Wearable Light Loggers in Field Conditions: Corneal Light Characteristics, User Compliance, and Acceptance
Abstract
:1. Introduction
2. Results
2.1. Reasons for Not Wearing the Dosimeter
- Charging battery (5×);
- Wetness in the environment (9×);
- Public (14×);
- Pain from lido (9×);
- Sport (11×).
2.2. Feedback About the Usability of the Devices
- Many looks from others (18×);
- Interest of others (15×);
- Looks like a camera (14×);
- Imbalance (5×);
- Positive reactions from others (3×);
- Does not look good (2×);
- Glasses pinching (2×);
- You become accustomed to wearing it (1×);
- LED flashes too bright in the dark (1×);
- No reaction from strangers (1×);
- Awareness of personal light exposure (1×).
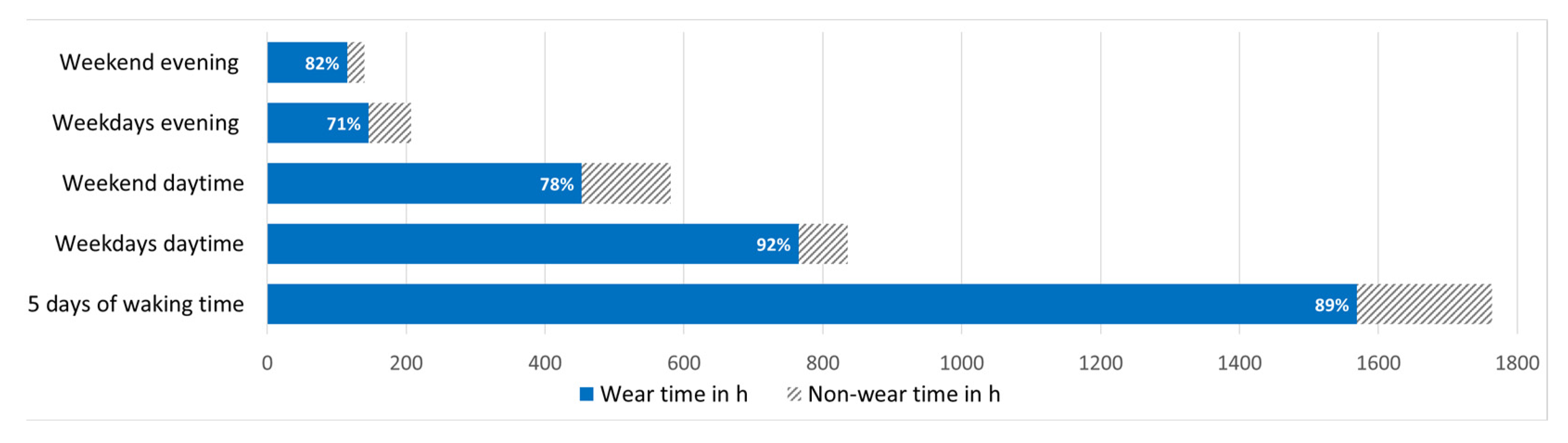
2.3. Recording Times and Wear Compliance
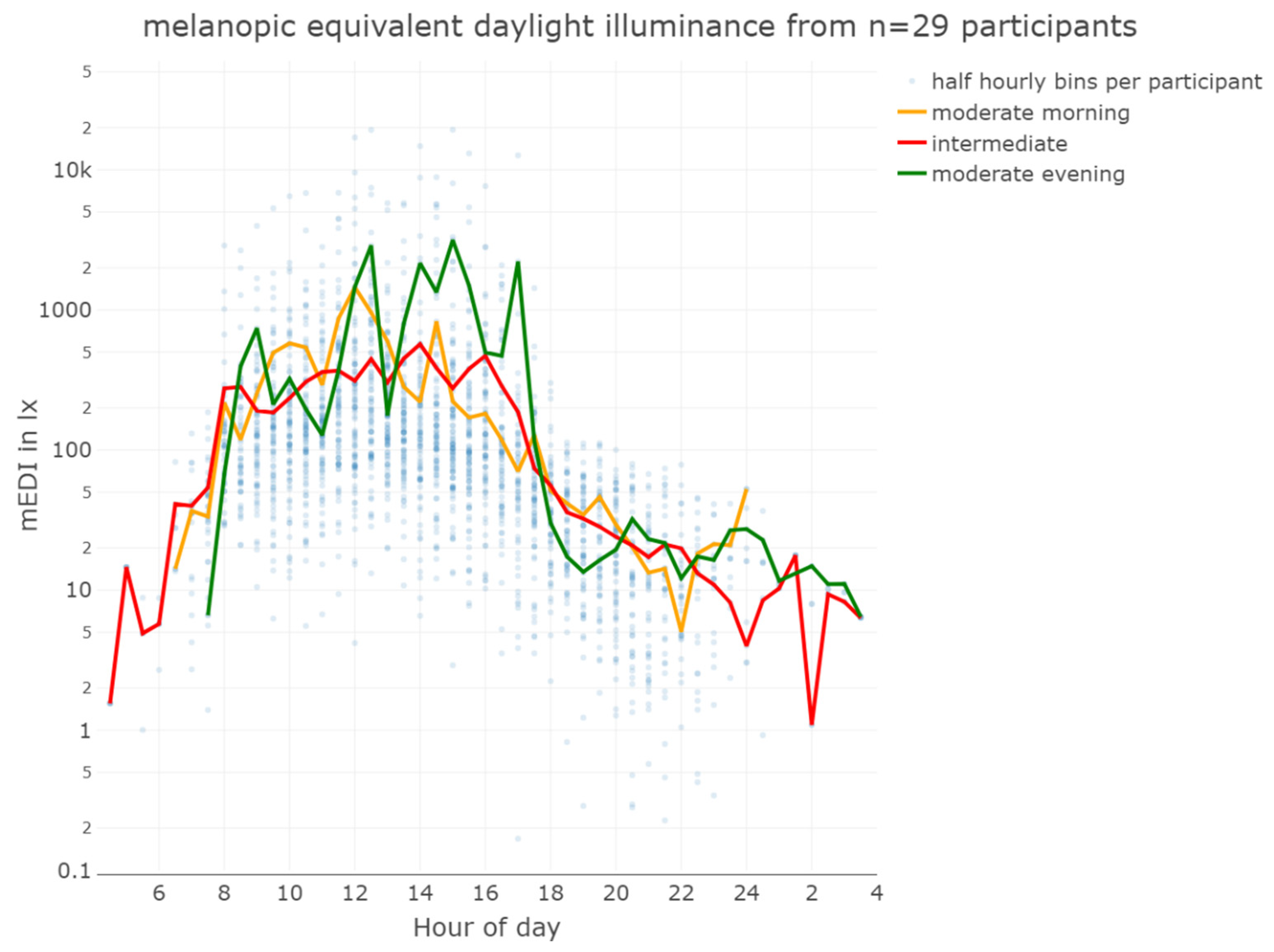
2.4. Light Characteristics Received by Subjects near the Plane of the Cornea
3. Discussion
4. Materials and Methods
4.1. Participants and Procedure
4.2. Instruments
- Please tell me when and where you mainly wore the lido.
- What activities did you do while you were carrying it?
- Aside from times when you slept and showered, how long did you not wear the lido when you could otherwise have worn it (time of the day)?
- What were the possible reasons for not wearing the lido, apart from the times when sleeping and showering?
- On which occasion did you find it particularly difficult to wear the lido?
- What experiences (your own experience and possibly also the reactions of other people) have you had while wearing the device? Please briefly describe your observations.
- When and where would you prefer to wear the lido?
4.3. Apparatus
4.4. Data Preprocessing
4.5. Statistics
5. Conclusions and Recommendations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Knoop, M.; Stefani, O.; Bueno, B.; Matusiak, B.; Hobday, R.; Wirz-Justice, A.; Martiny, K.; Kantermann, T.; Aarts, M.P.J.; Zemmouri, N.; et al. Daylight: What Makes the Difference? Light. Res. Technol. 2020, 52, 423–442. [Google Scholar] [CrossRef]
- DIN EN 12464-1:2021-11; Licht Und Beleuchtung_-Beleuchtung von Arbeitsstätten_-Teil_1: Arbeitsstätten in Innenräumen; Deutsche Fassung EN_12464-1:2021. DIN Media GmbH.: Berlin, Germany. [CrossRef]
- Boivin, D.B.; Duffy, J.F.; Kronauer, R.E.; Czeisler, C.A. Dose-Response Relationships for Resetting of Human Circadian Clock by Light. Nature 1996, 379, 540–542. [Google Scholar] [CrossRef] [PubMed]
- Khalsa, S.B.S.; Jewett, M.E.; Cajochen, C.; Czeisler, C.A. A Phase Response Curve to Single Bright Light Pulses in Human Subjects. J. Physiol. 2003, 549, 945–952. [Google Scholar] [CrossRef] [PubMed]
- Lewy, A.J. Effects of Light on Human Melatonin Production and the Human Circadian System. Prog. Neuropsychopharmacol. Biol. Psychiatry 1983, 7, 551–556. [Google Scholar] [CrossRef]
