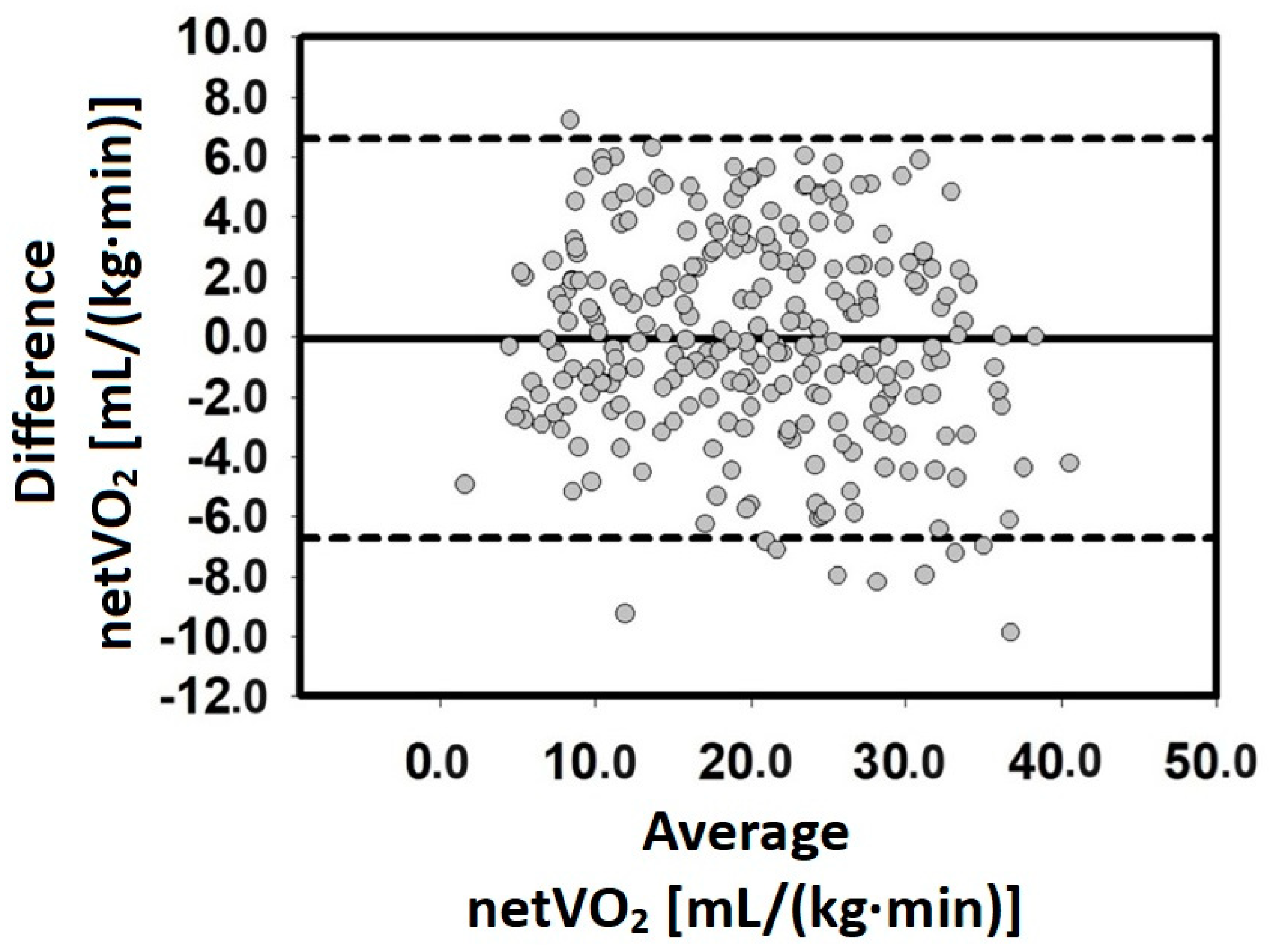
3. Results
4. Discussion
5. Conclusions
6. Practical Applications
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- McArdle, W.D.; Katch, F.I.; Katch, V.L. Exercise Physiology: Nutrition, Energy, and Human Performance, 8th ed.; Wolters Kluwer Health/Lippincott Williams & Wilkins: Philadelphia, MA, USA, 2015; ISBN 978-1-4511-9155-4. [Google Scholar]
- Hanson, N.J.; Scheadler, C.M.; Katsavelis, D.; Miller, M.G. Validity of the Wattbike 3-Minute Aerobic Test: Measurement and Estimation of Vo2max. J. Strength Cond. Res. 2022, 36, 400–404. [Google Scholar] [CrossRef] [PubMed]
- Voutilainen, A.; Setti, M.O.; Tuomainen, T.-P. Estimating Maximal Oxygen Uptake from the Ratio of Heart Rate at Maximal Exercise to Heart Rate at Rest in Middle-Aged Men. World J. Mens Health 2021, 39, 666. [Google Scholar] [CrossRef]
- Colosio, A.L.; Pedrinolla, A.; Da Lozzo, G.; Pogliaghi, S. Heart Rate-Index Estimates Oxygen Uptake, Energy Expenditure and Aerobic Fitness in Rugby Players. J. Sports Sci. Med. 2018, 17, 633–639. [Google Scholar] [PubMed]
- Marsh, C.E. Evaluation of the American College of Sports Medicine Submaximal Treadmill Running Test for Predicting VO2max. J. Strength Cond. Res. 2012, 26, 548–554. [Google Scholar] [CrossRef] [PubMed]
- Fudge, B.W.; Wilson, J.; Easton, C.; Irwin, L.; Clark, J.; Haddow, O.; Kayser, B.; Pitsiladis, Y.P. Estimation of Oxygen Uptake during Fast Running Using Accelerometry and Heart Rate. Med. Sci. Sports Exerc. 2007, 39, 192–198. [Google Scholar] [CrossRef] [PubMed]
- ACSM. Guidelines for Exercise Testing and Prescription, 10th ed.; LWW: Philadelphia, PA, USA, 2018. [Google Scholar]
- Lach, J.; Wiecha, S.; Sliz, D.; Price, S.; Zaborski, M.; Cieslinski, I.; Postula, M.; Knechtle, B.; Mamcarz, A. HR Max Prediction Based on Age, Body Composition, Fitness Level, Testing Modality and Sex in Physically Active Population. Front. Physiol. 2021, 12, 695950. [Google Scholar] [CrossRef] [PubMed]
- Andrews, R.B. Net Heart Rate as a Substitute for Respiratory Calorimetry. Am. J. Clin. Nutr. 1971, 24, 1139–1147. [Google Scholar] [CrossRef] [PubMed]
- Bragada, J.A.; Pedro, P.M.; Vasques, C.S.; Tiago, M.B.; Vitor, P.L. Net Heart Rate to Prescribe Physical Activity in Middle-Aged to Older Active Adults. J. Sports Sci. Med. 2009, 8, 616–621. [Google Scholar] [PubMed]
- Lin, S.-Y.; Lai, Y.-C.; Hsia, C.-C.; Su, P.-F.; Chang, C.-H. Validation of Energy Expenditure Prediction Models Using Real-Time Shoe-Based Motion Detectors. IEEE Trans. Biomed. Eng. 2017, 64, 2152–2162. [Google Scholar] [CrossRef] [PubMed]
- Gill, P.K.; Kipp, S.; Beck, O.N.; Kram, R. It Is Time to Abandon Single-Value Oxygen Uptake Energy Equivalents. J. Appl. Physiol. 2023, 134, 887–890. [Google Scholar] [CrossRef]
