The Effect of the Incorporation of a 3D-Printed Titanium Framework on the Mechanical Properties CAD/CAM Denture Base Materials
Abstract
1. Introduction
2. Materials and Methods
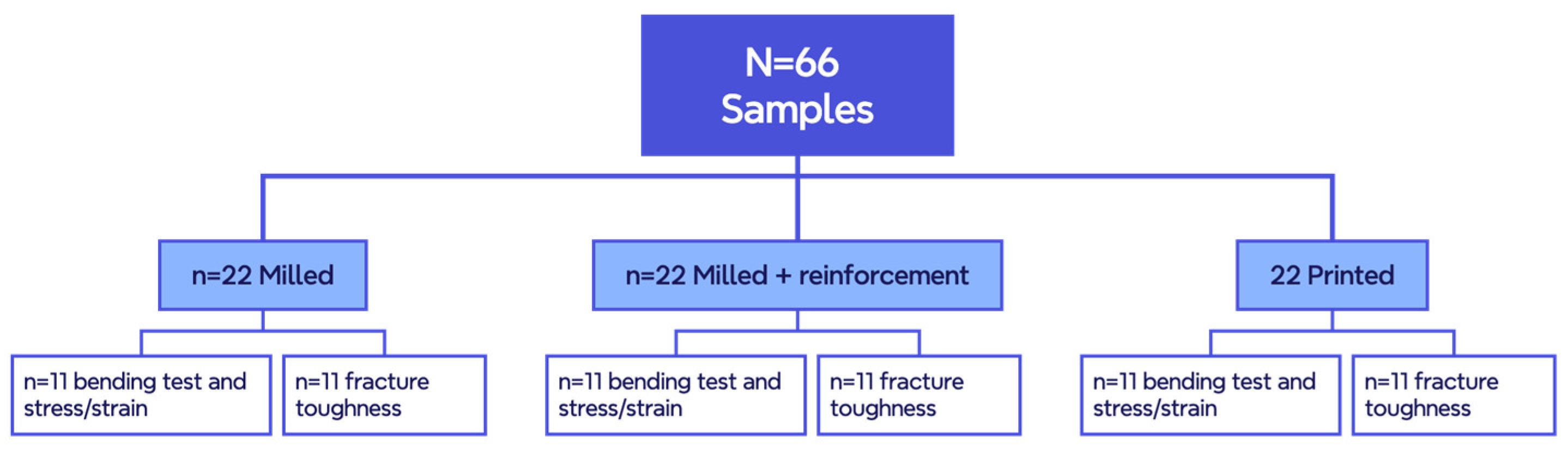
2.1. Experimental Design
2.2. Sample Design
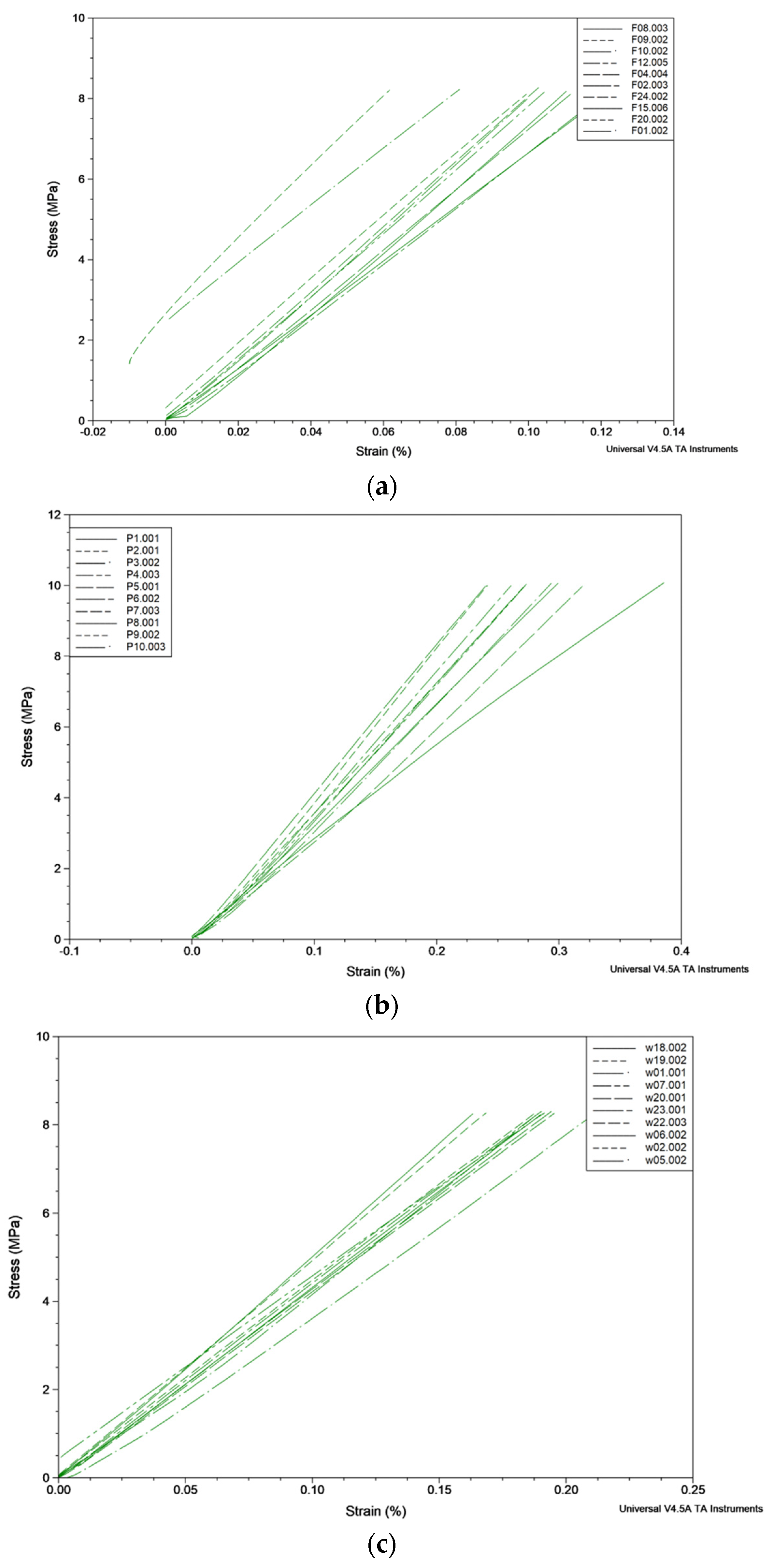
2.3. Deformation (Displacement) and Stress/Strain Curves within the Elastic Area
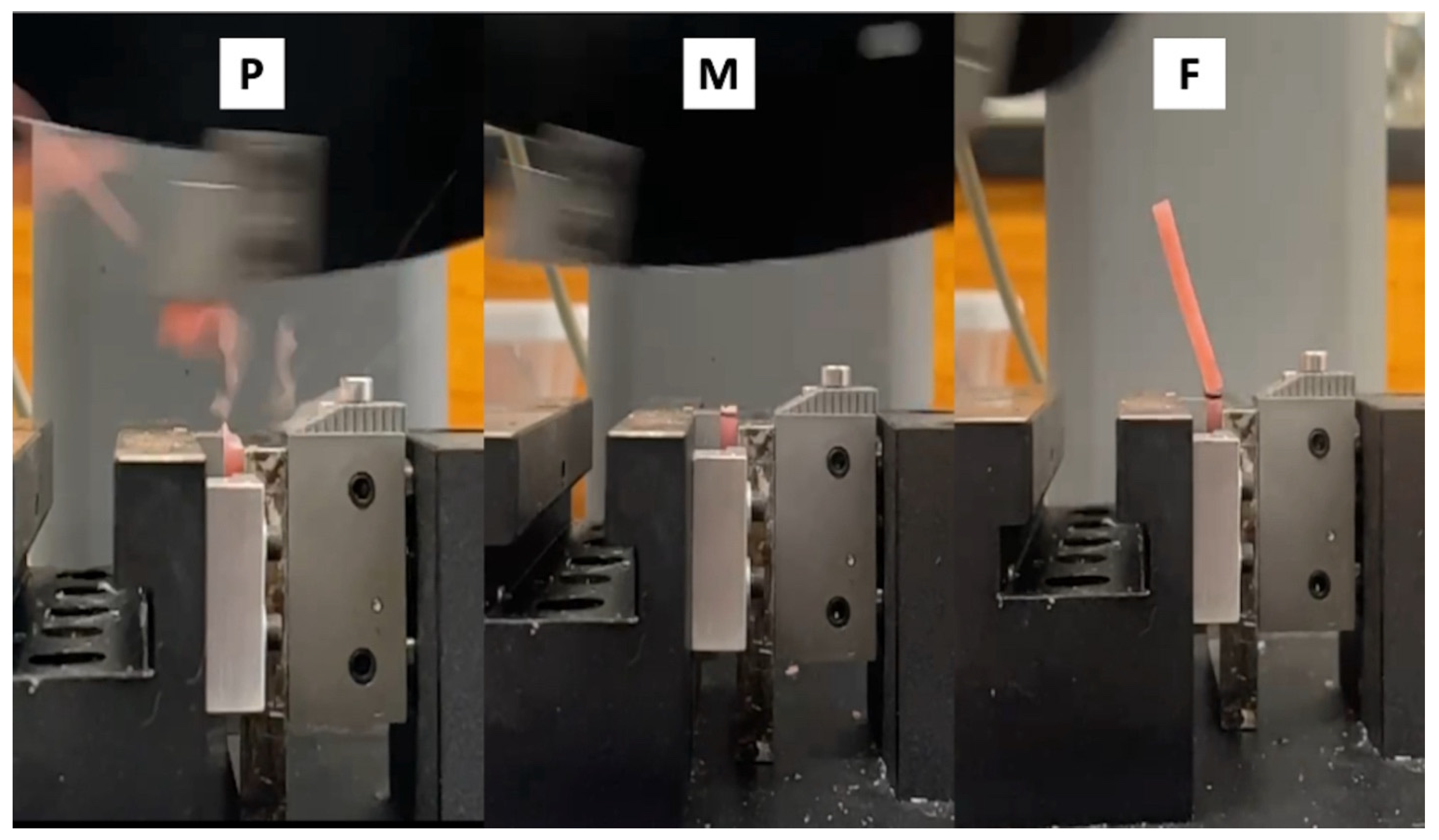
2.4. Impact Fracture Test
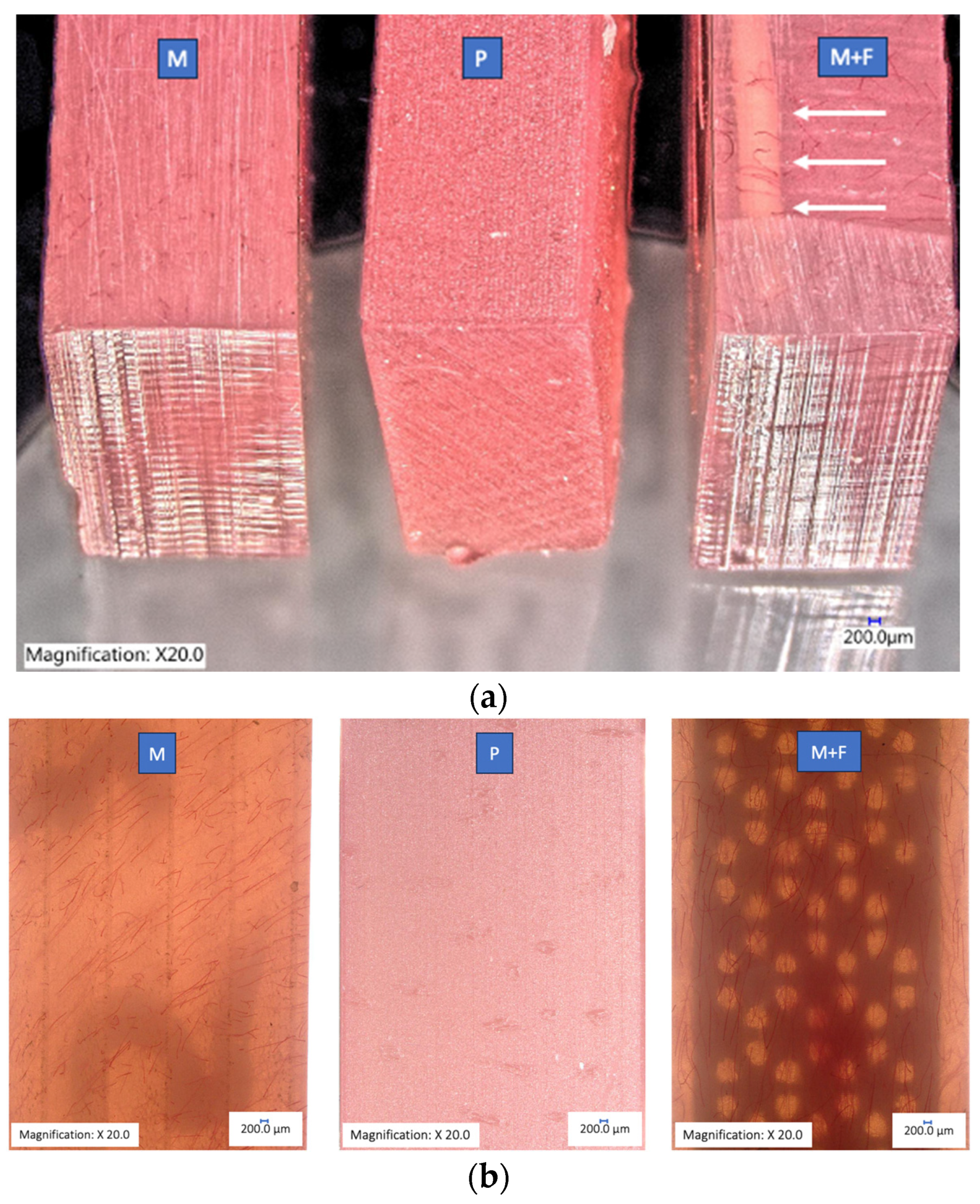
2.5. Fracture Analysis
3. Results
3.1. Stress/Strain Curves within the Elastic Area
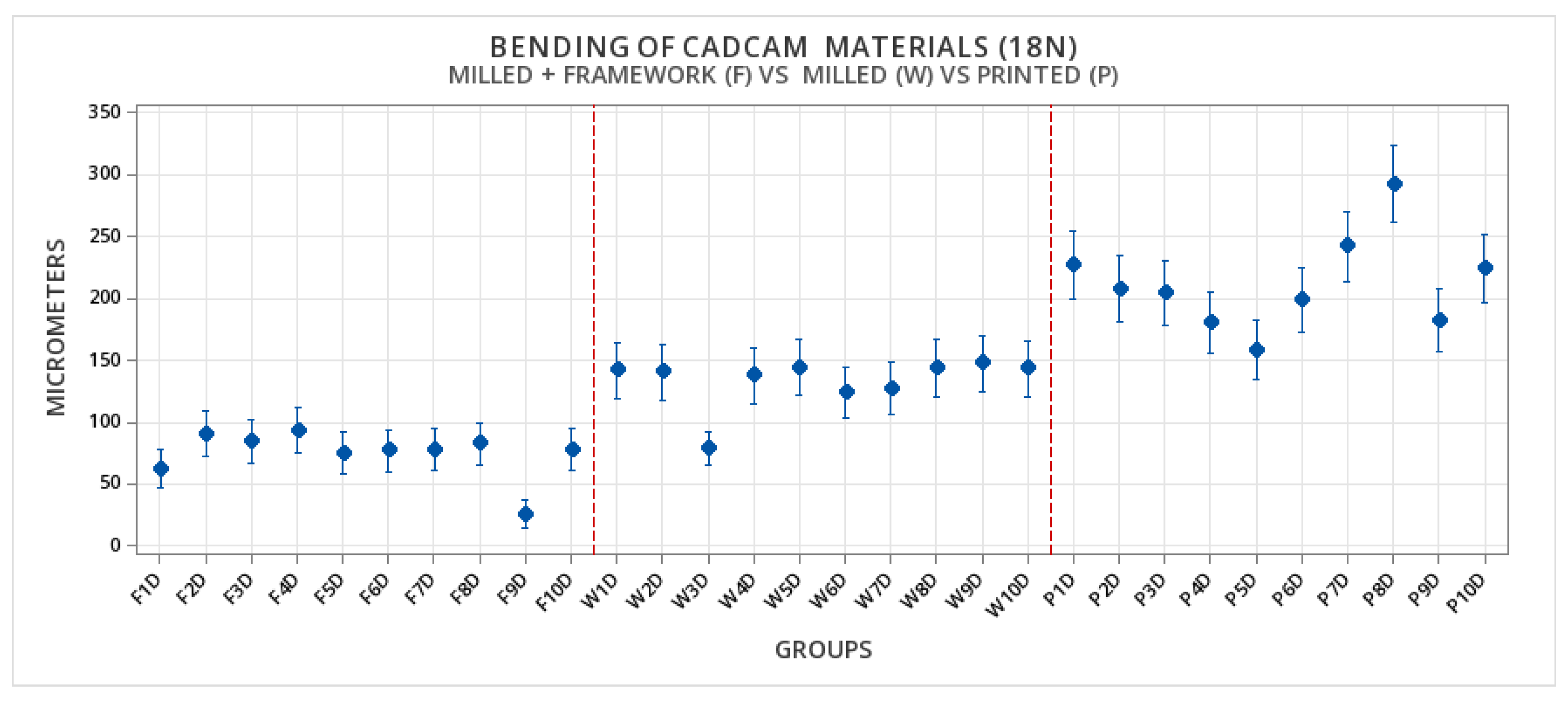
3.2. Deformation
Statistical Comparisons of the Elastic Deformation
3.3. Fracture Toughness Analysis
Statistical Comparisons of the Fracture Toughness of CAD/CAM Materials
3.4. Fractographic Analysis
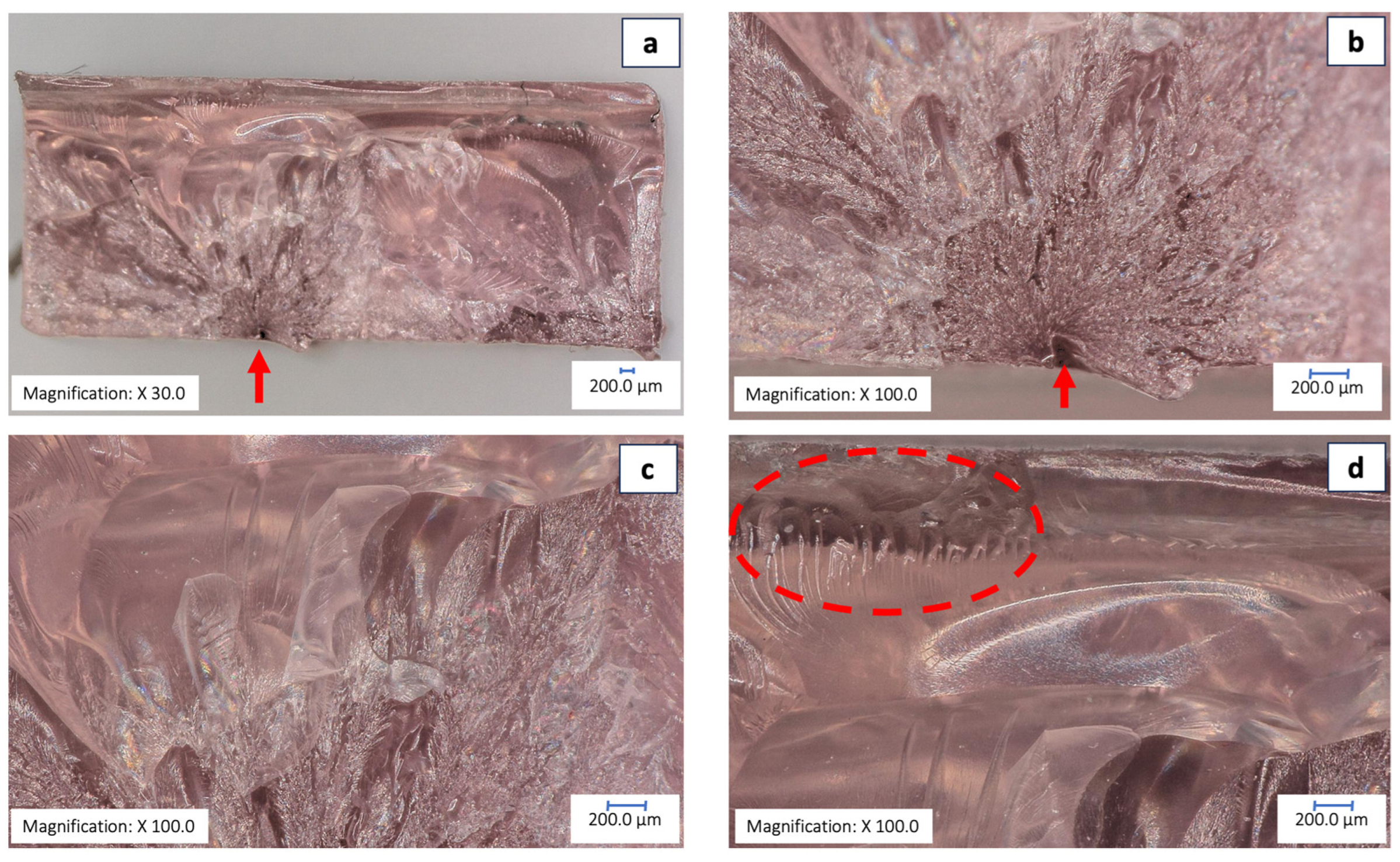
3.4.1. Fracture Analysis Printed Group
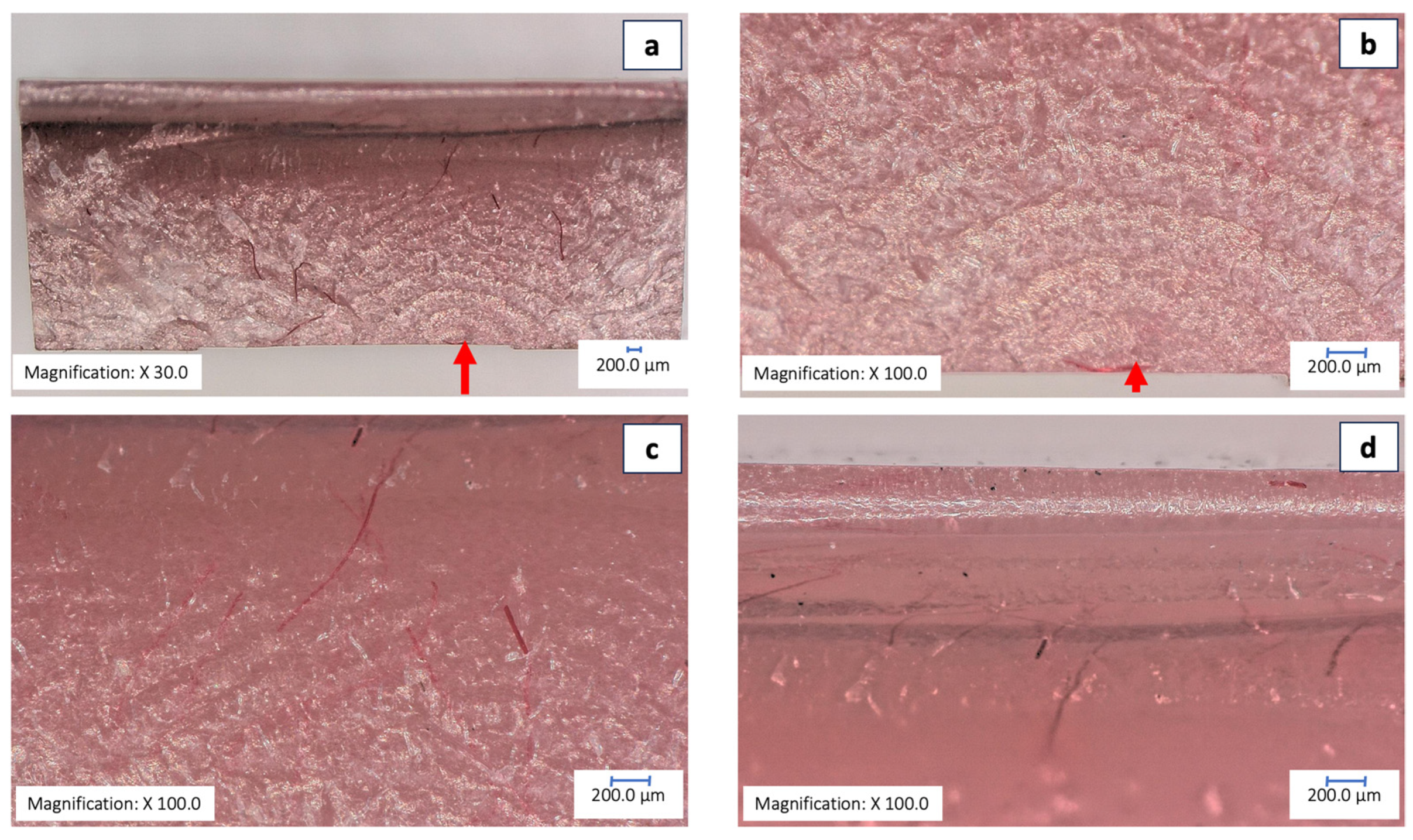
3.4.2. Fracture Analysis Milled Group
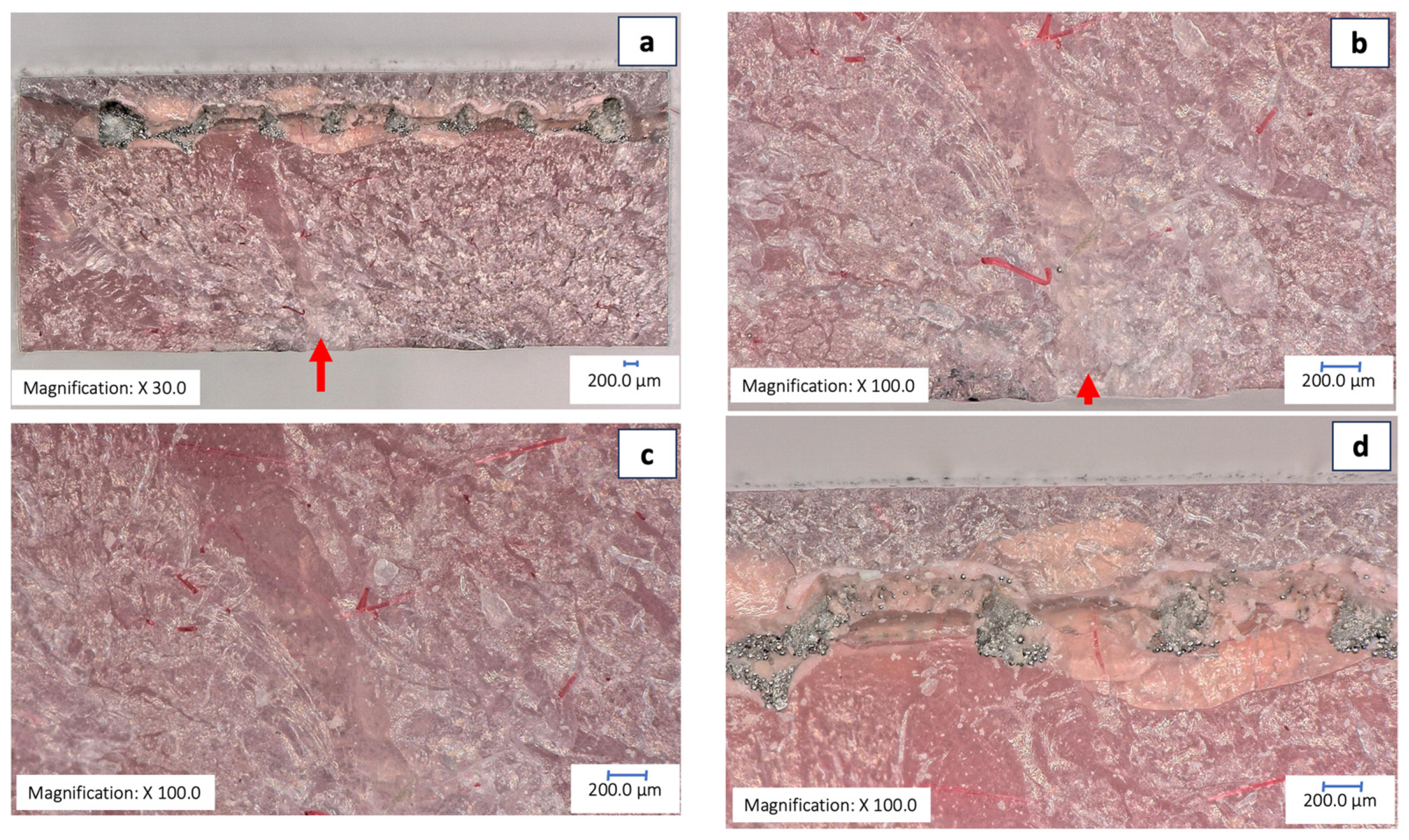
3.4.3. Fracture Analysis of the Milled-with-Framework Group
4. Discussion
4.1. Practical Implications
4.2. Opportunities for Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Xie, Q.; Ding, T.; Yang, G. Rehabilitation of Oral Function with Removable Dentures--Still an Option? J. Oral. Rehabil. 2015, 42, 234–242. [Google Scholar] [CrossRef] [PubMed]
- Salloum, A.M. Effect of Adding Basalt Powder on Flexural Strength of a Denture Base Acrylic Resin. BJSTR 2019, 18, 13205–13210. [Google Scholar] [CrossRef]
