Seminar Lessons: Infectious Diseases Associated with and Causing Disaster
Abstract
:1. Introduction
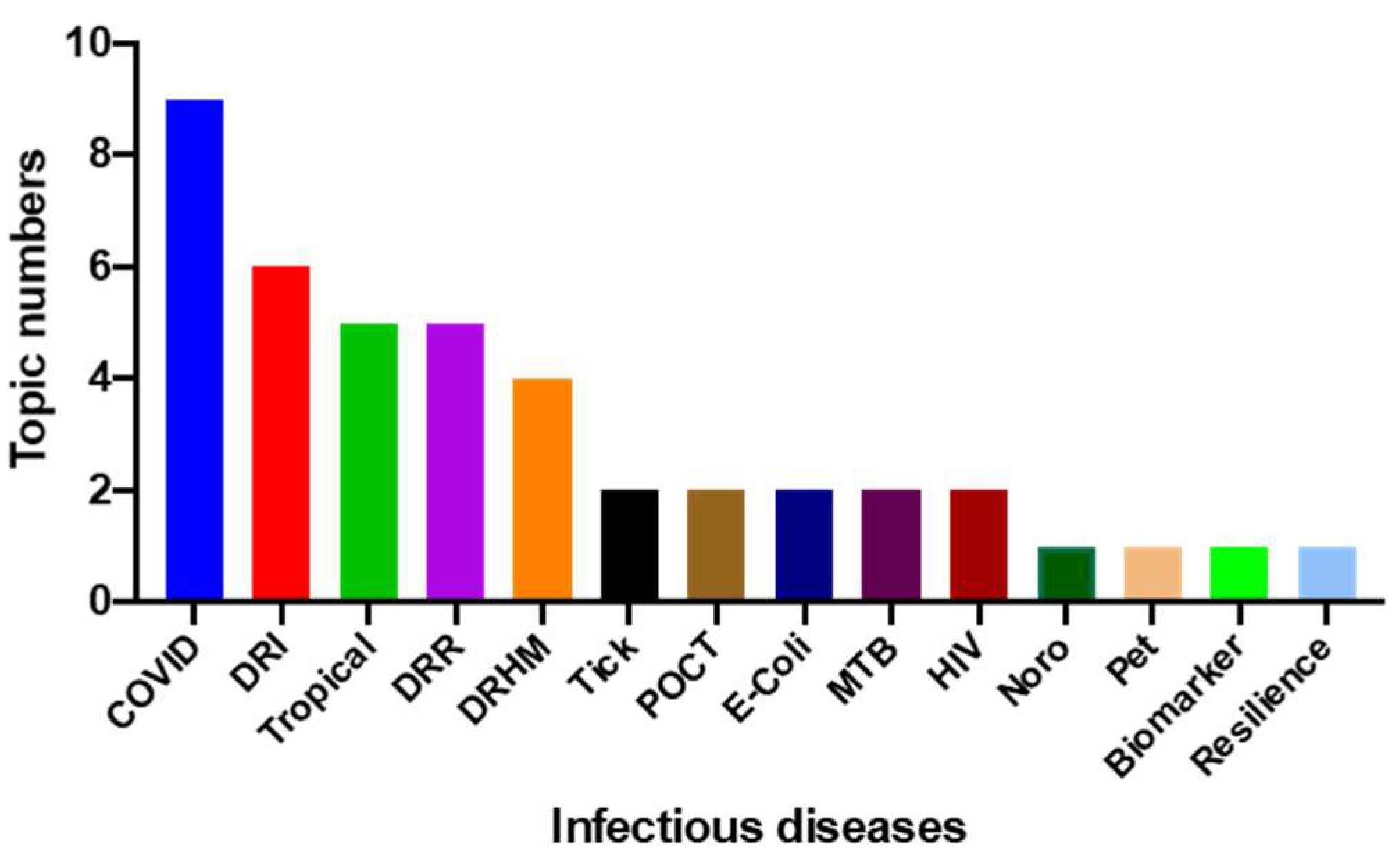
2. Content of Seminars
3. Disaster-Related Infectious Diseases
3.1. Leptospirosis
3.2. Tick-Borne Disorders
3.3. Mosquito-Borne Disorders
4. COVID-19 Caused a Disaster
5. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| JBCL | Japan Biosciences Co., Ltd.; (Sendai, Miyagi, Japan) |
| U. | University |
| IRIDeS | International Research Institute of Disaster Science; (Tohoku University, Sendai, Miyagi, Japan) |
| SMU | Sapporo Medical University; (Sapporo, Hokkaido, Japan) |
| SGH | Shizuoka General Hospital; (Shizuoka, Shizuoka, Japan) |
| SSH | Saiseikai Shizuoka Hospital; (Shizuoka, Shizuoka, Japan) |
| NCGM | National Center for Global Health and Medicine;(Tokyo, Japan) |
| SCHC | Shizuoka City Health Center; (Shizuoka, Shizuoka, Japan) |
| SSK | Saiseikai Kumamoto Hospital; (Kumamoto, Kumamoto, Japan) |
| TBA | Tohoku Bio-Array Co., Ltd.; (Sendai, Miyagi, Japan) |
| NIID | National Institute for Infectious Disease; (Tokyo, Japan) |
| KIUI | Kibi International University; (Takahashi, Okayama, Japan) |
| CMDS | Crisis Management Department Shizuoka; (Shizuoka, Shizuoka, Japan) |
| NIES | National Institute for Environmental Studies;(Tsukuba, Ibaragi, Japan) |
| KHSU | Kumamoto Health Science University; (Kumamoto, Kumamoto, Japan) |