- St Hilaire, M.A.; Ámundadóttir, M.L.; Rahman, S.A.; Rajaratnam, S.M.W.; Rüger, M.; Brainard, G.C.; Czeisler, C.A.; Andersen, M.; Gooley, J.J.; Lockley, S.W. The Spectral Sensitivity of Human Circadian Phase Resetting and Melatonin Suppression to Light Changes Dynamically with Light Duration. Proc. Natl. Acad. Sci. USA 2022, 119, e2205301119. [Google Scholar] [CrossRef]
- Gubin, D.; Danilenko, K.; Stefani, O.; Kolomeichuk, S.; Markov, A.; Petrov, I.; Voronin, K.; Mezhakova, M.; Borisenkov, M.; Shigabaeva, A.; et al. Blue Light and Temperature Actigraphy Measures Predicting Metabolic Health Are Linked to Melatonin Receptor Polymorphism. Biology 2023, 13, 22. [Google Scholar] [CrossRef]
- Ishihara, A.; Courville, A.B.; Chen, K.Y. The Complex Effects of Light on Metabolism in Humans. Nutrients 2023, 15, 1391. [Google Scholar] [CrossRef]
- Cajochen, C.; Zeitzer, J.M.; Czeisler, C.A.; Dijk, D.J. Dose-Response Relationship for Light Intensity and Ocular and Electroencephalographic Correlates of Human Alertness. Behav. Brain Res. 2000, 115, 75–83. [Google Scholar] [CrossRef]
- Chellappa, S.L.; Steiner, R.; Blattner, P.; Oelhafen, P.; Götz, T.; Cajochen, C. Non-Visual Effects of Light on Melatonin, Alertness and Cognitive Performance: Can Blue-Enriched Light Keep Us Alert? PLoS ONE 2011, 6, e16429. [Google Scholar] [CrossRef]
- Milosavljevic, N. How Does Light Regulate Mood and Behavioral State? Clocks Sleep 2019, 1, 319–331. [Google Scholar] [CrossRef]
- Rahman, S.A.; Flynn-Evans, E.E.; Aeschbach, D.; Brainard, G.C.; Czeisler, C.A.; Lockley, S.W. Diurnal Spectral Sensitivity of the Acute Alerting Effects of Light. Sleep 2014, 37, 271–281. [Google Scholar] [CrossRef] [PubMed]
- Vandewalle, G.; Schwartz, S.; Grandjean, D.; Wuillaume, C.; Balteau, E.; Degueldre, C.; Schabus, M.; Phillips, C.; Luxen, A.; Dijk, D.J.; et al. Spectral Quality of Light Modulates Emotional Brain Responses in Humans. Proc. Natl. Acad. Sci. USA 2010, 107, 19549–19554. [Google Scholar] [CrossRef]
- Vandewalle, G.; Maquet, P.; Dijk, D.-J. Light as a Modulator of Cognitive Brain Function. Trends Cogn. Sci. 2009, 13, 429–438. [Google Scholar] [CrossRef]
- Zauner, J.; Plischke, H.; Stijnen, H.; Schwarz, U.T.; Strasburger, H. Influence of Common Lighting Conditions and Time-of-Day on the Effort-Related Cardiac Response. PLoS ONE 2020, 15, e0239553. [Google Scholar] [CrossRef] [PubMed]
- Münch, M.; Wirz-Justice, A.; Brown, S.A.; Kantermann, T.; Martiny, K.; Stefani, O.; Vetter, C.; Wright, K.P.; Wulff, K.; Skene, D.J. The Role of Daylight for Humans: Gaps in Current Knowledge. Clocks Sleep 2020, 2, 61–85. [Google Scholar] [CrossRef]