- Rickman, L.J.; Padipatvuthikul, P.; Satterthwaite, J.D. Contemporary Denture Base Resins: Part 1. Dent. Update 2012, 39, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Zafar, M.S. Prosthodontic Applications of Polymethyl Methacrylate (PMMA): An Update. Polymers 2020, 12, 2299. [Google Scholar] [CrossRef] [PubMed]
- Beyli, M.S.; von Fraunhofer, J.A. An Analysis of Causes of Fracture of Acrylic Resin Dentures. J. Prosthet. Dent. 1981, 46, 238–241. [Google Scholar] [CrossRef] [PubMed]
- Nandal, S.; Ghalaut, P.; Shekhawat, H.; Gulati, M. New Era in Denture Base Resins: A Review. Dent. J. Adv. Stud. 2013, 01, 136–143. [Google Scholar] [CrossRef]
- Prombonas, A.E.; Vlissidis, D.S. Comparison of the Midline Stress Fields in Maxillary and Mandibular Complete Dentures: A Pilot Study. J. Prosthet. Dent. 2006, 95, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Cilingir, A.; Bilhan, H.; Baysal, G.; Sunbuloglu, E.; Bozdag, E. The Impact of Frenulum Height on Strains in Maxillary Denture Bases. J. Adv. Prosthodont. 2013, 5, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Polyzois, G.L.; Tarantili, P.A.; Frangou, M.J.; Andreopoulos, A.G. Fracture Force, Deflection at Fracture, and Toughness of Repaired Denture Resin Subjected to Microwave Polymerization or Reinforced with Wire or Glass Fiber. J. Prosthet. Dent. 2001, 86, 613–619. [Google Scholar] [CrossRef]