| ShCH | Shizuoka City Hospital; (Shizuoka, Shizuoka, Japan) |
| IMS | The Institute of Medical Science;(Tokyo, Japan) |
| NMC | Nagoya Medical Center; (Nagoya, Aichi, Japan) |
| OGMC | Osaka General Medical Center; (Osaka, Osaka, Japan) |
| SDCH | Sendai City Hospital; (Sendai, Miyagi, Japan) |
| E. coli | Esherichia coli |
| DRI | Disaster related infectious diseases |
| DRR | Disaster risk reduction |
| Tropical | Tropical infectious diseases |
| DRHM | Disaster risk health management |
| MTB | Mycobacterium tuberculosis |
| HIV | Human immunodeficiency virus |
| POCT | Point of care test |
| Tick | Tick-borne diseases |
| Pet infection | Pet-derived infectious diseases |
| COVID-19 | Coronavirus Disease in 2019 |
References
- Center for Research on the Epidemiology of Disasters, Natural Disaster 2019. Available online: https://landsliderisk.wordpress.com/2020/08/28/cred-report-natural-disasters-2019/ (accessed on 30 December 2021).
- Hattori, T.; Chagan-Yasutan, H.; Shiratori, B.; Egawa, S.; Izumi, T.; Kubo, T.; Nakajima, C.; Suzuki, Y.; Niki, T.; Alisjahbana, B.; et al. Development of Point-of-Care Testing for Disaster-Related Infectious Diseases. Tohoku J. Exp. Med. 2016, 238, 287–293. [Google Scholar] [CrossRef] [Green Version]
- Ministry of Land, Infrastructure, Transport and Tourism. Overview of Nankai Trough Mega Earthquake Operation Plan; MLITT: Tokyo, Japan, 2021.