- Boubekri, M.; Cheung, I.N.; Reid, K.J.; Wang, C.-H.; Zee, P.C. Impact of Windows and Daylight Exposure on Overall Health and Sleep Quality of Office Workers: A Case-Control Pilot Study. J. Clin. Sleep Med. JCSM Off. Publ. Am. Acad. Sleep Med. 2014, 10, 603–611. [Google Scholar] [CrossRef] [PubMed]
- Figueiro, M.G.; Rea, M.S. Office Lighting and Personal Light Exposures in Two Seasons: Impact on Sleep and Mood. Light. Res. Technol. 2016, 48, 352–364. [Google Scholar] [CrossRef]
- Hubalek, S.; Brink, M.; Schierz, C. Office Workers’ Daily Exposure to Light and Its Influence on Sleep Quality and Mood. Light. Res. Technol. 2010, 42, 33–50. [Google Scholar] [CrossRef]
- Didikoglu, A.; Mohammadian, N.; Johnson, S.; van Tongeren, M.; Wright, P.; Casson, A.J.; Brown, T.M.; Lucas, R.J. Associations between Light Exposure and Sleep Timing and Sleepiness While Awake in a Sample of UK Adults in Everyday Life. Proc. Natl. Acad. Sci. USA 2023, 120, e2301608120. [Google Scholar] [CrossRef]
- CIE S 026 CIE S 026/E:2018 CIE System for Metrology of Optical Radiation for ipRGC-Influenced Responses to Light. Color Res. Appl. 2019, 44, 316. [CrossRef]
- Hartmeyer, S.L.; Webler, F.S.; Andersen, M. Towards a Framework for Light-Dosimetry Studies: Methodological Considerations. Light. Res. Technol. Lond. Engl. 2001 2022, 55, 377–399. [Google Scholar] [CrossRef]
- Spitschan, M.; Smolders, K.; Vandendriessche, B.; Bent, B.; Bakker, J.P.; Rodriguez-Chavez, I.R.; Vetter, C. Verification, Analytical Validation and Clinical Validation (V3) of Wearable Dosimeters and Light Loggers. Digit. Health 2022, 8, 20552076221144858. [Google Scholar] [CrossRef] [PubMed]
- Figueiro, M.G.; Hamner, R.; Bierman, A.; Rea, M.S. Comparisons of Three Practical Field Devices Used to Measure Personal Light Exposures and Activity Levels. Light. Res. Technol. 2013, 45, 421–434. [Google Scholar] [CrossRef] [PubMed]
- Bhandari, K.R.; Mirhajianmoghadam, H.; Ostrin, L.A. Wearable Sensors for Measurement of Viewing Behavior, Light Exposure, and Sleep. Sensors 2021, 21, 7096. [Google Scholar] [CrossRef] [PubMed]
- Stampfli, J.R.; Schrader, B.; Di Battista, C.; Häfliger, R.; Schälli, O.; Wichmann, G.; Zumbühl, C.; Blattner, P.; Cajochen, C.; Lazar, R.; et al. The Light-Dosimeter: A New Device to Help Advance Research on the Non-Visual Responses to Light. Light. Res. Technol. 2023, 55, 147715352211471. [Google Scholar] [CrossRef]
- Aarts, M.P.J.; van Duijnhoven, J.; Aries, M.B.C.; Rosemann, A.L.P. Performance of Personally Worn Dosimeters to Study Non-Image Forming Effects of Light: Assessment Methods. Build. Environ. 2017, 117, 60–72. [Google Scholar] [CrossRef]