- Schantz, P.; Salier Eriksson, J.; Rosdahl, H. The Heart Rate Method for Estimating Oxygen Uptake: Analyses of Reproducibility Using a Range of Heart Rates from Cycle Commuting. PLoS ONE 2019, 14, e0219741. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, H.S.; Nakamura, F.Y.; Papoti, M.; da Silva, A.S.; Dos-Santos, J.W. Relationship Between Heart Rate, Oxygen Consumption, and Energy Expenditure in Futsal. Front. Psychol. 2021, 12, 698622. [Google Scholar] [CrossRef] [PubMed]
- Chevance, G.; Golaszewski, N.M.; Tipton, E.; Hekler, E.B.; Buman, M.; Welk, G.J.; Patrick, K.; Godino, J.G. Accuracy and Precision of Energy Expenditure, Heart Rate, and Steps Measured by Combined-Sensing Fitbits Against Reference Measures: Systematic Review and Meta-Analysis. JMIR Mhealth Uhealth 2022, 10, e35626. [Google Scholar] [CrossRef] [PubMed]
- Olson, M.S.; Williford, H.N.; Blessing, D.L.; Wilson, G.D.; Halpin, G. A Test to Estimate VO2max in Females Using Aerobic Dance, Heart Rate, BMI, and Age. J. Sports Med. Phys. Fitness 1995, 35, 159–168. [Google Scholar]
- Hansen, D.; Jacobs, N.; Thijs, H.; Dendale, P.; Claes, N. Validation of a Single-Stage Fixed-Rate Step Test for the Prediction of Maximal Oxygen Uptake in Healthy Adults. Clin. Physiol. Funct. Imaging 2016, 36, 401–406. [Google Scholar] [CrossRef]
- Tanaka, H.; Monahan, K.D.; Seals, D.R. Age-Predicted Maximal Heart Rate Revisited. J. Am. Coll. Cardiol. 2001, 37, 153–156. [Google Scholar] [CrossRef] [PubMed]
- Bragada, J.A.; Bartolomeu, R.F.; Rodrigues, P.M.; Magalhaes, P.M.; Bragada, J.P.; Morais, J.E. Validation of StepTest4all for Assessing Cardiovascular Capacity in Young Adults. Int. J. Environ. Res. Public Health 2022, 19, 11274. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, W.G. A Scale of Magnitude for Effect Statistics. In A New View of Statistics; Will, G., Ed.; Hopkins: Melbourne, Australia, 2002; p. 50. [Google Scholar]
- Martin Bland, J.; Altman, D.G. Statistical Methods for Assessing Agreement between Two Methods of Clinical Measurement. Lancet 1986, 327, 307–310. [Google Scholar] [CrossRef]
- Jensen, M.M.; Poulsen, M.K.; Alldieck, T.; Larsen, R.G.; Gade, R.; Moeslund, T.B.; Franch, J. Estimation of Energy Expenditure during Treadmill Exercise via Thermal Imaging. Med. Sci. Sports Exerc. 2016, 48, 2571–2579. [Google Scholar] [CrossRef][Green Version]
- Moon, J.; Oh, M.; Kim, S.; Lee, K.; Lee, J.; Song, Y.; Jeon, J.Y. Intelligent Estimation of Exercise Induced Energy Expenditure Including Excess Post-Exercise Oxygen Consumption (EPOC) with Different Exercise Intensity. Sensors 2023, 23, 9235. [Google Scholar] [CrossRef]