- Wiskott, H.W.; Nicholls, J.I.; Belser, U.C. Stress Fatigue: Basic Principles and Prosthodontic Implications. Int. J. Prosthodont. 1995, 8, 105–116. [Google Scholar]
- Steinmassl, P.-A.; Wiedemair, V.; Huck, C.; Klaunzer, F.; Steinmassl, O.; Grunert, I.; Dumfahrt, H. Do CAD/CAM Dentures Really Release Less Monomer than Conventional Dentures? Clin. Oral. Investig. 2017, 21, 1697–1705. [Google Scholar] [CrossRef] [PubMed]
- Aldegheishem, A.; AlDeeb, M.; Al-Ahdal, K.; Helmi, M.; Alsagob, E.I. Influence of Reinforcing Agents on the Mechanical Properties of Denture Base Resin: A Systematic Review. Polymers 2021, 13, 3083. [Google Scholar] [CrossRef] [PubMed]
- Gad, M.M.; Abualsaud, R.; Al-Thobity, A.M.; Baba, N.Z.; Al-Harbi, F.A. Influence of Addition of Different Nanoparticles on the Surface Properties of Poly(Methylmethacrylate) Denture Base Material. J. Prosthodont. 2020, 29, 422–428. [Google Scholar] [CrossRef] [PubMed]
- Abdulrazzaq Naji, S.; Behroozibakhsh, M.; Jafarzadeh Kashi, T.S.; Eslami, H.; Masaeli, R.; Mahgoli, H.; Tahriri, M.; Ghavvami Lahiji, M.; Rakhshan, V. Effects of Incorporation of 2.5 and 5 Wt% TiO2 Nanotubes on Fracture Toughness, Flexural Strength, and Microhardness of Denture Base Poly Methyl Methacrylate (PMMA). J. Adv. Prosthodont. 2018, 10, 113. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.A.; Fareed, M.A.; Alshehri, A.H.; Aldegheishem, A.; Alharthi, R.; Saadaldin, S.A.; Zafar, M.S. Mechanical Properties of the Modified Denture Base Materials and Polymerization Methods: A Systematic Review. Int. J. Mol. Sci. 2022, 23, 5737. [Google Scholar] [CrossRef] [PubMed]