- Balajadia, E.; Garcia, S.; Stampfli, J.; Schrader, B.; Guidolin, C.; Spitschan, M. Usability and Acceptability of a Corneal-Plane α-Opic Light Logger in a 24-h Field Trial. Digit. Biomark. 2023, 7, 139–149. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using Thematic Analysis in Psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Kelly, N.; Gilbert, S.B. The Wearer, the Device, and Its Use: Advances in Understanding the Social Acceptability of Wearables. Proc. Hum. Factors Ergon. Soc. Annu. Meet. 2018, 62, 1027–1031. [Google Scholar] [CrossRef]
- Kelly, N.; Gilbert, S. The WEAR Scale: Developing a Measure of the Social Acceptability of a Wearable Device. In Proceedings of the 2016 CHI Conference Extended Abstracts on Human Factors in Computing Systems, San Jose, CA, USA, 7–12 May 2016; Association for Computing Machinery: New York, NY, USA, 2016; pp. 2864–2871. [Google Scholar]
- Brown, T.M.; Brainard, G.C.; Cajochen, C.; Czeisler, C.A.; Hanifin, J.P.; Lockley, S.W.; Lucas, R.J.; Münch, M.; O’Hagan, J.B.; Peirson, S.N.; et al. Recommendations for Daytime, Evening, and Nighttime Indoor Light Exposure to Best Support Physiology, Sleep, and Wakefulness in Healthy Adults. PLOS Biol. 2022, 20, e3001571. [Google Scholar] [CrossRef]
- Wittmann, M.; Dinich, J.; Merrow, M.; Roenneberg, T. Social Jetlag: Misalignment of Biological and Social Time. Chronobiol. Int. 2006, 23, 497–509. [Google Scholar] [CrossRef]
- Scheuermaier, K.; Laffan, A.M.; Duffy, J.F. Light Exposure Patterns in Healthy Older and Young Adults. J. Biol. Rhythms 2010, 25, 113–122. [Google Scholar] [CrossRef]
- Guillemette, J.; Hébert, M.; Paquet, J.; Dumont, M. Natural Bright Light Exposure in the Summer and Winter in Subjects with and without Complaints of Seasonal Mood Variations. Biol. Psychiatry 1998, 44, 622–628. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.E.; Amritwar, A.; Hong, L.E.; Mohyuddin, I.; Brown, T.; Postolache, T.T. Daily and Seasonal Variation in Light Exposure among the Old Order Amish. Int. J. Environ. Res. Public. Health 2020, 17, 4460. [Google Scholar] [CrossRef]
- Thorne, H.C.; Jones, K.H.; Peters, S.P.; Archer, S.N.; Dijk, D.-J. Daily and Seasonal Variation in the Spectral Composition of Light Exposure in Humans. Chronobiol. Int. 2009, 26, 854–866. [Google Scholar] [CrossRef]
- Horne, J.A.; Ostberg, O. A Self-Assessment Questionnaire to Determine Morningness-Eveningness in Human Circadian Rhythms. Int. J. Chronobiol. 1976, 4, 97–110. [Google Scholar]
- Kelly, N. The WEAR Scale: Development of a Measure of the Social Acceptability of a Wearable Device. Ph.D. Thesis, Iowa State University, Digital Repository, Ames, IA, USA, 2016; p. 9199807. [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2014. [Google Scholar]
- CIE JTC 8 CIE S 017/E:2020; ILV: International Lighting Vocabulary, 2nd Edition 2020. Commission Internationale de L’Eclairage: Vienna, Austria, 2020.