- Taboni, A.; Vinetti, G.; Piva, S.; Gorghelli, G.; Ferretti, G.; Fagoni, N. Comparison of Resting Energy Expenditure Measured with Metabolic Cart and Calculated with Predictive Formulas in Critically Ill Patients on Mechanical Ventilation. Respir. Physiol. Neurobiol. 2023, 311, 104025. [Google Scholar] [CrossRef]
- Looney, D.P.; Santee, W.R.; Hansen, E.O.; Bonventre, P.J.; Chalmers, C.R.; Potter, A.W. Estimating Energy Expenditure during Level, Uphill, and Downhill Walking. Med. Sci. Sports Exerc. 2019, 51, 1954–1960. [Google Scholar] [CrossRef]
- Hongu, N.; Orr, B.J.; Roe, D.J.; Reed, R.G.; Going, S.B. Global Positioning System Watches for Estimating Energy Expenditure. J. Strength Cond. Res. 2013, 27, 3216–3220. [Google Scholar] [CrossRef]
- Wickham, J.B.; Mullen, N.J.; Whyte, D.G.; Cannon, J. Comparison of Energy Expenditure and Heart Rate Responses between Three Commercial Group Fitness Classes. J. Sci. Med. Sport 2017, 20, 667–671. [Google Scholar] [CrossRef] [PubMed]
- Tikkanen, O.; Kärkkäinen, S.; Haakana, P.; Kallinen, M.; Pullinen, T.; Finni, T. EMG, Heart Rate, and Accelerometer as Estimators of Energy Expenditure in Locomotion. Med. Sci. Sports Exerc. 2014, 46, 1831–1839. [Google Scholar] [CrossRef] [PubMed]
- Kortelainen, L.; Helske, J.; Finni, T.; Mehtatalo, L.; Tikkanen, O.; Karkkainen, S. A Nonlinear Mixed Model Approach to Predict Energy Expenditure from Heart Rate. Physiol. Meas. 2021, 42, abea25. [Google Scholar] [CrossRef]
- Rotstein, A.; Meckel, Y. Estimation of %VO2 Reserve from Heart Rate during Arm Exercise and Running. Eur. J. Appl. Physiol. 2000, 83, 545–550. [Google Scholar] [CrossRef]
- Achten, J.; Jeukendrup, A.E. Heart Rate Monitoring: Applications and Limitations. Sports Med. 2003, 33, 517–538. [Google Scholar] [CrossRef] [PubMed]
- Sommerfeldt, S.L.; Schaefer, S.M.; Brauer, M.; Ryff, C.D.; Davidson, R.J. Individual Differences in the Association Between Subjective Stress and Heart Rate Are Related to Psychological and Physical Well-Being. Psychol. Sci. 2019, 30, 1016–1029. [Google Scholar] [CrossRef]
- Toohey, K.; Pumpa, K.L.; Arnolda, L.; Cooke, J.; Yip, D.; Craft, P.S.; Semple, S. A Pilot Study Examining the Effects of Low-Volume High-Intensity Interval Training and Continuous Low to Moderate Intensity Training on Quality of Life, Functional Capacity and Cardiovascular Risk Factors in Cancer Survivors. PeerJ 2016, 4, e2613. [Google Scholar] [CrossRef]
- De Carvalho, M.R.P.; Sato, E.I.; Tebexreni, A.S.; Heidecher, R.T.C.; Schenkman, S.; Neto, T.L.B. Effects of Supervised Cardiovascular Training Program on Exercise Tolerance, Aerobic Capacity, and Quality of Life in Patients with Systemic Lupus Erythematosus. Arthritis Rheum. 2005, 53, 838–844. [Google Scholar] [CrossRef] [PubMed]