- Bangera, M.K.; Kotian, R.; Ravishankar, N. Effect of Titanium Dioxide Nanoparticle Reinforcement on Flexural Strength of Denture Base Resin: A Systematic Review and Meta-Analysis. Jpn. Dent. Sci. Rev. 2020, 56, 68–76. [Google Scholar] [CrossRef] [PubMed]
- Alla, R.K.; Sajjan, S.; Alluri, V.R.; Ginjupalli, K.; Upadhya, N. Influence of Fiber Reinforcement on the Properties of Denture Base Resins. JBNB 2013, 4, 91–97. [Google Scholar] [CrossRef]
- Oluwajana, F.; Walmsley, A.D. Titanium Alloy Removable Partial Denture Framework in a Patient with a Metal Allergy: A Case Study. Br. Dent. J. 2012, 213, 123–124. [Google Scholar] [CrossRef] [PubMed]
- Mourouzis, P.; Pandoleon, P.; Tortopidis, D.; Tolidis, K. Clinical Evaluation of Removable Partial Dentures with Digitally Fabricated Metal Framework after 4 Years of Clinical Service. J. Prosthodont. 2024, 33, 5–11. [Google Scholar] [CrossRef]
- Park, K.; Kang, N.-G.; Lee, J.-H.; Srinivasan, M. Removable Complete Denture with a Metal Base: Integration of Digital Design and Conventional Fabrication Techniques. J. Esthet. Restor. Dent. 2023, 36, 255–262. [Google Scholar] [CrossRef]
- Peterson, L.J.; Ellis, E.; Hupp, J.R.; Tucker, M.R. Contemporary Oral and Maxillofacial Surgery; Elsevier Health Sciences: Philadelphia, PA, USA, 2018. [Google Scholar]