- Brown, T.M. Melanopic Illuminance Defines the Magnitude of Human Circadian Light Responses under a Wide Range of Conditions. J. Pineal Res. 2020, 69, 12655. [Google Scholar] [CrossRef] [PubMed]
- Giménez, M.C.; Stefani, O.; Cajochen, C.; Lang, D.; Deuring, G.; Schlangen, L.J.M. Predicting Melatonin Suppression by Light in Humans: Unifying Photoreceptor-Based Equivalent Daylight Illuminances, Spectral Composition, Timing and Duration of Light Exposure. J. Pineal Res. 2022, 72, e12786. [Google Scholar] [CrossRef] [PubMed]
- Lucas, R.J.; Peirson, S.N.; Berson, D.M.; Brown, T.M.; Cooper, H.M.; Czeisler, C.A.; Figueiro, M.G.; Gamlin, P.D.; Lockley, S.W.; O’Hagan, J.B.; et al. Measuring and Using Light in the Melanopsin Age. Trends Neurosci. 2014, 37, 4. [Google Scholar] [CrossRef]
- Zauner, J.; Hartmeyer, S.; Spitschan, M. LightLogR: Reproducible analysis of personal light exposure data with an open-source R package. OSF Preprints 2024. [Google Scholar] [CrossRef]