- UNDRR. Sendai Framework for Disaster Risk Reduction 2015–2030; UNDRR: Geneva, Switzerland, 2016. [Google Scholar]
- Torgerson, P.; Hagan, J.; Costa, F.; Calcagno, J.; Kane, M.; Martinez-Silveira, M.S.; Goris, M.G.A.; Stein, C.; Ko, A.; Abela-Ridder, B. Global Burden of Leptospirosis: Estimated in Terms of Disability Adjusted Life Years. PLoS Negl. Trop. Dis. 2015, 9, e0004122. [Google Scholar] [CrossRef] [Green Version]
- Sumi, A.; Telan, E.F.O.; Chagan-Yasutan, H.; Piolo, M.B.; Hattori, T.; Kobayashi, N. Effect of temperature, relative humidity and rainfall on dengue fever and leptospirosis infections in Manila, the Philippines. Epidemiol. Infect. 2017, 145, 78–86. [Google Scholar] [CrossRef] [Green Version]
- Furin, J.; Mathew, T. Tuberculosis Control in Acute Disaster Settings: Case Studies from the 2010 Haiti Earthquake. Disaster Med. Public Health Prep. 2013, 7, 129–130. [Google Scholar] [CrossRef]
- Koenig, S.P.; Rouzier, V.; Vilbrun, S.C.; Morose, W.; Collins, S.E.; Joseph, P.; Decome, D.; Ocheretina, O.; Galbaud, S.; Hashiguchi, L.; et al. Tuberculosis in the aftermath of the 2010 earthquake in Haiti. Bull. World Health Organ. 2015, 93, 498–502. [Google Scholar] [CrossRef]
- Chagan-Yasutan, H.; Ndhlovu, L.; Lacuesta, T.L.; Kubo, T.; Leano, P.S.A.; Niki, T.; Oguma, S.; Morita, K.; Chew, G.M.; Barbour, J.D.; et al. Galectin-9 plasma levels reflect adverse hematological and immunological features in acute dengue virus infection. J. Clin. Virol. 2013, 58, 635–640. [Google Scholar] [CrossRef] [Green Version]
- Phetsuksiri, B.; Rudeeaneksin, J.; Srisungngam, S.; Bunchoo, S.; Roienthong, D.; Mukai, T.; Nakajima, C.; Hamada, S.; Suzuki, Y. Applicability of In-House Loop-Mediated Isothermal Amplification for Rapid Identification of Mycobacterium tuberculosis Complex Grown on Solid Media. Jpn. J. Infect. Dis. 2013, 66, 249–251. [Google Scholar] [CrossRef] [Green Version]
- Liles, V.R.; Pangilinan, L.-A.S.; Daroy, M.L.G.; Dimamay, M.T.A.; Reyes, R.S.; Bulusan, M.K.; Dimamay, M.P.S.; Luna, P.A.S.; Mercado, A.; Bai, G.; et al. Evaluation of a rapid diagnostic test for detection of dengue infection using a single-tag hybridization chromatographic-printed array strip format. Eur. J. Clin. Microbiol. 2019, 38, 515–521. [Google Scholar] [CrossRef]
- Mitsuhashi, S.; Kryukov, K.; Nakagawa, S.; Takeuchi, J.S.; Shiraishi, Y.; Asano, K.; Imanishi, T. A portable system for rapid bacterial composition analysis using a nanopore-based sequencer and laptop computer. Sci. Rep. 2017, 7, 5657. [Google Scholar] [CrossRef]
- The 2012 National Antenatal Sentinel HIV & Herpes Simplex Type-2 Prevalence Survey in South Africa; Directorate Epidemiology Cluster, HIMME National Department of Health: Pretoria, South Africa, 2013.