- de Oliveira Limírio, J.P.J.; de Luna Gomes, J.M.; Alves Rezende, M.C.R.; Lemos, C.A.A.; Rosa, C.D.D.R.D.; Pellizzer, E.P. Mechanical Properties of Polymethyl Methacrylate as a Denture Base: Conventional versus CAD-CAM Resin—A Systematic Review and Meta-Analysis of in Vitro Studies. J. Prosthet. Dent. 2022, 128, 1221–1229. [Google Scholar] [CrossRef]
- Abdul-Monem, M.M.; Hanno, K.I. Effect of Thermocycling on Surface Topography and Fracture Toughness of Milled and Additively Manufactured Denture Base Materials: An in-Vitro Study. BMC Oral Health 2024, 24, 267. [Google Scholar] [CrossRef]
- Hanno, K.I.; Abdul-Monem, M.M. Effect of Denture Cleansers on the Physical and Mechanical Properties of CAD-CAM Milled and 3D Printed Denture Base Materials: An in Vitro Study. J. Prosthet. Dent. 2023, 130, 798.e1–798.e8. [Google Scholar] [CrossRef]
- Amaral, C.F.; Gomes, R.S.; Rodrigues Garcia, R.C.M.; Del Bel Cury, A.A. Stress Distribution of Single-Implant-Retained Overdenture Reinforced with a Framework: A Finite Element Analysis Study. J. Prosthet. Dent. 2018, 119, 791–796. [Google Scholar] [CrossRef]
- Fouda, S.M.; Gad, M.M.; Abualsaud, R.; Ellakany, P.; AlRumaih, H.S.; Khan, S.Q.; Akhtar, S.; Al-Qarni, F.D.; Al-Harbi, F.A. Flexural Properties and Hardness of CAD-CAM Denture Base Materials. J. Prosthodont. 2023, 32, 318–324. [Google Scholar] [CrossRef]