- Hastie, T.; Tibshirani, R. Generalized Additive Models. Stat. Sci. 1986, 1, 297–310. [Google Scholar] [CrossRef]
- Wood, S.N. Generalized Additive Models: An Introduction with R, 2nd ed.; Chapman and Hall/CRC: New York, NY, USA, 2017; ISBN 978-1-315-37027-9. [Google Scholar] [CrossRef]
- Pedersen, E.J.; Miller, D.L.; Simpson, G.L.; Ross, N. Hierarchical Generalized Additive Models in Ecology: An Introduction with Mgcv. PeerJ 2019, 7, e6876. [Google Scholar] [CrossRef] [PubMed]
- Simpson, G.L. Modelling Palaeoecological Time Series Using Generalised Additive Models. Front. Ecol. Evol. 2018, 6, 149. [Google Scholar] [CrossRef]

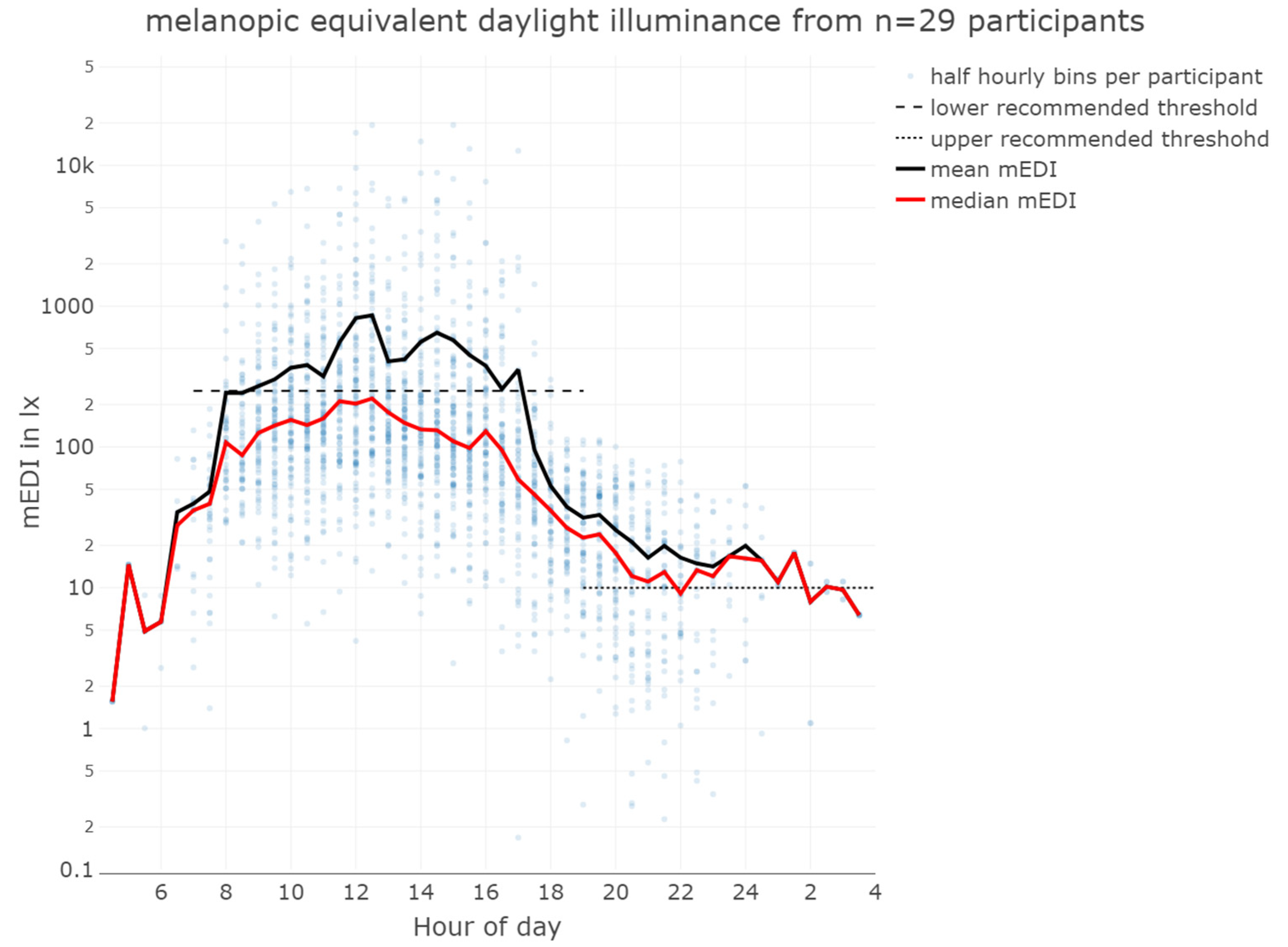
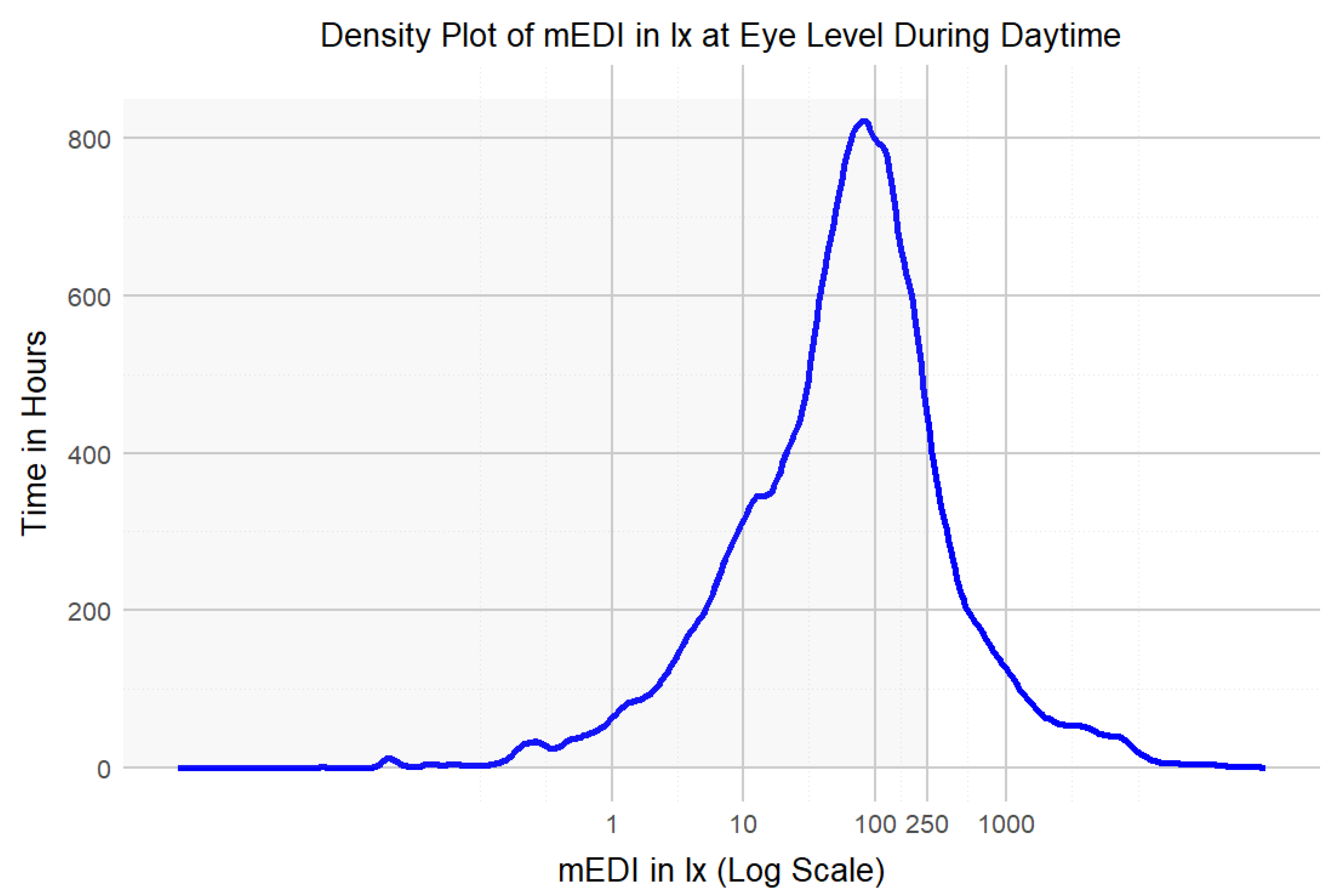


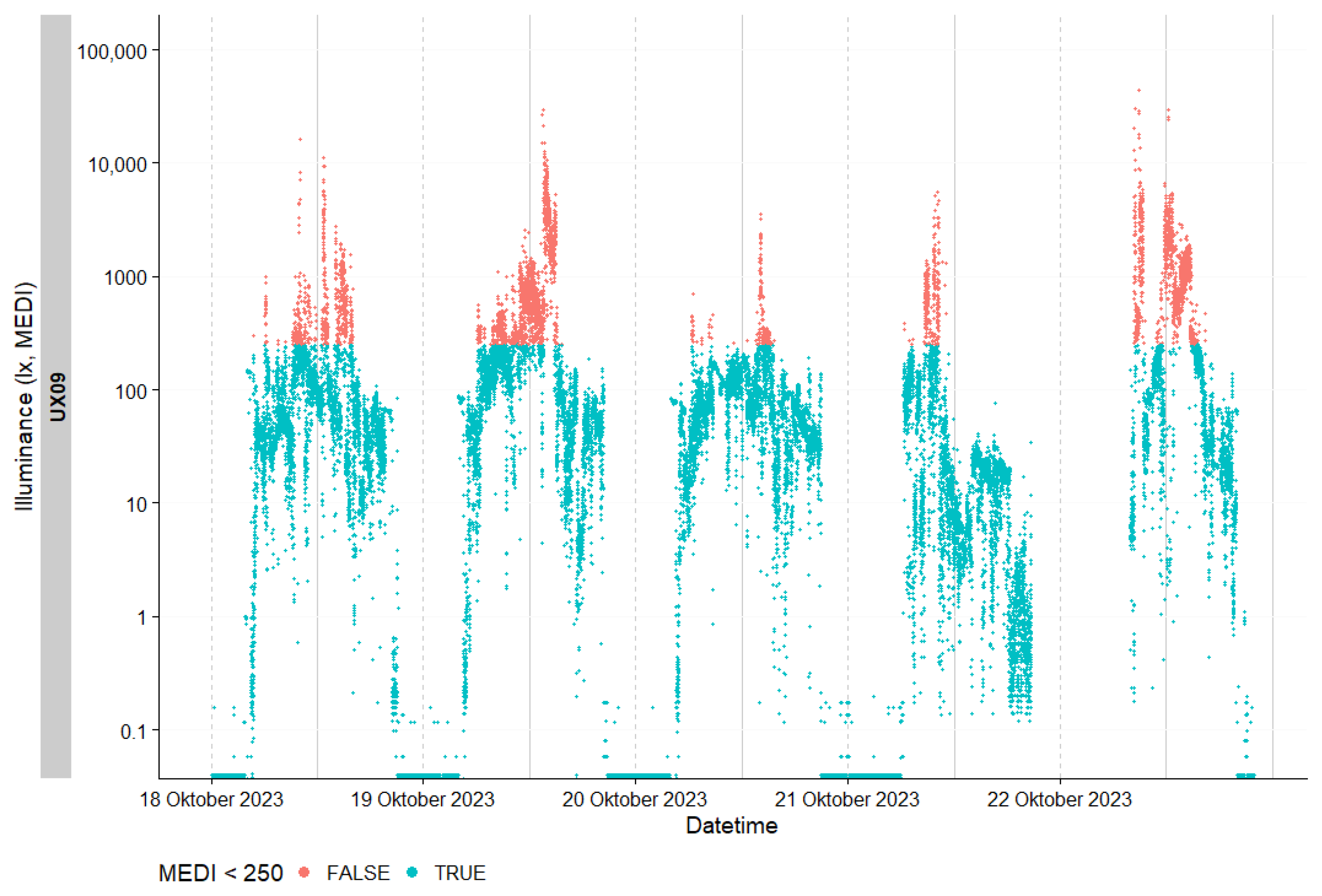
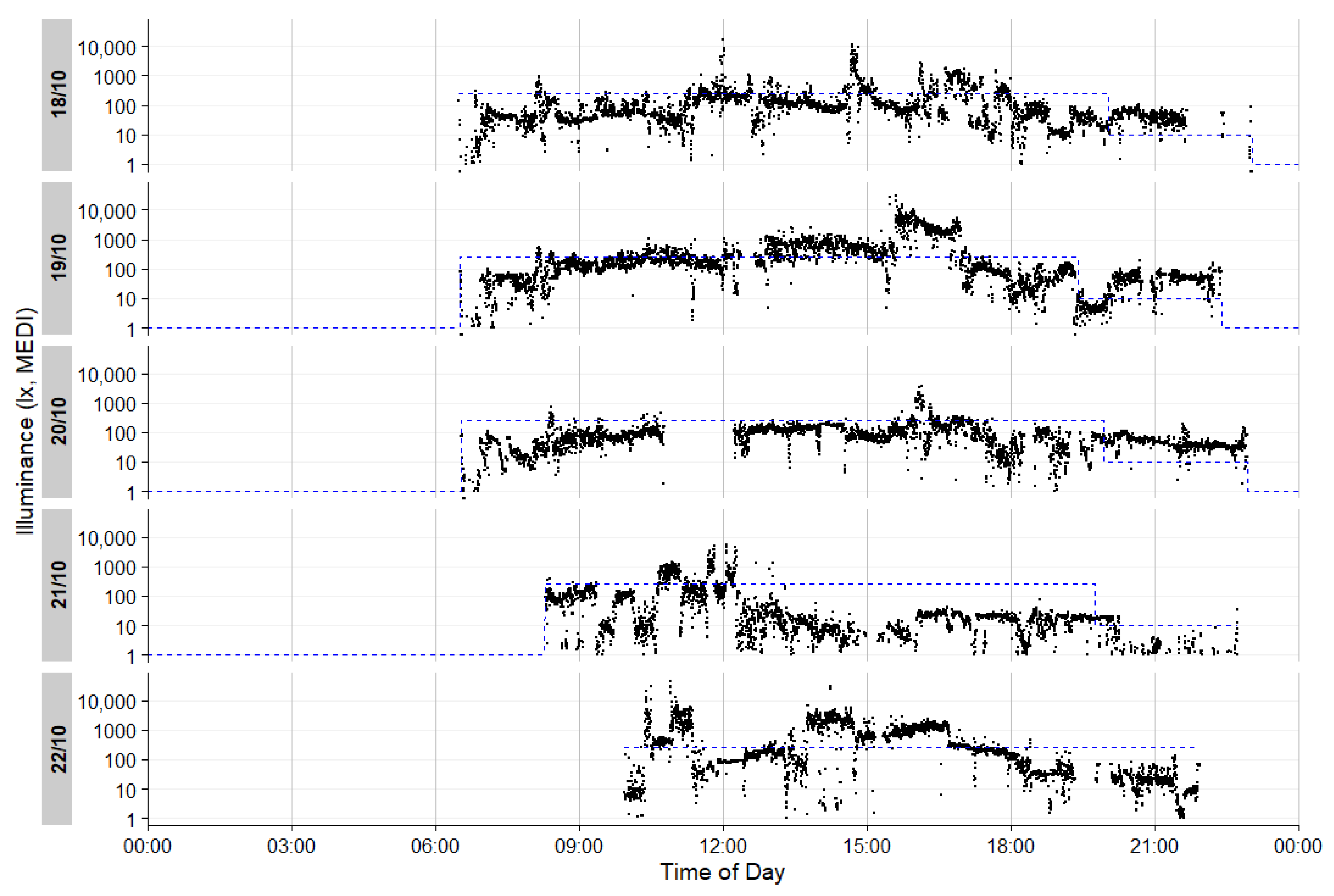