- Müller, M.J.; Enderle, J.; Bosy-Westphal, A. Changes in Energy Expenditure with Weight Gain and Weight Loss in Humans. Curr. Obes. Rep. 2016, 5, 413–423. [Google Scholar] [CrossRef] [PubMed]
- Çekici, H.; Acar Tek, N. Determining Energy Requirement and Evaluating Energy Expenditure in Neurological Diseases. Nutr. Neurosci. 2020, 23, 543–553. [Google Scholar] [CrossRef] [PubMed]

| N | Minimum | Maximum | Mean | SD | |
|---|---|---|---|---|---|
| Age [years] | 156 | 18 | 81.0 | 42.0 | 20.7 |
| Body mass [kg] | 156 | 47.8 | 116.0 | 73.1 | 11.7 |
| Height [cm] | 156 | 138 | 190 | 169 | 11 |
| BMI [kg/m2] | 156 | 17.7 | 44.3 | 25.9 | 4.3 |
| HRrest [bpm] | 156 | 49 | 110 | 68 | 11 |
| VO2rest [mL/(kg·min)] | 156 | 1.2 | 6.4 | 3.2 | 0.9 |
| Group | Mean | SD | t-Test (p-Value) | |
|---|---|---|---|---|
| Age [years] | 1 (n = 79) 2 (n = 77) | 41.6 42.3 | 20.4 21.1 | −0.20 (0.841) |
| Body mass [kg] | 1 (n = 79) 2 (n = 77) | 73.5 72.8 | 11.6 11.8 | 0.360 (0.719) |
| Height [cm] | 1 (n = 79) 2 (n = 77) | 169 167 | 12 11 | 0.535 (0.593) |
| BMI [kg/m2] | 1 (n = 79) 2 (n = 77) | 25.8 26.0 | 4.0 4.7 | −0.186 (0.853) |
| HRrest [bpm] | 1 (n = 79) 2 (n = 77) | 69 67 | 11 11 | 0.464 (0.644) |
| VO2rest [mL/(kg·min)] | 1 (n = 79) 2 (n = 77) | 3.3 3.2 | 1.0 0.8 | 0.227 (0.821) |
| Measured netVO2 [mL/(kg·min)] | Estimated netVO2 [mL/(kg·min)] | |||
|---|---|---|---|---|
| Mean ± 1SD | Mean ± 1SD | Mean Difference (95% CI) | t-Test (p-Value) | d [Descriptor] |
| 20.09 ± 8.91 | 20.29 ± 8.41 | 0.0568 (−0.36 to 0.47) | 0.27 (0.788) | 0.01 [trivial] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bragada, J.A.; Magalhães, P.M.; São-Pedro, E.; Bartolomeu, R.F.; Morais, J.E. Net Heart Rate for Estimating Oxygen Consumption in Active Adults. J. Funct. Morphol. Kinesiol. 2024, 9, 66. https://doi.org/10.3390/jfmk9020066
Bragada JA, Magalhães PM, São-Pedro E, Bartolomeu RF, Morais JE. Net Heart Rate for Estimating Oxygen Consumption in Active Adults. Journal of Functional Morphology and Kinesiology. 2024; 9(2):66. https://doi.org/10.3390/jfmk9020066
Chicago/Turabian StyleBragada, José A., Pedro M. Magalhães, Eric São-Pedro, Raul F. Bartolomeu, and Jorge E. Morais. 2024. "Net Heart Rate for Estimating Oxygen Consumption in Active Adults" Journal of Functional Morphology and Kinesiology 9, no. 2: 66. https://doi.org/10.3390/jfmk9020066
APA StyleBragada, J. A., Magalhães, P. M., São-Pedro, E., Bartolomeu, R. F., & Morais, J. E. (2024). Net Heart Rate for Estimating Oxygen Consumption in Active Adults. Journal of Functional Morphology and Kinesiology, 9(2), 66. https://doi.org/10.3390/jfmk9020066