- Hu, B.; Guo, H.; Zhou, P.; Shi, Z.-L. Characteristics of SARS-CoV-2 and COVID-19. Nat. Rev. Microbiol. 2021, 19, 141–154. [Google Scholar] [CrossRef]
- Nations United. Human Development Report 1994; Oxford University Press: Oxford, UK, 1994. [Google Scholar]
- Fatehpanah, A.; Jahangiri, K.; Seyedin, S.H.; Kavousi, A.; Malekinezhad, H. Water safety in drought: An indigenous knowledge-based qualitative study. J. Water Health 2020, 18, 692–703. [Google Scholar] [CrossRef]
- McKinnon, J. Community culture: Strengthening persistence to empower resistance. In Living at the Edge of Thai Society; Routledge: Oxfordshire, UK, 2003; pp. 64–85. [Google Scholar]
- Kato, A.; Nakamura, K.; Hiyama, Y. The 2016 Kumamoto earthquake sequence. Proc. Jpn. Acad. Ser. B 2016, 92, 358–371. [Google Scholar] [CrossRef] [Green Version]
- Yee, E.L.; Palacio, H.; Atmar, R.L.; Shah, U.; Kilborn, C.; Faul, M.; Gavagan, T.E.; Feigin, R.D.; Versalovic, J.; Neill, F.H.; et al. Widespread Outbreak of Norovirus Gastroenteritis among Evacuees of Hurricane Katrina Residing in a Large “Megashelter” in Houston, Texas: Lessons Learned for Prevention. Clin. Infect. Dis. 2007, 44, 1032–1039. [Google Scholar] [CrossRef] [Green Version]
- Harada, T.; Hiroi, M.; Kawamori, F.; Furusawa, A.; Ohata, K.; Sugiyama, K.; Masuda, T. A food poisoning diarrhea outbreak caused by enteroaggregative Escherichia coli serogroup O126:H27 in Shizuoka, Japan. Jpn. J. Infect. Dis. 2007, 60, 154–155. [Google Scholar]
- Pascapurnama, D.N.; Murakami, A.; Chagan-Yasutan, H.; Hattori, T.; Sasaki, H.; Egawa, S. Prevention of Tetanus Outbreak Following Natural Disaster in Indonesia: Lessons Learned from Previous Disasters. Tohoku J. Exp. Med. 2016, 238, 219–227. [Google Scholar] [CrossRef] [Green Version]
- Luo, T.; Sumi, A.; Zhou, D.; Kobayashi, N.; Mise, K.; Yu, B.; Kong, D.; Wang, J.; Duan, Q. Seasonality of reported tuberculosis cases from 2006 to 2010 in Wuhan, China. Epidemiol. Infect. 2014, 142, 2036–2048. [Google Scholar] [CrossRef]
- Dembele, B.P.P.; Chagan-Yasutan, H.; Niki, T.; Ashino, Y.; Tangpukdee, N.; Shinichi, E.; Krudsood, S.; Kano, S.; Hattori, T. Plasma levels of Galectin-9 reflect disease severity in malaria infection. Malar. J. 2016, 15, 408. [Google Scholar] [CrossRef] [Green Version]
- Chagan-Yasutan, H.; Hanan, F.; Niki, T.; Bai, G.; Ashino, Y.; Egawa, S.; Telan, E.F.O.; Hattori, T. Plasma Osteopontin Levels is Associated with Biochemical Markers of Kidney Injury in Patients with Leptospirosis. Diagnostics 2020, 10, 439. [Google Scholar] [CrossRef]
- Mori, K.; Lee, H.T.; Rapoport, D.; Drexler, I.R.; Foster, K.; Yang, J.; Schmidt-Ott, K.M.; Chen, X.; Li, J.Y.; Weiss, S.; et al. Endocytic delivery of lipocalin-siderophore-iron complex rescues the kidney from ischemia-reperfusion injury. J. Clin. Investig. 2005, 115, 610–621. [Google Scholar] [CrossRef]
- Mori, K.; Mori, N. Diagnosis of AKI: Clinical Assessment, Novel Biomarkers, History, and Perspectives. Acute Kidney Inj. Regen. Med. 2020, 47–58. [Google Scholar] [CrossRef]