| mEDI in lx | Mean | Median | Minimum | 1st Quartile | 3rd Quartile | Maximum |
|---|---|---|---|---|---|---|
| daytime | 356 | 67 | 0 | 20 | 165 | 93,432 |
| evening | 32 | 7 | 0 | 2 | 22 | 19,376 |
| overall | 299 | 51 | 0 | 11 | 138 | 93,432 |
| Options | 5-Point Likert Scale | 6-Point Likert Scale | 7-Point Likert Scale |
|---|---|---|---|
| (current study) | (Kelly [31,39]) | (Balajadia et al. [28]) | |
| Strongly disagree | 1 | 1 | 1 |
| Disagree | 2 | 2 | 2 |
| Somewhat disagree | 3 | 3 | |
| Neither agree nor disagree | 3 | 4 | |
| Somewhat agree | 4 | 5 | |
| Agree | 4 | 5 | 6 |
| Strongly agree | 5 | 6 | 7 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stefani, O.; Marek, R.; Schwarz, J.; Plate, S.; Zauner, J.; Schrader, B. Wearable Light Loggers in Field Conditions: Corneal Light Characteristics, User Compliance, and Acceptance. Clocks & Sleep 2024, 6, 619-634. https://doi.org/10.3390/clockssleep6040042
Stefani O, Marek R, Schwarz J, Plate S, Zauner J, Schrader B. Wearable Light Loggers in Field Conditions: Corneal Light Characteristics, User Compliance, and Acceptance. Clocks & Sleep. 2024; 6(4):619-634. https://doi.org/10.3390/clockssleep6040042
Chicago/Turabian StyleStefani, Oliver, Reto Marek, Jürg Schwarz, Sina Plate, Johannes Zauner, and Björn Schrader. 2024. "Wearable Light Loggers in Field Conditions: Corneal Light Characteristics, User Compliance, and Acceptance" Clocks & Sleep 6, no. 4: 619-634. https://doi.org/10.3390/clockssleep6040042
APA StyleStefani, O., Marek, R., Schwarz, J., Plate, S., Zauner, J., & Schrader, B. (2024). Wearable Light Loggers in Field Conditions: Corneal Light Characteristics, User Compliance, and Acceptance. Clocks & Sleep, 6(4), 619-634. https://doi.org/10.3390/clockssleep6040042