- Valenti, C.; Isabella Federici, M.; Masciotti, F.; Marinucci, L.; Xhimitiku, I.; Cianetti, S.; Pagano, S. Mechanical Properties of 3D-Printed Prosthetic Materials Compared with Milled and Conventional Processing: A Systematic Review and Meta-Analysis of in Vitro Studies. J. Prosthet. Dent. 2022. Online ahead of print. [Google Scholar] [CrossRef]
- Prpić, V.; Schauperl, Z.; Ćatić, A.; Dulčić, N.; Čimić, S. Comparison of Mechanical Properties of 3D-Printed, CAD/CAM, and Conventional Denture Base Materials. J. Prosthodont. 2020, 29, 524–528. [Google Scholar] [CrossRef]
- Takahashi, T.; Gonda, T.; Mizuno, Y.; Fujinami, Y.; Maeda, Y. Reinforcement in Removable Prosthodontics: A Literature Review. J. Oral Rehabil. 2017, 44, 133–143. [Google Scholar] [CrossRef]
- ELsyad, M.A.; Errabti, H.M.; Mustafa, A.Z. Mandibular Denture Base Deformation with Locator and Ball Attachments of Implant-Retained Overdentures. J. Prosthodont. 2016, 25, 656–664. [Google Scholar] [CrossRef]
- Gibreel, M.F.; Khalifa, A.; Said, M.M.; Mahanna, F.; El-Amier, N.; Närhi, T.O.; Perea-Lowery, L.; Vallittu, P.K. Biomechanical Aspects of Reinforced Implant Overdentures: A Systematic Review. J. Mech. Behav. Biomed. Mater. 2019, 91, 202–211. [Google Scholar] [CrossRef]
- Tokgoz, S.; Ozdiler, A.; Gencel, B.; Bozdag, E.; Isık-Ozkol, G. Effects of Denture Base Thicknesses and Reinforcement on Fracture Strength in Mandibular Implant Overdenture with Bar Attachment: Under Various Acrylic Resin Types. Eur. J. Dent. 2019, 13, 64–68. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Steinmassl, O.; Offermanns, V.; Stöckl, W.; Dumfahrt, H.; Grunert, I.; Steinmassl, P.-A. In Vitro Analysis of the Fracture Resistance of CAD/CAM Denture Base Resins. Materials 2018, 11, 401. [Google Scholar] [CrossRef] [PubMed]