- Saitoh, H.; Koizumi, N.; Seto, J.; Ajitsu, S.; Fujii, A.; Takasaki, S.; Yamakage, S.; Aoki, S.; Nakayama, K.; Ashino, Y.; et al. Leptospirosis in the Tohoku Region: Re-emerging Infectious Disease. Tohoku J. Exp. Med. 2015, 236, 33–37. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Villanueva, S.Y.A.; Saito, M.; Tsutsumi, Y.; Segawa, T.; Baterna, R.A.; Chakraborty, A.; Asoh, T.; Miyahara, S.; Yanagihara, Y.; Cavinta, L.L.; et al. High virulence in hamsters of four dominant Leptospira serovars isolated from rats in the Philippines. Microbiology 2014, 160, 418–428. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saito, M.; Miyahara, S.; Villanueva, S.Y.A.M.; Aramaki, N.; Ikejiri, M.; Kobayashi, Y.; Guevarra, J.P.; Masuzawa, T.; Gloriani, N.G.; Yanagihara, Y.; et al. PCR and Culture Identification of Pathogenic Leptospira spp. from Coastal Soil in Leyte, Philippines, after a Storm Surge during Super Typhoon Haiyan (Yolanda). Appl. Environ. Microbiol. 2014, 80, 6926–6932. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kawamura, R. Studies on tsutsugamushi disease (Japanese flood fever). Med Bull. Coll. Med. Univ. Cincinnati 1926, 4, 217–222. [Google Scholar]
- Dittrich, S.; Rattanavong, S.; Lee, S.J.; Panyanivong, P.; Craig, S.B.; Tulsiani, S.M.; Blacksell, S.; Dance, D.; Dubot-Pérès, A.; Sengduangphachanh, A.; et al. Orientia, rickettsia, and leptospira pathogens as causes of CNS infections in Laos: A prospective study. Lancet Glob. Health 2015, 3, e104–e112. [Google Scholar] [CrossRef]
- Marx, G.E.; Spillane, M.; Beck, A.; Stein, Z.; Powell, A.K.; Hinckley, A.F. Emergency Department Visits for Tick Bites–United States, January 2017–December 2019. MMWR. Morb. Mortal. Wkly. Rep. 2021, 70, 612–616. [Google Scholar] [CrossRef]
- Krause, P.; Fish, D.; Narasimhan, S.; Barbour, A. Borrelia miyamotoi infection in nature and in humans. Clin. Microbiol. Infect. 2015, 21, 631–639. [Google Scholar] [CrossRef] [Green Version]
- Platonov, A.E.; Karan, L.S.; Kolyasnikova, N.M.; Makhneva, N.A.; Toporkova, M.G.; Maleev, V.V.; Fish, D.; Krause, P.J. Humans Infected with Relapsing Fever SpirocheteBorrelia miyamotoi, Russia. Emerg. Infect. Dis. 2011, 17, 1816–1823. [Google Scholar] [CrossRef]
- Eisen, R.J.; Paddock, C.D. Tick and Tickborne Pathogen Surveillance as a Public Health Tool in the United States. J. Med. Èntomol. 2021, 58, 1490–1502. [Google Scholar] [CrossRef]
- Charnley, G.E.C.; Kelman, I.; Gaythorpe, K.; Murray, K. Understanding the risks for post-disaster infectious disease outbreaks: A systematic review protocol. BMJ Open 2020, 10, e039608. [Google Scholar] [CrossRef]
- Boyce, R.M.; Hollingsworth, B.D.; Baguma, E.; Xu, E.; Goel, V.; Brown-Marusiak, A.; Muhindo, R.; Reyes, R.; Ntaro, M.; Siedner, M.J.; et al. Dihydroartemisinin-Piperaquine Chemoprevention and Malaria Incidence After Severe Flooding: Evaluation of a Pragmatic Intervention in Rural Uganda. Clin. Infect. Dis. 2021. [Google Scholar] [CrossRef] [PubMed]
- Singh, M.K.; Neog, Y. Contagion effect ofCOVID-19 outbreak: Another recipe for disaster on Indian economy. J. Public Aff. 2020, 2171. [Google Scholar] [CrossRef] [PubMed]
- Ellison, E.C.; Shabahang, M.M. COVID-19 Pandemic and the Need for Disaster Planning in Surgical Education. J. Am. Coll. Surg. 2021, 232, 135–137. [Google Scholar] [CrossRef]
- Kirwan, R.; McCullough, D.; Butler, T.; De Heredia, F.P.; Davies, I.G.; Stewart, C. Sarcopenia during COVID-19 lockdown restrictions: Long-term health effects of short-term muscle loss. GeroScience 2020, 42, 1547–1578. [Google Scholar] [CrossRef]
- Miyasaka, M. COVID-19 and immunity: Quo vadis? Int. Immunol. 2021, 33, 507–513. [Google Scholar] [CrossRef]
- Kamikubo, Y.; Takahashi, A. Epidemic trends of SARS-CoV-2 modulated by economic activity, ethnicity, and vaccination. Camb. Open Engag. 2021. Available online: https://researchmap.jp/read0146204/published_papers/31864267 (accessed on 30 December 2021).