- Galati, M.; Minetola, P. On the measure of the aesthetic quality of 3D printed plastic parts. Int. J. Interact. Des. Manuf. 2020, 14, 381–392. [Google Scholar] [CrossRef]
- Erokhin, K.; Naumov, S.; Ananikov, V. Defects in 3D Printing and Strategies to Enhance Quality of FFF Additive Manufacturing. A Review. 2023. Available online: https://chemrxiv.org/engage/chemrxiv/article-details/6516b0aba69febde9eea81b1 (accessed on 1 June 2024).
- Holzmond, O.; Li, X. In situ real time defect detection of 3D printed parts. Addit. Manuf. 2017, 17, 135–142. [Google Scholar] [CrossRef]
| Factor | N | Mean | StDev |
|---|---|---|---|
| Printed | 10 | 212.0 | 129.03 |
| Milled | 10 | 133.01 | 85.12 |
| Milled + reinforcement | 10 | 74.48 | 47.57 |
| Comparisons between Groups | Difference of Means | 95% CI | Adjusted p-Value |
|---|---|---|---|
| Milled Vs Printed | −79.0 | (−103.9, −54.0) | 0.001 |
| Milled + reinforced Vs Printed | −137.5 | (−162.5, −112.6) | 0.001 |
| Milled + reinforced Vs Milled | −58.5 | (−83.5, −33.6) | 0.002 |
| Groups | N | Mean | StDev |
|---|---|---|---|
| Milled kJ/m2 | 10 | 8.634 | 1.225 |
| Milled + reinforcement kJ/m2 | 10 | 15.203 | 2.244 |
| Printed kJ/m2 | 10 | 6.304 | 2.600 |
| Difference of Levels | Difference of Means | 95% CI | Adjusted p-Value |