- Sugiyama, T.; Gursel, M.; Takeshita, F.; Coban, C.; Conover, J.; Kaisho, T.; Akira, S.; Klinman, D.M.; Ishii, K.J. CpG RNA: Identification of Novel Single-Stranded RNA That Stimulates Human CD14+CD11c+Monocytes. J. Immunol. 2005, 174, 2273–2279. [Google Scholar] [CrossRef] [Green Version]
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Pérez Marc, G.; Moreira, E.D.; Zerbini, C.; et al. Safety and efficacy of the BNT162b2 mRNA COVID-19 vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef]
- Zekavat, S.M.; Lin, S.-H.; Bick, A.G.; Liu, A.; Paruchuri, K.; Wang, C.; Uddin, M.; Ye, Y.; Yu, Z.; Liu, X.; et al. Hematopoietic mosaic chromosomal alterations increase the risk for diverse types of infection. Nat. Med. 2021, 27, 1012–1024. [Google Scholar] [CrossRef]
- Tajima, Y.; Suda, Y.; Yano, K. A case report of SARS-CoV-2 confirmed in saliva specimens up to 37 days after onset: Proposal of saliva specimens for COVID-19 diagnosis and virus monitoring. J. Infect. Chemother. 2020, 26, 1086–1089. [Google Scholar] [CrossRef]
- Ashino, Y.; Chagan-Yasutan, H.; Hatta, M.; Shirato, Y.; Kyogoku, Y.; Komuro, H.; Hattori, T. Successful Treatment of a COVID-19 Case with Pneumonia and Renal Injury Using Tocilizumab. Reports 2020, 3, 29. [Google Scholar] [CrossRef]
- Bai, G.; Furushima, D.; Niki, T.; Matsuba, T.; Maeda, Y.; Takahashi, A.; Hattori, T.; Ashino, Y. High Levels of the Cleaved Form of Galectin-9 and Osteopontin in the Plasma Are Associated with Inflammatory Markers That Reflect the Severity of COVID-19 Pneumonia. Int. J. Mol. Sci. 2021, 22, 4978. [Google Scholar] [CrossRef] [PubMed]
- Leaning, J.; Guha-Sapir, D. Natural Disasters, Armed Conflict, and Public Health. N. Engl. J. Med. 2013, 369, 1836–1842. [Google Scholar] [CrossRef] [PubMed]
- Crotty, S.; Cameron, C.E.; Andino, R. RNA virus error catastrophe: Direct molecular test by using ribavirin. Proc. Natl. Acad. Sci. USA 2001, 98, 6895–6900. [Google Scholar] [CrossRef] [Green Version]
- Shete, A.; Bichare, S.; Pujari, V.; Virkar, R.; Thakar, M.; Ghate, M.; Patil, S.; Vyakarnam, A.; Gangakhedkar, R.; Bai, G.; et al. Elevated Levels of Galectin-9 but Not Osteopontin in HIV and Tuberculosis Infections Indicate Their Roles in Detecting MTB Infection in HIV Infected Individuals. Front. Microbiol. 2020, 11, 1685. [Google Scholar] [CrossRef]
- Fischer, W.; Giorgi, E.E.; Chakraborty, S.; Nguyen, K.; Bhattarcharya, T.; Theiler, J.; Goloboff, P.A.; Yoon, H.; Abfalterer, W.; Foley, B.T.; et al. HIV-1 and SARS-CoV-2: Patterns in the evolution of two pandemic pathogens. Cell Host Microbe 2021, 29, 1093–1110. [Google Scholar] [CrossRef]
- Callaway, E. Beyond Omicron: What’s next for COVID’s viral evolution. Nature 2021, 600, 204–207. [Google Scholar] [CrossRef]
- Iwasaki-Hozumi, H.; Chagan-Yasutan, H.; Ashino, Y.; Hattori, T. Blood Levels of Galectin-9, an Immuno-Regulating Molecule, Reflect the Severity for the Acute and Chronic Infectious Diseases. Biomolecules 2021, 11, 430. [Google Scholar] [CrossRef]
- Hattori, T.; Iwasaki-Hozumi, H.; Bai, G.; Chagan-Yasutan, H.; Shete, A.; Telan, E.F.; Takahashi, A.; Ashino, Y.; Matsuba, T. Both Full-Length and Protease-Cleaved Products of Osteopontin Are Elevated in Infectious Diseases. Biomedicine 2021, 9, 1006. [Google Scholar] [CrossRef]

| No. | Date | Speaker | Affiliation | Title | Classification |
|---|---|---|---|---|---|
| 1 | 24 February 2014 | Sato T | JBCL | Examination of digestive system required for disaster infectious diseases | E. coli |
| Koga S | U. Shizuoka | Disaster infectious diseases, after earthquakes and tsunamis | DRI | ||
| Hattori T | IRIDeS | Human security program against disasters and infectious diseases | DRR | ||
| 2 | 19 July 2014 | Sato T | JBCL | Examination of digestive system required for disaster infectious diseases | E. coli |
| C.-Y. H | IRIDeS | Disaster-related infectious diseases in the Philippines | Tropical | ||
| Ashino Y | Tohoku U. | Actual condition of HIV infections in the Tohoku region of Japan | HIV | ||
| Egawa S | IRIDeS | Medical response in the Great East Japan Earthquake | DRHM | ||
| 3 | 13 March 2015 | C.-Y. H | IRIDeS | Collaborative research on disaster-related infectious diseases with Philippines | Tropical |
| Sumi A | SMU | Seasonal tuberculosis epidemic | MTB | ||
| Ndhlovu LC | U. Hawaii | Consideration of the HIV epidemic during disaster related events | HIV | ||
| Hakamata Y | SGH | Preparation for disaster-related infectious diseases in Shizuoka Prefecture | DRI | ||
| Suzuki Y | Hokkaido U. | Tuberculosis as a disaster-related disorders | MTB | ||
| 4 | 4 July 2015 | Fukuoka T | SSH | Experience of outbreak of pathogenic Escherichia coli O157 | E. coli |
| Kutsuna K | NCGM | Dengue fever | Tropical | ||
| Kaji M | SCHC | About infectious disease measures in Shizuoka city | DRI | ||
| Yanagihara Y | U. Shizuoka | Floods and leptospirosis in the Philippines | Tropical | ||
| Egawa S | IRIDeS | Reports of the United Nations world conference on disaster risk reduction | DRR | ||
| 5 | 19 November 2016 | Nakayama Y | SKH | “Chain of survival” Kumamoto earthquake, crisis of life. | DRHM |
| C.-Y. H | IRIDeS | Actual conditions of mosquito-borne infectious diseases and its spreading | Tropical | ||
| Sato T | JBCL | Countermeasures against norovirus infection in the event of disaster | Norovirus | ||
| Kawase M | TBA | Development of new diagnostic method STH-PAS for infectious diseases | POCT | ||
| Koga S | U. Shizuoka | Current status and countermeasures for important tick-borne infectious diseases | Tick | ||
| 6 | 12 December 2017 | Suzuki Y | Hokkaido U. | Tuberculosis; never-ending threat | MTB |
| Kawamori F | U. Shizuoka | Tick-born infectious diseases in Shizuoka prefecture | Tick | ||
| Hakamata Y | SGH | Summary of pet infectious diseases of concern at evacuation center | Pet infection | ||
| Matsui T | NIID | Risk assessment method for infectious disease at evacuation center—to facilitate ‘common language’ between infection control specialists and public health sectors | DRHM | ||
| Iwata K | Shizuoka U. | From disaster mitigation to disaster prevention society | DRR | ||
| 7 | 1 December 2018 | Nakagawa S | Tokai U. | How to utilize the portable DNA/RNA sequencer MiniON for disaster medical care | POCT |
| Mori K | SGH | Kidney disease biomarkers in disaster infectious diseases | Biomarker | ||
| Kaji M | SCHC | Measures against infectious diseases in the event of a disaster | DRI | ||