|---|---|---|---|
| Milled + reinforcement Vs Milled | 6.569 | (4.968, 8.170) | 0.001 |
| Printed Vs Milled | −2.330 | (−3.931, −0.729) | 0.003 |
| Printed Vs Milled + reinforcement | −8.899 | (−10.499, −7.298) | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Delgado-Ruiz, R.; Brintouch, I.; Ali, A.; Fang, Y.; Romanos, G.; Rafailovich, M. The Effect of the Incorporation of a 3D-Printed Titanium Framework on the Mechanical Properties CAD/CAM Denture Base Materials. Prosthesis 2024, 6, 753-766. https://doi.org/10.3390/prosthesis6040053
Delgado-Ruiz R, Brintouch I, Ali A, Fang Y, Romanos G, Rafailovich M. The Effect of the Incorporation of a 3D-Printed Titanium Framework on the Mechanical Properties CAD/CAM Denture Base Materials. Prosthesis. 2024; 6(4):753-766. https://doi.org/10.3390/prosthesis6040053
Chicago/Turabian StyleDelgado-Ruiz, Rafael, Ido Brintouch, Aisha Ali, Yiwei Fang, Georgios Romanos, and Miriam Rafailovich. 2024. "The Effect of the Incorporation of a 3D-Printed Titanium Framework on the Mechanical Properties CAD/CAM Denture Base Materials" Prosthesis 6, no. 4: 753-766. https://doi.org/10.3390/prosthesis6040053
APA StyleDelgado-Ruiz, R., Brintouch, I., Ali, A., Fang, Y., Romanos, G., & Rafailovich, M. (2024). The Effect of the Incorporation of a 3D-Printed Titanium Framework on the Mechanical Properties CAD/CAM Denture Base Materials. Prosthesis, 6(4), 753-766. https://doi.org/10.3390/prosthesis6040053