| Hattori T | KIUI | Disaster measures learned from South East Asia | Resilience | ||
| Ueda T | CMDS | Earthquake and tsunami countermeasures in Shizuoka prefecture | DRR | ||
| 8 | 16 November 2019 | Goka K | NIES | Fire ants, ticks, mosquitoes--biological risks caused by environmental disturbances and globalization | DRI |
| Kawaguchi T | KHSU | Infection prevention and control during natural disaster: lessons learned from the Kumamoto Earthquake | DRI | ||
| Tosaka N | SGH | Repones of medical institutions in infectious disease crisis management | DRHM | ||
| Ueda T | CMDS | Shizuoka prefecture disaster prevention drill | DRR | ||
| 9 | 20 March 2021 | Miyasaka M | Osaka U. | What did we learn from a novel coronavirus infection? | COVID-19 |
| Takahashi A | KIUI | Japanese immune strategy and measures against medical collapse | COVID-19 | ||
| Yano K | HMC | About new coronavirus information from CDC | COVID-19 | ||
| Iwai K | ShCH | COVID-19 from the medical side | COVID-19 | ||
| 10 | 27 November 2021 | Ishii K | IMS | Disruptive innovation in vaccine development research advancing COVID-19 disaster | COVID-19 |
| Iwatani Y | NMC | Characteristics and mutations in SARS-CoV-2 | COVID-19 | ||
| Fujimi S | OGMC | Response of the critical care center in Osaka during the COVID-19 pandemic | COVID-19 | ||
| Ashino Y | SDCH | COVID-19 treatment recommendations from Sendai city hospital | COVID-19 | ||
| Terao C | SGH | Cloned cell proliferation and infection | COVID-19 |
| Classification (No.) and Pathogens | ||
|---|---|---|
| Virus infection (17) | RNA (14) | Human Immunodeficiency Virus (HIV); Coronavirus type 1, type 2; Middle east respiratory virus syndrome; Ebola virus; Dengue virus; Zika virus; Severe fever with thrombocytopenia syndrome virus; Rabies; Lyssavirus; Influenza virus; Norovirus; Hepatitis C virus; Measles virus; Rubella virus. |
| DNA (3) | Human papilloma virus; Hepatitis B virus; Varicella zoster virus; Chickenpox virus. | |
| Bacteria (8) | Mycobacterium tuberculosis; Escherichia coli; Clostridium tetani; Legionella; Leptospira spp.; Bartonella henselae; Coxiella burnetii; Chlamydia psittaci. | |
| Fungi (1) | Chytrid fungi | |
| Parasite (2) | Plasmodium falciparum Malaria; Trypanosoma cruzi; | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hattori, T.; Chagan-Yasutan, H.; Koga, S.; Yanagihara, Y.; Tanaka, I. Seminar Lessons: Infectious Diseases Associated with and Causing Disaster. Reports 2022, 5, 7. https://doi.org/10.3390/reports5010007
Hattori T, Chagan-Yasutan H, Koga S, Yanagihara Y, Tanaka I. Seminar Lessons: Infectious Diseases Associated with and Causing Disaster. Reports. 2022; 5(1):7. https://doi.org/10.3390/reports5010007
Chicago/Turabian StyleHattori, Toshio, Haorile Chagan-Yasutan, Shin Koga, Yasutake Yanagihara, and Issei Tanaka. 2022. "Seminar Lessons: Infectious Diseases Associated with and Causing Disaster" Reports 5, no. 1: 7. https://doi.org/10.3390/reports5010007
APA StyleHattori, T., Chagan-Yasutan, H., Koga, S., Yanagihara, Y., & Tanaka, I. (2022). Seminar Lessons: Infectious Diseases Associated with and Causing Disaster. Reports, 5(1), 7. https://doi.org/10.3390/reports5010007







